Notice of Filing of Corrected Exhibits to Amend Hiscock Declaration
Public Court Documents
December 7, 1992
10 pages
Cite this item
-
Case Files, Thompson v. Raiford Hardbacks. Notice of Filing of Corrected Exhibits to Amend Hiscock Declaration, 1992. 02ed1e79-5c40-f011-b4cb-002248226c06. LDF Archives, Thurgood Marshall Institute. https://ldfrecollection.org/archives/archives-search/archives-item/57035d31-d404-45e8-b444-ecc4d36007d3/notice-of-filing-of-corrected-exhibits-to-amend-hiscock-declaration. Accessed February 12, 2026.
Copied!
Nt Aull Bog 6
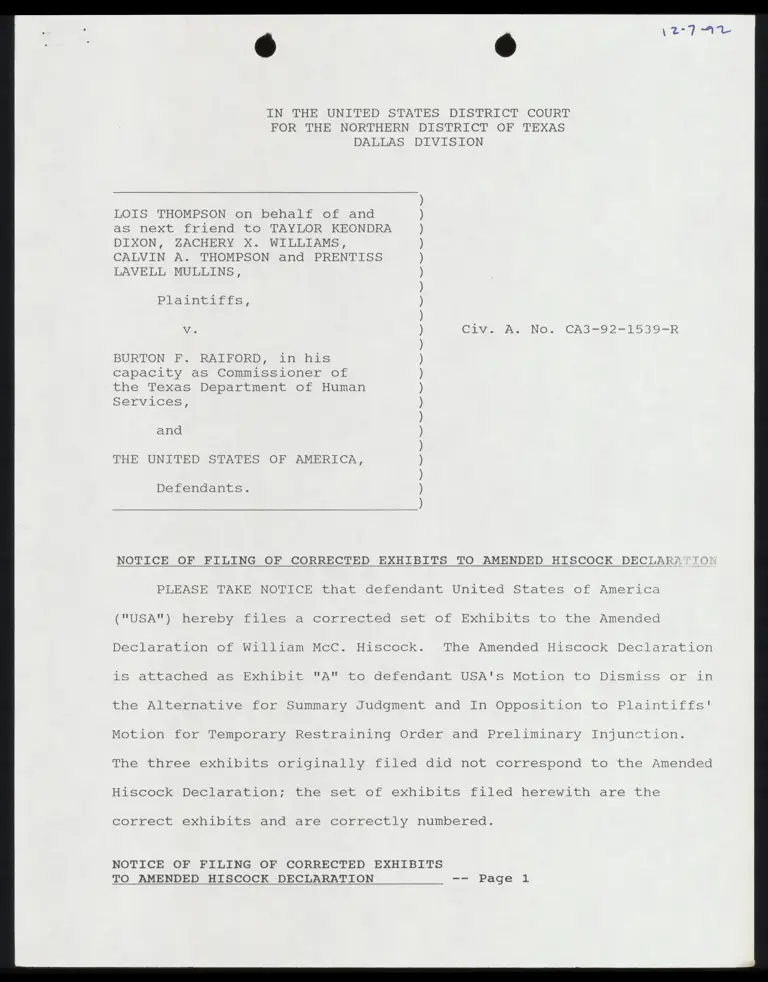
IN THE UNITED STATES DISTRICT COURT
FOR THE NORTHERN DISTRICT OF TEXAS
DALLAS DIVISION
LOIS THOMPSON on behalf of and
as next friend to TAYLOR KEONDRA
DIXON, ZACHERY X. WILLIAMS,
CALVIN A. THOMPSON and PRENTISS
LAVELL MULLINS,
Plaintiffs,
Vv. Civ. A. No. CA3-92-1539-R
BURTON PF. RAIFORD, in his
capacity as Commissioner of
the Texas Department of Human
Services,
and
THE UNITED STATES OF AMERICA,
Defendants.
N
a
r
?
M
e
?
N
e
?
N
e
”
S
a
”
S
e
”
S
a
N
a
S
a
S
a
S
a
S
a
”
S
a
S
a
S
a
S
a
S
e
”
S
a
S
a
S
a
”
S
a
S
N
NOTICE OF FILING OF CORRECTED EXHIBITS TO AMENDED HISCOCK DECLARZ
PLEASE TAKE NOTICE that defendant United States of America
("USA") hereby files a corrected set of Exhibits to the Amended
Declaration of William McC. Hiscock. The Amended Hiscock Declaration
is attached as Exhibit "A" to defendant USA's Motion to Dismiss or in
the Alternative for Summary Judgment and In Opposition to Plaintiffs’
Motion for Temporary Restraining Order and Preliminary Injunction.
The three exhibits originally filed did not correspond to the Amended
Hiscock Declaration; the set of exhibits filed herewith are the
correct exhibits and are correctly numbered.
NOTICE OF FILING OF CORRECTED EXHIBITS
TO AMENDED HISCOCK DECLARATION ww Page 1
Dated: December 7, 1992
OF COUNSEL:
HENRY R. GOLDBERG, Deputy Chief
Counsel for Litigation
DAVID V. "PEERY, Altorney
Office of the General Counsel
Department of Health and
Human Services
Room 500, East Highrise Building
6325 Security Boulevard
Baltimore, MD 21207
(410) 965-8871
(410) 966-5187 (Fax #)
Respectfully submitted,
STUART M. GERSON
Assistant Attorney General
MARVIN COLLINS
United States Attorney
MARY ANN MOORE
Assistant United States
Texas Bar No. 14360400
ide
SHEILA LIEBER /
Attorney
Gotima. nt! BJ,
ALINA S. KOFSKY
Lire
ZZ 7
AO
STEVEN H. HARTMANN gil
Attorneys, Department of
Federal Programs Branch, Civil
Division
901 FE Street, N.W., Room 1010
Washington, D.C. 20530
(202) 514-4527
(202) 616-8470
Tot 1 (
(Fax #)
ATTORNEYS FOR DEFENDANT
UNITED STATES OF AMERICA
NOTICE OF FILING OF CORRECTED EXHIBITS
TO AMENDED HISCOCK DECLARATION -- Page 2
CERTIFICATE OF SERVICE
I hereby certify that on this 7th day of December, 1992, a copy
of Defendant United States of America's Notice of Filing of Corrected
Exhibits to Amended Hiscock Declaration was served on the following
individuals listed below, via overnight mail:
Laura B. Beshara Bill Lann Lee
Michael M. Daniel Kirsten D. Levingston
MICHAEL M. DANIEL, P.C. NAACP Legal Defense & Educational
3301 Elm Street Fund, Inc.
Dallas, Texas. 75226-1637 315 West Ninth Street, Suite 308
Los Angeles, California 90015
Edwin N. Horne
Assistant Attorney General
Office of the Attorney General
State of Texas
P.O. BOX 12548
Capitel Station
Austin, Texas 78711-2548
STEVEN H. HARTMANK
NOTICE OF FILING OF CORRECTED EXHIBITS
TO AMENDED HISCOCK DECLARATION -= "Page 4
A
r
y
Wo.
1
N
e
-~
a
PA
NT
T
F
GE
ER
T
Y
T
W
E
T
I
E
T
N
\
A
r
e
t
a
V
O
¢
G
U
I
D
w
a
n
e
G
E
E
R
,
©
D
E
N
v
DEPARTMENT OF HEALTH, EDUCATION, AND WELFARE
HEALTH CARE FINANCING ADMINISTRATION
WASHINGTON, D. C. 20201
PROGRAM INSTRUCTION
ACTION TRANSMITTAL
HCFA-AT-78-59 (MMB)
July 7, 1978
TO: STATE AGENCIES ADMINISTERING MEDICAL ASSiSTANCE
PROGRAMS
SUBJECT: Screening, Detection, and Treatment of Undue
Lead Absorption and Federal Financial Partici-
pation (FFP) for the Treatment of Undue Lead
Absorption.
ACTION RECOMMENDED: Implement recommendations made by the Center
for Disease Control for the detection of undue
lead absorption in the EPSDT-eligible popula-
tion. ;
BACKGROUND: The Center for Disease Control, Environmental
Health Services Division, recently released a
publication which describes current recommenda-
tions for screening children for undue lead
absorption. This requires a modification in
methods previously recommended in "A Guide to
Administration, Diagnosis, and Treatment for
the Early and Periodic Screening, Diagnosis
and Treatment (EPSDT) Program under Medicaid",
and IM-77-32, ''"New Technology Available in the
Screening and Detection of Lead Poisoning and
EPSDT', transmitted June 9, 1977.
ATTACHMENTS : (1) Discussion and recommendations.
(2) Federal Financial Participation.
(3) Preventing Lead Poisoning in Young Chil-
dren, Center for Disease Control,
April 1978.
EFFECTIVE: On issuance.
INQUIRIES TO: Regional Medicaid Directors.
ea :
Corrected Exhibit 1 to Director,
Amended Hiscock Declaration Medicaid Bureau
j 3 coe Sait a 2 Tr tr A I La a
ST a me ee men CE TIEN arn X FETA IIE IEC + ma pm p STR nite LTE EE | Em AS | rg 1 TOT IT ROAM EY SRA GER PI RUSS A Co Rls A RE Sh
s /
Discussion
This Action Transmittal was developed by the Office of Child Health
(OCH) and the Environmental Health Services Division of the Center for
Disease Control (CDC) to implement current technology for the detection
of undue lead absorption in the EPSDT population.
Problem
All children are at risk for undue lead absorption, since all indivi-
duals are exposed to lead daily. Large scale screening studies of chil-
dren without symptoms have demonstrated that the number with undue lead
absorption is greater than previously thought. While once considered a
problem only in the inner cities of the Northeast, data from both urban
and rural areas indicate that from 3 to 20% of children tested have undue
lead absorption. The magnitude of the problem is greater and the con-
sequences more severe than previously thought.
Excessive lead exposure has serious and largely irreversible effects
on the central nervous system (CNS). These CNS effects vary from severe
brain damage to altered neuropsychologic behavior of considerable conse-
quence which may be recognized by parents, teachers, and clinicians as
attentional disorders, learning disabilities, or emotional disturbances
which impair progress in school. Undue lead absorption also affects the
bone marrow, impairing the formation of blood cells. Kidney damage can
also occur. It should be noted that minor symptomology (e.g., malaise,
anorexia, irritability) may often be attributed to some other cause or
there may even be no overt symptoms. Only a laboratory analysis will
determine whether the child has undue lead absorption.
Risk
Increased long-term institutional care and increased welfare cost
can result from undetected childhood lead absorption. All children are
at risk from this environmental contaminant; however, children who live in,
or frequently visit, poorly maintained housing units constructed prior to
the 1960's are at particularly high risk.
Background
Screening for undue lead absorption is recommended in "A Guide to
Administration, Diagnosis, and Treatment for the Early and Periodic
Screening, Diagnosis, and Treatment (EPSDT) Program under Medicaid".
Since its publication there have been considerable advances in techno-
logy and information relating to undue lead absorption.
In the past, screening for this disease was expensive, time-consuming,
and required extraordinary care in the collection and handling of sam-
ples. In April 1978, the Center for Disease Control, Environmental
Health Services Division, released a statement (copy attached) entitled
"Preventing Lead Poisoning in Young Children'. The statement recommends
the use of the erythrocyte protoporphyrin (EP) test for screening.
Le — a We tetia Cetera m—. . ". es Ve a an ” — oan am — Pa arn. oj — — ————— ® —_— » -—— —— < et et Yt. © cn kA Dt
The CDC statement also discusses in detail the interpretation of test
results, and serves as a guide for providers in the management of
children with undue lead absorption.
Recommendations
Because the EP test is a simple, cost-effective tool for screening
all children for undue lead absorption, the Office of Child Health re
commends the immediate implementation of routine screening utilizing
i the EP for all children ages one through five years. An additional
% advantage of the EP test is its use to screen for iron deficiency as
well.
The specimens collected should be processed by a laboratory with
known technical competence in this analytic field. Assistance in
identifying these laboratories can be obtained from State Health De-
4 partments. Those childrea who exhibit abnormal EP levels (greater
than 49 micrograms/deciliter) require diagnostic evaluation for both
: undue lead absorption and iron deficiency (e.g., blood lead and hemo-
globin).
The identification of the sources of the lead affecting the child
is required as part of the treatment for all children with undue lead
" absorption. After these sources are identified, follow-through by
other agencies (health department or housing authority) for housing
rehabilitation or relocation of the family is essential. Appropriat
interagency agreements at the State and local level, where not exte:
should be developed (see HCFA-AT-78-2, January 13, 1978).
Federal Financial Participation (FFP)
The cost incurred for the epidemiological investigation which is
necessary to identify the source of lead contamination for an indi-
vidual who has been identified with undue lead absorption is reim-
bursable at the same FFP rate as that given for necessary medical diag-
nosis and treatment.
® | o
5-70-00 p. 15
Medical
Assistance |
Manual
Services and Payment in Medical Assistance Programs
-70-00 Early and Periodic Screening, Diagnosis, and Treatment of ¢
Eligible Individuals Under Age 21
-70-20 E. Screening (Continued)
f. Vision Testing. Administer a vision screening test appropriate
to the child's age. Consultation by ophthalmologists and
optometrists can be of help in determining the type of tests
to be used and the criteria for determining when a child should
‘be referred for diagnostic examination.
g. Hearing Testing. Administer a hearing screening test appropriate
to the child's age. Consultation on suitable tests for screening
and on methods of administering the tests should be obtained from i
audiologists or from State health or education departments.
h. Anemia Test, The most easily administered test for anemia is
a microhematocrit determination from venous blood or a finger- ;
stick, This should be done on all children or, if possible, ;
a hemoglob.in concentration which will give a more accurate
determination of anemia should be done.
i. Sickle Cell Test. Check all Negro children for sickle cell trait.
This may be done with a sickle cell preparation or a hemoglobin
solubility test. If a child has been properly tested once for
sickle cell disease, he does not have to be tested again.
j« Tuberculin Test. Give a tuberculin test to every child-who hag
not had one within one year.
k. Urine Screening. Carry out a rapid urine screening on all
children for the presence of sugar, albumin and bacteria.
1, Lead Poisoning Screening. It is not possible to identify which
children may have had undue exposure to lead-based paint and other
sources of lead poisoning, except by determination of blood- lead
levels, Therefore, all children between the ages of 1-6 should be
periodically screened for lead poisoning. Children 6 and over should
Corrected Exhibit 2 to MSA- PRG-21
Amended Hiscock Declaration 6-28-72
5-70-00
Pe 16
Medical
Assistance
Manual
i aE
Part Se. Services and Payment in Medical Assistance Programs
-70-00 Early and Periodic Screeni
Eligible Individuals
Under
5-70-20 E. Screening (Continued)
of thildhood
when medically indicated.
lead poisoning {s lead-based paint,
Diagnosis, and Treatment of
e 21
The principal gource
but pollution
of the environment from such things as burning lead batteries
and repeated exposure
into the goil and
lead poisoning.
of symp
:
of whole blood) cases
lead poisoning, such a
and involvement of the
capillary blood .sample
laboratory facilities.
Nutritiong- —————
carried out in the screening process will usually yield
{information
useful in a
ticular importance
circumference
and hemog
child having any
be referred to & nutritionist
or
consultation.
Immunization
Status.
tool in
gtatus, 8a ma jor
During the gcreening process,
whether he has
status; 1.€«»
pertussis, tetanus, pol
whether he ig in need of
the child's {mmunization record should be brought to the
|
center OT
to whom the child goes
are ingested
tomatic and asymptomatic
(over
are measurements
of height, weight,
detectable autritional
deficiencies
ghould
The screening
excellent opportunity to ascertain a child's
of lead that get
a child may also result in to fall-out
i
milliliters
serious sequelae of
mental retardation
Venous OT
can prevent the
g mental impairment,
central nervous
gs may be used,
and laboratory determinations
gsessing nutritional
status. Of pa?
head
lobin concentration
otf hematocrite
p
public health nurse for
program presents an
{smunigation
preventing disease and disability.
child's {mmunization
against diphtheria;
and mumps, and
io, measles,
:
¥hen it is available,
booster shots.
jmaunizatio
n
{mmunization
OT updating at the gcreening
through the facility or provider
MSA-PRG-21
6-28-72
DEPARTMENT OF HEALTH & HUMAN SERVICES Health Care Financing Administrat uor
6325 Security Boulevard
Baltimore, MD 21207
MEDICAID BUREAU
Dear State Medicaid Director:
The purpose of this letter is tO clarify certain aspects of the lead screening
requirements published in the September 1992 revision of the State Medicaid
Manual (SMM), Part 5, for the Early and Periodic Screening, Diagnostic, and
Treatment (EPSDT) program.
We consulted with the Centers for Disease Control (CDC) and other organizations
prior to revising our instructions, and we continue to consult with CDC about
developments in the capacity for screening and for performing blood lead tests.
We believe that our published guidelines are consistent with the CDC statement,
Preventing Lead Poisoning in Young Children (October, 1991).
Effective September 19, 1992, States are required to screen all Medicaid eligible
children between the ages of 6 months and 72 months of age at their next
scheduled EPSDT screening for lead poisoning. Screening consists of both a verbal
risk assessment and a blood lead level assessment. A child answering "yes" to ore
or more of the risk assessment questions is determined to be at high risk, and a
blood-lead test must be performed. A child answering "no" to all questions 1s
determined to be at low risk, and may receive either a blood-lead test or an
erythrocyte protoporphyrin (EP) test. We believe that most Medicaid eligible
children will be at high risk for lead poisoning.
We consider all children between the ages 6 through 72 months to be at risk for
elevated blood lead levels. In the vast majority of cases, HCFA expects Medicaid
eligible children will receive a blood lead test. Children who live in a community
officially declared "lead free" by a State or local health authority and answer "no" to
all risk assessment questions, do not need a blood lead level assessment. However,
such a child must still receive a verbal risk assessment at every periodic screen to
determine if any changes have occurred which would change the child’s risk status.
Although our SMM instructions are only the first phase in a transition period, and
take into account the currently available state of the art of lead screening
technology, I am aware that concerns have been raised over the continued use of
the EP test, even for children who are at low risk. Direct blood lead testing is the
preferred mode of ascertaining blood lead levels for all Medicaid eligible children,
and Federal financial participation is available for any Medicaid expenditures for
that purpose. While the EP test is not as sensitive as tests which directly measure
Corrected Exhibit 3 to
Amended Hiscock Declaration
¢ ®
Page 2 - State Medicaid Director
blood lead levels, it is easier and somewhat less expensive to perform than the
blood-lead test. In addition, the EP test will identify most children with blood lead
levels at or above 25 micrograms per deciliter, for whom medical interventions are
clearly indicated. We recognize, as does CDC, that not all communities currently
have the technology and laboratory capacity to perform blood-lead tests on all
children, while they do have the capability of performing the EP test. We do not
believe it appropriate to wait until a simpler and cheaper blood-lead test 1S
available, and permit many lead poisoned children to go undetected in the interim.
Thus, our instructions require initial blood lead testing for those children assessed
to be at high risk. The EP test is allowed only for low risk children, although the
blood lead test is preferred.
I am asking the HCFA regional office staff to help you implement the revised
policy, and to identify and work through any barriers you may encounter.
Acknowledging that States require time to develop the needed capacities, CDC is
currently pursuing research and development efforts to develop instrumentation and
protocols for simpler blood-lead tests. At this time, we cannot set a firm date for
the end of the transition period. As research and development efforts progress an:
capacity becomes available, we will be providing further guidance which will
culminate with the requirement for blood lead testing of all Medicaid eligible
children, whether at high or low risk.
I hope this letter clarifies our recent instructions on lead screening.
Sincerely yours,
Che
Christine Nye
4 Director
CC:
All Regional Administrators
All Associate Regional Administrators
Division of Medicaid