Thompson v. Raiford Unopposed Motion for Leave to File Brief and Brief Amici Curiae in Opposition to Defendant's Alternative Motions to Dismiss and For Summary Judgment with Declarations
Public Court Documents
November 23, 1992
Cite this item
-
Brief Collection, LDF Court Filings. Thompson v. Raiford Unopposed Motion for Leave to File Brief and Brief Amici Curiae in Opposition to Defendant's Alternative Motions to Dismiss and For Summary Judgment with Declarations, 1992. 13b8b204-c69a-ee11-be37-00224827e97b. LDF Archives, Thurgood Marshall Institute. https://ldfrecollection.org/archives/archives-search/archives-item/2f4dd95b-ebdc-4efa-9fd1-a77499c69160/thompson-v-raiford-unopposed-motion-for-leave-to-file-brief-and-brief-amici-curiae-in-opposition-to-defendants-alternative-motions-to-dismiss-and-for-summary-judgment-with-declarations. Accessed February 22, 2026.
Copied!
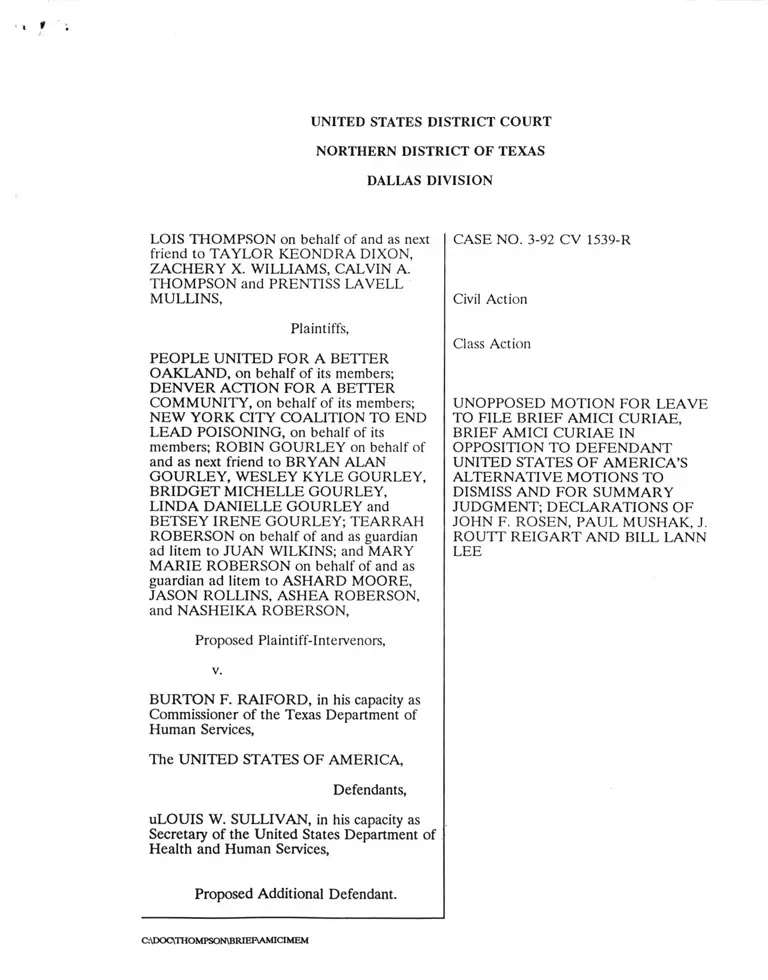
UNITED STATES DISTRICT COURT
NORTHERN DISTRICT OF TEXAS
DALLAS DIVISION
LOIS THOMPSON on behalf of and as next
friend to TAYLOR KEONDRA DIXON,
ZACHERY X. WILLIAMS, CALVIN A.
THOMPSON and PRENTISS LAVELL
MULLINS,
Plaintiffs,
PEOPLE UNITED FOR A BETTER
OAKLAND, on behalf of its members;
DENVER ACTION FOR A BETTER
COMMUNITY, on behalf of its members;
NEW YORK CITY COALITION TO END
LEAD POISONING, on behalf of its
members; ROBIN GOURLEY on behalf of
and as next friend to BRYAN ALAN
GOURLEY, WESLEY KYLE GOURLEY,
BRIDGET MICHELLE GOURLEY,
LINDA DANIELLE GOURLEY and
BETSEY IRENE GOURLEY; TEARRAH
ROBERSON on behalf of and as guardian
ad litem to JUAN WILKINS; and MARY
MARIE ROBERSON on behalf of and as
guardian ad litem to ASHARD MOORE,
JASON ROLLINS, ASHEA ROBERSON,
and NASHEIKA ROBERSON,
CASE NO. 3-92 CV 1539-R
Civil Action
Class Action
UNOPPOSED MOTION FOR LEAVE
TO FILE BRIEF AMICI CURIAE,
BRIEF AMICI CURIAE IN
OPPOSITION TO DEFENDANT
UNITED STATES OF AMERICA’S
ALTERNATIVE MOTIONS TO
DISMISS AND FOR SUMMARY
JUDGMENT; DECLARATIONS OF
JOHN F. ROSEN, PAUL MUSHAK, J.
ROUTT REIGART AND BILL LANN
LEE
Proposed Plaintiff-Intervenors,
v.
BURTON F. RAIFORD, in his capacity as
Commissioner of the Texas Department of
Human Services,
The UNITED STATES OF AMERICA,
Defendants,
uLOUIS W. SULLIVAN, in his capacity as
Secretary of the United States Department of
Health and Human Services,
Proposed Additional Defendant.
C:\DOC\THOMPSON\BRIEF\AMICIMEM
BRIEF AMICI CURIAE
TABLE OF CONTENTS
Interest of Amici ............................................................................................................................. 1
Introduction .................................................................................................................................... 1
Summary of Argument ................................................................................................................. 2
Statement ......................................................................................................................................... 3
A. The Extent of Lead Poisoning in Poor Children ................................................. 3
1. Prevelence............................................................................................................ 3
2. Exposure.............................................................................................................. 4
3. Symptoms ............................................................................................................ 6
B. The Appropriate Test for Poor Children .............................................................. 6
Argument ............................................................................................................................................ 8
A. The Plain Terms of the Statute Require A Blood Lead Test............................. 8
B. Legislative History Confirms that Congress Intended to Mandate A
Blood Lead Test to Screen For Lead Poisoning............................................... 10
C. The Agency Construction of the Statute Is Entitled to No Deference............. 11
D. The Remedial Purpose of the EPSDT Statute and the CDC Report Mandate
that Blood Lead Testing Be Required................................................................ 14
1. The Remedial Purpose of the EPSDT Statute Requires Blood Lead
Testing .................................................................................................... 13
2. The CDC Statement Requires Blood Lead Testing ..................... 13
Inappropriateness of Questioning and EP Testing for Screening . . 15
Indefinite Transiton Period..................................................................... 16
Conclusion......................................................................................................................................... 19
Affidavit of John F. R o se n ............................................................................................................ 21
Declaration of Paul M ushak........................................................................................................... 126
Declaration of J. Routt Reigart ....................................................................................................276
Declaration of Bill Lann Lee ................................................................................ 280
C:\DOC\THOMPSON\PLEADING\AMICIMEM 1
TABLE OF AUTHORITIES
Cases: Pages:
American Tobacco Co. v. Patterson,
456 U.S. 63 (1 9 8 2 )........................................................................................................... 9, 11
Beltran v. Myers,
701 F.2d 91, (9th Cir.) ceret denied sub nom.,
Rank v. Beltran, 462 U.S. 1134 (1 9 8 3 ).............................................................................. 9
Chandler v. Roudebush,
425 U.S. 840 (1 9 7 6 )............................................................................................................ 11
Chevron, U.S.A., Inc., v. Natural Resources Defense Council, Inc.,
467 U.S. 837 (1984).............................................................................................................. 12
Citizens Action League v. Kizer,
887 F.2d 1003 (9th Cir. 1989), cert denied,
494 U.S. 1056 (1 9 9 0 ) ............................................................................................................ 8
Consumer Product Safety Com’n v. GTE Sylvania, Inc.
447 U.S. 102 (1 9 8 0 ).............................................................................................................. 8
EEOC v. Arabian American Oil Co.,
113 L.Ed.2d 274 (1991) .................................................................................................... 13
Fleetwood Enterprises, Inc., v. U.S. Department of Housing and Urban Development,
818 F.2d 1188 (5th Cir. 1987).......................................................................................... 12
Fort Stewart Schools v. Federal Labor Relations Authority,
495 U.S. 641 (1 9 9 0 )............................................................................................................ 12
General Electric Co. v. Gilbert,
429 U.S. 125 (1 9 7 6 )............................................................................................................ 13
K Mart Corp. v. Cartier, Inc.,
486 U.S. 281 (1 9 8 8 )............................................................................................................ 12
United States v. Chen,
913 F.2d 183 (5th Cir. 1990) ............................................................................................. 8
United States v. Moody,
923 F.2d 341 (5th Cir.) cert, denied, 112 S.Ct. 80 (1991)............................................... 8
West Virginai University Hospitals Inc., v. Casey,
111 S.Ct. 1138, 113 L.Ed.2d 68, (1 9 9 1 ) ....................................................................... 8, 11
Statutes and Regulations:
42 U.S.C. §1396d(r)(i)(B)(iv) .............................................................................................. passim
42 U.S.C. §1396(a)(a)(43)..................................... .......................................................................... 9
42 U.S.C. §1396d(a)(4)(B) ............................................................................................................. 9
42 U.S.C. §1396d(r)......................................................................................................................9, 11
16 C.F.R. pt 1303 ...................................................................................................................................
42 U.S.C. §1396d(a).......................... ............................................................................................ 10
C:\DOC\THOMPSON\PLEADING\AMICIMEM 11
Pages:
Other Materials'.
Centers for Disease Control,
Statement on Preventing Lead Poisoning in Young Children (1991) ............ passim
Conference Report on H.R. 101-386,
101 Cong., 1st Sess. (1989)............................................................................................... 12
HHS, The Nature and Extent of Lead Poisoning in Children in the United States:
A Report to Congress (1 9 8 8 )................................................................................... passim
HHS, Strategic Plan for the Elimination of Childhood Lead Poisoning (1991) . . . . passim
H. R. Rep. No. 213, 89th Cong., 1st Sess. (1 9 6 5 )..................................................................... 9
McElvain, M.D., Orbach, H.G., Binder, S., Blanksma, L.A., Maes, E.F. and Krieg, R.M.
"Evaluation of the Erythrocyte Protoporphyrin Test as a Screen
for Elevated Blood Lead Levels," 1 1 9 / Pediatrics 548 (1991)........................... 10, 11
Report of the House Budget Comm, on H.R. 3299
101 Cong. 1st Sess., (Sept. 20, 1989) reprinted in
Medicare and Medicaid Guide (CCH)
Extra Edition No. 596 (October 5, 1989) ........................................................ 11, 12, 14
State Medicaid M anual..............................................................................................................14, 18
Welfare of Children,
H.R.Doc. No.54, 90th Cong., 1st Sess.7 (1967) .......................................................... 14
C:\DOC\THOMFSON\PLEADINGVAMICIMEM 111
UNOPPOSED MOTION FOR LEAVE TO
FILE BRIEF AMICI CURIAE
Proposed plaintiff-intervenors People United for a Better Oakland, et al. seek leave to
submit the attached brief amici curiae in response to federal defendant’s alternative motions
to dismiss and for summary judgment. Leave should be granted for the following reasons:
1. Proposed plaintiff-intervenors are parents and guardians of Medicaid eligible
children from North Carolina, and organizations that advocate adequate screening for lead
poisoning whose members include parents and guardians of Medicaid eligible children from
California, Colorado and New York.
2. Proposed plaintiff-intervenors have submitted a motion to intervene in the instant
proposed nationwide class action to challenge federal defendant’s failure to comply with the
requirements of the Medicaid statute for mandatory blood lead testing of poor children.
3. Proposed plaintiff-intervenors submit this brief amici curaie because federal
defendants’ alternative motions may dispose of the issues on which they wish to be heard as
plaintiff-intervenors while their motion to intervene is still pending.
4. Proposed plaintiff-intervenors and their counsel — the NAACP Legal Defense Fund,
National Health Law Program and New York and North Carolina legal services offices — have
experience which the Court may find of assistance. They also have obtained declarations from
leading medical and public health experts on factual issues presented by federal defendant’s
alternative motions.
5. Both plaintiffs and federal defendant consent to the filing of the brief.
6. Should the motion to intervene be granted, proposed plaintiff-intervenors adopt this
brief as their response to federal defendant’s alternative motions.
////
////
////
////
////
////
C:\DOC\THOMPSON\PLEADING\AMICIMEM 1
Wherefore, proposed plaintiff-intervenors request that leave be granted to file the
enclosed brief amici curiae.
Dated: November 23, 1992
Respectfully submitted,
Edward B. Cloutman, III
Law Office of Edward B. Cloutman, III
3301 Elm Street
Dallas, TX 75226
(214) 939-9222
Julius L. Chambers
Alice Brown
NAACP Legal Defense & Educational
Fund, Inc.
99 Hudson Street, Suite 1600
New York, NY 10013
(212) 219-1900
Bill Lann Lee
Kirsten D. Levingston
NAACP Legal Defense & Educational
Fund, Inc.
315 West Ninth Street, Suite 208
Los Angeles, CA 90015
(213) 624-2405
Jane Perkins
National Health Law Program
313 Ironwoods Drive
Chapel Hill, NC 25716
(202) 887-5310
Carlene NcNulty
North State Legal Services
114 West Corbin Street
Hillsborough, N.C. 27278
(919) 732-8137
Lucy Billings
Marie-Elena Ruffo
Bronx Legal Services
579 Courtlandt Avenue
(212) 993-6250
Edward B. Cloutman, III
Texas Bar No. 04411000
By_________________________
Bill Lann Lee
Attorneys for Amici
People United for a Better Oakland, et al.,
C:\DOC\THOMPSON\PLEADING\AMICIMEM 2
BRIEF AMICI CURIAE
Interest of Amici
Amici are advocacy organizations whose members include parents and guardians of
Medicaid eligible children from California, Colorado and New York as well as parents and
guardians of Medicaid eligible children from North Carolina. They have submitted a pending
motion to intervene as plaintiff-intervenors.
Amici parents and guardians, and parent and guardian members of amici organizations
seek either to obtain effective screening for lead poisoning or to safeguard effective screening
that is threatened by the actions of federal defendant. Amici are representatives of the
proposed nationwide plaintiff class of poor children, and their parents and guardians.
Introduction
The key substantive issue before the Court is the meaning of the Medicaid Act
provision that Early and Periodic Screening, Diagnostic and Treatment (hereinafter "EPSDT')
program "screening services . . . shall at a minimum include laboratory tests including lead
blood level assessment appropriate for age and risk factors" for lead poisoning. 42 U.S.C.
§1396d(r)(l)(B)(iv). Conceding that a blood lead level test, which directly assesses lead blood
levels, is "the test of choice" to screen for lead poisoning, USA motion 14, federal defendant
nevertheless contends that it may permit the use of an erythrocyte protoporphyrin (hereinafter
"EP") test, in combination with a verbal questionnaire for screening. This contention is
advanced notwithstanding the finding of federal defendant’s expert, as well as all others who
have studied the problem, that only a blood lead test can effectively detect lead poisoning and
that the EP test fails to identify most children who have been poisoned by lead.
As we show below, the statutory language, legislative history and remedial purpose of
the statute require that only a blood lead level test be used to screen for lead poisoning.
Summary judgment for federal defendant should be denied, and the Court should entertain
a summary judgment motion on behalf of plaintiffs and proposed plaintiff-intervenors.1
1Amici incorporate by reference plaintiffs’ arguments about standing. With respect to
the propriety of a TRO or preliminary injunction, the Court may wish to defer any such
ruling unless a summaiy judgment proves inadequate to protect the interests of plaintiffs
and plaintiffs-intervenors.
C:\DOC\THOMPSON\PLEADING\AMICIMEM 1
Summary of Argument
A. The terms of a statute are controlling unless they are unclear or ambiguous. In the
case of §1396d(r)(l)(B)(iv), the Medicaid Act clearly, unambiguously specifies that a
laboratory test to assess "lead blood level" or Pb-B is required under the EPSDT program.
All the parties agree that the only laboratory test that directly assesses Pb-B levels is a blood
lead test. The EP test, not a lead blood level test, cannot, as claimed by the government,
provide an accurate "indirect" measure of lead blood level. It is in fact completely unreliable,
identifying only one out of seven or eight children with toxic lead blood levels.
B. Legislative history is sparse but no less supportive of plaintiffs’ position. Prior to
1989, the Medicaid Act did not specifically require lead blood level assessments as a
mandatory part of the EPSDT screen. During the 1970’s the U.S. Department of Health and
Human Services ("HHS") had instructed state Medicaid agencies that the EP test was to be
used by EPSDT providers who decided to screen for lead poisoning. In 1988, however, the
Agency for Toxic Substances and Disease Registry presented a pivotal report to Congress, The
Nature and Extent of Lead Poisoning in Children in the United States: A Report to Congress
(hereinafter "Report to Congress"), Exhibit B to Declaration of Paul Mushak (hereinafter
"Mushak decl."), which quantified extensive levels of lead poisoning among poor children and
also concluded: "Reliance on EP level for initial screening can result in a significant incidence
of false negatives or failures to detect toxic Pb-B levels." Report to Congress II-9. The Report
to Congress formally recommended to Congress that the EP test not be used to screen for lead
poisoning. Just a year later, Congress passed amendments to the Medicaid Act which codified
and changed the EPSDT program, specifically to add a laboratory testing requirement for
"lead blood level assessment appropriate for age and risk factors." 42 U.S.C.
§1396d(r)(l)(B)(iv).
C. The federal defendant’s construction of the statute is entitled to no deference in
light of the unambiguous statutory language and legislative background. Moreover, this
construction contradicts its other recent pronouncements on the subject, such as the 1991
Strategic Plan for the Elimination of Childhood Lead Poisoning (hereinafter "Strategic Plan"),
Exhibit B to Declaration of John F. Rosen (hereinafter "Rosen decl."), which declares that
C:\DOCVTHOMPSON\PLEADING\AMICIMEM 2
"blood lead measurements must be used for childhood lead screening instead of EP
measurements." Strategic Plan 23 (emphasis added). Finally, the federal defendant’s position
is simply incorrect as a factual matter. The federal defendant admits that neither a verbal risk
assessment nor the EP test are able adequately to screen for lead poisoning. Yet, it asks the
Court to accept that these two inadequate tests, combined together, somehow produce the
valid "lead blood level assessment" that is required by Congress. The experts reject this
approach -- as has the federal defendant itself by admitting that this scheme is to be used as
an interim measure during an undefined transition to universal use of the congressionally-
mandated lead blood level assessment for poor children.
D. The purpose of §1396d(r)(iv) is remedial and it is to be construed liberally to
advance the overall goal of the EPSDT program to improve the nation’s health by early
detection and prevention of childhood illnesses. If, as federal defendant concedes, the
majority of Medicaid eligible children are at high risk for lead poisoning, §1396d(r)(l)(B)(iv)
should be read to require blood lead testing to assess Pb-B levels consistent with the Statement
on Preventing Lead Poisoning in Young Children issued in 1991 by the Centers for Disease
Control (hereinafter "CDC Statement"), Exhibit 1 to Declaration of Sue Binder (hereinafter
"Binder decl."). EP testing and verbal questioning (alone or in combination) are ineffective
substitutes. Purported limited laboratory capacity is a mere pretext. See Declarations of John
F. Rosen (Chairperson of the CDC’s Advisory Committee Childhood Lead Poisoning
Prevention Advisory Committee); Paul Mushak (author of the 1988 Report to Congress)-, and
J. Routt Reigart (Chairman of the American Academy of Pediatrics Committee on
Environmental Health) (hereinafter "Reigart decl.")
Statement
A. The Extent of Lead Poisoning in Poor Children.
1. Prevalence.
Lead poisoning, according to HHS, is "the most common and societally devastating
environmental disease of young children." Strategic Plan xiv. Using the outdated definition
of lead poisoning in 1988, the Report to Congress found that in 1984 2.4 million white and
African-American pre-school children — 17% of all such children - in metropolitan areas had
C:\DOC\THOMPSON\PLEADING\AMICIMEM 3
projected toxic lead blood levels, and that 400,000 fetuses per year are at risk of being bom
lead poisoned. See Mushak deck at 11 16; Rosen deck at 11 13.
Medicaid eligible children by definition are at high risk for lead poisoning. Their low
income status is an indicator that they live in older, deteriorated or recently rehabilitated
housing that has exposed them to lead paint. The 1988 Report to Congress, showed the
incidence of lead poisoning is 2-3 times higher among other Medicaid eligible children than
among other children of the same age. See Rosen deck at 11 30; Reigart deck at HIT 11-12;
Hiscock deck at H 20.
Applying the CDC’s present 10 jxg/dL toxicity level to 1984 national data shows the
following prevalence projections in America’s poor communities: In smaller cities with
populations less than one million, 79% of all children with family incomes below $6000 —
91.6% of all African-American children — were projected to have lead levels exceeding the
new CDC action level of 10 /xg/dL. In larger cities, 88% of all children with family incomes
below $6000 — 96.5% of all African-American children -- were projected to be affected. For
children living in smaller cities whose families earn between $6000 and $14,999, approximately
67% had blood lead levels associated with early toxicity; 83% of African-American children
in this category were affected. In larger cities, 78.5% of all children whose families earn
between $6000 - $14,999 -- 92% of all African-American children — have lead levels at or
exceeding the 10 /xg/dL level. Prevalence of blood lead levels above 5 /xg/dL, a level only one-
half that for early toxicity, in poor children is virtually 100 percent. While corresponding
prevalence for the current year, 1992, will be lower overall, it is likely that inner-city, poor
children will show the least declines. See Mushak deck at HU 18 - 19.
According to the CDC Statement, "[although all children are at risk for lead toxicity,
poor and minority children are disproportionately affected. Lead exposure is at once a by
product of poverty and a contributor to the cycle that perpetuates and deepens the state of
being poor." CDC Statement 12.
2. Exposure.
Ingesting lead particles can cause severe damage to the brain and central nervous
system. Children from birth through age six years are by definition at risk from lead
C:\DOC\THOMPSON\PLEADING\AMICIMEM 4
poisoning. Their normal hand-to-mouth activity causes more frequent ingestion of lead
particles. More significantly, the developmental stages of children’s brains and nervous systems
are particularly vulnerable. Environmental factors may put older children at risk. Ingestion
of lead particles by pregnant women also causes damage to the developing fetus. See Rosen
decl. at U 12 - 13; Mushak deck at H 10 - IT, Report to Congress 1, 10, III-12, IV-7; CDC
Statement 7 - 12.
As detailed extensively in the 1988 Report to Congress, lead is pervasive in the
environment. Children are exposed to lead from six environmental sources, three of which still
persist as major sources or pathways: paint, dust/soil, and water. Lead in gasoline, foods, and
stationaiy sources is declining in importance. Although residential use of lead-based paint is
now banned, lead paint in existing housing remains the most widespread and dangerous high-
dose source of lead exposure for young children. Lead paint remains in over 57,000 homes
nationwide; 74% of all homes constructed before 1980 contain lead paint. Lead paint
continues to be used on the exteriors of painted steel structures, such as bridges and
expressways. Children living near such sites as expressways have been shown to have elevated
blood lead levels. See Mushak deck at H 12; Rosen deck at 11 14; 16 C.F.R. pt 1303; CDC
Statement 18.
Lead deposited in soil or as dust does not biodegrade or decay since lead is a chemical
element. Children playing around contaminated dust and soil will remain exposed indefinitely.
The water distribution system can also pose a lead risk. Contamination of drinking water
occurs in or near residences and schools when lead leaches into water from lead connectors,
service pipes, lead-soldered joints, or lead-lined watercoolers. See Mushak deck at 111113 -14.
Lead entering the body from different sources and through different pathways presents
a combined toxicological threat. Thus, multiple, low-level inputs of lead can result in
significant aggregate exposure. See Mushak deck at 11 15. See Report to Congress 6 - 8 ,
chapters VI & VIII.
C:\DOCVTHOMPSON\PLEADING\AMICIMEM 5
3. Symptoms.
Very severe lead poisoning (associated with lead levels at or above 80 p,g/dL) can result
in coma, convulsions, profound mental retardation, and even death. At lower concentrations,
lead mainly interferes with normal development of IQ and other neuro-behavioral measures
in children; with the body’s heme-forming system, which is critical to the production of heme
and blood; and with the vitamin D regulatory system, which involves the kidneys and plays an
important role in calcium metabolism. See Mushak decl. at H 10; Rosen deck at H 16.
Lead poisoning is often asymptomatic in its early stages, and its symptoms are the same
as many other childhood diseases and impairments. Lead toxicity produces altered behavior
such as attention disorders, learning disability, and cognitive disturbances. Symptoms and signs
of severe toxicity are fatigue, pallor, constipation, vomiting, and changes in consciousness
(coma) due to early encephalopathy, which may lead to death. Mental retardation is a
frequent result. See Rosen deck at U 17; CDC Statement 7-15.
According to currently published data, all cases of lead poisoning cause some persisting,
irreversible brain damage, reduced IQ, delayed cognitive development, and other physical and
mental impairments. Such effects occur at blood lead levels above and even below 10 /xg/dL.
In fact, there is no apparent threshold. Lead causes adverse effects even below 2 /zg/dL. At
least three longitudinal studies of young children in Boston, Cincinnati and Australia show that
prenatal and early childhood exposure to lead has adverse effects at low exposure levels on
a child’s IQ and other neurobehavioral measures, and that these effects persist into the school-
age years. See Rosen deck at U 16; Mushak deck at U 11.
B. The Appropriate Test for Poor Children.
The only way to determine that lead poisoning is the cause of such symptoms and to
bring them to a halt is to test for the level of lead in blood or Pb-B. According to all recent
scientific studies, only direct measurement of blood lead concentration has the clinical and
diagnostic capability to determine whether a child has lead poisoning. 1988 Report to Congress-,
1991 Strategic Plan-, 1991 CDC Statement 41. See Rosen deck at 11 18. The parties agree that
only a blood lead test directly measures Pb-B. See USA motion 12.
C:\DOC\THOMPSON\PLEADINO\AMICIMEM 6
Verbal questioning about a child’s possible exposure to lead does not provide a lead
blood level assessment, nor can it elicit complete, definitive, or accurate data to indicate a
child’s blood lead level. Many patients, especially Medicaid recipients, simply may not know
all the answers to the verbal assessment questions. See Rosen decl. at 11 19, Mushak decl. at
11 19; Reigart decl. at H 9. According to the CDC, "[t]he questions are not a substitute for a
blood lead test." CDC Statement 42 (original emphasis).
A blood test that does not test for the level of lead in blood does not elicit complete,
definitive, or accurate enough data either. The EP test is such a test. The EP test does not
test for the level of lead in blood at all. In fact, it is only an indirect reflection of iron or lead
status. For lead status, this test is an insensitive index of any blood lead values below 40
/xg/dL. At blood lead values between 10 and 30 /zg/dL, EP measurements will totally fail as
a screening method to identity the overwhelming majority (over 95%) of children whose blood
lead levels fall in this danger zone. See Rosen decl. at U 20; Mushak decl. at 11 23 - 24; Reigart
decl. at 11 10.
The EP test - a low cost, high volume procedure - is used to predict lead absorption.
In children exposed to elevated concentrations of lead, the lead interferes with the body’s
ability to make heme, which is used to carry oxygen when in the form of hemoglobin. Lead
retards formation of heme from the protoporphyrin molecule and protoporphyrin builds up
in the blood. The EP test measures this build up of protoporphyrin. It does not give directly
discreet blood lead concentrations; rather, protoporphyrin levels are a surrogate indicator for
the likelihood of elevated blood lead levels.
At the clinic operated by the Lead Poisoning Prevention Program at the Montefiore
Medical Center, Bronx, New York, where Dr. Rosen has performed blood lead tests and EP
tests together, there have been a significant number of cases where the EP test result was
normal, and the blood lead level was above 25 /zg/dL. Such occurrences were demonstrated
nationally by the Second National Health and Nutrition Examination Survey (NHANES II),
in 1976-90. See Rosen declaration at 1121; Report to Congress V-31. Significantly, the data was
analyzed and presented to Congress in the 1988 Report to Congress. O f 118 children with Pb-B
levels above 30 /zg/dL (the CDC criterion level at the time of the NHANES II study), 47% had
C:\DOCVTHOMPSON\PLEADING\AMICIMEM 7
EP levels at or below 30 /xg/dL, and 58% had EP levels less than an EP cutoff value of 35
/xg/dL. Report to Congress II-9. Of course, the CDC has revised the criterion level to 10
jag/dL, an action which introduces even more false negatives into the EP test results. See
Mushak decl at 11 24.
In sum, the EP test serves only to predict the presence of lead in the blood. It cannot,
however, be used as a predictive surrogate for lead blood levels below 40 pgJtiL. The test does
not act as a preventive test which allows the health care provider to detect lead poisoning at
its early, more manageable stages. Rather, the EP test can only accurately predict that
unacceptably high lead exposure and greater risk of more severe poisoning have already
occurred. See Mushak decl. at 11 25.
For a pediatrician pursuing a diagnosis, the only responsible course of action is to carry
out a test that provides safe and definitive results for all children, according to current
standards of pediatric practice. A blood lead test provides definitive information concerning
the extent to which a child has been recently exposed to lead. An EP test provides, only for
one child out of seven or eight, at best, marginal information indicating that a child may be
lead poisoned. For a pediatrician seeking a conclusive diagnosis, to perform such an
unreliable test for lead poisoning is irresponsible pediatric practice. See Rosen decl. at H 22;
see also Reigart decl. at 1111 10, 11 & 13; See Mushak decl. at 1111 23, 25 - 26.
Argument
A. The Plain Terms of the Statute Require A Blood Lead Test.
In construing a statute, we look first to the plain meaning of the statutory language.
Consumer Product Safety Com’n v. GTE Sylvania Inc., 447 U.S. 102, 108 (1980). Terms used
by a statute are to be given their ordinary, commonly understood meaning. United States v.
Moody, 923 F.2d 341, 347 (5th Cir.), cert, denied, 112 S.Ct. 80 (1991); United States v. Chen,
913 F.2d 183,189 (5th Cir. 1990); Citizens Action League v. Kizer, 887 F.2d 1003, 1006 (9th Cir.
1989), cert denied, 494 U.S. 1056 (1990). Where the statutory language is clear and
unambiguous, consideration of legislative history and other extrinsic guidance is unnecessary.
See, e.g., West Virginia Univ. Hospitals, Inc., v. Casey, 111 S.Ct. 1138,113 L.Ed.2d 68, 83 (1991)
("[w]here, as here, the statute’s language is plain, ‘the sole function of the court is to enforce
C:\DOC\THOMPSON\PLEADING\AMICIMEM 8
it according to its terms.’") (citation omitted); American Tobacco Co. v. Patterson, 456 U.S.
63, 68 (1982).
The instant case concerns the EPSDT provisions of the Medicaid Act, which was passed
by Congress in 1965 as a cooperative federal-state medical assistance program for the poor.
See Beltran v. Meyers, 701 F.2d 91, 92 (9th Cir.) cert denied sub nom., Rank v. Beltran, 462 U.S.
1134 (1983). The federal law requires states participating in the Medicaid program to cover
certain "essential" services for recipients, H.R. Rep. No. 213, 89th Cong., 1st Sess. 9 - 10, 70
(1965), including a disease and developmental disability prevention program for children under
age 21 known as the Early and Periodic Screening, Diagnostic and Treatment ("EPSDT')
program. 42 U.S.C. 1396a(a)(43), d(a)(4)(B), and d(r).
The EPSDT program requires, inter alia, mandatory medical screening of poor children
to diagnose their "physical or mental defects" as early as possible. 42 U.S.C. 1396d(a)(4)(B).
In 1989, Congress amended the EPSDT statute to specify that EPSDT screening services were
to include, at a minimum, "laboratory tests (including lead blood level assessment appropriate
for age and risk factors)." 42 U.S.C. 1396d(r)(l)(B)(iv). It is this latter phrase which the
federal defendant would have the court ignore.
The term "lead blood level," a scientific term, refers to the amount of lead in blood.
The federal defendant concedes that only a blood lead test "directly" measures lead blood
levels. USA Motion at 12, Hiscock deck at 11 9, Binder deck at 11 14.
Notwithstanding the plain language, federal defendant argues that the statutory
language does not require a blood lead test on two grounds. It first contends that Congress
did not intend to give such a "narrow, technical meaning" to the statutory term "lead blood
level." USA motion 29. Plaintiff-intervenors disagree. Had Congress not meant to bind the
agency to coverage of the lead blood test, it needed to mandate no requirement beyond
"laboratoiy testing," thus leaving federal and state authorities free to decide which type of tests
to cover. Congress, of course, specifically mandated a lead blood level assessment.
That Congress specifically mentioned lead blood laboratory testing in the Medicaid Act
is compelling in its own right. For the most part, Congress has chosen simply to list broad
categories of services (e.g., hospital services, physician services) rather than enumerate specific
C:\DOOTHOMPSON\PLEADING\AMICIMEM 9
procedures by name. Compare, 42 U.S.C. 1396d(r)(l)(B)(iv) with, 42 U.S.C. 1396d(a). When
it included a statutorily-required laboratory test in an otherwise generally drawn Medicaid
statute, Congress surely chose its terms carefully and deliberately.
Federal defendant also argues that the EP test is an "indirect" assessment of lead blood
level. USA motion 12. Again, plaintiff-intervenors disagree. Notably federal defendant,
however, fails to inform the Court that shortly before drafting §1396d(r)(l)(B)(iv), the House
Committee on Energy and Commerce was informed by HHS in its 1988 Report to Congress
that "reliance on EP level for initial screening can result in a significant incidence of false
negatives and failure to detect toxic Pb-B levels", and received the recommendation that the
EP test should be replaced by the blood lead test. Report to Congress 11-9.
With the lowering by the CDC of the toxicity level to 10 /xg/dL, the EP test is even
more unreliable.
Since erythrocyte protoporphyrin (EP) is not sensitive enough to identity more
than a small percentage of children with blood lead levels between 10 and 25
/xg/dL and misses many children with blood lead levels > 25 /xg/dL . . .
measurement of blood lead levels should replace the EP test as the primary
screening method.
CDC Statement 41; see also 2 ("Because the erythrocyte protoporphyrin level is not sensitive
enough to identity children with elevated blood lead levels below 25 jixg/dL, the screening test
of choice is now blood lead measurement.") Indeed, federal defendant’s expert, Dr. Binder,
is not only an author of the Report to Congress, with its admission that the significant number
of false negatives invalidates the EP test for screening, but an author as well of the very study
that the CDC cited in support of its assertion that the EP test is too insensitive to screen for
lead blood levels between 10 and 25 jxg/dL. See CDC Statement 41, 49, citing McElvaine,
M.D., Orbach, H.G., Binder, S., Blanksma, L.A., Maes, E.F. and Krieg, R.M., "Evaluation of
the Erythrocyte Protoporphyrin Test as a Screen for Elevated Blood Lead Levels," 119 J.
Pediatrics 548 (1991) (hereinafter "McElvaine, Orbach, Binder"), Exhibit A to Declaration of
Bill Lann Lee (hereinafter "Lee decl."). That study concluded that: "The sensitivity of the EP
test is . . . good for identifying children with vefy high Pb-B levels, those who most urgently
need follow-up. For identification of the children with Pb-B levels of 10 to 25 /xg/dL, another
screening method, probably Pb-B measurement, will be needed." McElvaine, Orbach, Binder
C:\DOC\THOMPSON\PLEADING\AMICIMEM 10
at 550. In fact, the EP test overall will only identity one out of seven or eight children with
lead poisoning at the levels the CDC now considers toxic. Rosen decl. at U 22.2
Neither the oral questions nor the EP test, alone or in combination, is a substitute for
the blood lead test. Had Congress intended to permit the use of the EP test, it could easily
have done so by substituting "erythrocyte protoporphyrin level" for the statutory phrase "blood
lead level" in § 1396d(r) or adopting HHS’ contemporaneous Medicaid guidance which
expressly identified the (EP) test as "the primary screening test." See Hiscock decl. at H 9.
Congress, however, did neither. Instead, it opted for a laboratory test to assess lead blood
level. See, e.g., Chandler v. Roudebush, 425 U.S. 840, 848 (1976) ("‘The plain, obvious and
rational meaning of a statute is always to be preferred to any curious, narrow, hidden sense
that nothing but the exigency of a hard case and the ingenuity and study of an acute and
powerful intellect would discover.’").
B. Legislative History Confirms that Congress Intended to Mandate A
Blood Lead Test to Screen For Lead Poisoning.
Legislative history analysis is unnecessary where, as here, the terms of the statute are
clear and unambiguous. Casey, 113 L.Ed.2d at 83; Patterson, 456 U.S. at 68. The available
legislative history, however, merely confirms the statute’s plain meaning.
Section 1396d(r)(l)(B)(iv) was added to the EPSDT statute by the Energy and
Commerce and Ways and Means Committees. Report of the House Budget Comm, on H.R
3299 101 Cong. 1st Sess., (Sept. 20, 1989), reprinted in Medicare and Medicaid Guide (CCH),
Extra Edition No. 596 (Oct. 5, 1989) (Explanation of the Energy and Commerce of Ways and
Means Committees Affecting Medicare-Medicaid Programs) (hereinafter "House Report"),
Exhibit B to Lee decl. Noting that "[t]he EPSDT benefit is not currently defined in statute"
the House Report explained that the Committee bill amended the statute to specify that
"screening services, at a minimum, include . . . laboratory tests (including lead blood level
2Dr. Binder’s study found that, at 10 /xg/dL, the EP test identified more children with
elevated lead blood level, 26%, but failed to identify fully 74% of the poisoned children.
McElvaine at 549 (table II). The study noted, however, that the population studied may
have exhibited iron deficiency, which is also detected by the EP test, resulting in possibly
skewed results. Id. at 549 - 50.
C:\DOC\THOMPSON\PLEADING\AMICIMEM 11
assessment appropriate for age and risk factors)." House Report at 399.
The obvious reason for the amendment was the July 1988 Report to Congress in which
HHS specifically recommended to the House Energy and Commerce Committee that the EP
test, which HHS permitted State Medicaid authorities to use for screening under the EPSDT
program, should be abandoned as a screening test for lead poisoning because it failed to detect
toxic lead blood levels. See Report to Congress II-9.
The House Committee bill was accepted unchanged by the Conference Committee, and
the Conference Report adds little to the legislative history. It briefly explained that the package
of EPSDT amendments "[cjodifies the current regulations on minimum components of EPSDT
screening . . . , with minor changes. Provides that screenings must include blood testing when
appropriate, as well as health education." Conference Report on HR 101-386, 101 Cong. 1st
Sess. 53 (1989). The report’s characterization of the "lead blood level assessment" provision
as a minor change is understandable because one laboratory test was merely being substituted
for another. While the Conference Report refers generically to "blood testing," the reference
appears to be a short-hand contraction used in the course of contrasting testing with the public
education component of screening rather than a studied gloss on the meaning of the statutory
term or a covert attempt to render superfluous the statutory terms "lead level."
C. The Agency Construction of the Statute Is Entitled to No Deference.
An agency construction of a statute that conflicts with the plain language and legislative
history of a statute is entitled to no deference. Fort Stewart Schools v. Federal Labor Relations
Authority, 495 U.S. 641, 645 (1990).
If, upon examination of "the particular statutory language at issue, as
well as the language and design of the statute as a whole," KMart Corp. v.
Cartier, Inc., 486 U.S. 281, 291 (1988), it is clear that the [agency] interpretation
is incorrect, then we need look no further, "for the court, as well as the agency,
must give effect to the unambiguously stated intent of Congress." Chevron
[U.S.A., Inc. v. Natural Resources Defense Council, Inc., 467 U.S. 837,] 842-43
[(1984).] If, on the other hand, "the statute is silent or ambiguous" on the point
at issue, we must decide "whether the agency’s answer is based on a permissible
construction of the statute." Ibid.
See also, Fleetwood Enterprises v. HUD, 818 F.2d 1188, 1193 (5th Cir. 1987).
C:\DOC\THOMPSON\PLEADING\AMICIMEM 12
In the instant case, no deference is due to the agency’s interpretation of the statute
because Congress spoke clearly and unambiguously about the meaning of §1396d(r)(l)(B)(iv).
See supra. Moreover, the present position of HHS that the terms "lead blood level assessment"
permit use of the EP test conflicts with its prior statements. See EEOC v. Arabian American
Oil Co., 113 L.Ed.2d 274, 287-88 (1991); General Electric Co. v. Gilbert, 429 U.S. 125, 141
(1976) (level of deference depends upon consistency with earlier pronouncements as well as
thoroughness of consideration and validity of reasoning). The 1988 Report to Congress stated
that the EP test should be abandoned because it produced many false negatives and failed to
detect toxic lead blood levels. The Strategic Plan declared that when the lead blood toxicity
level was lowered, as it was later in 1991, "blood lead measurements must be used for
childhood lead screening instead of EP measurements." Strategic Plan 23. In addition, the
CDC Statement termed the blood lead test the "screening test of choice" for the detection of
lead poisoning. CDC Statement 2.
Deference, in any event, would be anomalous because the statute was designed to
correct the very practice, use of the EP test, that HHS’ erroneous construction would
reimpose.
Federal defendant also argues at some length that HHS has a longstanding
commitment toward identifying and paying for the cost of treating lead poisoned Medicaid
eligible children, USA motion 9. The record of HHS speaks for itself. Congress enacted
§1396d(r)(l)(B)(iv) to change an HHS practice because the agency resisted acting upon the
recommendation of its own 1988 Report to Congress that the EP test should not be used. What
HHS seeks in this case is to continue using a test that even its own expert has found produces
so many false negatives that it fails to identify most children with toxic Pb-B levels.
While it is true that HHS historically has revised its EPSDT agency guidance following
CDC changes, USA motion at 10-11, the agency has by no means hastened to do so. HHS
waited three years before lowering the lead toxicity level for poor, at-risk children in response
to the 1985 CDC Statement. Id. And then, HHS lowered the toxicity level for Medicaid
eligible, at-risk children to 30 /xg/dL although the CDC had lowered it significantly for all
children to 25 /xg/dL.
C:\DOC\THOMPSON\PLEADING\AMICIMEM 13
The failure of HHS to comply with §1396d(r)(l)(B)(iv), unfortunately, is not
unprecedented. As the director of HHS Medicaid Bureau admitted in responding to the
protests of plaintiff-intervenors’ counsel; "in the past neither Medicaid’s EPSDT program nor
any other program have been successful in screening for lead poisoning a sufficient proportion
of children." Letter of Christine Nye to Julius L. Chambers, dated August 10, 1992,
Attachment B to the proposed Complaint in Intervention.
D. The Remedial Purpose of the EPSDT Statute and the CDC Report Mandate that Blood
Lead Testing Be Required.
1. The Remedial Purpose of the EPSDT Statute Requires Blood Lead Testing.
Congress enacted the underlying EPSDT statute with the remedial intent of "discovering], as
early as possible, the ills that handicap our children." President Lyndon B. Johnson, Welfare
of Children, H.R.Doc. No.54, 90th Cong., 1st Sess.7 (1967). In 1989, the House Committee
explained that §1396d(r)(l)(B)(iv) was necessitated by the fact that "[t]he EPSDT benefit is,
in effect, the nation’s largest preventive health program for children" and would become "even
more important to the health status of children in this county" "as Medicaid coverage of poor
children expands." House Report 398. The remedial nature of the EPSDT program is highly
significant in the context of lead poisoning. "Lead poisoning, the most common and societally
devastating environmental disease of young children, is entirely preventable." Strategic Plan
xiv.
Using a blood lead test would plainly advance the remedial objective of the EPSDT
program by improving preventive health care for the nation’s poor children. It will also
advance the specific remedial purpose of §1396d(r)(iv) to reform HHS’s practice of using an
ineffective test to screen those most at risk for lead poisoning. The EP test will do neither.
2. The CDC Statement Supports Immediate Blood Lead Testing of Medicaid Eligible
Children.
Federal defendant also erroneously argues that the testing scheme in the September
1992 State Medicaid Manual fully complies with the 1991 CDC Statement. On the one hand,
reliance upon the 1991 CDC Statement is misplaced: It is Congress’ 1989 mandate to the
Medicaid agency in 42 U.S.C. 1396d(r)(l)(B)(iv) that is at issue in this case, not a CDC
C:\DOC\THOMPSON\PLEADING\AMICIMEM 14
Statement which was adopted two years later. On the other hand, the CDC Statement is a
ringing endorsement of Congress’ 1989 action and is binding as the authoritative expression
of the testing protocol deemed "appropriate for age and risk." Thus, the CDC Statement’s
declaration that all children between the ages of 6 and 72 months should be screened at least
twice using a blood lead test at age 6 - 12 months and 18 - 24 months, CDC Statement at 43,
is dispositive as to the "appropriate" testing schedule for very young children under the statute.
The CDC Statement is also binding because it embodies current medical standards of
pediatric practice. Dr. John Rosen, the Chairperson of the CDC’s Childhood Lead Poisoning
Prevention Advisory Committee, which produced the CDC Statement, states in the attached
declaration that "[t]he Statement was prepared with primary medical care providers foremost
in mind, so they could glean the current, essential standards of pediatric practice in a readily
digestible form." Rosen decl. at 11 24.
For a pediatrician pursuing a diagnosis, the only responsible course of
action is to carry out a test that provides safe and definitive results for all
children, according to current standards of pediatric practice. A blood lead test
provides definitive information concerning to what extent a child has been
recently exposed to lead. An EP test provides, at best, marginal information
only for the one child out of seven or eight indicating that a child may be lead
poisoned. For a pediatrician pursuing a conclusive diagnosis, to perform such
an unreliable test for lead poisoning is irresponsible pediatric practice.
Id. at H 23; see also U 36. Dr. Rosen’s co-chair, Dr. J. Routt Reigart, who is also Chairman
of the American Academy of Pediatrics’ Committee on Environmental Health, concurs.
Reigart decl. at 11 9 ("Although the American Academy of Pediatrics’ revised report is not yet
completed, one recommendation that will certainly come from the Committee is that there is
a need for more testing. Lead poisoning cannot be detected absent a blood test; a series of
questions cannot verify blood lead levels.").
The CDC Statement testing requirements also embody current public health standards.
See Mushak decl. at 1111 20 - 31.
Inappropriateness o f Questioning and EP Testing for Screening. Federal defendant
erroneously contends that the scheme of verbal assessment questioning to establish "low" and
"high" risk and EP testing of "low" risk children complies with the CDC Statement. According
to Dr. Rosen,
C:\DOC\THOMPSON\PLEADING\AMICI MEM 15
[A]s Chairperson of CDC’s Advisory Committee, I can state that it was
not our intent to suggest to Medicaid providers that the use of a questionnaire
should determine whether children, particularly in the most vulnerable age
group of 6 - 36 months, should receive a blood lead test. The CDC Statement
is unequivocal that for this population, a blood lead test must be conducted at
least once by the time a child reaches 12 months and again by 24 months of
age, even if the responses to the assessment questions indicate the child is at
"low risk" of lead poisoning. CDC Statement 43. The CDC screening schedule
is based on the fact that children’s blood lead levels increase most rapidly at 6 -
12 months and peak at 18 - 24 months. Id. at 42. The incidence of high blood
lead levels among this population is so high, it makes little sense to try to
ascertain with a questionnaire who within this group is at "high risk." See id. at
Figure 6 - 1. The CDC Statement explicitly states that for this group the
questionnaire is not a substitute for a blood lead test. Id. at 42.
Rosen deck at H 35, see also U 36; see Reigart deck at 11 9
According to the CDC Statement, all children between 6 and 72 months are at risk from
lead poisoning, CDC Statement 42. The limited purpose of a high or low risk categorization
in the CDC Statement is to establish the schedule for follow-up screening and intervention,
id. at 43-45, not to trigger a system of triage for initial screening. Following up an initial EP
test with a blood lead test if the EP test score is high does not cure the inability of the initial
EP test to detect lead poisoning.3
Indefinite Transition Period. Driven by concerns for administrative convenience and cost
savings, federal defendant has focused upon that portion of the CDC Statement that recognizes
the need for a transition to universally mandated use of blood lead testing. It uses this
language to support its contention that limited laboratory capacity for processing blood lead
tests in some states justifies permitting any state Medicaid program to continue to use EP tests
for "low" risk cases during a transition period of undefined length. USA motion at 19.
Federal defendant provides no substantiation of any lack of laboratory capacity or its
3The CDC Statement does contain language about elevated EP results being followed
with a blood lead test to determine if lead poisoning is responsible for the elevation. CDC
Statement 48. However, the elevated EP results to which the CDC Statement referred are
those at or above 35 /xg/dL, i.e.., levels at which the EP test is sensitive, not at lead blood
levels of 10-25 fig/dL for which "the EP test is not a sensitive test." Id. The limited
purpose of the follow-up blood lead test dictated by the CDC is to determine if the
elevated EP result is caused by lead poisoning or some other health condition, such as iron
deficiency. Id. It is not to detect where there is a false negative EP result, the essential
defect of the EP test. See Mushak deck at 11 25 ("[T]he EP test does not act as a
preventive test which allows the health care provider to detect lead poisoning at its early
more manageable stages. Rather, the EP test can only accurately predict that unacceptably
high lead exposure and greater risk of more severe poisoning have already occurred").
C:\DOC\THOMPSON\PLEADING\AMICIMEM 16
extent. Dr. Rosen, in any event, establishes that the purported lack of laboratory capacity is
a mere pretext.
I cannot fathom why, more than a year after the CDC Statement
dictated blood lead tests as the reasonable standard of medical practice, a
state’s medical care providers’ capacity of performing the tests, particularly if
reimbursable under the Medicaid program, would be limited.
The laboratory capacity certainly exists among the large commercial
laboratories, such as Roche, MetPath, or Smith Kline. Similar capacity must
exist at State and local public laboratories. The large commercial laboratories
are located around the country and routinely assess blood samples of Medicaid
patients in-state or out-of-state. These laboratories can process the blood lead
results of any children in the Medicaid program and be reimbursed by the
Medicaid program. See Declaration of William Hiscock 1111 15, 18.
CDC’s 1991 Statement did allow a "grace period" for transition from EP
to blood lead testing. As Chairperson of CDC’s Advisory Committee, I can
state that our intent was to provide a transition of up to a year for state and
local agencies to order proper equipment and implement blood lead
measurements as the diagnostic test for childhood lead poisoning. One year is
more than twice the time required to mount such a laboratory capability de
novo, including the time required to order an instrument, train a technician, and
set up a reporting system. The transition period was not intended to be a
bureaucratic vacation to extend until the next CDC Statement is issued. The
next CDC Statement, like the last, may not be issued for another six years or
more.
Although HCFA’s policy to reimburse any blood lead tests that are
performed eliminates cost as a factor, blood lead testing is not expensive
anyway.4 Throughout the Montefiore Medical Center-Albert Einstein College
of Medicine complex, including all their satellite clinics, we have established
that the total cost per blood lead test does not exceed $12 - 13. Colleagues’
findings in Pennsylvania, West Virginia, and North Carolina confirm these
results. One need only check the rates from the commercial mass laboratories
to find their charges in the same range.
4Of course, concern about cost savings is clearly a motivating factor here. The EP test
costs Medicaid less than $10, while a blood lead test costs between $10 - $15, depending on
volume and economies of scale. Mushak deck at 11 28. So long as the EP test is used, the
federal defendant saves on its laboratory testing expenditures - particularly in light of the
fact that providers are already using the EP test to detect other childhood conditions, such
as iron deficiency. Such cost concerns do not, however, provide adequate justification for
the continued use of the EP test for lead poisoning in young Medicaid eligible children.
Because of its unreliability for accurately predicting elevated Pb-B below 40 ;u.g/dL level,
the EP test is probably a waste of money for lead absorption prediction. Id. And, as
noted in the 1988 Report to Congress, direct lead blood level assessment is particularly cost -
effective in the long run. This was demonstrated by comparing data on the costs of
treating children who are poisoned because early lower levels of lead intoxication were not
detected by screening with the costs of testing. In the example used in the Report, the ratio
of medical costs to child screening costs was an astounding 50:1 in 1986 dollars (about
$20,000 to $25,000 per child in 1992 health care dollars). Id. at 29, 31.
C:\DOC\THOMPSON\PLEADING\AMICIMEM 17
Rosen decl. at 1111 25-27, 29; Mushak deck at 11 28.5 Dr. Mushak, an author of the Report to
Congress comes to the same conclusion from a public health perspective. Mushak decl. at 11
20 ("Delaying blood lead testing of Medicaid eligible children is . . . not justified by concerns
regarding laboratory capacity.").
The CDC called for a transition to blood lead testing over a year ago. Over three years
have passed since Congress mandated lead blood level testing as part of the EPSDT screen.
HHS’s current policy for lead screening is unacceptable and is, in fact, premised upon an
acknowledgement that what it is doing is wrong. In the September 1992 State Medicaid
Manual, HHS allows that the EP test is now an "inappropriate" test to detect lead poisoning.
It recognizes that lead blood levels cannot be assessed by asking questions. And, it states that
a lead blood test is the test of choice when measuring blood lead levels. Yet, it uses
statements contained in the later-adopted CDC Statement to excuse a testing scheme for the
poor that delays indefinitely implementation of the Congressional mandate for blood lead
testing. As established by the experts, the question of the appropriate test for lead exposure
and lead poisoning in Medicaid children is not arguable on cost or other logistical grounds
involving laboratory capacity, see Rosen decl. at 1111 25 - 29; Mushak decl. at U1I 29 - 31; Reigart
decl. at U 13. Such arguments do not justify the federal defendant’s failure to require reliable
lead blood level testing of the very group that all participants in this case agree is most at risk
of and tragically damaged by lead poisoning. The federal defendant has failed to meet its
burden of showing why further delay — now in the form of an indefinite transition period —
should be allowed.
////
5Even if these nationwide resources were somehow not available in a
particular area, it is not overly difficult or costly to develop independent
laboratory capacity, as we did years ago at Montefiore Medical Center. The
laboratory can be staffed with a laboratory technician and a clerk-typist with
a computer. The required instrumentation currently runs approximately
$60,000 - 75,000, plus $10,000 in consumables per year. This country
certainly has the technology to perform universal blood lead tests for all
Medicaid eligible children.
Rosen decl. at 11 30.
C:\DOQTHOMPSON\PLEADING\AMICIMEM 18
Conclusion
For the above reasons, amici proposed plaintiff-intervenors request that the Court deny
federal defendant’s alternative motions to dismiss and for summary judgment.
Dated: November 23, 1992
Respectfully submitted,
Edward B. Cloutman, III
Texas Bar No. 04411000
Law Office of Edward B. Cloutman, III
3301 Elm Street
Dallas, TX 75226
(214) 939-9222
B y________________________________
Edward B. Cloutman, III
Julius L. Chambers
Alice Brown
NAACP Legal Defense & Educational
Fund, Inc.
99 Hudson Street, Suite 1600
New York, NY 10013
(212) 219-1900
Bill Lann Lee
Kirsten D. Levingston
NAACP Legal Defense & Educational
Fund, Inc.
315 West Ninth Street, Suite 208
Los Angeles, CA 90015
(213) 624-2405
By____________
Bill Lann Lee
Jane Perkins
National Health Law Program
313 Ironwoods Drive
Chapel Hill, NC 25716
(202) 887-5310
B y ________________________
Jane Perkins
Carlene NcMulty
North State Legal Services
114 West Corbin Street
Hillsborough, N.C. 27278
(919) 732-8137
C:\DOQTHOMPSON\PLEADING\AMICIMEM 19
Lucy Billings
Marie-Elena Ruffo
Bronx Legal Services
579 Courtlandt Avenue
(212) 993-6250
By___________________________
Lucy Billings
Attorneys for Amici
People United for a Better Oakland, et al
C:\DOC\THOMPSON\PLEADING\AMICIMEM 20
DECLARATION OF BILL LANN LEE
I, BILL LANN LEE, declare and say:
1. I am one of the counsel for the amici curiae and the proposed plaintiff-
intervenors People United for a Better Oakland, et al.
2. Attached hereto as Exhibit A is a true and accurate copy of McElvaine, M.D.,
Orbach, H.G., Binder, S., Blanksma, L.A., Maes, E.F., & Krieg, R.M., Evaluation of the
Erythrocyte Protoporphyrin Test as a Screen for Elevated Blood Lead Levels, 119 J. of
Pediatrics 548 (1991).
3. Attached hereto as Exhibit B is a true and accurate copy of Report of the
House Budget Comm, on H.R. 3299, 101 Cong., 1st Sess. (September 20, 1989), reprinted in
Medicare and Medicaid Guide (CCH), Extra Edition No. 596 (October 5, 1989) ( pp. 398 - 410.
I declare under penalty of perjury that the foregoing is true and correct.
Executed the 23rd day of November, 1992, at Los Angeles, California.
Bill Lann Lee
C:\DOC\THOMPSON\PLEADING\AMICIMEM