Exhibits in Support of Plaintiffs' Motion for Partial Summary Judgement (Redacted)
Working File
June 21, 1991
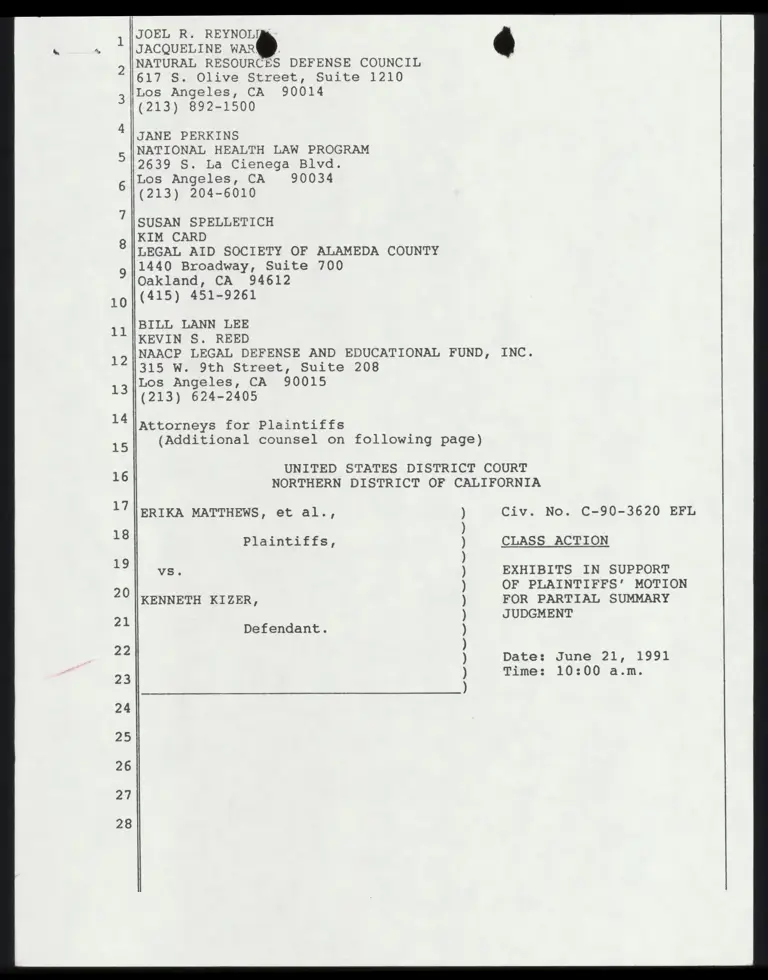
315 pages
Cite this item
-
Case Files, Matthews v. Kizer Hardbacks. Exhibits in Support of Plaintiffs' Motion for Partial Summary Judgement (Redacted), 1991. 06184496-fa4d-f011-8779-7c1e5267c7b6. LDF Archives, Thurgood Marshall Institute. https://ldfrecollection.org/archives/archives-search/archives-item/590b41da-a2a1-4b55-8f4c-153e2490652f/exhibits-in-support-of-plaintiffs-motion-for-partial-summary-judgement-redacted. Accessed February 21, 2026.
Copied!
27
28
JOEL R. REYNOLIL
JACQUELINE oe )
NATURAL RESOURCES DEFENSE COUNCIL
617 S. Olive Street, Suite 1210
Los Angeles, CA 90014
(213) 892-1500
JANE PERKINS
NATIONAL HEALTH LAW PROGRAM
2639 S. La Cienega Blvd.
Los Angeles, CA 90034
(213) 204-6010
SUSAN SPELLETICH
KIM CARD
LEGAL AID SOCIETY OF ALAMEDA COUNTY
1440 Broadway, Suite 700
Oakland, CA 94612
(415) 451-9261
BILL LANN LEE
KEVIN S. REED
NAACP LEGAL DEFENSE AND EDUCATIONAL FUND, INC.
315 W. 9th Street, Suite 208
Los Angeles, CA 90015
(213) 624-2405
Attorneys for Plaintiffs
(Additional counsel on following page)
UNITED STATES DISTRICT COURT
NORTHERN DISTRICT OF CALIFORNIA
ERIKA MATTHEWS, et al., Civ. No. C-90-3620 EFL
Plaintiffs, CLASS ACTION
vs. EXHIBITS IN SUPPORT
OF PLAINTIFFS’ MOTION
FOR PARTIAL SUMMARY
JUDGMENT
KENNETH KIZER,
Defendant.
Date: June 21, 1991
Time: 10:00 a.m.
V
a
t
”
Na
st
”
at
”
Nu
t?
N
a
”
a
t
”
u
l
?
“a
t?
“u
ni
“
v
u
?
“a
d?
“w
et
?
27
28
MARK D. ROSENBZgM
ACLU FOUNDATIO F SOUTHERN CALIFORNIA
633 South ShattC Place
Los Angeles, CA 90005
(213) 487-1720
EDWARD M. CHEN
ACLU FOUNDATION OF NORTHERN CALIFORNIA
1663 Mission Street, Suite 460
San Francisco, CA 94103
(415) 621-2493
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibits
Declaration of Dr. John F. Rosen
Declaration of Dr. Herbert L. Needleman
CHDP Provider Information Notice #91-6 from
Director Kenneth Kizer to CHDP Providers Re:
Lead Poisoning in Children (March 12, 1991)
S. Roan, "High Number of Lead Poison Cases
Found," L.A. Times, Aug. 30, 1990, A3, col.’1
DHS, Statewide: Fiscal Year 1989-90 Ethnicity
by Age Group by Funding Source by Lead Test
{Feb. 15, 1991)
DHS, Statewide: July 1990 thru January 1991
Ethnicity by Age Group by Funding Source by
Lead Test (Feb. 15, 1991)
DHS Medical Care Statistics Section,
California’s Medical Assistance Program
Annual Statistical Report Calendar Year 1989
Tables 20 and 29)
DHS, Fiscal Year 1989-90 Provider Number by
Age Group by Funding Source by Lead Test:
County of Residence = Santa Clara (Feb. 15,
1931)
DHS, Fiscal Year 1989-90 Ethnicity by Age
Group By Funding Source by Lead Test: County
of Residence = Los Angeles (Feb. 15, 1991)
Deposition of Ruth Range (excerpts)
Deposition of Dr. Maridee A. Gregory
(excerpts)
Health Care Coverage for Children: Hearing
Before the Senate Committee on Finance, 101st
Cong., lst Sess. 24 (statement of Kay A.
Johnson, Director, Children’s Defense Fund
Health Division) (June 20, 1989)
Report of the House Budget Committee on H.R.
3299 (Sept. 20, 1989) reprinted in Medicare &
Medicaid Guide (CCH), Extra Edition No. 596
(Oct. 5, 1989)
HCFA, State Medicaid Manual, § 5123.2(D)
(incorporating revisions contained in HCFA
transmittals of April and July 1990)
llExhibit 0 -- 9: Medical Assistance M@ghal, § 5-70-00 et
2 seq. (June 28, 1972)
3 Exhibit P -~- HCFA, State Medicaid Manual § 5122 (April
1988)
4 Exhibit Q -- HEW, A Guide to Screening-EPSDT Medicaid
5 (Chapter 21) (1974)
6 Exhibit R -- HEW, Information Memorandum, "New Technology
Available in the Screening and Detection of
. Lead Poisoning and EPSDT" (1M-77-32 (MSA))
(June 9, 1977), reprinted in Medicare &
8 Medicaid Guide (CCH) ¥ 28,505
9 Exhibit § =~ HEW, A Guide to Administration, Diagnosis and
Treatment for the EPSDT Program under
10 Medicaid (1977) (excerpts)
11 Exhibit T ~~ 135 Cong. Rec. S 13233 (October 12, 1989)
12 Exhibit U -- Explanation of the Conference Committee
Affecting Medicare - Medicaid Programs Re:
13 Omnibus Budget Reconciliation Act of 1989
(H.R. 3299), reprinted in Medicare & Medicaid
14 Guide (CCH), Extra Edition No. 603 (Dec. 15,
1989)
15 Exhibit V -- Letter from Charles A. Woffinden, Chief HHS
16 Medicaid Operations Branch to Michael Quinn,
CHDP Research Manager (April 11, 1991)
17 Exhibit W -- Letter from Charles A. Woffinden, Chief HHS
18 Medicaid Operations Branch, to Michael Quinn,
CHDP Research Manager (May 7, 1991)
19
20
21
22
23
24
25
26
27
28
2
27
28
é DECLARATION OF JANE PERIES
I, Jane Perkins, declare:
1. I am one of the attorneys of record for plaintiffs
in this case. The matters stated herein are true and correct,
and if called as a witness, I could competently testify thereto.
2. Attached hereto as Exhibit C is a true and correct
copy of a document entitled "CHDP Provider Information Notice
#91-6 from Director Kenneth Kizer to CHDP Providers Re: Lead
Poisoning in Children (March 12, 1991)."
3. Attached hereto as Exhibit E is a true and correct
copy of a document entitled "DHS, Statewide: Fiscal Year 1989-
90 Ethnicity by Age Group by Funding Source by Lead Test (Feb.
15, .19%91)."
4. Attached hereto as Exhibit F is a true and correct
copy of a document entitled "DHS, Statewide: July 1990 thru
January 1091 Ethnicity by Age Group by Funding Source by Lead
Test (Feb. 15, 1991)."
5. Attached hereto as Exhibit G is a true and correct
copy of a document entitled "DHS Medical Care Statistics
Section, California’s Medical Assistance Program Annual
Statistical Report Calendar Year 1989."
6. Attached hereto as Exhibit H is a true and correct
copy of a document entitled "DHS, Fiscal Year 1989-90 Provider
Number by Age Group by Funding Source by Lead Tests: County of
Residence = Santa Clara (Feb. 15, 1991)."
7. Attached hereto as Exhibit I is a true and correct
copy of a document entitled "DHS, Fiscal Year 1989-90 Ethnicity
by Age Seev dl Funding Source by ge ah County of
Residence = Los Angeles (Feb. 15, 1991)."
8. Attached hereto as Exhibit L is a true and correct
copy of a document entitled "Health Care Coverage for Children:
Hearing Before the Senate Committee on Finance, 10lst Cong., lst
Sess. (statement of Kay A. Johnson, Director, Children’s Defense
Fund Health Division) (June 20, 1989)."
9. Attached hereto as Exhibit M is a true and correct
copy of a document entitled "Report of the House Budget
Committee on H.R. 3299 (Sept. 20, 1989), reprinted in Medicare
& Medicaid Guide (CCH), Extra Edition No. 596 (Oct. 5, 1989)."
10. Attached hereto as Exhibit N is a true and
correct copy of a document entitled "HCFA, State Medicaid
Manual, § 5123.2(D) (April and July 1990)."
11. Attached hereto as Exhibit O is a true and
correct copy of a document entitled "HEW, Medical Assistance
Manual, § 5-70-00 (June 29, 1972)."
12. Attached hereto as Exhibit P is a true and
correct copy of a document entitled "HCFA, State Medicaid Manual
$ 5122 (April 1988)."
13. Attached hereto as Exhibit Q is a true and
correct copy of Chapter 21 from a document entitled "HEW, A
Guide to Screening-EPSDT Medicaid (1974)."
14. Attached hereto as Exhibit R is a true and
correct copy of HEW, Information Memorandum, "New Technology
Available in the Screening and Detection of Lead Poisoning and
EPSDT" (IM-77-32 (MSA)) (June 9, 1977).
27
28
15. @ coche hereto as Exhibiy S is a true and
correct copy of an excerpt from a document entitled, "HEW, A
Guide to Administration, Diagnosis and Treatment of the EPSDT
PRogram under Medicaid (1977)."
16. Attached hereto as Exhibit T is a true and
correct copy of a document entitled, "135 Cong. Rec. S 13233
(Oct. 12, 1989).
17. Attached hereto as Exhibit U is a true and
correct copy of a document entitled, "Explanation of the
Conference Committee Affecting Medicare-Medicaid Programs Re;
Omnibus Budget Reconciliation Act of 1989 (H.R. 3299), reprinted
in Medicare & Medicaid Guide (CCH), Extra Edition No. 603 (Dec.
15, 1989).
18. Attached hereto as Exhibit V is a true and
correct copy of a document entitled, "Letter from Charles A.
Wwoffinden, Chief of HHS Region IX Medicaid Operations Branch,
to Michael Quinn, CHDP Research Manager (April 11, 1991).
19. Attached hereto as Exhibit W is a true and
correct copy of a document entitled, "Letter from Charles A.
Wwoffinden, Chief of HHS Region IX Medicaid Operations Branch,
to Michael Quinn, CHDP Research Manager (May 7, 1991).
I declare under the penalty of perjury that the
foregoing is true. Dated this 23rd day of May 1991 in Los
Angeles, California.
Cel
rene Perkins
TABLE OF CONTENTS
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibit
Exhibits
Declaration of Dr. John F. Rosen
Declaration of Dr. Herbert L. Needleman
CHDP Provider Information Notice #91-6 from
Director Kenneth Kizer to CHDP Providers Re:
Lead Poisoning in Children (March 12, 1991)
S. Roan, "High Number of Lead Poison Cases
Found," L.A. Times, Aug. 30, 1990, A3, col. 1
DHS, Statewide: Fiscal Year 1989-90 Ethnicity
by Age Group by Funding Source by Lead Test
(Feb. 15, 1991)
DHS, Statewide: July 1990 thru January 1991
Ethnicity by Age Group by Funding Source by
Lead Test (Feb. 15, 1991)
DHS Medical Care Statistics Section,
California’s Medical Assistance Program
Annual Statistical Report Calendar Year 1989
Tables 20 and 29)
DHS, Fiscal Year 1989-90 Provider Number by
Age Group by Funding Source by Lead Test:
County of Residence = Santa Clara (Feb. 15,
1991)
DHS, Fiscal Year 1989-90 Ethnicity by Age
Group By Funding Source by Lead Test: County
of Residence = Los Angeles (Feb. 15, 1991)
Deposition of Ruth Range (excerpts)
Deposition of Dr. Maridee A. Gregory
(excerpts)
Health Care Coverage for Children: Hearing
Before the Senate Committee on Finance, 101lst
Cong., lst Sess. 24 (statement of Kay A.
Johnson, Director, Children’s Defense Fund
Health Division) (June 20, 1989)
Report of the House Budget Committee on H.R.
3299 (Sept. 20, 1989) reprinted in Medicare &
Medicaid Guide (CCH), Extra Edition No. 596
(Oct. 5, 1989)
HCFA, State Medicaid Manual, § 5123.2(D)
(incorporating revisions contained in HCFA
transmittals of April and July 1990)
Exhibit 0 -- 3 HEW, Medical Assistance 9... § 5-70-00 et
5 seq. (June 28, 1972)
3 Exhibit P -- HCFA, State Medicaid Manual § 5122 (April
1988)
4 Exhibit Q -- HEW, A Guide to Screening-EPSDT Medicaid
5 (Chapter 21) (1974)
6 Exhibit R -- HEW, Information Memorandum, "New Technology
Available in the Screening and Detection of
. Lead Poisoning and EPSDT" (1M-77-32 (MSA))
(June 9, 1977), reprinted in Medicare &
a Medicaid Guide (CCH) 9 28,505
9 Exhibit S -- HEW, A Guide to Administration, Diagnosis and
Treatment for the EPSDT Program under
10 Medicaid (1977) (excerpts)
11 Exhibit T -- 135 Cong. Rec. 8 13233 (October 12, 19389)
12 Exhibit U -- Explanation of the Conference Committee
Affecting Medicare - Medicaid Programs Re:
13 Omnibus Budget Reconciliation Act of 1989
(H.R. 3299), reprinted in Medicare & Medicaid
14 Guide (CCH), Extra Edition No. 603 (Dec. 15,
1989)
15 lpxhibit V -- Letter from Charles A. Woffinden, Chief HHS
16 Medicaid Operations Branch to Michael Quinn,
CHDP Research Manager (April 11, 1991)
17 Exhibit W -- Letter from Charles A. Woffinden, Chief HHS
18 Medicaid Operations Branch, to Michael Quinn,
CHDP Research Manager (May 7, 1991)
18
20
21
22
23
24
25
26
27
28
EXHIBIT A
Py £
f {
DECLARATION OF DR. JOHN F. ROSEN
I, Dr. John F. Rosen, declare and say:
1. The facts set forth herein are personally known to me
and I have first hand knowledge of them. If called as a witness,
I could and would testify competently thereto under oath.
2. I am currently a Professor of Pediatrics at Albert
Einstein College of Medicine, where I have been on the faculty
since 1969 and Head of the Division of Pediatric Metabolism since
1980. I am the Director of Metabolism Services and Attending
Physician at Montefiore Hospital and Medical Center
("Montefiore"), located in Bronx, New York. During the past 20
years, I have conducted research, written, and consulted
extensively on matters relating to lead poisoning, and I
currently am Chairman of the United States Department of Health
and Human Services ("HHS") Centers for Disease Control’s { CDC?)
Advisory Committee on Childhood Lead Poisoning Prevention, as I
was in 1985. A copy of my Curriculum Vitae is attached.
(Exhibit A hereto.)
3. At Montefiore, I direct the most comprehensive lead
poisoning prevention and research program in the United States,
involving basic research, clinical research, and clinical
service. Our Lead Poisoning Prevention Project, involving a team
of 22 health professionals, provides a bridge between medical and
environmental intervention and management. Under my supervision,
approximately 3,000 lead blood tests are conducted each year, and
i R i
more people are treated for lead poisoning than at any other
facility in the United States.
4. Childhood lead poisoning is the most common and
preventable pediatric health problems in the United States today.
According to the CDC and the Agency for Toxic Substances and
Disease Registry, lead poisoning is the number one environmental
health hazard for children in the United States. No
socioeconomic group, geographic area, or racial or ethnic
population is spared. At least three to four million children -
- one in six -- have lead levels in their blood (from lead paint
exposure alone) high enough to cause significant impairment of
their neurologic development. Experts have estimated that over
67% of black inner-city children and 17% of all children in the
United States under the age of six are at high risk for
developing lead poisoning.
5. These astonishing levels of exposure are due to the
ubiquitous nature of lead in the human environment -- in lead-
based paint and gasoline, drinking-water and pipes, printing inks
and pigments used in toys, fertilizers, lead-soldered food cans,
and soil and dust. And, because of their tendency to hand-to-
mouth activity and because of the vulnerability of the developing
central nervous system, young children are particularly
susceptible both to exposure and to lead’s toxic effects.
Although all children are at risk for lead poisoning, poor and
minority children are disproportionately affected because they
are more likely to (1) live or visit in homes with peeling or
chipping paint; (2) live or visit in homes built before 1959 with
planned or ongoing renovation; or (3) live in homes built before
1978 which may be deteriorating and still contain hazardous
quantities of leaded paint. According to the Agency for Toxic
Substances and Disease Registry’s Report to Congress (Exhibit B
hereto), approximately 52 percent of current housing stock (more
than 40 million household dwellings) still contain some 3 million
tons of leaded paint (or approximately 110 pounds per dwelling).
6. Lead is a poison that affects virtually every system in
the body. Although it is particularly harmful to the developing
brain and nervous system of young children, the adverse effects
of lead exposure on children and adults are wide-ranging. Very
severe lead exposure (70 ug/dL or greater) can cause coma,
convulsions, and even death. Lower levels cause adverse effects
on the central nervous system, kidney, reproductive system
(impotence, sterility, spontaneous abortion), and blood system
(anemia). Blood lead levels as low as 10 ug/dL are associated
with decreased intelligence and slowed neurobehavioral and
cognitive development that are likely to be irreversible. Other
effects of even low lead exposure include decreased stature and
hearing acuity, impaired biosynthesis of the active Vitamin D
metabolite and hemoglobin, and reduced serum total and ionized
calcium levels -- in other words, multiple, cascading normal
physiological systems and pathways, essential to the functioning
of many critical organs.
-” - a ’
* | é
7. Most poisoned children, however, have no symptoms. As a
2
result, the vast majority of lead poisoning cases go undiagnosed
and untreated. Because of this and the fact that early lead
toxicity has the potential to be reversible, monitoring of blood
lead levels of young children through periodic screening is
absolutely essential. Once detected, lead poisoning and related
health effects can often be treated and, in many cases, measures
can be undertaken to detect and eliminate the source of exposure.
Screening programs have had a tremendous impact on reducing the
occurrence of symptomatic lead poisoning in the United States.
Symptomatic lead poisoning almost invariably results in
irreversible, severe, and clinically evident neurological
sequelae.
8. Measuring blood lead content is the most accurate and
reliable method of screening for recent lead exposure. Blood
lead level testing is essential to adequate lead screening
programs, in part because an oral assessment of risk factors is
totally unreliable to identify toxicity in young children. Only
direct measurements of lead in blood can establish the presence
or absence of recent excessive exposure. For all children, I am
not aware of any protocol for lead screening satisfying accepted
professional standards that fails to include periodic blood lead
level tests. In my opinion, periodic screening by blood lead
measurement should be conducted at least once per year for any
child under the age of six because virtually all young children -
- especially those who are poor -- are at risk for lead
poisoning. For children considered to be at high risk for lead
exposure due to positive testing results or environmental or
other factors, blood lead testing should be conducted, at the
very least, every three to six months. To do otherwise would be
unconscionable in light of what we now know of the effects of
lead at relatively low exposure levels.
9. The CDC is currently in the process of drafting a Lead
Statement entitled "Preventing Lead Poisoning in Young Children"
(March 1991 (Draft)). As part of that process, the CDC’s
Advisory Committee on Childhood Lead Poisoning Prevention in
November 1990 voted unanimously that all children be screened for
lead poisoning -- in other words, that lead screening of children
be universal -- and recommended further that screening include a
blood lead test. In my opinion, the requirement that all
Medicaid eligible children ages 1-5 be tested for lead poisoning
is reasonable, medically appropriate, and an essential part of
even a minimally adequate and medically effective lead screening
and prevention program.
Executed at Bronx, New York this ‘22day of May 1991.
I declare under penalty of perjury that the foregoing is
ot ST
true and correct.
DR. JOHN F. ROSEN
: 1
} i
CURRICULUM VITAE
JOHN FRIESNER ROSEN, M.D.
BORN: JUNE 3, 1935, NEW YORK CITY
EDUCATION:
POST
Harvard College, 1953-1957, B.A.
Columbia University College of Physicians and Surgeons
1957-1961, M.D.
GRADUATE TRAINING:
Montefiore Hospital and Medical Center
1961-1962, Internship
Columbia-Presbyterian Medical Center
1962-1965, Resident in Pediatrics (Babies Hospital)
Rockefeller University, 1965-1967, Guest Investigator (Post
Doctoral Fellow) (Mineral Metabolism and Peptide Chemistry)
Intern - Montefiore Hospital and Medical Center, 1961-1962
Junior Resident - Babies Hospital, New York City, 1962-1964
Senior Resident - Babies Hospital, New York City, 1964-1965
PROFESSIONAL EMPLOYMENT AND HOSPITAL APPOINTMENTS:
Assistant Physician - The Rockefeller University, 1965-1969
Guest Investigator - The Rockefeller University, 1965-1967
Research Associate - The Rockefeller University, 1967-1969
Research Collaborator - Brookhaven National Laboratory
(Departments of Medicine and Physics), 1975-Present
Chairman, Research Advisory Committee - Tandem = Van de
Graaff Facility, Brookhaven National Laboratory
Department of Physics), 1979-Present
Director, Metabolism Services
Montefiore Medical Center, 1969-Present
Head, Division of Pediatric Metabolism, Albert Einstein
College of Medicine, 1980-Present
Adjunct Attending Physician - Montefiore Hospital and Medical
Center, 1969-1974
Associate Attending Pediatrician - Montefiore Hospital and
Medical Center, 1974-1978
/
Attending Pediatrician - Montefiore Hospital and Medical
Center, 1978-Present
Assistant Professor of Pediatrics - Albert Einstein College of
o Medicine, 1969-1975
Associate Professor of Pediatrics - Albert Einstein College of
Medicine, 1975-1980
Professor of Pediatrics - Albert Einstein College of Medicine,
1980-Present
BOARD CERTIFICATION: Diplomate, American Board of Pediatrics, 1966
PROFESSIONAL SOCIETY MEMBERSHIPS:
American Chemical Society, 1967-Present
Sigma XI, 1967-Present
American Association for the Advancement of Science, 1967-
Present
American Federation for Clinical Research, 1969-Present
Fellow of the American Academy of Pediatrics, 1966-Present
Harvey Society, 1966-Present
New York Academy of Sciences, 1971-Present
Society for Pediatric Research, 1972-Present
Lawson Wilkins Pediatric Endocrine Society, 1975-Present
American Pediatric Society, 1979-Present
American Institute of Nutrition, 1979-Present
American Society for Bone and Mineral Research, 1979-Present
Society of Toxicology, 1984-Present
OTHER PROFESSIONAL ACTIVITIES:
Research Committee - Montefiore Hospital and Medical Center,
1980-Present
Committee on Appointments and Promotions to Rank of Full
Professor - Albert Einstein College of Medicine, 1982-1984
Peer Review Panel, Health Effects Chapters, Lead Criteria
Document, EPA - 1982-1984
Consultant and Author, E.P.A. (Washington). Writing of
Air Lead Quality Criteria Document - 1981, 1985.
Ad Hoc Member, Toxicology Study Section, Division of
Research Grants, N.I.H. - 1982-1984
Chairman, Centers for Disease Control Advisory Committee on
Childhood Lead Poisoning Prevention. CDC, 1984
Member, Toxicology Study Section, Division of Research Grants,
N.1.H., 1985-1989
Member, National Academy of Science, National Research Council
Committee on Low Level Exposure in Susceptible Populations.
1989-
Chairman, Centers for Disease Control Advisory Committee on
childhood Lead Poisoning Prevention. CDC, 1990-
CURRENT GRANT SUPPORT:
1. The metabolism of lead in bone.
NIH #ES 01060-12-16
Dr. J.F. Rosen - Principal Investigator
12/01/86-11/30/96 (MERIT AWARD)
2. Treatment outcomes in moderately lead toxic children.
NIH #ES 04039-02-06
Dr. J.F. Rosen - Principal Investigator
3/1/86-4/30/92
3. A Nutritional Survey in Homeless Children.
Diamond Foundation
Dr. J.F. Rosen - Principal Investigator
1988-1992
4. Lead Poisoning Prevention Project.
Aron/JC Penney and Robert Wood Johnson Foundations
Dr. John F. Rosen - Principal Investigator
1987-1992
5. MERIT AWARDEE of the National Institute of Environmental
Health Sciences - 1986-1996 (ES 01060)
6. SAFE House (Transition Housing) For Successfully Treated
Lead Poisoned Children and Their Families.
Robert Wood Johnson Foundation
Dr. John F. Rosen - Principal Investigator
1990-1993.
REVIEWER FOR:
American Journal of Physiology
Annals of Internal Medicine
Journal of Clinical Endocrinology and Metabolism
Journal of Laboratory and Clinical Medicine
Journal of Neurochemistry
Journal of Pediatrics
Life Sciences
New England Journal of Medicine
Pediatric Research
Pediatrics
Science
Toxicology and Applied Pharmacology
® i
3 3
ARTICLES: (Selected)
l.
la.
12.
Haymovits, A.H. and Rosen, J.F.: Human thyrocalcitonin.
Endocrinology 81:993-1000, 1967.
Rosen, J.F., and Haymovits, A.H.!: Liver lysosomes in
congenital osteopetrosis: A study of lysosomal function,
calcitonin, parathyroid hormone, and 3',5' AMP. J. Peds.
81:518-527, 1972.
Rosen, J.F. and Finberg, L.: Vitamin D dependent rickets:
Actions of parathyroid hormone and 25-hydroxycholecalciferol.
Ped. Res. 6:552-562, 1972.
Rosen, J.F.: The microdetermination of blood lead in children
by flameless atomic absorption. The carbon rod atomizer. J.
Lab. and Clin. Med. 80:567-576, 1972.
Rosen, J.F. and Finberg, L.: Vitamin D dependent rickets:
Actions of parathyroid hormone and 25-hydroxycholecalciferol.
In, Clinical Aspects of Metabolic Bone Disease. Frame,
Parfitt and Duncan (Eds)., Excerpta Medica Foundation, 1973,
pp. 388-393.
Rosen, J.F.: The microdetermination of blood lead in children
by nonflame atomic absorption spectroscopy. In, Proceedings of
the Institutional Consortium on Endemic Lead Poisoning.
Clinical Toxicology Bulletin 3:111-118, 1973.
Daum, F., Rosen, J.F. and Boley, S.J.: Parathyroid adenoma,
parathyroid crisis, and acute pancreatitis in an adolescent.
J. Peds. 83:275-277, 19173.
Rosen, J.F., Zarate-Salvador, C. and Trinidad, E.E.: Plasma
lead levels in normal and lead-intoxicated children. J. Peds.
84:45-48, 1974.
Lamm, S. and Rosen, J.F.: Lead contamination in milks fed to
infants: 1972-1973. Pediatrics 53:137-141, 1974.
Rosen, J.F., Roginsky, M., Nathenson, G. and Finberg, L.: 25-
hydroxyvitamin D: Plasma levels in mothers and their premature
infants with neonatal hypocalcemia. Amer. J. Dis. Child.
1271:220~-223, 1974.
Rosen, J.F. and Trinidad, E.E.: The significance of plasma
lead levels in normal and lead-intoxicated children. Environ.
Health Perspect. 7:139-144, 1974.
Rosen, J.F. and Lamm, S.H.: Further comments on the lead
content of milks fed to infants. Pediatrics 53:144-145, 1974.
13.
14.
15,
le6.
1%.
18.
19.
20.
21.
22.
a3.
24.
Sorell, M. and Rosen, J.F.: Ionized calcium: Serum levels
during symptomatic hypocalcemia. J. Peds. 87:67-70, 1975.
Daum, F., Rosen, J.F., Roginsky, M., Cohen, M. and Finberg,
L.: 25-hydroxycholecalciferol in the management of rickets
associated with extrahepatic biliary atresia. J. Peds.
88:1041-1043, 1976.
Rosen, J.F. and Wexler, E.E.: Studies of lead transport in
bone organ culture. Biochem. Pharm. 26:650-652, 1977.
Rosen, J.F. and Sorell, M.: Interactions of lead, calcium,
vitamin D, and nutrition in lead-burdened children. In,
Clinical Chemistry and Chemical Toxicology of Metals. Brown,
8.8. (Ed.), Elsevier, 1977, pp. 27-31.
Rosen, J.F., Fleischman, A.R., Finberg, L., Eisman, J. and
DeLuca, H.F.? 1,25-dihydroxycholecalciferol: Oral
administration and sterol levels in the long-term management
of idiopathic hypoparathyroidism in children. In, Vitamin D:
Biochemical, Chemical and Clinical Aspects Related to Calcium
Metabolism. Norman, A.W. et al (Eds.) Walter de Gruyter,
Berlin, 1977, pp. 827-830.
Sorell, M., Rosen, J.F., and Roginsky, M.: Interactions of
lead, calcium, vitamin D and nutrition in 1lead-burdened
children. Arch. Environ. Health 32:160-164, 1977.
Rosen, J.F., Fleischman, A.R., Finberg, L., Eisman, J., and
DeLuca, H.F.: 1,25-dihydroxyvitamin D;: Its use in the long-
term management of idiopathic hypoparathyroidism in children.
J. Clin. Endocrinol. Metab. 45:457-468, 1977.
Rosen, J.F., Wolin, D. and Finberg, L.: Immobilization
hypercalcemia after single limb fractures in children and
adolescents. Amer. J. Dis. Child. 132:560-564, 1978.
Fleischman, A.R., Rosen, J.F., and Nathenson, G.: 25-
hydroxyvitamin D: Serum levels and oral administration in
neonates. Arch. Int. Med. 138:869-873, 1978.
Fleischman, A.R., Rosen, J.F., and Nathenson. G.: Oral 25-
hydroxycholecalciferol for the prevention of early neonatal
hypocalcemia in premature neonates. Amer. J. Dis. Child.
132:973-977, 1978.
Rosen, J.F., Fleischman, A.R., Finberg, L., Hamstra, A., and
DeLuca, H.F.: Rickets with alopecia: An inborn error of
vitamin D metabolism. J. Peds. 94:729-735, 1979.
Fleischman, A.R., Rosen, J.F., Nathenson, G. and Finberg, L.:
Oral 25-OHD in preventing neonatal hypocalcemia. In,
Pediatric Diseases Related to Calcium. Anast, DeLuca
(Eds.) ,Elsevier, 1980, pp. 345-354.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
ny ™
3 3
Chesney, R.W., Rosen, J.F., Hamstra, A. and Deluca, H.F.:
Serum 1,25-dihydroxyvitamin D levels in normal children and in
vitamin D disorders. Amer. J. Dis. Child. 134:135-139, 1980.
Rosen, J.F., Chesney, R.W., Hamstra, A., Deluca, H.F. and
Mahaffey, K.R.: Reduction in 1,25-dihydroxyvitamin D in
children with increased lead absorption. New Engl. J. Med.
302:1128-1131, 1980.
Rosen, J.F., and Markowitz, M.: D-Penicillamine: Its actions
on lead transport in bone organ culture. Ped. Res. 14:330-
335, 1980.
Fleischman, A.R., Rosen, J.F., Smith, C.M. and Deluca, H.F.:
Maternal and fetal levels of 1,25-dihydroxyvitamin D levels at
term. J. Peds. 97:640-642, 1980.
Sorell, M., Rosen, J.F., Kapoor, N., Rirkpatrick, D., Raju
S.K., Chaganti, Good, R.A., and O'Reilly, R.J.: Marrow
transplantation for juvenile osteopetrosis. Amer. J. Med.
70:1280-1287, 1981}.
Chesney, R.W., Rosen, J.F., Smith, C.M. and DeLuca, H.F.:
Absence of seasonal variation in serum concentrations of 1,25-
dihydroxyvitamin D despite a rise in 25-hydroxyvitamin D in
summer. J. Clin. Endocrinol. Metab. 53:139-142, 1981.
Eil, C., Liberman, U.A., Rosen, J.F., and Marx, S.J.: A
cellular defect in hereditary vitamin D-dependent rickets Type
II: Defective nuclear uptake of 1,25-dihydroxyvitamin D in
cultured skin fibroblasts. New Engl. J. Med. 304:1588-1591,
1981. :
Rosen, J.F., Chesney, R.W., Hamstra, A., and DeLuca, H.F.:
Reduction in 1,25-dihydroxyvitamin D in children with
increased lead absorption. In, Chemical Indices and
Mechanisms of Organ-Directed Toxicity. Brown, S$.8. {£d4.),
Pergamon Press, 1981, pp. 91-95.
Rosen, J.F.: The metabolism of lead-210 in isolated bone
cells. In, Chemical Indices and Mechanisms of Organ-Directed
Toxicity. Brown, S.S. (Ed.), Pergamon Press, 1981, pp. 305-
310.
Saenger, P., and Rosen, J.F.: 68-hydroxycortisol: A non-
invasive probe to evaluate inhibitory effects of lead on drug
metabolism in children. In, Chemical Indices and Mechanisms
of Organ-Directed Toxicity. Brown, S.S. (Ed.), Pergamon
Press, 1981, pp. 297-303.
Markowitz, M.E., Rotkin, L., and Rosen, J.F.: Circadian
rhythms of blood minerals in humans. Science 213:672-674,
1981.
® (1)
Rosen, J.F., Kraner, H.W., and Jones, K.W.: Effects of
CaNa,EDTA on lead and trace metal metabolism in bone organ
culture. Tox. Appl. Pharm. 64:230~-236, 1982.
Saenger, P., Rosen, J.F., and Markowitz, M.E.: The diagnostic
significance of EDTA testing in children with increased lead
absorption. Amer. J. Dis. Child. 136:312-315, 1982.
Wielopolski, L., Rosen, J.F., Slatkin, D., and Cohn, S.: Non-
invasive L-X-ray fluorescence analysis of lead in the human
tibia. Medical Physics 10:248-251, 1983.
Wisniewski, K.E., French, J.H., Rosen, J.F., Kozlowski, P.,
Tenner, M. and Wisniewski, N.H.: Basal ganglia calcification
(BGC) in Down's syndrome (DS)-another manifestation of
premature aging. Annals New York Acad. Sci. 396:179-192,
1982.
Mahaffey, K.R., Rosen, J.F., Chesney, R.W., Peeler, J.R.,
Smith, C.M. and DeLuca, H.F.: Association between age, blood
lead concentration, and serum 1,25-dihydroxycholecalciferol
levels in children. Am. J. Clin. Nutrition 35:1327-1331,
1981.
Markowitz, M.E., Rosen, J.F., Smith, C.M., and DeLuca, H.F.:
1-25-Dihydroxyvitamin D;-treated hypoparathyroidism: 35
patient years in 10 children. J. Clin. Endocrinol. Metab.
55:727-733, 1982.
Rosen, J.F.: The metabolism of lead in isolated bone cell
populations: Interactions between lead and calcium.
Toxicology and Applied Pharmacology 71:101-112, 1983.
Liverman, U.A., Ei}, C., Holst, P., Singer, F., Rosen, J.F.,
and Mary, S.J. Hereditary resistance to 1,25~
dihydroxyvitamin D: Defective function of receptors for 1,25-
dihydroxyvitamin D in cells cultured from bone. J.: Clin.
Endocrinol. 57:958-962, 1983.
Rosen, J.F.: Interactions between lead and calcium in
isolated bone cell populations. In, Clinical Chemistry and
Chemical Toxicity of Metals. Bronx, S.S. (Ed.), Academic
Press, 1983, pp. 247-250.
Saenger, P., Markowitz, M.E., and Rosen, J.F.: Depressed
excretion of 6g-hydroxycortisol in lead-toxic children. J.
Clin. Endocrinol. Metab. 58:363-367, 1984.
Markowitz, M., Rosen, J.F., and Mizruchi, M.: Circadian and
ultradian rhythms of blood minerals during adolescence.
Pediatr. Res. 18:456-462, 1984.
CB a ;
Markowitz, M.E. and Rosen, J.F.: Assessment of body lead
stores in children: Validation of an 8-hour CaNa,EDTA
provocative test. J. Peds. 104:337-342, 1984.
Gundberg, C., Markowitz, M.E., and Rosen, J.F.: Osteocalcin
in human serum: A circadian rhythm. J. Clin. Endocrinol.
Metab. 60:737-739, 1985.
Markowitz, M.E., Rosen, J.F. and Mizruchi, M.: Circadian
variations in serum zinc concentrations: correlation with
blood ionized calcium serum total calcium and phosphate in
humans. Amer. J. Clin. Nut. 41:689-696. 1985.
Markowitz, M.E., Rosen, J.F. and Mizruchi, M.: Effects of
1,25-dihydroxyvitamin D; administration on circadian minerals
rhythms in humans. Calcif. Tiss. Internat. 37: 351-356, 1985.
Markowitz, M.E. Rosen, J.F., Holick, M.F., Hannifan N. an
Endres, D.: Time-related variations in serum 1,25-
dihydroxyvitamin D concentrations in humans. In, Vitamin D:
Biochemical Chemical and Clinical Aspects. Normal, A. (Ed.),
W. de Gruyter, Berlin, 1985, pp. 249-251.
Pounds, J.G. and Rosen, J.F.: The cellular metabolism of
lead: A kinetic analysis in cultured osteoclastic bone cells.
Tox. Appl. Pharmacol. 83:531-545, 1986.
Markowitz, M.E., Gundberg, C., and Rosen, J.F.: A rapid rise
in serum osteocalcin following 1,25-(OH),D; administration in
normal adults. Calcif. Tiss. Internat. 40:179-183, 1987.
Rosen, J.F. and Pounds, J.G.: The cellular metabolism of lead
and calcium: A kinetic analysis in cultured osteoclastic bone
cells. Contributions to Nephrology 64:64-71, 1988.
Pounds, J.G. and Rosen, J.F.: Cellular Ca" homeostasis and
Ca™-mediated cell processes as critical targets for toxicant
action; Conceptual and methodological pitfalls. Toxicology and
Applied Pharmacology 94:331-341, 1988.
Morris, V., Markowitz, M.E., and Rosen, J.F.: Serial
measurements of ALA dehydratase in lead toxic children. J.
Pediatrics 112:916-919, 1988.
Markowitz, M.E., Rosen, J.F., Arnaud, S.B., Thorpy, M. and
Laxminarayan, S.: Temporal interrelationships between the
circadian rhythms of serum parathyroid hormone and calcium
concentrations. J. Clin. Endocrinol. Metab. 67:1068-1073,
1988.
58.
59.
60.
61.
62.
63.
64.
65.
66.
67.
68.
® @
Rosen, J.F., Markowitz, M.E., Bijur, P.E., Jenks, 85.T.,
Wielopolski, L., Kalef-Ezra, J.A. and Slatkin, D.N.: L-x-ray
fluorescence of cortical bone lead compared with the CaNa,EDTA
test in lead-toxic children: Public health implications.
Proc. Nat. Acad. Sci. (USA). 86:685-689, 1989.
Rosen, J.F. and Pounds, J.G.: Quantitative interactions
between lead and calcium in osteoclastic bone cells. Toxicol.
Appl. Pharmacol. 98:530-543, 1989.
Wielopolski, L., Kalef-Ezra, J., Slatkin, D.N. and Rosen,
J.F.: Polarized L-x-ray fluorescence to measure cortical bone
lead. Medical Physics 16:521-529, 1989.
Markowitz, M.E., Fishman, K., Rosen, J.F., and Saenger, P.:
Effects of growth hormone therapy on circadian osteocalcin
rhythms in idiopathic short stature. J. Clin. Endocrinol.
Metab. 69:420-425, 1989.
Schanne, F.A.X., Dowd, T.L., Gupta, R.K. and Rosen, gsFe?
Lead increases free ca? concentration in cultured osteoblastic
bone cells: Simultaneous detection of intracellular free pPb%*
by 9F NMR. Proc. Natl. Acad. Sci. (USA). 86:5133-5135, 1989.
Long, G.J., Rosen, J.F., and Pounds, J.G.: Cellular lead
toxicity and metabolism in primary and clonal osteoblastic
bone cells. Toxicol. Appl. Pharmacol. 102:346-361, 1990.
Fullmer, C.S. and Rosen, J.F.: Effect of dietary calcium and
lead states on intestinal calcium absorption. Environ. Res.
51:91-99, 1990.
Markowitz, M.E., Rosen, J.F., and Bijur, P.E.: Effects of
iron deficiency on lead metabolism in moderately lead toxic
children. J. Pediatr. 116:360-364, 1990.
Kalef-Ezra, J.A., Slatkin, D.N., Rosen, J.F. and Wielopolski,
L.: Radiation risk to the human conceptus attributable to
measurement of maternal tibial bone lead by L-line x-ray
fluorescence. Health Physics 58:217-219, 1990.
Schanne, F.A.X. Dowd, T.L., Gupta, R.K. and Rosen, J.F.:
Development of 9F NMR for measurements of [Ca?*] and [Pb®] in
cultured osteoblastic bone cells. Environmental Health
Perspectives, 84:99-106, 1990.
Rosen, J.F., Markowitz, M.E., Bijur, P.E., Jenks, S.T.,
Wielopolski, L., Kalef-Ezra, J.A. and Slatkin, D.N.:
Sequential measurements of bone lead content by L-x-ray-
fluorescence in CaNa.EDTA-treated lead-toxic «children.
Environmental Health Perspectives, In press, 1990.
69.
70.
71.
® i i
Long, G.J., Pounds, J.G. and Rosen, J.F.: Lead impairs the
hormonal regulation of osteocalcin in rat osteosarcoma (ROS
17/2.8) cells. Toxicol. Appl. Pharmacol., In press, 1990.
Schanne, F.A.X., Dowd, T.L., Gupta, R.J., and Rosen, JeF.$
Differential effects of lead on parathyroid hormone-induced
changes in clonal osteoblastic bone cells using '’F NMR.
Biochim. Biophys. Acta., 1054:250-255, 1990.
Dowd, T.L., Rosen, J.F., and Gupta, R.K.: 3p NMR and
saturation transfer studies of the effect of lead on cultured
osteoblastic bone cells. J. Biol. Chem., In press, 1990.
10
® 3
REVIEWS:
1.
10.
11.
12.
Haymovits, A.H. and Rosen, J.F.: Calcitonin: Its nature and
role in man. Pediatrics 45:133-149, 1970.
Haymovits, A.H. and Rosen, J.F.: Calcitonin in metabolic
disorders. In, Advances in Metabolic Disorders. Levine, R.
and Luft. R. (Eds.), 6:177-212, 1972.
Rosen, J.F. and Finberg, L.: The real and potential uses of
new vitamin D; analogues in the management of metabolic bone
disease in intants and children. In, Nutritional Imbalances
in Infant and Adult Disease. Seelig, M. (Ed.), Spectrum,
1977, Pp. 87-102.
Rosen, J.F.: The metabolism and subclinical effects of lead in
children. In, The Biogeochemistry of Lead in the Environment.
Nriagu, J.0. (Ed.), Elsevier/North Holland, 1978, pp. 151-172.
Chesney, R.W., Rosen, J.F., Hamstra, A., Mazess, R.B. and
Deluca, H.F.: The use of serum 1,25-dihydroxyvitamin D
(Calcitriol) concentrations in the clinical assessment of
demineralizing disorders in children. In, Hormonal Control of
Calcium Metabolism. Excerpta, 1981, pp. 252-260.
Markowitz, M.E. and Rosen, J.F.: Mineral interactions in
health and disease. In, Pediatric Update. Moss, A. (Ed.),
Elsevier, 1982, pp. 97-114.
Rosen, J.F. and Chesney, R.W.: Circulating calcitriol
concentrations in health and disease. J. Peds. 103:1-17, 1983
(Medical Progress Article).
Chesney, R.W., Rosen, J.F., and DeLuca, H.F.: Disorders of
calcium metabolism in children. In, Recent Progress in
Pediatric Endocrinology, Raven Press, 1983, pp. 5-24.
Rosen, J.F.: Nuclear analytical methods and heavy metals -
real and potential applications in the biomedical sciences.
Neurotoxicology 4:218-219, 1983.
Piomelli, S., Rosen, J.F., and Chisolm, J.J. Jr.: Treatment
guidelines for the management of childhood lead poisoning. J.
Pediatrics 105:523-532, 1984.
Rosen, J.F.: Lead and the vitamin D-endocrine system. In,
Air Quality Criteria For Lead. Grant, L. and Davis, M.
(Eds.), Volume 4, Chapter 12, 1984, pp. 42-47.
Rosen, J.F.: Metabolic and cellular effects of lead: A guide
to low level lead toxicity in children. In, Dietary and
Environmental Lead Exposure. Mahaffey, K.R. (Ed.), Elsevier,
1985, Pp. 157-185,
11
13.
14.
15.
16.
17.
18.
19.
Rosen, J.F.: An overview of metabolic effects of lead in
children. In, Health Effects of Lead. Hotz, M. (Ed.), Royal
Society of Canada, Commission on Lead in the Environment,
1986, pp. 203-224.
Needleman, H.L., Rosen, J.F., Piomelli, S., Landrigan, P. and
Graef, J.: The hazards of benign neglect of elevated blood
lead levels. Amer. J. Dis. Child. 141:941-942, 1987.
Rosen, J.F.: The toxicological importance of lead in bone:
The evolution and potential uses of bone lead measurements by
x-ray fluorescence to evaluate treatment outcomes in
moderately lead toxic children. In, Biological Monitoring of
Toxic Metals. Clarkson, T. (Ed.), Plenum Press, 1988, pp.
603-621.
Rosen, J.F.: Metabolic abnormalities in lead-toxic children:
Public health implications. Bull. New York Acad. 65:1067-1084,
1989.
Rosen, J.F., Novak, R.F. and Galvin, M.J.: The calcium
messenger system: Implications for toxicological research.
Environmental Health Perspectives, 84:3-5, 1990.
Pounds, J.G., Long, G., and Rosen, J.F.: The toxicology of
lead in bone. Environ. Health Perspectives, In press, 1990.
Rosen, J.F., and Pounds, J.G. The metabolism of lead in bone.
CRC Review in Toxicology, In preparation, 1990.
12 A
The Nature and Extent of
Lead Poisoning in Children
in the United States:
A Report to Congress
July 1988
PART 1
EXECUTIVE SUMMARY
Exposure to lead continues to be a serious public health problem --
particularly for the young child and the fetus. The primary target organ for
lead toxicity is the brain or central nervous system, especially during early
child development. In children and adults, very severe exposure can cause
coma, convulsions, and even death. Less severe exposure of children can produce
delayed cognitive development, reduced IQ scores, and impaired hearing -- even
at exposure levels once thought to cause no harmful effects. Depending on the
amount of lead absorbed, exposure can also cause toxic effects on the kidney,
impaired regulation of vitamin D, and diminished synthesis of heme in red blood
cells. All of these effects are significant. Furthermore, toxicity can be
persistent, and effects on the central nervous system (CNS) may be irreversible.
In recent years, a growing number of investigators have examined the
effects of exposure to low levels of lead on young children. The history of
research in this field shows a progressive decline in the lowest exposure
levels at which adverse health effects can be reliably detected. Thus, despite
some progress in reducing the average level of lead exposure in this country,
it is increasingly apparent that the scope of the childhood lead poisoning
problem has been, and continues to be, much greater than was previously
realized.
The "Nature and Extent of Lead Poisoning in Children in the United States:
A Report to Congress" was prepared by the Agency for Toxic Substances and
Disease Registry (ATSDR) in compliance with Section 118(f) of the 13986
Superfund Amendments and Reauthorization Act (SARA) (42 U.S.C. 9618(f)). This
Executive Summary is a guide to the structure of the document and, in partic-
ular, to the organization of the responses to the specific directives of
Section 118(f). It also provides an overview of issues and directions to the
U.S. lead problem.
® p
The report comprises three parts: Part 1, consisting of the Executive
Summary; Part 2, consisting of Chapter I. "Report Findings, Conclusions, and
Overview," which provides a more detailed overview of information and conclu-
sions abstracted from the main body of the report; and Part 3, consisting of
Chapters II through XI, which constitute the main body of the report.
Before addressing the specific directives of Section 118(f), it is
important to point out that childhood lead poisoning is recognized as a major
public health problem. In a 1987 statement, for example, the American Academy
of Pediatrics notes that lead poisoning is still a significant toxicological
hazard for young children in the United States. It is also a public health
problem that is preventable.
In recognition of evolving scientific evidence of the harmful effects of
lead exposure, Congress directed ATSDR to examine (1) the long-term health
implications of low-level lead exposure in children; (2) the extent of low-
level lead intoxication in terms of U.S. geographic areas and sources of lead
exposure; and (3) methods and strategies for removing lead from the environment
of U.S. children.
The childhood lead poisoning problem encompasses a wide range of exposure
levels. The health effects vary at different levels of exposure. At low
levels, the effects on children, as stated subsequently in this report, may not
be as severe or obvious, but the number of children adversely affected is
large. Moreover, as adverse health effects are detected at increasingly lower
levels of exposure, the number of children at risk increases. At intermediate
exposure levels, the effects are such that a sizable number of U.S. children
require medical and other forms of attention, but usually they do not need to
be hospitalized, nor do they need conventional medical treatment for lead
poisoning. For these children, the only appropriate solution, at present, is
to eliminate or reduce all significant sources of lead exposure in their
environment. At high levels, the effects are such that children require
immediate medical treatment and follcw-up. Various clinics and hospitals,
particularly in larger cities, continue to report such cases.
Lead exposure may be characterized in terms of either external or internal
concentrations. External exposure levels are the concentrations of lead in
environmental media such as air or water. For internal exposure, the most
widely accepted and commonly used measure is the concentration of lead in
blood, conventionally denoted as micrograms of lead per deciliter (100 ml) of
whole blood -- abbreviated pg/dl. For example, when ATSDR estimated the number
2
@ Q
of children considered to be at risk for adverse health effects, the Agency
used blood lead (Pb-B) levels of 25, 20, and 15 pg/dl to group children by their
degree of exposure.
These levels are not arbitrary. In 1985 the Centers for Disease Control
(CDC) identified a Pb-B level of 25 pg/dl along with an elevated erythrocyte
protoporphyrin level (EP) as evidence of early toxicity. For a number of
practical considerations, CDC selected this level as a cutoff point for medical
referral from screening programs, but it did not mean to imply that Pb-B levels
below 25 pg/dl are without risk. More recently, the World Health Organization
(WHO), in its 1986 draft report on air quality guidelines for the European
Economic Community, identified a Pb-B level of 20 pg/dl as the then-current
upper acceptable limit. In addition, the Clean Air Scientific Advisiory Commit-
tee to the U.S. Environmental Protection Agency (EPA) has concluded that a Pb-B
level of 10 to 15 pg/dl in children is associated with the onset of effects that
“may be argued as becoming biomedically adverse". In this connection, the
available evidence for a potential risk of developmental toxicity from lead
exposure of the fetus in pregnant women also points towards a Pb-8 level of 10
to 15 pg/dl, and perhaps even lower. These various levels represent an evolving
understanding of low-level lead toxicity. They provide a reasonable means of
quantifying aspects of the childhood lead poisoning problem as it is currently
understood. With further research, however, these levels could decline even
further.
A. RESPONSE TO DIRECTIVES OF SECTION 118(f) of SARA
Section 118(f) and its five directives give ATSDR the mandate to prepare
this report. These directives are identified in the five subsections below.
1. Section 118(f)(1)(A)
This subsection requires an estimate of the total number of children,
arrayed according to Standard Metropolitan Statistical Area (SMSA) or other
appropriate geographic unit, who are exposed to environmental sources of lead
at concentrations sufficient to cause adverse health effects. Chapter V,
"Examination of Numbers of Lead-Exposed Children by Areas of the United
States," and Chapter VII, "Examination of Numbers of lLead-Exposed Women of
Childbearing Age and Pregnant Women," respond to this directive.
3
i
w » |
Valid estimates of the total number of lead-exposed children according to
SMSAs or some other appropriate geographic unit smaller than the Nation as a
whole cannot be made, given the available data. The only national data set for
Pb-B levels in children comes from the National Health and Nutrition Examina-
tion Survey II (NHANES II) of CDC's National Center for Health Statistics. The
NHANES II statistical sampling plan, however, does not permit valid estimates
to be made for geographic subsets of the total data base.
In this report, the numbers of white and black children (ages 6 months to
5 years) living in all SMSAs are quantified according to selected blood lead
levels and 30 socioeconomic and demographic strata. Within large SMSAs (those
with over 1 millfon residents each) for 1984, an estimated 1.5 million children
had Pb-B levels above 15 pg/dl. In smaller SMSAs (with fewer than 1 million
residents), an estimated 887,000 children had Pb-B levels above 15 pg/dl.
In short, about 2.4 million white and black metropolitan children, or
about 17X of such children in U.S. SMSAs, are exposed to environmental sources
of lead at concentrations that place them at risk of adverse health effects.
This number approaches 3 million black and white children if extended to the
entire U.S. child population. If the remaining racial categories are included
in these totals, between 3 and 4 million U.S. children may be affected. The
numbers of children in SMSAs with blood lead levels above 20 and 25 pg/d) are
715,000 (5.2) and 200,000 (1.5X), respectively. These figures, however, are
for all strata combined; many strata (e.g., black. inner-city, or low-income)
have much higher percentages of children with elevated Pb-B levels.
Although these projected figures, based on the NHANES II survey, provide
the best estimate that can now be made, they were derived from data collected
in 1976-1980 (the years of NHANES II) and extrapolated to 1984. With respect
to bounds to the above projections, variables in the methods used to generate
these figures contribute to both overestimation and underestimation. The major
source of overestimation is the unavoidable omission of declines in food lead
that may have occurred in the interval 1978-1964 and that would have affected
the results of the projection methodology. On the other hand, two significant
factors contribute to underestimation. One is the restriction of the estimates
to the SMSA fraction of the U.S. child population, some 75% to 80% of the total
population. The other is the unavoidable omission of children of Hispanic,
Asian, and other origins in the U.S. population. In a number of SMSAs in the
West and South west, children in such segments outnumber black children. In
balancing all sources of overestimates and underestimates, including variance
4
® ®
in the projection mode) itself, the projections given are probably close to the
actual values. |
A breakdown of the above estimates according to national socioeconomic and
demographic strata shows that no economic or racial subgrouping of children is
exempt from the risk of having Pb-B levels sufficiently high to cause adverse
health effects. Indeed, sizable numbers of children from families with incomes
above the poverty level have been reported with Pb-B levels above 15 pg/dl.
Nevertheless, the prevalence of elevated Pb-B levels in inner-city, underprivi-
leged children remains the highest among the various strata. Although the
percentage of children with elevated Pb-B levels is not as high in, for example,
the more affluent segment of the U.S. population living outside central cities,
the total number of children with these demographic characteristics is much
greater than the number of poor, inner-city children. Consequently, the
absolute numbers of children with elevated Pb-B levels are roughly equivalent
for some of these rather different strata of the U.S. child population.
In this report, ATSDR has also used data from lead screening programs and
1980 U.S. Census data on age of housing to estimate SMSA-specific numbers of
children exposed to lead-based paint. In December 1986, ATSDR conducted a
survey of lead screening programs. Of 785,285 children screened in 1985,
11,739 (1.5%) had symptoms of lead toxicity by one of two definitions. Because
CDC criteria for lead toxicity changed in 1985, some programs were still using
the 1978 CDC criteria (Pb-B 230 pg/d) and EP 250 pg/dl) in 1985, whereas others
used the new 1985 CDC criteria (Pb-B 225 pg/dl and EP 235 pg/dl).
Differences in the estimates of children with lead toxicity become
apparent when using the NHANES II data and the childhood lead screening program
data. Estimates derived from screening program data very likely underestimate
the actual magnitude of childhood lead exposure by a considerable margin. This
is especially evident when the percentages of positive test results from
screening programs are compared with the much higher NHANES II prevalences of
elevated Pb-B levels in strata corresponding to screening program target
groups, for example, poor, inner-city children in major metropolitan areas.
An analysis of 318 SMSAs, based on 1980 Census data on age of housing,
showed that 35 SMSAs had 50% or more of the children living in housing built
before 1950. A total of 4,374,600 children (from these 318 SMSAs alone) lived
in pre-1950 housing. The percentage of these children with lead exposures
sufficient to cause adverse health effects could not be estimated, but the
older housing in which they live is likely to contain paint with the highest
levels of lead and is, therefore, likely to pose an elevated risk of dangerous
lead exposure. A noteworthy finding concerns the distribution of children in
older housing according to family income. Actual enumerations (not estimates)
show that children above the poverty level constitute the largest proportion of
children who reside in older housing. The implication, consistent with the
conclusion based on projections from NHANES II data that was stated above, is
that children above the poverty level are not exempt from lead exposure at
levels sufficient to place them at risk for adverse health effects. Children
above the poverty level are the most numerous group within the U.S. child
population.
Although Section 118(f)(1)(A) does not explicitly request such information,
an accurate description of the full childhood lead poisoning problem requires
an estimate of the number of fetuses exposed to lead in utero, given the
susceptibility of the fetus to low-level lead-induced disturbances in develop-
ment that first become evident at birth or even some time later during early
childhood. Accordingly, in a given year, an estimated 400,000 fetuses (within
SMSAs alone) are exposed to maternal Pb-B levels of more than 10 pg/dl and are
therefore at risk for adverse health effects. This number pertains to a single
year; the cumulative number of children who have been exposed to undesirable
levels of lead during their fetal development is much greater, particularly in
view of the higher average levels of exposure that prevailed in past years.
2. Section 118(f)(1)(B)
This subsection requires an estimate of the total number of children
exposed to environmental sources of lead arrayed according to source or source
types. Chapters VI ("Examination of Numbers of Lead-Exposed Children in the
United States by Lead Source") and VIII ("The Issue of Low-Level Lead Sources
and Aggregate Lead Exposure of Children in the United States") respond to this
directive.
The six major environmental sources of lead are paint, gasoline, stationary
sources, dust/soil, food, and water. Dust/soil is more properly classified as
a pathway rather than a source of lead, but since it is often referred to as a
source, it is included. (Figure 11-1 in the main report shows how lead from
these sources reaches children.) The complex and interrelated pathways from
® @®
these sources to children severely complicate efforts to determine source-
specific exposures. Consequently, exact counts of children exposed to specific
sources of lead do not exist.
The first step in approximating the number of children exposed to lead
from each of the six major sources is to define what constitutes exposure. For
each lead source, approximate exposure categories are defined and range from
potential exposures through actual exposures known to cause lead toxicity.
Because the type and availability of data for each lead source vary consider-
ably, definitions of exposure categories also differ for each lead source. The
total numbers of children estimated for each source and category are therefore
not comparable and cannot be used to rank the severity of the lead problem by
source of exposure in a precise, quantitative way. Furthermore, because of the
nature of methods used to calculate the numbers of children in these exposure
categories, it is not possible to provide estimate errors. Some numbers are
best estimates, but others may represent upper bounds or lower bounds.
One should not overlook the limitations and caveats for these calculations,
lest the estimates be misinterpreted and misapplied. In addition, source-based
exposure estimates of children have different levels of precision. The
estimated number of children potentially exposed to a given lead source at any
level is necessarily greater than the number actually exposed at a level
sufficient to produce a specified Pb-B value. Source-specific estimates of
potentially and actually exposed children, based on the best available informa-
tion and reasonable assumptions, are summarized as follows:
) For leaded paint, the number of potentially exposed children
under 7 years of age in all housing with some lead paint at
potentially toxic levels is about 12 million. About 5.9 million
children under 6 years of age live in the oldest housing, that
is, housing with the highest lead content of paint. For the
oldest housing that is also deteriorated, as many as 1.8 to
2. 0 million children are at elevated risk for toxic lead expo-
sure.
The number of young children likely to be exposed to enough
paint lead to raise their Pb-B levels above 15 pg/dl is esti-
mated to be about 1.2 million.
0 An estimated 5.6 millfon children under 7 years old are poten-
tially exposed to lead from gasoline at some level.
Actual exposure of children to lead from gasoline, was projec-
ted, for 1987, to affect 1.6 million children up to 13 years of
age at Pb-B levels above 15 pg/dl.
7
The estimated number of children potentially exposed to U.S.
stationary sources (e.g., smelters) is 230,000 children.
The estimated number of children exposed to lead emissions from
primary and secondary smelters sufficient to elevate Pb-B concen-
trations to toxic levels is about 13,000; estimates for other
stationary sources are not available.
The number of children potentially exposed to lead in dust and
soil can only be derived as a range of potential exposures to
the primary contributors to lead in dust and sofl, namely, paint
lead and atmospheric lead fallout. This range is estimated at
5.9 million to 11.7 million children. :
The actual nusber of children exposed to lead in dust and soil
at concentrations adequate to elevate Pb-B levels cannot be
estimated with the data now avajlable.
Because of lead in old residential plumbing, 1.8 million chil-
dren under 5 years old and 3.0 million children 5 to 13 years
old, are potentially exposed to lead; for new residences (less
than 2 years old), the corresponding estimates of children are
0.7 and 1.1 million, respectively.
Some actual exposure to lead occurs for an estimated 3.8 million
children whose drinking water lead level has been estimated at
greater than 20 pg/1.
EPA, in a recent study, estimated that 241,000 children under
6 years old have Pb-B levels above 15 pg/dl because of elevated
concentrations of lead in drinking water. Of this number, 100
have Pb-B levels above 50 pg/dl, 11,000 have Pb-B levels between
30 and S50 pg/dl, and 230,000 have Pb-B levels between 15 and
30 pg/dl.
Most children under 6 years of age in the U.S. child population
are potentially exposed to lead in food at some level.
Actual exposure to enough lead in food to raise Pb-B levels to
an early toxicity risk level has been estimated to impact as
many as 1 million U.S. children.
Despite limitations in the precision of the above estimates, relative
judgments can be made about the impact of different exposure sources. Some key
findings are:
As persisting sources for childhood lead exposure in the United
States, lead in paint and lead in dust and soil will continue as
major problems into the foreseeable future.
po
0 As a significant exposure source, leaded paint is of particular
concern since it continues to be the source associated with the
severest forms of lead poisoning.
0 Lead levels in dust and soil result from past and present inputs
from paint and air lead fallout and can contribute to signifi-
cant elevations in children's body lead burden (i.e., the
accumulation of lead in body tissues).
] In large measure, paint and dust/soil lead problems for children
are problems of poor housing and poor neighborhoods.
0 Lead in drinking water is a significant source of lead exposure
in terms of its pervasiveness and relative toxicity risk. Paint
and dust and soil lead are probably more intense sources of
exposure.
0 Greater attention must be paid to lead exposure sources away
from the home, especially lead in paint, dust, soil, and drink-
ing water in and around schools, kindergartens, and similar
locations.
0 The phasing down of lead in gasoline has markedly reduced the
number of children impacted by this source as well as the rate
at which lead from the atmosphere is deposited in dust and soil.
0 Lead in food has been reduced to a significant degree in recent
years and contributes less to body burdens in the United States
than in the past.
0 Significant exposure of unkown numbers of children can also
occur under special circumstances: renovation of old houses
with lead-painted surfaces, secondary exposure to lead trans-
ported home from work places, lead-glazed pottery, certain folk
medicines, and a variety of others unusual sources.
3. Section 118(f)(1)(C)
This subsection requires a statement of the long-term consequence for
public health of unabated exposure to environmental sources of lead.
Chapters 111 ("Lead Metabolism and Its Relationship to lead Exposure and
Adverse Effects of Lead") and IV ("Adverse Health Effects of Lead") address
this issue.
Infants and young children are the subset of the U.S. population considered
most at risk for excessive exposure to lead and its associated adverse health
effects. In addition, because lead is readily transferred across the placenta,
the developing fetus is at risk for lead exposure and toxicity. For this
reason, women of childbearing age are also an identifiable, albeit surrogate,
9
subset of the population of concern, not because of direct risk to their
health, but because of the vulnerability of the fetus to lead-induced harmful
effects.
Direct, significant impacts of lead on target organs and systems are
evident across a broad range of exposure levels. These toxic effects may range
from subtle to profound. In this report, the primary focus has been on effects
that are chronic and that are induced at levels of lead exposure not uncommon
in the United States. Cases of severe lead poisoning are, however, still being
reported, particularly in clinics in our major cities.
The primary target organ for lead toxicity is the brain or central nervous
system (CNS), especially during early child development. Other key targets
in children are the body heme-forming system, which is critical to the
production of heme and blood, and the vitamin D regulatory system, which
involves the kidneys and plays an important role in calcium metabolism. Some
of the major health effects of lead and the lowest-observed-effect levels (in
terms of Pb-B concentrations) at which they occur can be summarized as follows:
0) Very severe lead poisoning with CNS involvement commonly
includes coma, convulsions, and profound, irreversible mental
retardation and seizures, and even death. Poisoning of this
severity occurs in some persons at Pb-B levels as low as
80 pg/dl. Less severe but still serious effects, such as
peripheral neuropathy and frank anemia, may start at Pb-B levels
between 40 and 80 pg/dl.
0 Numerous epidemiologic studies of children have related lower
levels of lead exposure to a constellation of impairments in CNS
function, including delayed cognitive development, reduced IQ
scores, and impaired hearing. For example, peripheral nerve
dysfunction (reduced nerve conduction velocities) have been
found at Pb-B levels below 40 pg/dl in children. In addition,
deficits in IQ scores have been established at Pb-B levels below
25 pug/dl. Preliminary data suggest that effects on one test of
children's intelligence may be associated with childhood Pb-8
levels below 10 pg/dl.
0 Adverse impacts on the heme biosynthesis pathway and on vitamin
D and calcium metabolism, all of which have far-reaching physio-
logical effects, have been documented at Pb-B levels of 15 to
20 pg/dl in children. At levels around 40 pg/dl, the effects on
heme synthesis increase in number and severity (e.g., reduced
hemoglobin formation).
0 Of particular concern are consistent findings from several
recent. longitudinal cover a period of years epidemiologic
studies showing low-level lead effects on fetal and child
development, including neurobehavioral and growth deficits.
10
® @®
These effects are associated with prenatal exposure levels of 10
to 15 pg/dl.
With regard to the long-term consequences of lead exposure during early
development, the American Academy of Pediatrics (1987) has noted that utmost
concern should be given to the irreversible neurological consequences of
childhood lead poisoning. Recent findings from longitudinal follow-up studies
of infants starting at birth (or even before birth) show persistent deficits in
mental and physical development through at least the first two years of life as
a function of low-level prenatal lead exposure. It {is not yet known, however,
whether deficits fn later childhood development will continue to show a signif-
icant linkage to prenatal exposure or whether, at older ages, postnatal lead
levels will overshadow the effects of earlier exposure. Human development is
quite plastic, with well known catch-up spurts in growth and other aspects of
development. On the other hand, even if early lead-induced deficits are no
longer detected at later ages, this apparent recovery does not necessarily
imply that earlier impairments are without consequence. In view of the complex
interactions that figure into the cognitive, emotional, and social development
of children, compensations in one facet of a child's development may exact a
cost in another area. Very little information is available for evaluating such
interdependencies and trade-offs, but at this point even "temporary" develop-
mental perturbations cannot be viewed as inconsequential.
In addition, given the poor prospects for immediate improvements in the
environments of many children (e.g., deteriorated housing occupied by under-
privileged, inner-city children), lead exposure and toxicity often are, in
practice, irreversible. Thus, the issue of persistence must encompass the
reality of exposure circumstances as well as the potential for biological
recovery.
4. Section 118(f)(1)(D)
This subsection asks for information on the methods and options available
for reducing children's exposure to environmental sources of lead. Chapter IX
("Methods and Alternatives for Reducing Environmental Lead Exposure for Young
Children and Related Risk Groups") addresses this issue. Abatement methods
include primary as well as secondary measures. Primary abatement refers to
reducing or eliminating lead's entrance into pathways by which people are
11
exposed; secondary abatement refers to ways of dealing with lead after it has
already entered the environment or humans. Biological ‘approaches such as
improved nutrition may fall into either of these two categories, depending on
whether they are intended primarily as prophylactic or treatment measures.
Extra-environmental approaches to prevention (e.g., legal actions and stric-
tures) are also discussed.
Here are some key points on the abatement of childhood lead exposure and
poisoning :
0 Efforts in the United States to remove or reduce human lead
exposure have produced notable successes as well as notable
failures.
) Effective primary lead abatement measures have included EPA's
phase-down regulations for gasoline lead, EPA's national ambient
air quality standard for lead, and cooperative actions between
the Food and Drug Administration and the food industry to reduce
lead in food.
0 A number of new initiatives are being implemented by EPA to
reduce lead in the drinking water of children and other popula-
tion segments. Of particular interest is water as it comes from
the tap not only in homes but in public facilities such as
kindergartens and elementary schools. The schools, in partic-
ular, present special exposure characteristics that have not yet
been adequately assessed.
0 Existing leaded paint in U.S. housing and public buildings
remains an untouched and enormously serious problem despite some
regulatory action in the 1970s to limit further input of new
leaded paint to the environment. For this source, corrective
actions have been a clear failure.
0 Lead in dust and soil also remains a potentially serious exposure
source, and remediation attempts have been unsuccessful.
] Secondary prevention measures in the form of U.S. lead screening
programs for children at high risk still appear to require
improved standardization of screening methodology (criteria for
populations, measurement techniques, data collection, data
reporting and statistical analysis) and central coordination.
) The effectiveness of screening children for lead poisoning is
well demonstrated in terms of deferred or averted medical
interventions, and in most settings is quite cost-effective.
0 Extra-environmental measures, such as comprehensive good nutri-
tion programs, have a role in mitigation of lead toxicity, but
they cannot be used as substitutes for initiatives to reduce
lead in the environment.
12
® {2
At present, legal sanctions do not appear to be very effective; to be effective, sanctions have to be both meaningful and rigidly enforced. So long as it is cheaper to pay a fine than to remove lead from the child's environment, little progress is likely to be made on this front.
The "easiest" steps to lead abatement have already been taken or are being taken. These steps, not surprisingly, have involved reducing lead in large-scale sources, such as gasoline and food, With more-or-less centralized distribution mechanisms.
Enormous masses of lead remain in housing along with large amounts of lead in du highly dispersed sources are to be abated, required.
5. Section 118(f)(2)
Chapter X (
Superfund"
Ss ] 1 Protection Agency (EPA)
The National Priorities List (NPL) of September 30, 1987, was reviewed to identify those Sites containing lead. Of the 457 sites, 307 have lead as an identified contaminant and 174 have an observed release of lead to air,
lead-based paint.
(HRS). (The minimu
site's listing on the NPL is 28.5.) Revisions of the HRS by EPA could change the urban site's score, depending on what revisions are made.
SUMMARY OF REPORT RECOMMENDATIONS
The report concludes with Chapter XI ("Lead Exposure and Toxicity in Children and Other Related Groups in the United States: Information Gaps, Research Needs, and Report Recommendations"), an overview of information gaps, research needs, and recommendations. Of key importance are the various general and specific recommendations of the report.
In view of the multiple sources of lead exposure, an attack on the problem
of childhood lead poisoning in the United States must be integrated and
coordinated, if it is to be effective. In addition, such an attack must
incorporate well-defined goals so that its progress can be measured. For
example, the lead exposure of children and fetuses must be monitored ang
assessed in a systematic manner if efforts to reduce their exposure are to
succeed. A comprehensive attack on the lead problem in the United States
should not preclude focused efforts by Federal, State, or local agencies with
existing statutory authorities to deal with different facets of the same
problem. Indeed, it is important that all relevant agencies continue to
respond to this important public health problem, but they should do so with an
awareness of how their separate actions relate to the goals of a comprehensive
attack.
Specific recommendations, by category, are summarized below:
0 Coordinated efforts to reduce lead levels in sources that remain
as major causes of lead toxicity, particularly paint and
dust/soil lead, are strongly recommended.
0 Scientific assessments of lead levels in these sources, through
strengthening of existing programs to monitor environmental
levels of lead, should accompany removal/reduction efforts.
0 Major improvements in the collection, interpretation, and
dissemination of environmental lead data on a national level are
needed. In particular, lead screening data should be compiled
in a uniform manner on a nationwide basis.
0 Precise and sensitive methodologies for environmental monitoring
and in situ measurement of lead concentrations in various media
are required.
0 An integrated assessment of all exposure sources for children is
required, including those that are obvious and others that are
not. Attention should be given to the lead exposure of children
away from the home: paint lead, dust/soil lead, and lead in
drinking water in schools, day-care centers, custodial care
institutions, and similar sites. Particular attention should be
given to the investigation of lead leaching into the drinking
water of children in schools.
0 The report strongly recommends that lead abatement initiatives
include careful consideration of lead movement to avoid simply
shifting the lead problem from one part of the environment to
another.
14
» »
The report strongly recommends that much more attention be paid
to exposure of the fetus with screening of Pb-8 levels in all
high-risk pregnant women.
Key initiatives recommended by the American Academy of Pediat-
rics (1987) should be adopted. These initiatives include
screening of every child in the United States at risk of expo-
sure to lead.
The report recommends a careful examination of the role of
improved nutrition in ameliorating lead toxicity.
Continuing large-scale assessments of lead burdens in children,
including further national surveys and more regionally focused
studies are required.
Continued support should be given to the highly productive
prospective epidemiological studies now under way and to the
development and refinement of metabolic models that are used to
examine the quantitative relationship between source-specific
lead exposure levels and the resulting lead levels in blood or
other body compartments.
ISSUES, DIRECTIONS, AND THE FUTURE OF THE LEAD PROBLEM
Issues
A number of key scientific issues concerning lead as a major health
problem are of special concern for the establishment of public health policy in
the United States. These issues include:
The Indestructibility of the Problem. As an element, inorganic
lead cannot be processed by current technology and destroyed.
It will continue to be a potential problem in some form forever.
The Relative Non-Transferability of the Problem. Lead cannot be
easily shifted from a hazardous setting to a nonhazardous
setting without some concomitant increased potential risk
elsewhere. Once removed from its geologically bound forms by
human activities, lead poses a toxic threat for which there are
no natural defense mechanisms.
The Environmental Accumulation Factor. Lead accumulates
indefinitely in the environment so long as input continues -- no
matter in how small a quantity.
The Human Body Accumulation Factor. The human body accumulates
lead over the individual's active lifetime and does so even with
"small" intakes from common sources. For hazards to exist,
major exposures at given points in time need not occur.
15
— . - -—
0 The Risk Population Accumulation Factor. Estimates of exposure
and toxicity based on data from particular points in time, such
as the estimates provided in this report, greatly understate the
cumulative risk for a population posed by a uniquely persistent
and pervasive pollutant such as lead. This cumulative toll over
extended time is of much greater magnitude, and hence concern,
than the prevalence or total exposure estimates for any given
year.
(a) An individual fetus is never counted more than once in any
survey examining populations. In the absence of effective
abatement of lead exposure, the estimate of 400,000 indivi-
dual fetuses at risk for lead toxicity in a single year
becomes 4 million individual fetuses in 10 years, or
20 million in 50 years, of lead exposure.
(b) Within a given time period, successive sets of preschool
children are likely to move into the same housing unit,
particularly in the case of deteriorated inner-city tenant
housing. Thus, the number of infants and toddlers at risk
for the exposure associated with such conditions (espe-
cially paint and dust/soil lead) is much greater than the
number of deteriorated houses. If one assumes 3 to 5 years
as the average period of residency, then perhaps 10 times
as many children would be exposed to such conditions over a
30- to 50-year period.
0 The Pervasiveness of the Problem. As a pervasive toxicant, lead
is shown in this report to affect totals of children that are
high in all socioeconomic/demographic strata. The U.S. lead
problem is not simply a problem of a generally neglected segment
of society. At present, little or no margin of safety exists
between existing Pb-B levels in large segments of the U.S.
population and those levels associated with toxicity risk.
4) Absence of a Truly Optimal Blood Lead Level. As a toxicant
serving no known physiological requirement, the presence of
lead at any level in the body is less than optimal. Current
average Pb-B levels in some U.S. population segments are 15- to
30-fold higher that the theoretical value of 0.5 g/dl calcu-
lated for early, pre-industrial humans.
2. Directions and Future of the Lead Problem
At the same time that progress is being made to reduce some sources of
lead toxicity, scientific determinations of what constitute "safe" levels of
lead exposure are concurrently declining even further. Thus, increasing
percentages of young children and pregnant women f211 into the "at-risk
category as permissible exposure limits are revised downward. Accompanying
these increases is the growing dilemma of how to deal effectively with such a
16
® s
widespread public health problem. Since hospitalization and medical treatment
of individuals with Pb-B levels below approximately 25 pg/dl is neither
appropriate nor even feasible, the only available option is to eliminate or
reduce the lead in the environment.
In large measure, the more tractable part of the lead abatement effort in
the United States is already underway, because the reduction of lead in
gasoline, food, and drinking water is amenable to centralized control
strategies. Lead in old paint, dust and soil, however, is pervasive and
dispersed, and fundamentally different approaches to abatement will be needed.
If the Nation is to solve these difficult facets of the lead problem, society
must make a strong effort to do so. Without this effort, large numbers of
young children in present and future generations will continue to be exposed to
persistent and massive sources of lead in their environment.
17
EXHIBIT B
Developed for the Risk Management Subcommittee, Committee
to Coordinate Environmental Health and Related Programs,
U.S. Department of Health and Human Services.
February 1991
LRVIC,
aes ts,
U.S. DEPARTMENT OF HEALTH
&
s
3 AND HUMAN SERVICES
iS Public Health Service
%, Centers for Disease Control
STRATEGIC PLAN FOR THE
ELIMINATION OF CHILDHOOD
LEAD POISONING
February 1991
STRATEGICPLAN FOR THE
ELIMINATION OF CHILDHOOD LEAD POISONING
TABLE OF CONTENTS
Preface ii Sh anna see a Ae EE Sti al ean x ne lls a ii
Authors, Contributors, Peer Reviewers, and Acknowledgements .............. iv
Executive SUMIMAIY. . i. eh tha ve sb vss pam cad tn ris yogis in ges Xi
Surnmary Of CHADIBIS seo uco i sive vas ss mrsesineiinbr rnd sinner. xiv
Chapter 1. Introduction: . 2- usin cctv vn vumarn et siownshac nr snan, 1
Chapter 2. Health Effects of Lead and Lead Exposure .................... 4
Chapter 3. Benefits of Preventing Lead Exposure of Children and Fetuses ...... 10
Chapter 4. ‘Program Agenda uc... occas vannergonsnnnsensvinssnn an 13
Chapter 'S. Research Agenda... ...ccouccntrravpriivacanvunrcnness 38
Chapter 6. Funds Needed for Implementation of the Strategic Plan ........... 45
Chapter 7. Summary of Recommendations ........c..cveeeinnnnee nn 52
THEIL Ul a UR DR ET RE eh lo 53
APPENDICES
I. Lead exposure and its effects on children and fetuses
11. Benefits of preventing lead exposure in the United States and costs and
benefits of lead-based paint abatement
I. History of childhood lead poisoning prevention programs
IV. Organizations and agencies that could help promote awareness of childhood
lead poisoning
v. Infrastructure development for abatement of lead hazards in housing
» »
PREFACE
Three striking conclusions about childhood lead poisoning have emerged in the past
several years: 1) the effects of exposure to even moderate amounts of lead are more
pervasive and long-lasting than previously thought, 2) significant impairment of
intelligence and neurobehavioral function is being reported at increasingly lower levels of
lead in blood, and 3) millions of children in the United States have blood lead levels in
this new range of concem. These findings have been reviewed in great detail elsewhere,
and they are summarized here. They are not, however, the main subject of this report.
The main subject is the public health response to our new understanding of childhood
lead poisoning.
In this report, we set forth a strategy for eliminating childhood lead poisoning as a public
health problem. Essential actions include increased support of programs that prevent
childhood lead poisoning, increased abatement of lead-based paint and paint-
contaminated dust in high-risk housing, reductions in other sources and pathways of lead
exposure in children, and national surveillance for children with elevated blood lead
levels. Finding and treating children with lead poisoning is critical, but not sufficient.
Preventive actions must be taken to remove sources of lead in the child's environment
before poisoning occurs.
Any plan to eliminate childhood lead poisoning in the United States must address the
formidable problems posed by lead-based paint. Lead-based paint abatement has been
neither widespread nor effective. Developing an effective, long-term lead-based paint
abatement effort is probably the most critical factor in eliminating childhood lead
poisoning. In this plan, approaches to developing this effort receive most attention.
From a national viewpoint, the relative contribution from different sources of lead for
children with high blood lead levels (that is, those with or likely to get lead poisoning) is
different from that for children with low or moderate blood lead levels. For children
with the highest blood lead levels, lead-based paint is a particularly important source.
Strategies will need to be developed to focus abatement efforts on the highest priority
groups (especially children with lead poisoning severe enough to require medical
intervention, e.g., blood lead levels > 25 ug/dL). Initial screening efforts will also have
to be focused on areas where there are the greatest numbers of children with the highest
blood lead levels (e.g., > 25 ug/dL).
This plan also calls for reducing lead in other major sources and pathways of exposure.
Ongoing regulatory and voluntary protective actions are important and must be
strengthened. Lead is widely distributed in water, food, and air, but this lead is less
likely to produce lead poisoning than lead in such concentrated sources as lead paint.
Reducing the amount of lead in these environmental media, however, can have a
profound effect on blood lead levels throughout the entire United States. This was
demonstrated when lead was removed from gasoline. Reducing the amount of lead in
water, food, and air would help reduce the prevalence of lead poisoning and would help
protect children with blood lead levels below the current definition of lead poisoning
from adverse effects.
The role of exposure to soil lead, both directly and through the contribution of soil lead
to lead in housedust, is still being investigated. The nature and degree of soil lead
abatement that would be appropriate is unclear. The research needed to resolve the soil
lead issues will take years. However, since so many children are being poisoned by
lead-based paint, significant action on lead-based paint abatement should not be delayed
while we await the results of research. Decisions on how to set up rational soil lead
abatement programs will have to be made separately as more data become available.
(However, it is critical not to further contaminate the soil during lead-based paint
abatement efforts.)
We have made substantial progress in reducing exposure to lead; deaths and severe
illness from lead poisoning (e.g., encephalopathy) are now rare. The results of recent
studies indicate, however, that blood lead levels previously believed to be safe are
adversely affecting the health of children. Millions of children in the United States are
believed to have blood lead levels high enough to affect intelligence and development.
The need to deal with preventing exposure at these lower levels will require increased
efforts. The Administration is responding to this problem with increased resources. In
FY 1992, the President’s budget calls for $14.95 million for the lead poisoning prevention
program at the Centers for Disease Control and $25 million for the new HOME
abatement program of the Department of Housing and Urban Development.
In many ways, the tone of this report is one of understatement. The enormity of the task
of eliminating childhood lead poisoning and the extensive public health benefits to be
gained are very clear. This strategic plan is at best a first step. More detailed plans for
implementation must follow, and then the work itself must be done.
Childhood lead poisoning has already affected millions of children, and it could affect
millions more. Its impact on children is real, however silently it damages their brains
and limits their abilities. Deciding to develop a strategic plan for the elimination of
childhood lead poisoning is a bold step, and achieving the goal would be a great
advance.
\ L »
AUTHORS, CONTRIBUTORS, PEER REVIEWERS, AND ACKNOWLEDGEMENTS
PRINCIPAL AUTHORS
Sue Binder, M.D.
Centers for Disease Control
Center for Environmental Health and Injury Control
1600 Clifton Road, NE
Atlanta, Georgia 30333
Henry Falk, M.D., M.P.H.
Centers for Disease Control
Center for Environmental Health and Injury Control
1600 Clifton Road, NE
Atlanta, Georgia 30333
CONTRIBUTORS
FEDERAL
Max Lum, E.D.
Agency for Toxic Substances and Disease Registry
Division of Health Education
1600 Clifton Road, NE
Atlanta, Georgia 30333
Susanne Simon
Agency for Toxic Substances and Disease Registry
Division of Health Education
1600 Clifton Road, NE
Atlanta, Georgia 30333
James L. Pirkle, M.D., Ph.D.
Centers for Disease Control
Center for Environmental Health and Injury Control
1600 Clifton Road, NE
Atlanta, Georgia 30333
Joel Schwartz, Ph.D.
Environmental Protection Agency
401 M Street, SW, PM-221
Washington, D.C. 20460
iv
£
{
{
CONTRIBUTORS (cont'd)
William McC. Hiscock
Health Care Financing Administration
Program Initiatives Branch
P.O. Box 26678
Baltimore, Maryland 21207
Jane Lin-Fu, M.D.
Health Resources and Services Administration
Maternal and Child Health Bureau
5600 Fishers Lane
Rockville, Maryland 20857
Donald T. Ryan
National Institute of Environmental Health Sciences
727 S. 26th Place
Arlington, Virginia 22202
STATE AND LOCAL
Charles G. Copley
Office of the Health Commissioner
City of St. Louis
Department of Health and Hospitals
634 N. Grand
St. Louis, Missouri 63178
PRIVATE SECTOR
Anne Elixhauser, Ph.D.
Human Affairs Research Center, Battelle
370 L'Enfant Promenade, SW, Suite 900
Washington, D.C. 20024-2115
Mark S. Kamlet, Ph.D.
Camegie Mellon University
Department of Social and Decision Sciences
Pittsburgh, Pennsylvania 15213
CONTRIBUTORS (cont'd)
Paul A. Locke, Esq.
Environmental Law Institute
1616 P Street, NW, Suite 200
Washington, DC 20036
Stephanie Pollack, Esq.
Conservation Law Foundation of New England
3 Joy Street
Boston, Massachusetts 02108-1497
PEER REVIEWERS
Anita S. Curran, M.D.
Robert Wood Johnson Medical School
University of Medicine and Dentistry of New Jersey
One Robert Wood Johnson Place
New Brunswick, New Jersey 08903
Richard J. Jackson, M.D.
Califomia Department of Health Services
Hazard Identification and Risk Assessment Branch
2151 Berkeley Way, Room 619
Berkeley, California 94704-1011
James C. Keck
Baltimore City Health Department
Lead Poisoning Prevention Program
303 East Fayette Street
Baltimore, Maryland 21202
John F. Rosen, M.D.
Albert Einstein College of Medicine
Montefiore Medical Center
111 East 210th Street
Bronx, New York 10467
i
£4
{
ACKNOWLEDGEMENTS
We appreciate the assistance of the following individuals who reviewed and commented
on drafts of this report:
FEDERAL
Vernon N. Houk, M.D.
Centers for Disease Control
Center for Environmental Health and Injury Control
1600 Clifton Road, NE
Atlanta, Georgia “30333
Robert W. Amler, M.D.
Agency for Toxic Substances and Disease Registry
1600 Clifton Road, NE
Atlanta, Georgia 30333
Elizabeth Cochran
Centers for Disease Control
Center for Environmental Health and Injury Control
1600 Clifton Road, NE
Atlanta, Georgia 30333
Gene Freund, M.D.
Centers for Disease Control
National Institute for Occupational Safety and Health
4676 Columbia Parkway
Cincinnati, Ohio 45226
Teri Guilmette
Centers for Disease Control
Center for Environmental Health and Injury Control
1600 Clifton Road, NE
Atlanta, Georgia 30333
Daniel A. Hoffman, Ph.D.
Centers for Disease Control
Center for Environmental Health and Injury Control
1600 Clifton Road, NE
Atlanta, Georgia 30333
vii
Robert S. Murphy, M.S.P.H.
Centers for Disease Control
National Center for Health Statistics
Hyattsville, Maryland 20782
Daniel C. Paschal. Ph.D.
Centers for Disease Control
Center for Environmental Health and Injury Control
1600 Clifton Road, NE
Atlanta, Georgia 30333
Jeffrey J. Sacks, M.D, M.P.H.
Centers for Disease Control
Center for Environmental Health and Injury Control
1600 Clifton Road, NE
Atlanta, Georgia 30333
Sandra C. Eberlee
Consumer Product Safety Commission
5401 Westbard Avenue
Bethesda, Maryland 20816
Brian C. Lee, Ph.D.
Consumer Product Safety Commission
5401 Westbard Avenue
Bethesda, Maryland 20816
Robert W. Elias, Ph.D.
U.S. Environmental Protection Agency
Office of Research and Development
Research Triangle Park, North Carolina 27711
Renate D. Kimbrough, M.D.
U.S. Environmental Protection Agency
Office of the Administrator
401 M Street, SE, A-101
Washington, DC 20460
Ronnie Levin
U.S. Environmental Protection Agency
Office of Research and Development
401 M Street, SE, H-8105
Washington, DC 20460
viii
® i»
Dave E. Schutz, M.S, M.P.P.
U.S. Environmental Protection Agency
Office of Toxic Substances
401 M Street, SE, TS-798
Washington, DC 20460
P. Michael Bolger, Ph.D., D.A.B.T.
U.S. Food and Drug Administration
Division of Toxicological Review and Evaluation
200 C Street, SW, HFF-156
Washington, DC 20204
Ellis Goldman, M.C.P.
U.S. Department of Housing and Urban Development
Office of Policy Development and Research
451 7th Street, SW
Washington, DC 20410
Ronald J. Morony, P.E.
U.S. Department of Housing and Urban Development
Office of Policy Development and Research
451 7th Street, SW
Washington, DC 20410
Steve Weitz, M.U.P.
U.S. Department of Housing and Urban Development
Office of Policy Development and Research
451 7th Street, SW
Washington, DC 20410
Kathryn MahafTey, Ph.D.
National Institute of Environmental Health Sciences
3223 Eden Avenue, Room 13
Cincinnati, Ohio 45267-0056
Mary McKnight
U.S. Department of Commerce
National Institute of Standards and Technology
Gaithersburg, Maryland 20899
STATE AND LOCAL
Mary Jean Brown
Massachusetts Department of Public Health
Childhood Lead Poisoning Prevention Program
State Laboratory Institute
305 South Street
Jamaica Plain, Massachusetts 02130
Mark Matulef, Ph.D.
Massachusetts Executive Office of Communities and Development
Office of Program and Policy Development
100 Cambridge Street
7
Boston, Massachusetts 02202 : : >
Lewis B. Prenney
Massachusetts Department of Public Health
Childhood Lead Poisoning Prevention Program
State Laboratory Institute
305 South Street
Jamaica Plain, Massachusetts 02130
PRIVATE SECTOR
- John B. Moran
Laborers’ National Health and Safety Fund
Occupational Safety and Health
905 16th Street, NW
Washington, DC 20006
Herbert L. Needleman, M.D.
University of Pittsburgh School of Medicine
3811 O'Hara Street
Pittsburgh, Pennsylvania 15213
Margery Turner
The Urban Institute
2100 M Street, NW
Washington, DC 20037
A ®
STRATEGIC PLAN FOR THE
ELIMINATION OF CHILDHOOD LEAD POISONING
EXECUTIVE SUMMARY
The U.S. Public Health Service Year 1990 and Year 2000 Objectives for the Nation aim
for progressive declines in the numbers of lead-poisoned children in the United States,
leading to the elimination of this disease. We believe that a concerted society-wide
effort could virtually eliminate this disease as a public health problem in 20 years.
This plan, developed for the Committee to Coordinate Environmental Health and
Related Programs of the U.S. Department of Health and Human Services, provides an
agenda for the first 5 years of a comprehensive society-wide effort to eliminate childhood
lead poisoning. The results and experience from this 5-year program will lead to the
agenda for the following 15 years.
Lead is a poison that affects virtually every system of the body. Results of recent studies
have shown that lead’s adverse effects on the fetus and child occur at blood lead levels
previously thought to be safe: in fact, if there is a threshold for the adverse effects of
lead on the young, it may be close to zero.
Lead poisoning remains the most common and societally devastating environmental
disease of young children. Enormous strides have been made in the past 5S to 10 years
that have increased our understanding of the damaging, long-term effects of lead on
children’s intelligence and behavior. Today in the United States, millions of children
from all geographic areas and socioeconomic strata have lead levels high enough to
cause adverse health effects. Poor, minority children in the inner cities, who are already
disadvantaged by inadequate nutrition and other factors, are particularly vulnerable to
this disease.
Childhood lead exposure costs the United States billions of dollars from medical and
special education costs for poisoned children, decreased future eamings, and mortality of
newborns from intrauterine exposure to lead. Childhood lead poisoning continues in our
society primarily because of lead exposure in the home environment, with lead-based
paint being the principal high-dose source. It is the most important source for the
highest-risk children (e.g., those with blood lead levels > 25 ug/dL); preventive actions
for such exposures should receive the highest priority.
xi
\
® »
Federal regulatory actions have significantly reduced or eliminated lead from many
consumer products, including new paint and gasoline. Federal agencies continue to take
actions further to reduce lead exposure from water, food, soil, air, and the workplace.
Unfortunately, we are making little progress in eliminating the major source of high-dose
lead poisoning, leaded paint from older housing.
In a new benefits analysis based on data from three studies, we estimate that the
abatement of lead from all pre-1950 housing containing lead-based paint over the next
20 years would result in societal benefits of $62 billion. This anticipated economic
benefit is an additional incentive to society, since even if no economic benefits of
abatement could be demonstrated, prevention of childhood lead poisoning would still be
a worthwhile public health activity. i.
This plan contains recommendations for program and research activities. * The four
immediately essential elements of this effort are:
1) Increased childhood lead poisoning prevention programs and activities.
2) Effective abatement of leaded paint and lead paint-contaminated dust in
high-risk housing.
3) Continued reduction of children’s exposure to lead in the environment,
particularly from water, food, air, soil, and the workplace.
4) Establishment of national surveillance for children with elevated blood lead
levels.
Increased childhood lead poisoning prevention activities and national surveillance for
elevated lead levels are essential parts of a national strategy to eliminate childhood lead
poisoning for several reasons. Children should be screened for elevated blood lead
levels so that affected children will receive appropriate medical attention and
environmental follow-up. Initially, screening activities must focus on those areas with the
greatest prevalence of children with the highest blood lead levels. Screening and
surveillance data are also important for defining those areas in greatest need of intensive
abatement programs and for evaluating the success of the national abatement program in
eliminating this disease in targeted areas.
Effective lead-based paint abatement is essential for the elimination of childhood lead
poisoning. Lead-based paint is the most concentrated source of lead to children and,
historically, is the source most closely linked to lead poisoning in children. Many sources
of lead, for example, food and soil, contribute to overall exposure of U.S. children to
lead, but for children with the highest blood lead levels, that is, children with lead
poisoning, lead-based paint is of particular importance.
i
: 3
The development of a national strategy to abate lead-based paint is critical to the success
of the effort to prevent lead poisoning. At present, far too few homes are being abated.
To achieve maximum impact in the shortest time, lead-based paint abatement programs
need to be closely linked with public health programs.
We recommend development of a national strategy for lead-based paint abatement that
includes actions by both the private and the public sectors. Since the public health
benefits and cost-effectiveness of lead-based paint and dust abatement are greatest in the
housing most likely to contribute to lead poisoning, in the early years the emphasis
should be on abating the housing units of affected children and the units likely to poison
children in the near future. |
To eliminate completely this disease, however, will require that all housing with
lead-based paint eventually be addressed. A prioritized program will allow the
highest-risk housing to be abated first, while enhanced programs, infrastructure, and :
technology continue to be developed. This national lead-based paint abatement program
must include an evaluation component to ensure efficacy and safety for occupants as well
as workers and their families.
This strategic plan focuses heavily on lead-based paint because of its key role in lead
poisoning and because of the limited nature of previous efforts to reduce this source of
lead. A national plan to eliminate childhood lead poisoning, however, must also focus
on other widespread sources and pathways of lead exposure to children. Lead in water,
food, soil, and air, in particular, may affect large numbers of children and may contribute
to overall levels of lead in the population. Continued efforts to reduce these sources and
pathways of lead exposure will result in lower average blood lead levels in the United
States and will thereby further diminish the likelihood of lead poisoning developing even
in children exposed to a high-dose source.
Childhood lead poisoning usually does not cause distinctive clinical symptoms, but the
effects of childhood lead poisoning on intellectual and neurobehavioral functioning are
pronounced and may persist for life. Furthermore, lead poisoning is entirely preventable.
We understand the causes of lead poisoning and, most importantdy, how to eliminate
them. This plan establishes priorities and identifies steps toward that end.
i i
S §
SUMMARY OF CHAPTERS
Chapter 1. Introduction
Lead poisoning, the most common and societally devastating environmental disease of
young children, is entirely preventable. We understand the causes of childhood lead
poisoning and, most importantly, how to eliminate them. A concerted societal effort
could virtually eliminate this disease in 20 years.
Chapter 2. Health Effects of Lead and Lead Exposure
L
I
Lead is a dangerous and pervasive environmental poison, particularly harmful to fetuses
and young children. The threshold for some of lead’s health effects may be close to
zero. The Agency for Toxic Substances and Disease Registry (ATSDR) estimated that
between 3 and 4 million children in the U.S. (17% of all children) had blood lead levels
above 15 ug/dL in 1984, levels high enough to adversely affect intelligence and behavior.
Lead in the home environment, principally from lead-based paint, is the major source of
lead poisoning. (See Appendix I for more details on the material in this chapter.)
Chapter 3. Benefits of Preventing Lead Exposure of Children and Fetuses |
A benefits analysis was performed for this report, taking into account recent data on the
effects of lead on children and fetuses. (In addition, an example of a cost-benefit
analysis of a national lead-based paint abatement program, along with the detailed
benefits analysis, appears in Appendix II) For this analysis, the benefits of preventing
children and fetuses from being exposed to lead are the costs that would have been
associated with exposure had it occurred. On the basis of this analysis, the average
benefits of preventing a child's blood lead level from exceeding 24 ug/dL (the level at
which medical evaluation is necessary) are $4,631 for avoided medical and special
education costs. For all children, including those with blood lead levels below 25 ug/dL,
the average increased wages to be expected from preventing each 1 ug/dL increase in a
child’s blood lead level are $1,147. The average benefits of preventing a 1 ug/dL
increase in the blood lead level of a pregnant woman are $300. Based on data from
three programs (see Appendix II), the benefits of abating all pre-1950 housing with
lead-based paint over a 20-year period would be $62 billion, discounted to the present.
Chapter 4. Program A end
The four essential program components of a strategy to eliminate childhood lead
poisoning are:
1) Increased childhood lead poisoning prevention programs and activities.
xiv
2) Increased abatement of leaded paint and paint-contaminated dust in housing.
3) Continued reduction of children's exposure to lead in the environment,
particularly from water, food, air, soil, and the workplace.
4) Establishment of national surveillance for children with elevated blood lead
levels.
Increased childhood lead poisoning prevention activities include both funding of public
lead poisoning prevention programs and increased awareness and action by private
physicians. Increased abatement should also result from a combination of efforts by the
private and public sectors. Before we can safely and effectively conduct as many
abatements as are needed, the infrastructure for abatement must be developed. :
(Appendix V discusses infrastructure development in more detail.) Other environmental \
sources of lead should also continue to be addressed as part of the strategic plan;
reductions of lead in water, food, soil, air, and the workplace are of most importance.
National surveillance for elevated blood lead levels is needed to target areas requiring ©
increased lead poisoning prevention activities and abatement, to track our progress in
eliminating childhood lead poisoning, and to evaluate lead exposure in abatement
workers and workers in other lead-contaminated environments.
Chapter 5. Research Agenda
Research activities to complement the four essential program components are described
in this chapter.
Chapter 6. Funds Needed for Implementation of the Strategic Plan
Significant Federal, State, local, and private resources must be committed to meet the 5-
year goals. Preliminary estimates indicate that as much as $974 million in combined
resources may be required to implement the first 5 years of this Strategic Plan.
Chapter 7. Summary of Recommendations
The five most urgent recommendations of this plan include increased prevention
activities, increased abatement, reduced exposure to other sources of environmental lead,
national surveillance, and research.
XV
DECLARATION OF DR. HERBERT L. NEEDLEMAN
I, Dr. Herbert L. Needleman, declare and say:
1. The facts set forth herein are personally known to me
and I have first hand knowledge of them. If called as a witness,
I could and would testify competently thereto under oath.
2. I am currently a Professor of Psychiatry and Pediatrics
at the University of Pittsburgh School of Medicine. I am a
member of the Institute of Medicine of the National Academy of
Sciences and the Committee on Environmental Hazards of the
American Academy of Pediatrics. I have served as a consultant to
the Environmental Protection Agency on the writing of the Air
Lead Criteria Document and the Water Lead Criteria Document. For
my research in low level lead toxicity, I have been awarded the
Sarah Poiley Medal of the New York Academy of Sciences and the
Charles A. Dana Award for Pioneering Achievement in Public
Health. During the past 20 years, I have conducted research,
written, and consulted extensively on matters relating to lead
poisoning, and I currently am a member of the Centers for Disease
Control’s ("CDC") Advisory Committee on Childhood Lead Poisoning
Prevention. A copy of my Curriculum Vitae is attached.
3. Childhood lead poisoning is the number one environmental
health hazard for children in the United States today. Although
all young children are at particular risk for lead poisoning due
to their developing neurological systems, poor and minority
children are disproportionately affected because they are more
likely to (1) live or visit in homes with peeling or chipping
p . § £
{ )
paint; (2) live or visit in homes built before 1950 with planned
or ongoing renovation; (3) have a brother, sister, or playmate
with confirmed lead poisoning; (4) live with an adult whose job
or hobby involves exposure to lead; or (5) live near industry
likely to release lead (e.g., a lead smelter, battery recycling
plant, ete,).
4. Recent studies of lead toxicity have both lowered the
perceived threshold for observed health effects and demonstrated
toxic effects in new areas. Epidemiological studies have now
shown IQ changes of four to seven points in children at blood
levels as low as 15ug/dL. When cumulative distributions are
compared, a six point shift in the median results in a four-fold
increase in the rate of severe IQ deficit (IQ less than 80). My
own studies have documented that children exposed to moderate
levels of lead in preschool years as indicated by tooth lead
levels were seven times more likely to fail to graduate from high
school and six times more likely to have a significant reading
disability than children who had lower lead exposure. In
addition, intrauterine and early infant exposure to lead at low
dose interferes with growth on the infant during the first year
of life. Blood lead levels are inversely correlated with linear
height and chest circumference. Hearing deficits have been
measured in association with blood lead levels; no threshold was
found.
5. I have studied the relationship between exposure to lead
at doses too small to produce clinical symptoms and the
development of the young child and infant. The work of my group
has shown that lead exposure in the absence of symptoms is
associated with lower IQ scores, impaired speech and language
function, and impaired classroom performance. Exposure during
pregnancy leads to lower IQ scores in childhood.
6. These studies draw a convincing picture of lead’s broad
impact on children’s intelligence, growth, ability to hear and
perceive language, and to focus, maintain, and shift attention.
They certify, to the satisfaction of all but representatives of
the lead industry, that lead is a potent, versatile, and widely
distributed toxicant. Lead poisoning produces hyperactivity and
aggression, and studies of low dose exposure show an increased
incidence of those behaviors subsumed under the attention deficit
syndrome. Attention deficit and learning disorders are well
established risk factors for antisocial behavior. Whether there
is a causal link between lead and delinquency has not been
subject to systematic study, but the clues are a subject for
troubled conjecture.
7. Because lead poisoning is frequently asymptomatic at the
early, preventable stages, the vast majority of lead poisoning
cases go undiagnosed and untreated. Consequently, monitoring of
blood lead levels of young children through periodic screening is
critical. Measuring blood lead content is the most accurate and
reliable method of screening for lead exposure. Although perhaps
more invasive than an oral assessment of history, blood testing
for other conditions (iron deficiency, anemia, etc.) is typically
part of a standard medical examination for children. More
important, blood lead level testing is essential to an adequate
lead screen because no oral assessment of risk factors is
foolproof. Periodic screening by blood lead measurement should
be conducted at least once per year for any poor or minority
child under the age of six because all such young children are at
risk for lead poisoning. For children considered to be at high
risk for lead exposure due to positive testing results or
environmental or other factors, blood lead testing should be
conducted every three to six months. A lead screening program
that failed to require such periodic lead blood testing would, in
my opinion, be both unsound and inadequate. The requirement that
all Medicaid eligible children ages 1-5 be tested for lead
poisoning is reasonable, medically appropriate, and an essential
part of even a minimally adequate and medically effective lead
screening program.
8. It is also economically sensible given the longterm
societal costs associated with failure to treat and prevent lead
poisoning. As the United States Department of Health and Human
Services recently recognized in its Strategic Plan For the
Elimination of Childhood Lead Poisoning (February 1991), lead
exposure in U.S. children is estimated to cost society billions
of dollars a year in medical care, special education and
institutionalization, and lost productivity and lifetime earnings
due to impaired cognition. By contrast, the estimated cost of
increased screening are minimal. According to HHS, the cost of
® Et
increased screening through EPSDT, WIC, and Head Start is only
$1.25 million over the next five years.
Executed at Pittsburgh, Pennsylvania this 2+ day of May
1991.
I declare under penalty of perjury that the foregoing is
Wook | Mandtontr,
true and correct.
DR. HERBERT L. NEEDLEMAN
CURRICULUM VITAE
Herbert L. Needleman, M.D.
Birthdate: December 13, 1927
Birthplace: Philadelphia, PA
Citizenship: U.5.A.
Social Security #:
Business Address: School of Medicine
University of Pittsburgh
Western Psychiatric Institute and Clinic
3811 O'Hara Street
Pittsburgh, PA 15213 (412) 624-0877
Home Address:
EDUCATION AND TRAINING
Undergraduate Muhlenberg College B.S.
Allentown, PA 1948
Graduate University of Pennsylvania M.D.
School of Medicine 1952
Philadelphia, PA
Post-Graduate
1952 - 1953 Philadelphia General Hospital
Philadelphia, PA
Intern
1953 - 1954 Children's Hospital of Philadelphia
Philadelphia, PA
National Heart Institute Research Fellow
1957 - 1958 Children's Hospital of Philadelphia
Philadelphia, PA
Resident in Pediatrics
1958 = 1959 Children's Hospital of Philadelphia
Philadelphia, Pennsylvania
Chief Resident in Pediatrics
1962 - 1965 Temple University Medical Center
Philadelphia, Pennsylvania
Resident in Psychiatry
1965 - 1967 Special Fellow in Psychiatry (NIMH)
APPOINTMENTS AND POSITIONS
Academic
1967 1971 Temple University Medical Center
Philadelphia, Pennsylvania
Assistant Professor of Psychiatry
' Harvard Medical School
Boston, Massachusetts
Assistant Professor of Psychiatry
Harvard Medical School
Boston, Massachusetts
Associate Professor of Psychiatry
University of Pittsburgh
School of Medicine
Pittsburgh, Pennsylvania
Associate Professor of Child Psychiatry
and Pediatrics
University of Pittsburgh
School of Medicine
Pittsburgh, Pennsylvania
Professor of Psychiatry
University of Pittsburgh
School of Medicine
Pittsburgh, Pennsylvania
Professor of Pediatrics
» ; »
Positions
1968 - 1971 Temple Community Mental Health Center
Philadelphia, Pennsylvania
Director of Consultation and Education
1871 = 1973 Massachusetts Mental Health Center
Boston, Massachusetts
Director, Mental Retardation Unit
1971 - 1981 The Children's Hospital Medical Center
Boston, Massachusetts
Associate in Psychiatry
1983 - 1987 Children's Hospital of Pittsburgh
Pittsburgh, Pennsylvania
Director, Behavioral Science Division
Non-Acadenic
1955 -57 Captain, U.S. Army
Fort George Meade, Maryland
CERTIFICATION AND LICENSURE
1959 American Board Certification in Pediatrics
1981 American Board Certification in Psychiatry
MEMBERSHIPS IN PROFESSIONAL AND SCIENTIFIC SOCIETIES
1970 - present American Association for the Advancement
of Science
1975 - present Ambulatory Pediatric Society
1976 - 1981 Governor's Advisory Board on Lead Paint
Poisoning
1981 - 1983 Society of Toxicology
1983 - present American Pediatric Society
1986 - present American Academy of Pediatrics - Fellow
1986 - present Sigma Xi
1948
1969
1982
1985
1987
1989
1990
1990
HONORS
Omicron Delta Kappa
B'nai B'rith Humanitarian of the Year
Award
First National Scientific Studies Award
Association for Children with Learning
Disabilities
The New York Academy of Sciences
The Sarah L. Poiley Memorial Award
Better Health and Living Magazine
Better Health and Living Award
The Charles A. Dana Award for Pioneering
Achievements in Health and
Higher Education
Phi Beta Kappa - Honorary Member
National Academy of Sciences, Institute of
Medicine
® : »
PUBLICATIONS
Refereed Articles
1. Needleman, H.L. and Horwitz, O. A comparative study of the
effects of three vasodilator drugs on the digital cutaneous blood
flow. American Journal of Medical Science 226:164, 1953.
2. Harris, T.N., Friedman, H.L., Saltzman, H.A., and Needleman,
H.L. Therapeutic effects of ACTH cortisone in rheumatic fever:
cardiologic observations in a controlled series of 100 cases.
Pediatrics 17:11, 1956.
3. Harris, T.N., Needleman, H.L., Harris, S. and Friedman, 8S.
Antistreptolysin and streptococcal anti-hyaluronidase titers in
sera of hormone-treated and control patients with acute rheumatic
fever. Pediatrics 17:29, 1956.
4. Harris, T.N. and Needleman, H.L. Study of cathode ray
oscillography of some innocent and pathologic cardiac murmurs of
children. American Heart Journal 52:889, 1955.
5. Harris, T.N., Saltzman, H.A., Needleman, H.L., and Lister, L.
Spectrographic comparison of ranges of vibration frequency among
some innocent cardiac murmurs in childhood and some murmurs of
valvular insufficiency. Pediatrics 19:57, 1957.
6. Needleman, H.L. and Root, A.W. Sex-linked hydrocephalus:
report of two families with chromosomal study of two cases.
Pediatrics 31:396, 1963.
7. Needleman, H.L. Tolerance and dependence in the planarian
after continuous exposure to morphine. Nature 215:784-785, 1967.
8. Needleman, H.L., Tuncay, 0.C., and Shapiro, I.M. Lead levels
in deciduous teeth of urban and suburban American children. Nature
235:111~-112, 19172.
9. Carroll, K.G., Needleman, H.L., Tuncay, 0.C., and Shapiro, I.M.
The distribution of lead in human deciduous teeth. Experientia
28:434-435, 1972.
10. Shapiro, I.M., Cohen, G.H., Needleman, H.L., and Tuncay, O.
The presence of lead in toothpaste. Journal of the American Dental
Association 86:394-395, 1972.
® : »
11. Shapiro, I.M., Needleman, H.L., and Tuncay, 0. The lead
content of human deciduous and permanent teeth. Environmental
Research 5:467-470, 1972.
12. Needleman, H.L. Lead poisoning in children: neurologic
implication of widespread clinical intoxication. Seminars in
Psychiatry 5:47-54, 1973.
13. Shapiro, 1.M., Dobkin, B., Tuncay, O., and. Needleman, H.L.
Lead levels in dentine of deciduous teeth of normal and
lead-poisoned children. Clinical Chemistry ACTA 46:119-123, 1973.
14. Needleman, H.L. and Shapiro, I.M. Dentine lead levels in
asymptomatic Philadelphia school children: subclinical exposure in
high and low risk groups. Environmental Health Perspectives 7:27,
1974.
15. Needleman, H.L., Sewell, E.M., Davidson, I., and Shapiro, I.M.
Lead exposure in Philadelphia school children: identification by
dentine lead analysis. New England Journal of Medicine
290:245-248, 1974.
16. Needleman, H.L. and Waber, D. Amitriptyline therapy in
patients with anorexia nervosa. Lancet 2:580, 1976.
17. Needleman, H.L. Exposure to lead: sources and effects.
New England Journal of Medicine 297:943-945, 1977.
18. Needleman, H.L., Gunnoe, C., Leviton, A., Reed, R., Peresie,
H., Maher, C., and Barrett, P. Deficits in psychological and
classroom performance in children with elevated dentine lead
levels. New England Journal of Medicine 300:689-695, 1979.
19. Needleman, H.L. Lead exposure and human health: recent data
on an ancient problem. Technology Review 82:38-45, 1980.
20. Needleman, H.L. and Bellinger, D. The epidemiology of low
level lead exposure in childhood. Journal of the American Academy
of Child Psychiatry 20:496-512, 1981.
21, Needleman, H.L. and Bellinger, D. Does lead at low dose
affect intelligence in children? Pediatrics 68:694-696, 1981.
22. Rabinowitz, M. and Needleman, H.L. Temporal trends in
umbilical cord blood lead levels. Science 216:1429-1431, 1982.
». ; »
23. Needleman, H.L., Leviton, A., and Bellinger, D. Lead-
associated neurological deficit. New England Journal of Medicine
306:367, 1982.
24. Needleman, H.L. The neuropsychological implications of low
level exposure to lead. Psychological Medicine 12(3):461-463,
1982.
25. Rabinowitz, M. and Needleman, H.L. Petrol lead sales and
umbilical cord blood lead levels in Boston, Massachusetts. Lancet
1:63, 1983.
26. Needleman, H.L. The neurobehavioral consequences of low level
lead exposure in childhood. Neurobehavioral Toxicology Teratology
4:729-732, 1982.
27. Bellinger, D. and Needleman, H.L. Lead and the relationship
between maternal and child intelligence. Journal of Pediatrics
102(4):523=527, 1983.
28. Needleman, H.L. Lead at low dose and the behavior of
children. Acta Psychiat Scand 67: (Suppl. 303):26-37, 1983.
29. Needleman, H.L., Rabinowitz, M., Leviton, A., Linn, S.,
Shoenbaum, S. The relationship between prenatal exposure to lead
and congenital anomalies. Journal of the American Medical
Association 22:2959, 1984.
30. Bellinger, D., Needleman, H.L., Bromfield, R., et al A
follow-up study of the academic attainment and classroom behavior
of children with elevated dentine lead levels. Biological Trace
Element Research 6:207-224, 1984.
31. Rabinowitz, M. and Needleman, H.L. Environmental,
demographic, and medical factors related to cord blood lead levels.
Biological Trace Element Research 6:57-67, 1984.
32. Rabinowitz, M., Leviton, A., Needleman, H.L. Variability of
blood lead concentrations during infancy. Arch. Environ. Health
39:74-77, 1984.
33. Bellinger, D., and Needleman, H.L., Leviton, A., et al Early
sensory-motor development and prenatal exposure to lead.
Neurobehavioral Toxicology and Teratology 6:387-402, 1984.
34. Rabinowitz, M., Leviton, A., and Needleman, H.L. Lead in milk
and infant blood, A dose response model. Arch. Environ. Health, 40
(5) :283-286, 1985.
35. Bellinger, D., leviton, A., Rabinowitz, M., Needleman, H.L.,
and Waternaux, C. Correlation of low level lead exposure in urban
children at two years of age. Pediatrics, 1985.
36. Needleman, H.L., Geiger, S.K., Frank, R. Lead and IQ scores:
A reanalysis. Science, 227:701-704, 1985.
37. Atkinson, S.E., Crocker, T.D., Needleman, H.L. The importance
of specification uncertainty and intolerance to measurement error
in a study of the impact of dentine lead on childrens' IQs.
International Journal of Environmental Studies, 29:127-138, 1986.
38. Bellinger, D., Leviton, A., Needleman, H.L., Waternaux, C.,
Rabinowitz, M. Low-level lead exposure and infant development in
the first year. Neurobehavorial Toxicology and Teratology, 8:151-
161, 1986
39. Bellinger, D., Leviton, A., Waternaux, C., Needleman, H.L.,
Rabinowitz, M. Longitudinal analyses of prenatal and postnatal
lead exposure and early cognitive development. New England Journal
of Medicine, 316:1037-1043, 1987.
40. Needleman, H.L. Low level lead exposure in the fetus and
young child. Neurotoxicology, 3: 389:394, 1987.
41. Needleman, BR.L. Introduction: Biomarkers in
neurodevelopmental toxicology. Environmental Health Perspectives,
74:149-152, 1987.
42. Needleman, H.L., Bellinger, D. Commentary: Recent
Developments. Environmental Research, 46:190-191, 1988.
43. Needleman, H.L. The persistent threat of lead: Medical and
sociological issues. Current Problems in Pediatrics. XVIII: 699-
744, 1988.
44. Needleman, H.L. The persistent threat of lead: A singular
opportunity. American Journal of Public Health, 79:643-645, 1989.
45. Needleman, H.L., Gatsonis, C.A. Low level lead exposure and
the IQ of children: A meta-analysis of modern studies. Journal
of the American Medical Association, 263:673-678, 1990.
46. Needleman, H.L., Schell, A., Bellinger, D., Leviton, A.,
Allred, E.N. Long term effects of childhood exposure to lead at
low dose; An eleven-year follow-up report. The New England Journal
of Medicine, 322:83-88, 1990.
* : *
PROCEEDINGS OF CONFERENCES, BOOKS, AND BOOK CHAPTERS
Y: Needleman, H.L. and Scanlon, J.W. Getting the lead
out. (editorial) New England Journal of Medicine 288:466-467, 1972.
2. Needleman, H.L. and Shapiro, I.M. Lead in deciduous teeth: A
marker of exposure in heretofore asymptomatic children. In D.
Barth, A. Berlin, R. Engel, P. Rect and J. Smeets (eds.),
Proceedings of International Symposium: Environmental Health
Aspects of lead. Luxembourg:Commission of European Communities,
1973, pp. 773-780.
3. Needleman, H.L. Lead poisoning in children: neurologic
implications of widespread clinical intoxication. In: Seminars in
Psychiatry 5:47-54, 1973.
4, Needleman, H.L. Lead-paint poisoning prevention: an
opportunity forfeited. (editorial) New England Journal of Medicine
292:588+589,-.1975.,
5. Needleman, H.L. Incidence and effects of low level lead
exposure. Proceedings of Symposium: International Conference on
Heavy Metals in the Environment, Toronto, Ontario, 1975.
6. Needleman, H.L. Low level lead exposure and neuropsychologic
function: Current status and future directions. Proceedings 4th
International Association for the Scientific Study of Mental
Deficiency. P. Mittler (ed.), 1976.
7. Needleman, H.L. and Waber, Deborah. The use of amitriptyline
in anorexia nervosa. In: Anorexia Nervosa, edited by R. Vigersky,
Raven Press, New York, 1977.
8. Needleman, H.L. Lead in the child's world: A model for action.
Proceedings 11th Annual Conference on Trace Substances in
Environmental Health, Columbia, Missouri, PP.
229~235,. 1977.
9. Needleman, H.L. Human lead exposure: Difficulties and
strategies in the assessment of neuropsychological impact. In:
Lead Toxicity, Singhal and Thomas (eds.), Urban and
Schwarzenburg, pp. 1-17, 1980.
10. Needleman, H.L. Lead and neuropsychological deficit: Finding
a threshold. In: Low Tevel Iead Exposure: The Clinical
Implications of Current Research. H. Needleman, (ed.) Raven Press,
New York, 1980.
® 10 »
1}. Averill, D.R. and Needleman, H.L. Neonatal lead exposure
retards cortical synaptogenesis in the rat. In: Low Level Lead
Exposure: The Clinical Implications of Current Research, H.
Needleman (ed.), Raven Press, New York, 1980.
12. Needleman, H.L. (Editor) Low Level Lead Exposure: TheClinical
Implication of Current Research, Raven Press, New York, 1980.
13. Needleman, H.L. Lead Poisoning. World Book Encyclopedia,
1980.
14. Needleman, H.L. and Landrigan, P.J. The health effects of low
level exposure to lead. Annual Review of Public Health 2:277-298,
1981.
15. Needleman, H.L. Why do patients with anorexia nervosa like to
cook? Speculations on reward behavior and hypothalamic
catecholamines. In: Textbook of Pediatric Nutrition, R. Suskind
(ed.), Raven Press, New York, 1981.
16. Needleman, H.L. Treatment of increased lead absorption and
acute lead poisoning. In: Current Pediatric Therapy, S. Gellis and
B. Kagan (eds.), 1981.
17. Needleman, H.L. Lead at low dose and the child's brain: Newer
data. In: Int. Conference on Heavy Metals in the Environment (WHO,
Ernst, ed.) CEP consultants, Edinburgh, 1982, pp. 549-552.
18. Bellinger, D. and Needleman, H.L. Low level lead exposure and
psychological deficit in children. Advances in Behavioral
Pediatrics 3:1-49, 1982.
19. Needleman, H.L. Lead Toxicity. Yearbook, Encyclopedia
Brittannica, 1982.
20. Needleman, H.L. Behavioral consequences of low level exposure
to lead. In: Biological Aspects of Metals and Metal-Related
Diseases, B. Sarkan (ed.), Raven Press, New York, 1983, pp.
219-224.
21. Needleman, H.L. Low level lead exposure and
neuropsychological performance. In: Lead Versus Health, M. Rutter
and R. Russell Jones, (eds.), John Wiley, New York, 1983, pp.
229-247.
® 11 J
32. Needleman, H.L. and Bellinger, D.B. The developmental
consequences of childhood exposure to lead. In: Advances in
Clinical child Psychology, B. Lahey and A. Kazdin (eds.), Plenum
Press, 1984.
23. Needleman, H.L. The hazard to health of lead exposure at
low dose. In: Changing Biogeochemical Cycles of Metals and
Human Health, Dahlem Konferenzen, Berlin, Germany, 1984.
24. Needleman, H.L. Neurotoxins: an ignored source of perturbed
development. In: Middle Childhood: Development and Dysfunction, M.
Levine and P. Satz (eds.), University Park Press, 1984.
25. Needleman, H.L. Lead: Nervous system effects.
In: Encyclopedia of Neuroscience, G. Adelman (ed.), Birkhauser
Boston, Inc., 1987. ;
26. Needleman, H.L. Prenatal exposure to pollutants and neural
development. In: Learning Disabilities and Prenatal Risk, M. Lewis
(ed.), University of Illinois Press, 1985.
27. Needleman, H.L. Methodologic and epistemologic issues in the
study of human health effects of low dose pollutants. Proceedings
4th International Conference on Neurotoxicology of Selected
Chemicals, NeuroToxicology, Vol. 4 (3):121-133, Intox Press, Little
Rock, 1983.
28. Needleman, H.L. The prevention of mental retardation and
learning disabilities due to lead exposure. In: The Handbook of
Prevention of Mental Retardation and Learning Disability, R.I.
Jahiel (ed.), 1985.
29. Needleman, H.L. Anorexia nervosa: Nutritional, pathogenic,
and therapeutic considerations. In: The Theory and Practice of
Nutrition in Pediatrics, R. Grand and J. Sutphen (eds.)
Butterworth's, pp. 645-650, 1985.
30. Needleman, H.L. Neurobehavioral effects of low level exposure
in childhood. International Journal of Mental Health, Vol. 14, No.
3, PP. 64-77, 1985.
31. Bellinger, D.C. and Needleman, H.L. Prenatal and early
postnatal exposure to lead: Developmental effects, correlates, and
implications. International Journal of Mental Health. Vol. 14, No.
3, pp. 78-111, 1985.
32. Needleman, H.L. and Landrigan, P. (Eds.) Psychiatric aspects
of pollutant exposure. Special issue: International Journal of
Mental Health, 1985.
33. Needleman, H.L. Exposure to lead at low dose in early
childhood and before birth. In: Developmental Behavioral
Pharmacology, Vol. 5. N.A. Krasnegor, D.B. Gray, and T. Thompson
(Eds.), L. Erlbaum Assoc., pp. 168-180, 1986.
34. Bellinger, D., Leviton, A., Waternaux, C., Needleman, H.L.,
Rabinowitz, M. Low-level lead exposure and early development in
socioeconomically-advantaged urban infants. Proceedings of the
International Workshop on Effects of Lead Exposure on
Neurobehavioral Development, Edinburgh, Scotland, 1986.
35. Needleman, H.L, Bellinger, D. Type II fallacies in the study
of childhood exposure to lead at low dose: A critical and
quantitative review. Proceedings of the International Workshop on
the Effects of Lead Exposure on Neurobehavioral Development,
Edinburgh, Scotland, 1986, pp 293-304.
36. Needleman, H.L. Low Level Lead Exposure in the Fetus and
Young Child. Proceedings on the Metals, Trace Elements and
Mammalian Development Conference. The University of Sydney Birth
Defects Foundation and Division of Human Nutrition, Sydney
Australia, 1986.
37. Needleman, H.L. Low Level Exposure and Children's
Intelligence: A Quantitative and Critical Review of Modern Studies.
(Plenary Address) International Conference Heavy Metals in the
Environment. New Orleans, 1987.
38. Needleman, H.L. Why we should worry about lead poisoning.
Contemporary Pediatrics, 5:34-56, 1988.
39. Needleman, H.L. The neurotoxic, teratogenic and behavioral
teratogenic effects of lead at low dose: A paradigm for
transplacental toxicants. In: Transplacental Effects on Fetal
Health: Progress in Clinical and Bilogical Research. Vol 281.
Editors: D.G. Scarpelli and G. Migaki. Publisher: Alan Liss, Inc.,
New York, 1988.
40. Needleman, H.L. Environmental Health Perspectives. The future
challenge of lead toxicity. Presented at NIEHS Conference
"Advances in Lead Research: Implications for Environmental Health."
86:85-89, 1989,
. 13 »
41. Needleman, H.L. Environmental Health Perspectives.
Strategies for Epidemiological Studies: General Population and
Pediatrics. Presented at "Lead in Bone: Implications for Dosimetry
and Toxicology" - Columbia, Md. 1989 (in press).
42. Needleman, H.L. Environmental Health Perspectives. What can
the study of lead teach us about other toxicants? 86:183-189.
43. Needleman, H.L. Low Level Lead Exposure: A continuing
problem. Pediatric Annals. 19:208-214, 1990.
44. Needleman, H.L. and Bellinger, D. The Health Effects of Low
Level Exposure to Lead. Annual Review of Public Health. 1990 (in
press).
45. Needleman, H.L. The behavioral and teratogenic properties of
lead at low dose: Recent evidence and some methodological issues.
In Global Perspectives on Lead, Mercury and Cadmium Cycling in the
Environment. Edited by T.C. Hutchinson and C.S. Gordon, and K.M.
Meema. Presented at SCOPE Metals Cycling Workshop, New Delhi,
India, 1987; Institute for Environmental Studies. Wiley Eastern,
New Delhi (in press).
“ 14
RESEARCH
Grants Received
Principal Investigator
EPA DU 73B43X 6/25/73 8/24/74
EPA 68-02-2217 6/26/76 9/30/79
NICHD HD 08945 12/01/75 11/08/82
EPA CR-810937-01-0 9/01/83 8/31/86
EPA CR-811041-01-0 8/01/83 1/31/88
NIEHS ES-04095-01A1 3/1/87 2/28/90
NIEHS ES-05015-01A1 4/1/90 3/31/94
Grant Foundation 1988-1992
Major Research Seminars and Lectureships
Amsterdam 1972: International Symposium on Lead in the Environment
(WHO, CEC), "Lead in Deciduous Teeth"
Research Triangle Park, North Carolina 1972: NIEHS Meeting on
Health Effects of Lead, "A New Marker of Lead Exposure"
Paris 1974: International Symposium on Heavy Metals in the
Environment (WHO), "Prevalence of Lead Exposure in 761 Asymptomatic
School Children"
Toronto 1975: International Conference on Heavy Metals in the
Environment (Conference Chairman), "Incidence and Effects of Low
Level Lead and Mental Retardation"
washington, DC 1976: International Association for the Scientific
Study of Mental Deficiency (Conference Chairman) "Low Level Lead
and Mental Retardation"
Washington, DC 1976: NIH Symposium on Anorexia Nervosa,
"Amitriptyline in the Treatment of Anorexia Nervosa"
Columbia, Missouri 1977: 11th Annual Meeting of Trace Metals in
the Environment (Keynote Speaker), "Incidence and Effects of
Exposure to Lead"
Washington, DC 1978: National Academy of Science/National Research
Council, Workshop on Lead in the Human Environment Plenary Session,
"Lead in Childhood"
Baltimore, Maryland 1978: Johns Hopkins University, Department of
Psychiatry Grand Rounds, "Incidence and Effects of Exposure to
Lead"
Providence, Rhode Island 1978: University of Rhode Island School
of Medicine, Department of Pediatrics Grand Rounds, "Studies in Low
Level Lead Exposure"
Boston, Massachusetts 1978: Boston City Hospital, Department of
Pediatrics Grand Rounds, "Studies in Low Level Lead Exposure"
Aspen, Colorado 1978: Toxicology Forum, "Clinical Studies of
Behavioral Effects of Environmental Pollutants"
New York City 1978: Society for Pediatric Research,
"Neuropsychologic Effects of Low Level Lead Exposure"
San Antonio 1979: Regional Center for Disease Control Meeting,
"Studies in Low Level Level Lead Exposure"
Detroit, Michigan 1979: Regional CDC Meeting, "Studies in Low
Level Lead Exposure"
Atlanta, Georgia 1979: American Academy of Child Psychiatry,
Symposium on Epidemiology, "The Epidemiology of Low Level Lead
Exposure in Childhood"
London, England 1979: Conservation Society Symposium, "Lead at Low
Dose and the Child's Brain"
Glasgow, Scotland 1979: University of Glasgow, Department of
Medicine Grand Rounds, "Lead at Low Dose and the Child's Brain"
New York City 1980: New York University School of Medicine,
Invited Lecture, "The Epidemiologic Approach to Lead Exposure"
Baltimore, 1980: Johns Hopkins University School of Public Health,
"Neurotoxicology of Lead In Childhood"
St. Louis, Missouri 1980: Regional CDC Meeting, "Studies in Low
Level Lead Exposure"
Boston, Massachusetts 1980: Harvard School of Public Health,
"Neurotoxicology of Lead"
Cleveland, Ohio 1980: Regional CDC Meeting, "Studies in Low Level
Lead Exposure"
Columbia, South Carolina 1980: South Carolina Department of Health
Seminar, "Low Level Lead Exposure"
® 16 »
Toronto, Canada 1981: American Association for the Advancement of
Science Annual Meeting, Symposium on Lead in the Environment,
"Neurotoxicity of Lead at Low Dose"
Stockholm, Sweden 1981: Third World Congress of Biological
Psychiatry, Lead at Low Dose and the Behavior of Children,
Chairman, Plenary Session, "Environmental Exposure to Neurotoxic
Agents and Psychiatric Disease - A New Problem"
Amsterdam 1981: International Conference on Heavy Metals in the
Environment, "Lead at Low Dose and the Child's Brain: Newer Data"
Toronto, Canada 1981: International Symposium on Biological
Aspects of Metals and Metal-Related Diseases, "Brain Effects of
Lead at Low Dose"
Pittsburgh, Pennsylvania 1981: Second Annual Public Health
Conference, Allegheny County Health Department and University of
Pittsburgh School of Public Health, "Behavioral Toxicology"
Los Angeles 1981: American Public Health Association,
"Epidemiological and Toxicological Approaches to Lead in the
Atmosphere"
Washington, DC 1981: Children's Hospital National Medical Center,
"Sources and Effects of Lead"
Washington, DC 1981: Grand Rounds at Howard University Hospital,
"Neurobehavioral Effects of Lead"
Tarpon Springs, Florida 1981: Ross Laboratories Symposium, "Brain
Effects of Environmental Pollutants"
New York City 1982: New York University School of Medicine,
"Neuroepidemiology of Lead"
New Orleans, Louisiana 1982: Johnson and Johnson Symposium on
Middle Childhood, "Environmental Toxins and their Impact"
Chicago, Illinois 1982: 19th International Conference of the
Association for Children and Adults with Learning Disabilities,
Neuroscience Workshop, "Relationships of Low Lead Exposure to
Academic Performance and Behavior"
Dusseldorf, Germany 1982: First World Congress of International
Brain Research Organization, Satellite Symposium on Environmental
Neurotoxicology, "Low Level Lead Exposure, Psychological, EEG,
and Behavioral Functioning in Childhood"
N 17 »
Pittsburgh, Pennsylvania 1982: Third Annual Symposium on
Environmental Epidemiology, "Neurobehavioral Effects of Low Level
Exposure to Toxic Agents"
London, England 1982: International Symposium on Low Level Lead
Exposure and Human Health, "Neurobehavioral Consequences of Low
Level Exposure to Lead"
London, England 1982: Grand Rounds Institute of Psychiatry,
University of London, "Lead in Psychiatry."
Television Appearance, May 1982: NBC Magazine
Washington, DC 1983: Association for Children with Learning
Disabilities, "Prenatal Exposure to Environmental Pollutants"
Montreal, Canada 1983: Canadian Association for Children with
Learning Disabilities, "Lead and Learning Disabilities"
Berlin, Germany 1983: Dahlem Conference, "Biogeochemistry of
Metals"
Detroit, Michigan 1983: Society for Research in Child Development,
"Prenatal Lead Exposure"
Brussells, Belgium 1983: Agglomeration de Bruxelle, Symposium on
Low Level Lead Exposure"
Brussells, Belgium 1983: Bureau Europeen des Unions de
Consommateurs, "The Rationale for Removing Lead from Petrol"
Gif Sur Yvette, France 1983: Centre Nationale de la Reserche
Scientifique, "Geochemistry and Health"
Washington, DC 1983: Society for Pediatric Research, "The Risk of
Congenital Anomalies in Relation to Umbilical Cord Blood Lead
Levels"
Washington, DC 1983: Society for Pediatric Research, "Umbilical-
cord Blood Lead Levels and Neuropsychological Performance at 12
Months of Age"
New York City 1984: Institute of Environmental Medicine, New York
University Medical Center, "The Epidemiology of Lead Poisoning in
Children"
Research Triangle Park, North Carolina 1984: CASAC, "Air Quality
Criteria Draft for Lead"
® 18 ®
Harrisburg, Pennsylvania 1984: Commonwealth of Pennsylvania,
Department of Health, Public Health Seminar
Charleston, South Carolina 1984: Medical University of South
Carolina, Televised Grand Rounds Presentation, "Recent Data on Low
Dose Lead Exposure and Brain Function"
Toronto, Canada 1984: Behavioral Toxicology Society, "Lead at Low
Dose and the Brain of Children and Infants: Historical,
Epidemiological, and Behavioral Data"
Washington, D.C. 1984: Institute of Medicine/National Research
Council, "Review of Methodologies for Assessing Low Level Lead
Health Effects and Their Implications for Prevention."
Toronto, Canada 1985: The Royal Society of Canada, Commission on
Lead in The Environment, "The Health Effects of Low Lead Exposure
to Lead"
Little Rock, Arkansas 1985: Fourth International Neurotoxicology
Conference, "Methodologic and Epistemologic Issues in the Study of
Human Health Effects of Low Dose Pollutants." Keynote address
Washington, D.C. 1985: American Public Health Association. (Chair)
Section on Psychiatric Implications of Environmental Pollutants
Columbus, Ohio 1986: Children's Hospital/Ohio State University,
Department of Pediatrics, Samuel Edelman/Bertha Johnson Visiting
Professor Lecture Series
New York City 1986: Institute of Environmental Medicine, New York
University Medical Center, "The Epidemiology of Lead Poisoning in
Children"
New York City 1986: Association for Children and Adults with
Learning Disabilities, ACLD International Conference, "Lead As A
Paradigm for Behavioral Teratogens"
Orlando, Florida 1986: American Academy of Pediatrics, "Lead:
Effects on Early Central Nervous System Development" (Plenary
Session)
Erie, Pennsylvania 1986: Saint Vincent Family Practice Residency
Program, "Effects of Low Level Lead Exposure on Children's Brains
and Behavior"
# 5 »
Edinburgh, Scotland 1986: U.S.E.P.A. and The Commission of the European Communities. International Workshop on the Effects of Lead Exposure on Neurobehavioral Development.
Sydney, Australia 1986: Metals, Trace Elements and Mammalian Development Conference. The University of Sydney Birth Defects Foundation and Commonwealth Scientific and Industrial Research Organisation (C.S.I.R.O.).
Pittsburgh, Pennsylvania, 1987: International Symposium on Epidemiology in Environmental Health.
San Francisco, California, 1987: Health Officers Association of California. Conference, "Preventing Lead Poisoning in Children".
New Orleans, La, 1987: 6th Int Conf Heavy Metals in the Environment. Plenary Address.
Bethesda, Md, 1987 Symposium on Transplacental Effects on Fetal Health.
Boston, Mass., 1987: Health Effects Institute. Conference, "Lessons from the Lead Story for the Study of Neurotoxins".
Research Triangle Park, North Carolina, 1988. NIEHS: Conference on Environmental Health in the 21st Century. Address: What can the study of lead teach us about other toxicants?
Helsinki, Finland, 1988. Speaker at Conference on Reproductive Health and Occupation.
Copenhagen, Denmark, 1988. World Health Organization. Speaker at Conference of: Euro Scientific Society and the Danish Society for Occupational Medicine and the Danish Society for Environ- Environ and Social Medicine.
Health and Environment Electronic Seminar, 1988. Association of State and Territorial Health Risk Assessors (ASTHRA) . Address: Low level lead exposure and children's health.
by 20 »
Washington, . D.C., 1988. Third International Symposium on
Neurobehavioral Methods in Occupational and Environmental Health.
Agency for Toxic Substances and Disease Registry and the Pan
American Health Organization. Address: Lessons from the history of
childhood plumbism for pediatric neurotoxicology.
Research Triangle Park, N.C., 1989. National Institute of
Environmental Health Sciences. Conference: Advances in Lead
Research; Implications for Environmental Health. Address: The
Future Challenge of Lead Toxicity.
Columbia, MD, 1989. International Workshop - Lead in Bone:
Implications for Dosimetry and Toxicology. Address: Strategies for
Epidemiological Studies - General Population, Pediatrics.
Washington, DC, 1989. American Pediatric Society and the Society
for Pediatric Research. 1989 Annual Meeting. Presentation: Long
Term Effects of Low-Level Lead Exposure: Ten-Year Follow-up.
Athens, Greece, 1989. International Symposium: Health -
Environment and Lead. Address: An Overview of Lead Effects on
Health.
Baltimore, MD, 1990. Johns Hopkins University. Pediatric Grand
Rounds. Lecture: Long-Term Health Effects of Childhood Lead
Poisoning: A Summary of Current Research.
Baltimore, MD, 1990. National Health/Education Consortium,
National Commission to Prevent Infant Mortality. Presentation:
Lead at Low Dose and Academic Failure.
Atlanta, GA, 1990. ATSDR - National Minority Health Conference.
Focus on Environmental Contamination.
Editor:
Referee:
® nl "
Research Related Activities
CDC publication, Preventing Childhood Lead
Poisoning, 1978
Science, New England Journal of Medicine, PNAS,
Pediatrics, Journal of Pediatrics, Journal of
Speech and Language, Environmental Research, Journal of
Developmental and Behavioral Pediatrics, Early Human
Development, American Journal of Industrial Medicine,
American Journal of Epidemiology, Clinical Psychology
Review
Extramural Grant Reviewing:
Chairman:
NIEHS site visitor (4 occasions)
March of Dimes
Canadian Department of Environment
National Health and Medical Research Council,
Australia
Developmental Toxicology Subpanel, 1986
National Research Council, National
Academy of Sciences Committe on
Biological Markers, Panel on
Reproductive and Reproductive and
Developmental Toxicology
p 22
Program Committee:
Institute for Environmental Studies
SCOPE Metals Conference, New Delhi, India, 1987
Natural Resources Defense Council -
Committee: Mothers and Others for Pesticide Limits
Technical Committee:
Member:
Member:
Member:
Member:
Sixth International Conference on Heavy Metals
New Orleans, 1987
National Advisory Committee
Center for Developmental Disabilities
University of Minnesota, 1986
Committee on Environmental Hazards
American Academy of Pediatrics, 1986
Editorial Board, Environmental Research, 1987
Advisory Committee on Childhood Lead
Poisoning Prevention
Centers for Disease Control, 1990
Testimony
Washington, DC 1974: Senate Subcommittee on Environmental
Pollution (Senator Joseph Biden)
Hartford, Connecticut 1974: State Department of Health, "Effects
of Lead in the Environment"
Sacramento, California 1975: State Air Resources Board
Washington, DC 1975: Senate Health Subcommittee (Senator
Edward Kennedy)
Washington, DC 1979: House Subcommittee on Health and the
Environment (Hon. Henry Waxman)
Washington, DC 1982: Environmental Protection Agency
Washington, DC 1982: House Subcommittee on Health and the
Environment (Representative Moffett)
Washington, DC 1984: Senate Committee on Environment and Public
Works (Senator Dave Durenberger)
Chicago, Illinois 1984: City Council, City of Chicago
Washington, DC 1987: House Subcommittee on Health and the
Environment (Hon. Henry Waxman)
Washington, DC 1990: U.S. Senate, Subcommittee on Toxic Substances,
Environmental Oversight, Research and Development of the
Environment, and Public Works Committee on Lead and its Effect on
Children's Health (Senator Lieberman). March, 1990; June, 1990.
Washington, D.C. House of Representatives, Select Committee on
Children, Youth, and Families. September, 1990.
Na 24 »
Consultant
U.S.E.P.A. - 1977 - Air Lead Criteria Document
U.S.E.P.A. - 1978 - Water Lead Criteria Document
U.S.E.P.A. - 1982 - Air Lead Criteria Document
Center for Disease Control - 1977 - Chairman, Ad Hoc Task Force on
Lead Poisoning Prevention
Science Advisory Board, Citizens for a Better Environment
London, 1982 =~ Temporary Advisor, World Health Organization
Planning Group to Design a European Study of Lead Neurotoxicity in
Childhood
Center for Disease Control, 1984. Ad Hoc Task Force on Lead
Poisoning Prevention
Center for Science in the Public Interest, 1986. Science Advisory
Board.
Natural Resources Defense Council, 1989. Committee: Mothers and
Others for Pesticide Limits.
R 25 »
Service
Residency Education Committee - Western Psychiatric
Institute and Clinic, Pittsburgh
Clinical Research Center Committee =- Children's Hospital of
Pittsburgh
Human Rights Committee - Children's Hospital of Pittsburgh
Executive Committee - Children's Hospital of Pittsburgh
Research Advisory Committee - Children's Hospital of Pittsburgh
Chairmanship Search Committee-Department of Pediatric Dentistry,
University of Pittsburgh
Education Executive Committee - Western Psychiatric Institute and
Clinic, Pittsburgh
Academic Promotions Committee ~- Western Psychiatric Institute and
Clinic, Pittsburgh
Massachusetts Governor's Advisory Board, 1978-1981
Environmental Defense Fund, Washington, D.C. - National Advisory
Committee on Children's Health and Toxins.
American Academy of Pediatrics - Committee on Environmental Hazards
Community Activities
Member, Board of Directors, Massachusetts Advocacy Center 1977-1981
Special Recognition
Keynote Speaker: Fourth International Neurotoxicology Conference,
Little Rock, Arkansas, 1985
Keynote Speaker: University of Sydney Birth Defects Foundation,
Commonwealth Scientific and Industrial Research Organization,
Sydney Australia, 1986.
EXHIBIT C
(a
MENCY
PETE WILSON, Gowrmor
[|
< - HE
||
=
IQ
a
n
>
ii
= ? < »
k
|»
ar = »
|
Z oO £ ~
~
o » w
714/744 P STREET
P.O. BOX 942732
SACRAMENTO, CA 942347320
(916) 445-1248
March 12, 1991
CHDP Provider Information Notice {91-6
To: CHDP Providers
Subject: Lead Poisoning in Children
1]
Lead poisoning is the most significant environmental health problem facing
California children today, and insufficient consideration is being given to
this potential problem during routine child health evaluations.
Epidemiologic evidence indicates that lead-induced neurological impairments
occur at very low exposure levels and that lead-related subclinical
neurological problems and learning impairments constitute a substantial cost
to society. Most children with lead poisoning are asymptomatic. In the near
future, the Centers for Disease Control (CDC) is expected to lower their
definition of lead poisoning from 25 micrograms per deciliter (mcg/dl) to 10
or 15 mcg/dl in children, reflecting their greater concern over low level
exposure.
Please take a few minutes to read the enclosed article, "Children and lead: a
statewide concern" that has been published in California Physician stressing
the importance of awareness of the problem and the need for testing. Lead
toxicity must be considered in children who are anemic, have an elevated
erythrocyte protoporphyrin (EP) level, have learning or behavioral problems,
and who reside in older homes possibly containing lead-based paint or who live
near environmental sources of lead such as battery manufacturing plants or
lead smelters.
The Child Health and Disability Prevention (CHDP) Program reimburses both the
erythrocyte protoporphyrin (EP) and blood lead tests. In addition, California
Children Services (CCS) covers diagnostic evaluations for possible lead
poisoning without regard to income eligibility. CCS also will provide for
treatment costs, if required, for children whose state adjusted gross annual
family income is less than $40,000.
Please feel free to call your local CHDP program director if you have any
questions.
Kenneth W. Kizer, M.D., M.P.H.
Director
Enclosure
Pras ¥r ay Ho oy NwITH
ph ie JR Els help ¢
with ils Childhood Le
‘Prevention Progra
SO CALIFORNIA PHYSICIAN / March 1991
ccupational lead poisoning has
been recognized for more than
2,000 years, but historically,
relatively little attention has
been directed to childhood lead expo
sure. In the early 1980s, however, epi-
demiologic evidence suggesting
lead-induced neurological impairments
at very low exposure levels began
accumulating. Now, a solid database
shows that children are considerably
more susceptible to lead poisoning
than adults and that lead-related neuro
logical problems and learning impair-
ments constitute a substantial cost to
society. California physicians should
be aware of this potential problem and
order relevant tests more frequently.
Beginning in 1985, the California
Department of Health Services (DHS)
directed attention to the potential lead
problem. The Department found that
essentially no routine childhood
screening for lead had been conducted
in California since the late 1970s, and
that past screening efforts focused on
higher blood lead concentrations than
are of concern today.
Mostly conducted in clinic and
school settings, previous lead-poison-
ing screenings did not provide statistics
about California's population as a whole
or information about which groups of
children might be particularly at risk.
Consequently, there was no way to
know the problem's extent and seventy
among California's children or to pro-
ject the costs and benefits of conduct:
ing screening and environmental
abatement programs. Because of these
limitations, prior to embarking on a
costly and possibly inefficient program,
DHS sought legislation to establish a
program of surveillance and targeted
epidemiological investigation of child-
hood lead exposure in California.
In late 1986, California's Childhood
Lead Poisoning Prevention Act was
enacted and authorized DHS to:
o Establish a laboratory-based report
ing system to identify childhood lead-
poisoning cases
* Require laboratories performing
blood lead tests to participate in a rec-
ognized proficiency testing program
* Conduct population-based studies of
childhood lead exposure in three high-
risk areas in the state in order to est-
mate the problem's extent and severity
¢ Report the study findings to the
Legislature, along with recommenda-
tions for further activities
Laboratory-based reporting
In order to estimate the extent of
California physicians’ lead-screening
efforts, and analyze the results of such
screening, DHS initiated a laboratory-
based lead poisoning reporting system
in April 1987. Through this system,
March 1991 / CALIFORNIA PHYSICIAN 51
-
laboratones are required to i
blood lead levels greater than 24
micrograms per deciliter (mcg/dl), as
well as all erythrocyte protoporphyrin
(EP) levels greater than 34 mcg/dl
whole blood.
Laboratories are required to
report elevated lead and EP levels to
both DHS and the local health depart-
ment The latter is to encourage fol
low-up in a timely manner by local
public health officials. However, physi
cians who suspect lead poisoning and
need assistance should not rely solely
on the reporting system to inform pub-
lic health officials, as laboratories are,
sometimes, slow to file reports.
Between April 1987 and October
1989. the DHS lead-reporting system
received 1,509 reports of potential
lead toxicity in persons younger than
17 vears of age. This number was
substantally less than expected, even
when using very modest estimates of
childhood lead poisoning for the state
as a whole.
Initial analyses of the laboratory
reports seemed to indicate that the
state had at least one “hot spot” for
However, upon investigation, it was
found that this was a clinic that had a
very comprehensive screening plan
- ee EY ‘ - TRE I Ee iy a
a
CIAN March |
lead exposure—in Santa Clara County.
for children entering the refugee
health program. That is. what
appeared to be a particular problem
was, in fact, pnmanily a reflection of
more aggressive testing.
Overall, the laboratory reporting
system's major finding so far is that
where screening is conducted, lead-
exposed children are found, but that
relatively few physicians are currently
screening children for lead exposure.
California's physicians need to more
often consider and, consequently, test
for lead poisoning.
Of the reports received through
October 1989, 926 (61 percent) were
for an elevated EP alone. Limited fol
low-up investigation of these elevated
EP levels has shown that (1) the EP
test is used most frequently by physi
cians to test for conditions other than
lead poisoning (such as hemoglobin-
opathies and iron deficiency anemia),
and (2) many physicians do not seem
to appreciate the possible connection
between an elevated EP and blood lead.
What complicates matters even
more is a connection between iron
deficiency and lead exposure, with
irondeficient children absorbing lead
more efficiently than other children.
DHS follow-up of children with elevat-
ed EP indicates that most physicians
do not investigate further with a blood
lead level once iron deficiency is iden-
tified, thereby missing some lead-poi-
soned persons in this high-risk group.
Among reports with blood lead
levels included, 287 reports (19 per-
cent) were for children with levels
greater than 15 mcg/dl, and 197 (13
percent) were for levels greater than
25 mcg/dL DHS and local health
departments investigated several of
these cases and found the sources of
environmental lead exposure were
interior and exterior paint and lead-
contaminated soil, dust, home reme-
dies, and hobbies, among other
things. In some cases, the lead
source was unknown. while in a few
cases there actually was no lead expo
sure—i.e., it was a false-positive test
Of interest were several reports
- of children poisoned from lead paint
dust generated from home remodel
ing activities in older inner<ity areas
undergoing “gentrification.”
The laboratory reporting system
has resulted in DHS initiating a coordi
~ nated follow-up and environmental
investigation program between the
~ state and local health departments, in
, partnership with California's physicians
and other medical practitioners. In
1988, DHS recommended to the
Legislature that this relationship be
strengthened, and resources have been
recently identified to carry out these
. activities.
Epidemiological studies
Because so little childhood lead
screening is currently conducted in
California, the best way, at this time,
to estimate the population prevalence
of childhood lead exposure is to con-
duct specially designed surveys. By
going door to door, it is possible to
find out about potential exposures in
all children tested, including those
~ vho do not receive frequent medical
* care. Because of the need to focus on
| preschool children, it is not possible
; to conduct the screening in public
schools or similar institutions.
So far, DHS has targeted screen
ing efforts to areas defined as “high
risk"—i.e., areas containing older
housing, having large numbers of
children under the age of six, having
—
—
.
—
—
—
—
—~
\ - °
relatively large number of ethnic
minonites. and located near environ-
mental sources of lead. Using data
from the U.S. Bureau of the Census.
along with environmental exposure
information gathered by state and
local regulatory agencies and local
health departments, the initial epi-
demiologic studies focused on three
specific areas:
¢ A neighborhood in east Oakland
that is mostly Hispanic but that also
has a large Asian population
¢ Two neighborhoods in Los
Angeles County—one in Wilmington,
with nearby lead-emitting industries
and a mostly Hispanic population, and
one in Compton, where housing is
older and dilapidated and the popula-
tion is African-American and Hispanic
e A neighborhood near downtown
Sacramento combining older housing
and a mixed African-American,
Hispanic, and Asian population
Surveys have been completed in
poisoning in these areas is higher
than expected. Between 0.5 and 1
percent of children tested in Oakland
and Los Angeles neighborhoods had
blood lead levels greater than 24
mcg/dl, and 19 percent of Oakland
study children and § percent of Los
Angeles and Sacramento study chil-
dren tested had blood lead levels
greater than 14 mcg/dl
Some of the environmental expo-
sure source data are stl being tabu-
lated, but the environmental testing
for Alameda County showed substan-
tially elevated lead levels in Oakland
each location. The prevalence of lead |
|
|
|
|
|
|
|
| | |
|
soil, where the médian household soil
lead level was 880 parts per million
(ppm). This level compares to a state
hazardous waste regulation of 1,000
ppm. In all three study areas, both
intenor and exterior paint had high
levels of lead. Of note, the majority of
households tested had paint lead lev-
els above the federal housepaint stan-
dard of 600 ppm.
Based on a review of similar
high-risk California census
tracts—i.e., ones with similar housing
and demographic characteristics—in
1989, it was estimated that statewide
there were probably at least 2,500
children with blood lead greater than
24 mcg/dl, and 10,000 with blood lead
greater than 14 mcg/dl in these “high
risk” tracts alone. It is unknown how
many lead-exposed children are in
other areas of the state. However,
environmental lead hazards, such as
older housing, contaminated soil, and
lead-emitting industrial sources exist
throughout the state and are accessi-
ble to children.
Tbe need for physician
involvement
The DHS Childhood Lead Poisoning
Prevention Program's preliminary
findings suggest that California does,
in fact, have a childhood lead-poison-
ing problem. This problem needs to
be better defined. and steps need to
be taken to abate lead exposure.
Essential to reducing such exposure
is a heightened awareness of this
potential problem among California's
physicians and commensurate
increased testing of children.
Physicians should consider possi
ble lead toxicity, and test accordingly,
particularly i in children who are ane
mic, have learning or behavioral prob-
lems, and who reside in older homes
possibly containing lead-based paint or
who live near environmental sources of
~ plants or lead smelters. Although
symptomatic lead poisoning in children
is very uncommon, children having
clinical signs or symptoms suggesuve
of lead poisoning (e.g., abdominal colic.
irritability, lethargy, or encephalopathy)
- must be appropriately tested.
Information about lead exposure
in California is rapidly evolving, so
. recommendations about lead testing
| may change in the future, especially
insofar as children with elevated
blood lead levels typically are asymp
| tomatic or have nonspecific symp
toms. Indeed, at this time, it would
appear that the most prudent course
is for physicians to obtain blood lead
tests whenever there is any suspicion
or concern about a child's possible
| lead exposure. CP
Dr. Kizer is director of the California
Department of Health Services. Dr.
Goldman is chief of the Department's
, Environmental Epidemiology and
| Toxicology Branch. Ms. Sutton, Ms.
. Flattery, and Mr. Schlag are research
| scientists with the Department's
| Exposure Assessment Section,
Environmental Epidemiology and
Toxicology Branch. Dr. Haan is ax
epidemiologist at the Kaiser Hospital,
Oakland.
—
_
—
_
"
"
"
.
LIFORNIA PHYSICIAN 53
RES SNEREE TY S
® REPORT OF DISTRIBUTION »
PROVIDER INFORMATION NOTICE 491-6
LEAD POISONING IN CHILDREN
TO:
PROVIDER INFORMATION CLERK
CALIFORNIA STATE DEPARTMENT OF HEALTH SERVICES
CHILD HEALTH AND DISABILITY PREVENTION BRANCH
714 P STREET, ROOM 708
P.O. BOX 942732
SACRAMENTO, CA 94234-7320
THIS PROVIDER INFORMATION NOTICE WAS SENT TO PROVIDERS IN
COUNTY /COMMUNITY ON
(DATE)
SIGNATURE OF SENDER
PLEASE NOTE THAT NO CHANGE IS TO BE MADE IN THIS NOTICE OR ATTACHMENTS.
PLEASE COMPLETE THIS FORM AND FORWARD TO ADDRESS SHOWN ABOVE.
THANK YOU FOR YOUR COOPERATION.
EXHIBIT D
A. Tay Jzio-1%e, A3, cel. !
High Number of Lead Poison Cases Found
m Health: State studies show many workers exposed in
Los Angeles County. Monitoring practices in industry
are criticized.
By SHARI ROAN
TIMES HEALTH WRITER §
Lead poisoning has been found in
surprisingly high numbers of Cali-
fornia workers, particularly in
high-risk industries in Los Angel-
es, two state studies have revealed.
In articles published in this
month's issue of the Amencan
Journal of Public Health, officials
at the stale Department of Health
Services report finding excessive
jead exposure to workers in a
handful of high-risk dccupations,
noting that monitoring practices to
| .
detect lead in the workplace envi-
ronment are inadequate.
Under a state law effective Jan.
1, 1987, state medical laboratories
performing tests for levels of lead
in blood have been required (0
report the findings to the Depart-
ment of Health Services, In one
study of those cases, pL least 5,000
workers were found. to have ele-
vated blood lead levels that were,
in some cases, hear LoXic.
The survey showed that most of
the exposed individuals were male
and a disproportionate percentage,
44%, Latino. The study showed
] rv
that 81% were residents of Los
Angeles County, where many
manufacturing processes using
lead are based.
Most of the individuals were
workers for lead smelters, battery
manufacturers and brass foundnes.
Construction, radiator repair, pot-
tery and ceramics manufacturing
and firing ranges accounted for the
remainder.
About half of the workers were
not in routine medical monitoring
programas.
In the second study by research-
ers at the state's Occupational
Health Program, only 2.6% of
lead -using industries in the state
reported they have done environ-
mental monitoring for lead and
only 1.4% have done routine bio-
logical monitoring programs.
In a third, unpublished study,
tests showed at least 2,500 Califor-
nia children have potentially toxic
levels of lead in their blood.
“There is more of a problem than
people thought there was,” said Dr.
Kenneth Kizer, state health direc-
tor. “The biggest problem is the
awareness, getting doctors Lo test
kids and think about il as a poten-
tial issue. You have to test for it.”
As for workplace exposure, laws
designed by the U.S. Occupational
Safely and Health Administration
to protect workers from lead expo-
sure have been overlooked, said
Dr. Philip J. Landrigan of ML Sinai
Medical Center in New York, in an
editorial accompanying the arti-
cles.
“Lead remains a serious problem
Please see LEAD, A39
5 ANGELES TIMES
* THUKSDAY, Ati inl 30, 19m A3Y
ce ve
EAD: Poisoning Cases
f {
resent but a fraction pf the tofal problem, inasmuch
+ only 14% of lead-uwng industries in California
ave developed biological momilonng programs for
nels lead -exposed workers.”
The lack of monytonng among California industries
aggests hat cases of occupauonal lead poisoning may
< METH underesumated, the study says.
if © the workplace the problem is ignorance,”
Kizer said. “It’s not knowing the laws, on the part of
workers and operators. Where you're seeing problems
is not with the big companies, it's with the smaller
operations where you don’t have the focus on health
and safety.”
In larger facilities, monitoring was more prominent.
“The problem is big, but vanes by industry, with the
larger. unionized companies more likely ‘to have
monitoring programs,” said Dr..Jon Rosenberg of the
Occupational Health Surveillance and Evaluation
Program.
Almost 80% of battery manufacturing employees
work in job classificauons that have been monitored,
compared to only 1% of radiator repair workers.
But, said Landrigan, “the number of OSHA inspec-
tors in the field must be increased. These inspectors
must be allowed to levy severe fines for repeated or
willful violations. Criminal penalties must be used
much more frequently than heretofore Lo punish
repeated and willful violators.”
According to Kizer, standards for lead exposure
have been changed in recent years as research showed
that lower levels than previously expected can cause
neurological damage. Few studies have looked at
potentially dangerous lead exposeure using the new,
more sensitive criteria for toxicity.
“We weren't totally surprised by what we found,
but by the same token, we didn’t have a basis for
knowing what it should be,” Kizer aid.
But the studies ire surprising? because lect jon on-
ing is traditionally viewed ax a problci a the
Northeastern part of the United States whee inany
industries using lead are based and where ole heanes
contain lead-based paint.
It is difficult to know if California resident . hove any
greater risk to lead exposure tha ather stat. feause
the California studies used the more sensing levels
for lead exposure, Kizer said.
But, he said, lear exposure can he easily oti J by
enforcement of OSHA regulatiens. Amon: viabdben,
most lead exposure come fron LIVING Near win ries
using lead or from lead-based paint in home .
EXHIBIT E
GS GE EGE ED Re ES ED ES ED EE ED TR WS GE GP EN WS GR TE SN GD WP ED Gh GR GP WS ES I GE GR ES Gh WD RG ER ED GP WS ED ES WS WY en wy ee
[ETHNICITY
| mmm mmr ccc dormer ———————
INDIAN|O-5 YRS | AMER | CAN
| AS | AN
|
| BLACK
|FILIPINO
IHISPANIC
IWHITE
| OTHER
IPACIFIC
| ISLANDER
SOURCE :
STATEWIDE: FISCAL YEAR 1989-90
ETHNICITY BY AGE GROUP BY FUNDING SOURCE BY LEAD TEST
OTHER TESTS...LEAD CODES 14 (FEP) AND 15 (BLOOD)
| AGE GROUP
16-20 YRS
-———— ro -————--————
|0-5 YRS
|16-20 YRS
- nn Sp
10-5 YRS
0-5 YRS
[6-20 YRS
- BF Cp ——
10-5 YRS
10-5 YRS
ae Ww wn ae -
|6-20 YRS
rt
e
tm
fp
mn
r
e
te
so
n
i
s
m
m
n
en
t
n
t
—
t
—
t
—
+
—
+
—
+
—
—
t
—
t
—
t
—
—
t
—
t
—
t=
t
=
—
4
—
EXCLUDES REFUSED ,CONTRA- INDICATED ,NOT NEEDED
|
|
MEDI-CAL | STATE | I
——————————— +rmmmm—————— | |
LEAD TEST | LEAD TEST | |
eee ——-——— frm ——- |
Wy=- | 15- | 14- | 15- | |
FEP |BLOOD| FEP |BLOOD|TOTAL |
- EE EE SE EEE SEE |
N Ji NE eee NE NY)
———— tata: Settee Settee Satertadatedl
| | | | |
| | | I |
11 I | | 11
se EE a rats sated: sedated |
2001 1] 51 2] 208]
————— tt eet EEE |
51 1] 51 2] 13]
————— is taeda Sabet tated
81 4 4 11 171
————— at taht: Sette: setae |
161 yj 2] 11 23]
on tm 10 tt EE EE EEE EE EE |
I 1] | | 11
————— a ttt Steet stated |
| 11 I | 1]
-———— tails hated St EEE TT |
121 9l 33] 381 92 |
tm LE EE ET EE |
31 11 101 61 20]
-——— lt ET EE |
11 11 21 i 4
-—--- att dette: Staats deta
21 11 21 | 51
————- Etat eT |
32] 11 2) 1] 361
- eat: Sth Setetetet adated |
61 | I I 6|
————— ts Satta: Settles atatatade
| | ! | |
11 I | 1]
———— at: Sedat State TELE
12] | 191 I 311
sm tm 1 ted EE |
71 | 20| | 271
-————— aa fe hts Rete Sadetatntedl
3061 25] 104] 51] 486]
DATA REFLECTS NUMBER OF CLAIMS PAID
HOSSHIP ,SAS ,OTHER.LEAD .FYR8990
17:36 FRIDAY, FEBRUARY 15, 1991 19
EXHIBIT F
STATEWIDE: JULY 1990 THRU JANUARY 1991 20:13 FRIDAY, FEBRUARY 15, 1991 7
ETHNICITY BY AGE GROUP BY FUNDING SOURCE BY LEAD TEST
OTHER TESTS...LEAD CODES 14 (FEP) AND 15 (BLOOD)
EXCLUDES REFUS®™ CONTRA-INDICATED,NOT NEEDED
| | I
| |
MEDI-CAL | STATE | |
——————————— tm m—m————— |
LEAD TEST | LEAD TEST | |
- Pom ———————— |
| | W4- | 15- | 14- | 15- | |
| | FEP |BLOOD| FEP |BLOOD|TOTAL |
| |= RA pn sm RAK tom |
| oN) Nd oN) Ne
| crm errr cnr rrr rrr rr ccc rrr cee —- tm———— pr nn RA spn re $m |
JETHRICITY | AGE GROUP )
- —--—————--—--
| ASIAN [0-5 YRS 191 11 11 | 21|
RE rm mmm mre —-—-—— bo ———— pm se mm ——— tom———— pm — |
| BLACK 10-5 YRS l 731 81 71 21 90 |
| | mmm ccm r cen ——— RA RU Form——— tomm———— m——— |
| 16-20 YRS ! 281 | 2] | 301
EE tt ttt tatter bm———— RU, Fm m——— sh se tm———— |
{HISPANIC 10-5 YRS | 2| 81 Yi 18 | 391
| | mmm rrr ps nh tm m—————— rom o———— |
| |6-20 YRS | 11 11 131 5) 20|
EE dom nn ee ee en tm———— trm——— fom ——— ro ———— Po———— |
IWHITE [0-5 YRS I 2] 1] | | 3)
| omer cmc torr ccm ————— to ———— pm ne to ———— ro ———— o———— |
| OTHER 10-5 YRS | 11 I 11 2]
EE tatters Frm —m mc cece —n—— bm———— tom abated mm——— A ——— |
| UNKNOWN 10-5 YRS | 2] | 3 | 51
| EE EE om————— pre me tem ——— tmm——— sp mn sm |
| |6-20 YRS | | | 4 | 4
EE ET pe sn RA sf rom m——— sp sw
| TOTAL | 128] 19] 42] 25| 24]
Cee EE EE EE EEE ER GN ED EP ED EP YE EP WR ES TE UD ES ES AS ED GP EP WS GE GS GE Gh GE Ge ES GD ED US ER WP GR EE EW eS ER ee a ee ee
SOURCE: HDSSHIP,SAS.OTHER.LEAD,.JULJAN.FYR9091
DATA REFLECTS NUMBER OF CLAIMS PAID
EXHIBIT G
_— Pe
CALIFORNIA'S MEDICAL ASSISTANCE PROGRAM
ANNUAL STATISTICAL REPORT
CALENDAR YEAR 1989
|
i | MEDICAL CARE STATISTICS SECTION
| GEORGE DEUKMEJIAN
! *:-GOVerNnor ht
| State of California
Secretary Director
Health and Welfare Agency Department of Health Services
1
|
] Clifford L. Allenby Kenneth W. Kizer, M.D., M.P.H.
)
ee TARY ry hs
Medical Care Statistics Section
State of California
Department of Health Services
TABLE 20
: MEDI-CAL PROGRAM
PERSONS CERTIFIED ELIGIBLE BY COUNTY, SEX, AND AGE
JULY 1989
BT
ns RR IRL
ERR
SE
oats
pi
SRY
18
>.
4
COTY
MALE
p
FEMALE
Total Under 5 | S-14 15-20 21-24 25-44 (5-64 | i650’ Total Under S | 5-14 15-20 21-28 25-44 5-64 6s.’
STATEV!DE 1,233,002 || 289,735 | 371,834 | 110,889 | 2¢,118 180,034 | 102,743 153.739 [1,877,718 || 278,011 | 358,816 | 172,L12 115,393 | «1,870 | 155,813 | 355,403
Lagi
t( ameda 56,980 12,825 | 17,410 5,319 1,025 8,903 5,143 6,355 | 91,585 12,679 | 16,955 | ‘BA. 5,73) 23,555 8,122 | ve
Alpine 4) 12 32 3 . 14 8 2 98 1" 33 fae," 7 26 6 6
Lmador 696 130 199 3 17 108 61 118 1,156 122 205 61 7 315 76
Butte 12,509 2,556 3,693 1,138 340 2,328 1,065 1,39 17,516 2.369 3,526 1,527 1,042 “72% 1,267 3.081
Calaveras 1,617 280 488 197 37 246 92 147 2,078 250 (32 168 120 592 144 372
= Colusa 897 193 281 104 17 101 73 128 1,270 172 262 141 wl 203 106 7
" zontra Costa 21,666 (,861 6,669 2,059 $51 3,682 1,720 2,326 34,802 4,779 6,179 3,130 2,120 | 8,545 3,120 6.629
Del Norte 2,063 395 658 151 «S «18 166 210 2,678 338 623 221 145 753 21% 383
£! Dorado 3,541 768 1,125 267 105 664 216 396 5,508 764 1,048 45 336 1,599 363 ou?
Fresno 63,822 15,849 | 22,008 6,040 1,393 8,819 4,056 5,657 88,671 1,976 | 21,173 8,525 5,875 | 20,916 s 997 | 11,209
Glenn 1,581 363 567 132 28 216 102 173 2,37 331 562 215 120 509 157 18?
Humboldt 8,481 1,692 2,534 &87 197 1,898 756 747 11,543 1,601 2.375 939 680 3,485 872 1.59
jmoer ial 10,483 1,902 3,211 Y, 008 188 1,284 954 1,900 14,074 1,76 3,140 1,526 762 3.350 1,237 2.208
| nyo 876 168 267 n 21 129 7 149 1,387 200 246 ?5 74 329 1 a 352
Kern 31,596 8,299 | 10,652 2.357 625 3,430 2,326 3,909 9,298 8,092 | 10,391 4,643 3,497 | 11,502 3.610 @®
Kings 6,344 1,646 2,237 $36 120 671 429 705 9,618 11. 1,537 1 ..2,187 924 707 2,180 646 1,037
Lake , LATS 796 1,212 352 98 740 397 628 5,880 806 1,056 (56 362 1.588 $00 12132
Lassen 1,545 345 .62 116 37 275 135 175 2,184 284 449 204 159 608 153 327
Los Ange! es 350,775 86,642 | 99,412 | 31,089 5.166 | 43,545 | 32,865 | 51,656 | 549,203 83,113 | 96,066 | ¢9,42¢ | 29,799 | 115,291 | 52,414 123,056
madera 6,309 1,627 2,013 $85 130 739 82 933 9,237 1,37 2,001 895 565 2.079 675 1,65)
Marin ‘ 3,401 607 | 88 32M 810 297 373 5,712 56% 786 L62 292 1,692 505 Y.410
Maripose 694 127 232 72 7 121 53 82 956 111 217 78 ‘6 288 $8 158
wendoc ino $,162 1,077 1,556 .o8 9 911 485 556 7,529 960 1,508 638 452 2.150 605 1.2%
werced 16,618 6,132 5,699 1,567 377 2,27 1,090 1,452 22,382 3,845 5,445 2,23 1.627 5,207 1,53¢ 2.69}
Modoc 682 13 229 $2 1" 133 $8 86 93 120 182 101 52 248 63 77
“ono 186 3 61 15 . 26 16 25 273 “9 $8 28 21 69 20 28
Monterey 12,491 3, 117 4,055 1,163 223 1,677 833 1,463 19,415 3,082 3,064 1,978 1,356 4,625 1,361 3,049
Napa 2,917 598 751 239 84 L57 246 542 4,738 613 725 418 328 1,150 357 $s SLY
Vevada 2.062 402 610 a3 $1 406 175 275 3,326 378 548 273 185 911 232 "799
orange «S281 10,953 13,298 $,712 1,143 8,080 3,876 6,221 76,100 10,429 12,630 7.814 B46 16,809 6,336 17,435
|
2223 EEIZITEIEEXEESEISSEES
TCEECICEESERSTXSTASITIZR
TABLE 20 (Continued)
MEDI-CAL PROGRAM
PERSONS CERTIFIED ELIGIBLE BY COUNTY, SEX, AND AGE
JULY 1989
J———————— TT Pr Eddie
SZC EEZSSEEISISSESIESZISSESSITIZIITZEES
oN
COUNTY
MALE
FEMALE '
Total Under 5 5-14 15-20 21-24 25-44 45-64 65+" Total Under $ 5-14 15-20 21-24 25-44 LS- 64 55+
Placer 4,576 999 1,288 358 105 839 405 582 7,845 969 1,337 S70 ¢87 2,161 631 1,710
Plumas 963 199 292 75 13 182 65 137 1,496 189 289 126 74 [AYA 117 287
Riverside 41,515 10,637 | 13,633 3,332 761 5,093 2,963 5,096 66,926 10,188 | 13,29 6,205 4,681 15,848 (B68 -°
Sacramento 64,197 15,294 20,800 5,631 1,466 10,788 5,180 5,238 94,403 14,803 20,449 8,767 6,626 25,17) 7.182 @
San Genito 1,519 358 $33 1466 3n 170 80 199 2,338 337 553 246 159 532 147 36s
San Bernardino 71,587 19,561 24,638 6,055 1,613 9,833 4,239 5,668 112,099 18,901 23,81 10,528 8,349 29,339 6,961 14,230
San Diego 80,190 18,886 23,618 7,561 1,658 12,384 6,145 9,938 126,252 18,205 23,062 11,477 8,030 33,220 9,972 24,284
san Francisco 38,158 5,375 7,626 3,019 $34 7,894 5,729 7,981 51,857 5,242 7,562 3,897 2,093 11,085 5,779 16,199
san Joaquin 41,003 9,322. 13,650 3,784 866 6,413 3,195 3. 70 $5,351 8,949 12,859 5,455 3.502 13,623 ¢£,180 {22}
San Luis Obispo 5,824 1,336: 1,673 476 152 897 438 852 9,454 1,212 1,573 781 593 2,461 730 2,104
San Mateo 11,347 2,454 2,814 891 2L4 1,756 940 2,250 19,703 2.377 2,792 1,516 1,148 3,929 1.756 6,185
Santa Barbara 10,170 2,496 3,076 812 250 1,520 766 27° 16,368 2,457 2,984 1,608 1,09 3,891 1,190 3,17
Santa Clara 63,788 9,425 12,074 4,936 1,031 6, TN 3,409 6,122 65,153 8,838 $Y, o0e 6,536 (£,218 14,493 5,501 16,295
Santa Cruz 6,724 1,591 1,817 L476 133 1,229 531 947 10,648 1,628 1,723 888 687 2,815 841 2,266
Shasta 10,548 2,190 3,305 827 269 1,993 899 1,065 15,244 2,015 3,160 1,273 958 6,204 1,214 2,419
Sierra 175 ~28 45 18 2 32 12 38 246 22 L7 21 6 60 23 67
Siskiyou 3,030 STIS)", 962 267 bh S01 278 381 4,375 510 959 336 225 1,217 368 760
solano 11,001 2, TOT 3,626 934 295 1,659 641 1,057 18,478 2,697 3,514 1,697 1,411 (,92 1,284 2.951
Sonoma 11,551 276°. 3,1 916 295 | 2,621 | 1,024 1,298 18,115 2,234 3,092 1,410 1,080 5,161 1,646 3,692
Stanislaus 25,215 5,551 8,080 2,087 529 3,936}. 2,201 2,801 37,653 5,336 7,950 3,679 2,612 9,273 3,013 5,990
Sutter 3,846 878 1,197 Jo? 101 614 i 296 653 5,851 849 1,104 $32 386 1,489 85 1,026
Tehama 3,496 688 1,168 287 85 540; 307 3 5,035 707 1,059 615 296 1,35¢4 395 7
Trinity 833 159 259 74 14 159 72 96 Y,153 14) 253 106 72 328 87 a
Tulare 30,303 7,10 10,221 2,630 630 4,188 2,108 3,625 42,046 6,727 9,856 3,996 2,658 9,546 3,084 0,179
Twoluwe’ 1,810 354 626 154 39 311 124 202 2,921 316 610 234 151 909 206 «95
Ventura 16,636 3,764 5,137 1,526 374 2,401 1,221 2,215 26,435 3,697 4,807 2,476 1,734 6,126 2,068 $2?
Yolo 7.130 1,695 2,169 587 149 1,101 621 817 10,167 1,521 2,114 870 700 2,657 810 1,495
Yuba 6,653 1,456 2,108 S64 \77 1,089 602 657 8,575 1,636 1,957 790 $28 2,182 673 , 009
* Includes Age Unknown.
Includes regular Fee-For-Service, Redwood Health Foundation, Sants Barbera Health Initiative,
Note:
Excludes sex not reported.
Excludes Prepaid Health Plans,
Source: State of California, Department of Health Services,
San Mateo Health Plan, and Delts Dental Service.
persons Certified Eligible for Medi-Cal by Age and Sex, July 1989, run date 2/16/90.
en ge ——
State of California
Medical Care Statistics Section
Department of Health Services
TABLE 21
MEDI-CAL PROGRAM
AVERAGE MONTHLY ELIGIBLES BY COUNTY, PROGRAM, AND AID CATEGORY
CALENDAR YEAR 1989
PUBLIC ASSISTANCE
* MEDICALLY NEEDY MEDICALLY INDIGENT
COUNTY TOTAL
Aged slind Disabled Families Aged Blind Disatled Families Adults Children
STATEVIZE 3,105,993 311,34 22,866 468,494 1,754,912 84,336 403 32,496 212,299 7,305 '® »
-
- Alameda wr, 716 12,756 1,204 26,128 89,779 |! 4,135 12 1,575 7,480 238 2,707
Alpine 170 5 ? 1" 13645: | - - 13 1 3
Amadar 1,856 27 | 15 290 988-7: I. 119 a 23 149 4 36
Butte 29,716 2.93) | 236 6,729 17,906 "| 750 3 197 | 2,132 78 96
Calaveras 3,525 282 27 619 2,258 42 1 35 EY : 278 4 82
Zolusa 2,174 207 15 265 1,008 56 > x PI 266 7 213
Contra Z0s3%d 56,451 5,258 495 10,625 32,445 1,840 1" S79 3,209 08 1.32
Del Norte 6,776 3 31 7 3,140 61 2 23 253 6 or
£1 Doraco 9,049 770 64 1,326 5.327 288 0 72 684 27 219
J Fresno 152,278 10,490 740 15,720 100, 760 2,095 8 $26 10,586 358 S, 781
Glenn | 3,879 339 30 462 2,264 82 . 29 323 1% 235
Humbo! dt | 20,034 1,452 132 3,636 12,018 348 1 195 1,739 6 $63
Imperial : 26,712 2,848 138 3,007 13,239 388 3 161 3,288 106 1,128
Inyo 2,27 312 17 IN 1,213 93 . 28 158 9 66
Kern 81,252 6,903 $65 12,116 47,728 1,288 2 458 6,707 185 3,536
X ings 15,967 1,413 85 1,904 9,890 264 1 n 1,109 27 682
Lake 10,025 1,058 | 72 1,686 5,981 226 3 87 663 16 180
Lassen 3. 02 280 | 30 535 2,612 87 - n 189 1 \3
Los Angeles 903,733 108, 504 | 7,066 141,366 460,613 28,177 129 10,399 61,342 2,257 B
Madera 15,629 1,563 | 102 2,152 8,028 328 4 104 1,430 £2 «(3
Marin/ | 9,075 927 95 2,203 3,715 524 3 139 778 28 351
Mor ifoss 1,666 162 9 151 1,076 47 - 17 128 9 60
Mendocino | 12,646 1,080 84 2,081 7,480 269 2 126 905 37 «2
Merced 38,940 2,647 201 3,832 27,045 489 2 154 2,196 rs 1,457
vodoc 1,659 154 7 227 1,020 51 2 13 99 S $9
] 1
Mono 458 29 2 55 275 10 . 6 39 3 20
Monterey 30,912 2,86! 210 3,916 16,502 655 1 225 4,078 80 1,198
Napa 7,656 757 72 1,410 3,730 583 1 141 $22 19 302
vevads 5,423 590 56 919 2,860 2N 1 64 429 1¢ 13
Orange | 122,928 "“w, 237 | 1,094 17,621 $3,860 5,376 16 2,03¢ 11,610 «95 7.676
O~
;
£323S3INSSIERSZTTIESEACECETERTITIEIR
UXCNNND
TABLE 21
PUBLIC ASSISTANCE
(Continued)
MEDI-CAL PROGRAM
AVERAGE MONTHLY ELIGIBLES BY COUNTY, PROGRAM, AND AID CATEGORY
CALENDAR YEAR 1989
MEDICALLY NEEDY
NEE EEEEISEANEEEESCESSANEASEEENAEISEENESASEEESEINENE
EEEEIEEEANE NESE NRS ENE ERE EAA EER IIEIITAREICIIIIIIIIIIARIIARAARI RATAN
MEDICALLY INDIGENT
A
COUNTY TOTAL
Aged Blind Disabled Femil ies Aged Blind Disabled Families Adults Chilagren
Placer 12,322 1,149 101 2,309 6,614 624 1 143 829 37 ; 384
Plumas 2,488 246 26 388 1,492 76 - 17 180 ; | 5
Riverside 107,518 10,582 816 15,480 63,476 2,401 1 896 7,846 281 3 An
Sacramento 158,822 9,606 993 23,546 110,443 LT a5 6,180 200 2}
San Benito 3,865 362 20 329 2,097 102 1 «0 $51 13 21%
San Bernardino 180,492 12,004 1,060 21,109 126,317 3,060 26 1,136 9,199 289 3,629
San Diego 207,526 21,481 1,698 31,860 116,408 6,168 22 2,185 13,037 639 7.9084
san Francisco 89,865 15,574 895 21,313 35,309 3,660 23 1,689 6,281 322 | 2.807
san Joaquin 96,167 6,147 530 12,524 65,763 1,657 7 786 4,918 110 i 1,949
San Luis Obispo 15,193 1,700 135 2,722 7,182 581 1 258 1,507 63 | 722
San Mateo 31,061 5,250 258 6,058 12,070 1,603 7 485 2,415 68 | 1,378
Santa Barbara 26,740 2,582 202 6,236 13,530 864 6 In 2,506 104 1,326
santa Clara 108,442 12,994 816 15,384 57,546 3,807 22 1,535 7,541 156 3 199
Santa Crut 17,157 1,902 167 3,199 8,151 622 3 196 1,733 0 $70
Shasta | 25,813 2,065 157 4,051 16,759 S47 1 193 1,276 50 | 60%
Sierras | 408 53 4 82 189 33 1 3 39 1 3
Siskiyou i 7,646 Nou, 103 S1 1,169 4,410 168 2 52 602 13 22%
Solano 29,351 “2,626 205 4,548 18,829 692 ‘ 262 1,623 «8 $31
Sonoma | 29,790 2.817 32¢ 6,193 15,153 966 10 919 2,154 $3 778
Stanislaus 61,8480 5,427 $16 8,694 . | 38,776 1,215 12 «88 4,088 100 | 1,639
Sutter ! 9,641 9.8 75 1.37 - 5,327 181 1 69 948 36 | cL.
Tehama 8,475 742 60 Y,204 ; 4,832 163 2 74 692 25
Trinity | 1,99 167 1% 283 .) 1,229 a . 20 172 6
Tulare 72,429 6,048 44 8,841 43,074 1,063 1" 956 5,761 149 3,846
jusiumiy | 4,760 &21 33 685 2,883 120 0 38 426 13 "hn
ventura 43,676 4,728 298 6,509 20,981 1,548 6 862 5,236 12 | 2,206
Yolo 17,223 1,237 103 2,478 10,830 521 6 173 936 “ 92%
Yuba 15,178 082 75 2,231 10,330 129 » 78 843 22 | 370
State of California
Department of Health Services
TABLE 24
MEDI-CAL PROGRAM
Medical Care Statistics Section
AVERAGE MONTHLY USERS BY COUNTY AND SELECTED TYPES OF PROVIDERS
CALENDAR YEAR 1989
COUNTY TOTAL PHYSICIANS [PHARMACIES | DENTISTS | OPTOMETRISTS COUNTY HOSPITAL COMMITS WOSPITAL | SALE io LINC
Inpatient Outpatient Inpatient| Outpatient CARE
STATEVIDES 1,507,718 | 685,954 878,859 112,850 ss, 0m | FEN, 35 |, 69,288 42,818 209,352 6,626 65,249
Alameda 70,293 30, 880 39,370 s,386 1,818 "f622 3,959 1,905 10, 942 27 3.016
Alpine 39 12 5 3 3 * ¥ ° 3 ald . »
Amador 974 318 581 L8 34 20 143 10 rf 1 93
Butte 15,302 6,739 9,269 953 502 3 39 “79 3 483% 3 586
Calaveras 1.637 649 939 124 66 13 82 2 392 2 99
Colusa 1,062 486 586 56 29 1 22 ‘s 215 a 51
Contra Costa 27.243 11,292 15,440 2.154 628 211 2,800 728 4,335 17 1,339
Del Norte 2.188 581 1.218 152 102 : 4 62 904 : ok
El Dorado 4.205 1,52% 2.313 279 163 2 19 159 89% 2 214
Fresno 68. 794 33,088 41,288 5,414 2.208 $77 3,501 1,405 9,598 12 1,963
Glenn 1,885 623 1,063 122 57 15 356 52 180 1 59
Humbo | dt 10,135 3,898 5.842 634 286 2 23 294 2,311 2 299
Imperial 11,051 5,309 6,450 678 358 3 17 408 1,949 1 185
Inyo '.180 «23 654 68 53 1 6 46 233 2 65
Kern 36,260 13,183 22,108 2,896 1,200 722 4,290 609 4,588 12 1,021
Kings 7,769 3,318 4,650 604 337 6 29 271 2,156 2 193
Lake S068 2.376 2.996 283 199 10 58 143 1.073 1 154
Lassen 1.896 670 1.104 77 60 1 6 59 337 2 81
Los Angeles «57.680 | 221,279 279,110 31,874 12,772 6,466 17,189 13,047 48,955 1,130 22,309
Maders 7,364 3, 264 4,334 697 251 36 114 213 1,177 2 284
Marin ‘902 2,187 2,678 390 78 3 23 142 mm 3 «78
Mariposa 755 318 377 38 24 7 38 20 218 . 33
Mendoc i no 6,440 2,526 3,443 $11 186 13 $38 202 1,376 4 286
Merced 17.291 8.510 10,044 953 450 259 2,125 282 2,361 3 384
Modoc 823 236 «25 3 51 » 4 2 258 . 52
Hono 207 6! 68 16 s tl.» 8 9 31 ‘ 7
Monterey 13,807 5,811 7,535 930 382 207 1,482 382 1,821 5 «65
NADY “148 1.854 2,176 217 9s 2 19 150 907 80 “24
Nevada 2.892 1,385 1,620 219 8 1 5 102 620 2 23%
Orange 64.816 30,973 36,595 ¢,899 1,367 23 140 2,641 9,000 1,064 3.918
s
State of California Medical Care Statistics Section
Department of Health Services
TABLE 28
MEDI-CAL PROGRAM
COUNTY POPULATION, MEDI-CAL ELIGIBLES, AND
MEDI-CAL ELIGIBLES AS A PERCENT OF COUNTY POPULATION
CALENDAR YEAR 1989
==z====SS
EEE RSE SRR ECE REN EEESSREESINSINES
ELIGIBLES
1 2 Ey eat 1 2 | AS A PERCENT b
AS A PERCEN
COUNTY POPULATION ELIGIBLES OF COUNTY county POPULATION = | ELIGIBLES OF COUNTY a
: L POPULATION
STATEWIOE 29,063,200 | 3,323,154 11.4%
Alameda 1,261,500 148,365
Alpine 1,200 170
Amador
Butte
Calaveras
Placer 162,900 12,322
Plumas 2 488
Riverside’ 108 483 .
Sacramento 158; "822:
San Benito 3 865%
e
o
a
oo
O
S
o
e
O
O
O
—
—
a
l
l
h
.
-—
San Bernardino 185,370
San Diego
Son Francisco
San Joaquin
San Luis Obispo 216, 1600
San Mateo 637,200
Santa Barbara
Santa Clara
Santa Cruz
Shasta
—
Colusa
Contra Costa
Del Norte
El Dorado
Fresno
~N
S
N
O
W
N
N
=
N
N
O
N
O
N
O
W
O
v
o
nN
Glenn
Humboldt
Imperial
Inyo
Kern
ee
eo
=
r
O
O
N
C
O
O
N
W
O
N
G
u
y
t
h
Sierra
Siskiyou
Solano
Sonoma
Stanislaus
Kings
Lake
Lassen
Los Angeles
Madera
¢
v
w
W
O
O
V
R
O
N
N
W
O
O
N
N
O
R
A
N
G
O
N
N
H
E
~
O
R
I
L
W
O
a
d
ad
h
d
wd
wd
PN
)
md
uD
a
O
N
W
O
E
O
V
I
N
O
D
Sutter
Tehama
Trinity
Tulare
Tuolumne
Marin
Mariposa
Mendocino
Merced
Modoc
.
.
-
t
PJ
)
ts
wa
N
N
O
—
B
N
O
N
E
V
I
N
N
O
Y
N
R
V
C
N
N
)
=
c
a
a
Ventura
Yolo
Yuba
Mono
Monterey O
N
O
V
H
A
NV
N
I
N
D
O
C
I
n
N
)
=
»
V
I
O
N
»
80,900
2,301,200
State of California, Department of Finance, population estimate as of July 1, 1989, Report 89 E-2.
Includes regular Fee-For-Service, Redwood Health Foundation, Santa Barbara Health Initiative, San Mateo Health Plan, and
Delta Dental Service.
Includes Prepaid Health Plans.
State of California, Department of Finance, Population Estimates for California Counties.
State of California, Department of Health Services, Medi-Cal Certified CID eligibles, Calendar Year 1989; and Prepaid
Health Plan Status Code Reports.
State of California / 4 Medical CF tatistics Section
Department of Health ices
TABLE 29
MEDI-CAL PROGRAM
: PLRSONS CERTIFIED ELIGIBLE
BY COUNTY AND RACE/ETHNICITY
JANUARY 1989
EEE TE LLC EE EE EE EE EE EE EF SF RRR Er Re I III TM
AMERICAN [WDIAN/ ASIAN/PACIFIC ¥O!
count om AUASCAN NATIVE ISLANDER BLAZR i Soa ils REPORTED
STATEWIDE 3,216,418 17,706 185,707 $73,857 748,939 1,277,001 £13,118
Nicds 146,420 502 5,007 63,926 | 10,59¢ 34,263 28,128
Amador 1,843 65 8 7 133 1,602 136
Butte 29,304 254 1,640 68 1,133 23,595 2.114
Calaveras 3.619 67 11 1 109 3,086 15%
Colusa 2,156 3s 33 23 6&1 1,259 165
Contra Coste 64,050 13% 4,764 20,628 $, 9 27,93 s,m
Del Norte 4,770 313 37 17 93 3,723 327
El Dorado 8,976 3 3% 78 225 8,023 $43
fresno 145,885 $09 2.875 15,612 $3,405 LO, 5686 32,708
Glenn 3,877 on 286 32 354 2,695 219
Humboldt 19,545 1,192 858 198 220 15,822 1.2% i
tmperiat 23,851 208 41 881 | 1¢,619 S$, 749 2,373 :
Inyo 2,2 17 3 9 130 1,628 224 :
Kern 77.928 268 $95 10,332 | 22,291 38,115 5,927
Cings 15,405 193 262 1,642 S,816 6,353 1,139
Lake 9.843 339 27 287 292 8,218 680
Lassen 3,762 84 12 70 7 3.3%? 212
Los Angeles 1,023,223 1,71 73,232 267,3%¢ | 300,99 284,333 95.599
Madera 14,976 120 108 [03 5.38% 6,537 1.892
Karin 8,845 29 73 1,189 $97 S,616 961
Mariposa 1,698 30 2 ¢ 21 1,565 76
Mendocino 12,407 e37 $1 122 566 9,888 843
Merced 37,901 17 8,057 2.813 | 10,319 1,076 2,519
Modoc 1,59 109 2 b3 32 1.45 106
Mono 30 132 1 . ° 224 33
Monterey 30,368 114 1,963 2,425 13,519 9.570 2,77
Napa 7,616 36 104 103 Mm S,847 81%
Nevada $,380 58 23 10 107 4,807 375
Orange 121,989 146 3,36 3,820 25,842 $1,904 37.131
Placer 12,20 97 $9 105 | 2 nes 10,338 919
Plumas 2,49 % . G1. se 2,09 157
Riverside 106,91 2 3,638 12,758, 25,73 $5,433 8,377
Sacramento 154,846 1,136 8,282 30,561 16,055 3,873 26,939
San Benito 3.88% 8 22 2? 2,220 1,313 295
San Bernardino 181,922 1,275 £,569 29,640, | ¢1,678 93,969 10, 791
San Diego 222,914 1,688 5.560 35,720 £6,961 95,570 37,615
San francisco 87.4% 132 12,3463 24,999 6,548 20,698 22,759
San Jooquin 93,943 378 23,450 9.962 | 18,401 203 7.569
San Luis Obispo 14,856 61 143 563 2,033 10,780 1,276
San Mateo 29,196 38 1,648 6.517 6,485 1,229 5.279
Santa Barbara . 25,615 96 526 1,611 9,130 1,731 2,521
Sante Clare 114,048 $45 $,217 8,500 32,029 35,545 32,212
Ssnte Cruz 16,475 (7 153 24 4,002 10,21$ 1,835
Shasta 25,649 651 1,191 382 381 21,248 1,796
Sierra : 420 S 1 S S 363 4
Siskiyou 7,512 294 142 2867 240 6,102 L487
Solano 28,626 101 1,118 8,377 2,098 13,572 3,363
Sonoma 29,317 827 289 1,100 2. 0M 21,450 3,780
stonisleus 80,442 202 7.431 1,639 9,977 36, 606 ¢,587
Sutter 9,698 77 301 | w 1,571 6,757 me
Tehoma 8,234 : Me... 29 a 2s $03 7.071 £91
Trinity 1,957 68 6 8 30 1,764 103
Tulasre 70,497 370 852 4 2,203 27,353 30,499 9.220
Tuolume 4,800 4S 19 in 122 4,325 rs
Venturs 43,012 133 1,011 2,103 16,468 19,275 £,022
Yolo 16,801 140 S16 716 3,598 9.409 2,422
Yuba 14,963 129 2.659 450 743 10,082 930
Not Reported 1 - . . . - 1
Source: State of Californias, Department of Kealth Services, MEDSTAT Eligible file, Jensary-Kerch 1989, run
08/89.
NS
87
EXHIBIT H
: FISCAL YEAR 1989-90 17:36 FRIDAY, FEBRUARY 15, 1991 35
PROVIDER NUMBER BY AGE GROUP BY FUNDING SOURCE BY LEAD TEST :
WITHIN COUNTY OF RESIDENCE
OTHER TESTS...LEAD CODES 14 (FEP) AND 15 (BLOOD)
EXCLUDES REFUSTD,CONTRA-INDICATED,NOT NEEDED
COUNTY OF RESIDENCE=SANTA CLARA
|
| |
| | ISTATE| I
| | MEDI-CAL |-==-~ |
| |r ILEAD | |
| | LEAD TEST |TEST | |
jevnvunswens dbeewun
I | 14- | 15- | 14- | |
| | FEP |BLOOD| FEP |TOTAL|
| | wom tt tom +m
I Foul Nao) NN
Eh ti iE A iris Prenns Po ewe hic
|PROVIDER NUMBER |AGE GROUP ‘
| emer rnc Frm —--———
| CMM70084F |0-5 YRS. | 214] 11 11 216]
ll | eeemcccnccccen- ata sh me tm ——— RA |
| [6-20 YRS | 51 | I 51
cece cr crc --- tr TE EE SE TE TELE »
|00A369020 |0-5 YRS | | 21 | 2]
= = = = = nn Bs
| TOTAL I 219] 31 1} 223}
PD Gh ES ES GR ES GSS SS WS EE SE EP GD GD ee EE GT en
SOURCE: HDSSHIP.SAS.OTHER.LEAD.FYR8990
DATA REFLECTS NUMBER OF CLAIMS PAID
EXHIBIT 1
FISCAL YEAR 1989-90 17:36 FRIDAY, FEBRUARY 15, 1991 5
ETHNICITY BY AGE GROUP BY FUNDING SOURCE BY LEAD TEST
WITHIN COUNTY OF RESIDENCE
OTHER TESTS...LEAD CODES 14 (FEP) AND 15 (BLOOD)
EXCLUDES REFUSED ,CONTRA- INDICATED ,NOT NEEDED
COUNTY OF RESIDENCE=LOS ANGELES
| | |
| | |
MEDI-CAL | STATE
- o-oo --
; LEAD TEST | LEAD TEST | ;
- o-oo rn -—-———---
| | W4- | 15- | 14- | 15- | |
| | FEP |BLOOD| FEP |BLOOD|TOTAL |
| | sm fp pn sp sp mm |
, SHIN oe NE LR
i EE EL EE EE El tL dpm sm so ne ated bom ——— bom——— rn mn Li
i JETUNICITY | AGE GROUP ; | ;
- ro ——————-—- - ---
| AS | AN 16-20 YRS I I 2! I I 11
EE a tadader frm e mn —————--—— dpm mm pre tm fom m—— mm
|BLACK 10-5 YRS | 21 | | 11 31
| | eeecsccccccccee=- mn Ap sm sp m———— RA J
| 16-20 YRS | 2] 3 | 11 6|
Ett EET EE LLL EE tom——— ated sp m———— sh me ne |
IHISPANIC {0-5 YRS | 11 51 16 23] u5|
| I Kettle rm——- atta bo————— spr ns RAC |
| 16-20 YRS | I | 11 6| TI
| merc cncccee—- ps stn sm 3 m———— br———— rm——— m———— ro———— |
IWHITE 16-20 YRS | 1] 11 | I 2
2 Eh rE tls ttt tiated
| OTHER 10-5 YRS | | J J 1) 11
|eemm—- - = nn em eo BA Be perme ps |
| TOTAL | 6| 101 171 32] 65 |
SOURCE: HDSSHIP,SAS. OTHER .LEAD.FYR8990
DATA REFLECTS NUMBER OF CLAIMS PAID
EXHIBIT J
© on rom,
~ i # &
IN THE UNITED STATES DISTRICT COURT
FOR THE NORTHERN DISTRICT OF CALIFORNIA
-=000™~
ERIKA MATTHEWS, et al
Plaintiff,
vs. No. Civ. No. C-90-3620 EFL
KENNETH KIZER, et al
Defendant.
CORY
--000--
Deposition of
RUTH S. RANGE
Friday, May 3, 1991
--000--
Reported by: Virginia A. Lathan, CSR No. 6394
CAL WEST REPORTERS
801-12th Street, Suite 600
Sacramento, CA 95814
(916) 442-9151
FAX (916) 442-1310
17 Qo. Have you attended any meetings with Lynn Goldman
18 regarding lead?
19 A. Yes.
20 + How frequently?
ETES yond URC a a dR Sadat hb TE Re a a TE _ wy
© 916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
24 Q. The subject matter of the meetings with Dr. Goldman,
25 can you tell me generally what they were about? -
26 A. The new CDC or the proposed CDC recommendations for
ee ett a. ee i et, er.
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
Q. Was there any discussion in the Goldman meetings
about what the State of California is doing regarding
Medi-Cal eligible children from determining exposure to
lead?
A. Not that I recollect.
Q. Were these -- did anyone raise that subject, as far
as you recall?
A. No.
Q. So, that as I understand your .testimony, what these
meetings discussed was what CDC was recommending; is that
correct?
A. Yes.
Q. Was there a discussion regarding what CDC was
recommending regarding screening methodologies?
Yes.
what was said?
That the EP test is no longer -- is not sensitive
enough for the new referral levels.
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
é o .
Q. And was another test or other tests suggested as
preferable to the EP test?
A. Two tests were discussed: blood lead and another
capillary test with a different technique.
Q. Do you know what that technique was?
A. It required a deeper blade to cut a better specimen.
Most likely, it would be a capillary specimen.
Q. But you‘re still talking about blood tests; is that
right?
A. Yes.
Q. Is "EP" capital “E," capital "P," when you use "EP"?
A. Yes.
|
Q. I'm going to come back to this shortly. But let me
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
IER 2h
» y 3
1 ask you, with respect to your background, Miss Range, have
( 2 you co-authored or authored any papers regarding screening
3 for purposes of determining physical or mental illnesses or
4 conditions relating to exposure to lead?
.. A. No.
6 0. Have you done any writing in the area of lead?
7 A. No.
) Q. Do you consider yourself an expert in terms of lead?
9 A. No.
10 Q. Putting aside these two meetings you mentioned, have
11 you attended any conferences or seminars with respect to
12 lead?
13 A. No.
14 Q. Your degree is in school nursing?
( 15 A. Yes.
16 Q. Did you have any specialized training in the school
17 of nursing?
18 A. Public health.
19 QS. Have you received any specialized training in the
20 area of lead?
21 A. No.
22 Q. Are there --
23 A. Would you define "specialized training"?
24 Q. I don’t mean the sort of training that every nurse
25 would get; I mean specific courses or areas of courses that
26 were devoted to lead in some detail?
, 27 A. No.
\ 28 Q. Do you, in your own mind, have a view as to who are
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
{
S—
Som,
\ EE TN,
14
the experts with respect to issues concerning exposure to
lead, in the profession?
A. Yes.
gy, Who are they?
A. The experts would be those folks in CDC and also
Dr. Goldman in the Department.
Q. When you say "those folks in CDC," can you name any
of them?
A. No.
Q. You do consider CDC as expert in the area of
childhood lead poisoning?
A. I would hope so.
Q1A/447-Q181 CAT. WFrST RFDPORTFRS FAY Q16/4472-131nN
28 Q. Why is it important to get a blood level of the
916/442-9151 CAL WEST REPORTFRS FAX 916/442-131n
[ ® 22
child?
A. To determine if the child has an elevated blood lead
level.
Q. When you say "elevated," what do you mean by that?
A. Currently, the referral level is 25 micrograms per
deciliter.
Q. What do you mean by that?
A. That would be the level at which the child would be
referred in for a further evaluation.
Q. Why is it important to know if a child has an
elevated blood lead level?
A. To remove the environmental causes of the lead or to
treat, if necessary, depending on the level.
Q. Do you know, Miss Range, in the year 1991, since
January 1, how many children have been determined to have
elevated blood levels among the Medi-Cal eligible children?
A. No.
Q. Has that data been collected?
A The laboratories must report it to the blood Lead
Program. They would have that data.
Q. Have you seen that data?
A. No.
Q. Have you made any attempt to get it?
A. No.
Q. Any reason why not?
A. That -- January 1991 -- depends on how quickly the
laboratories report it.
Q. Have you made an attempt to find out whether any of
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
Lo
2) » 0
that data is available?
A. No.
0, How about for 1990, do you know how many children who
were Medi-Cal eligible had an elevated level of 252
No.
Did you make any attempt to get that information?
A
Q
A. No.
Q Any reason why not?
A It was one of the areas that I knew was being taken
care of by somebody else.
Q. Who?
A. The blood lead people who report it to the local
health department to then do investigations of these
children.
Q. How about for ‘89 or ‘90 or any year ‘going back to
1986? Have you seen any data regarding the number of
children with elevated blood levels?
A. No.
Q. Is it fair to say you haven’t made any attempt to get
that information?
A. Certain cases have been discussed, but I haven't
gotten the information, no.
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
Q. Does EPSDT, in your understanding, deal with the
exposure to lead in children?
A. Yes.
0. And can you tell me what your understanding is as to
what the purposes of the EPSDT program are with respect to
exposure in children to lead?
A. To assess children that could be at risk for lead
exposure and test those that are determined to be at risk.
Q. Now, when you say "who live in an environment where
they could be exposed to lead,” what do you mean by that?
A. 014 housing, peeling paint.
Q. When you say "old housing," what do you mean by
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
or Hs
Fai aa
® » 25
1 that?
f 2 A. I think mostly prior to 1950, where the housing is
3 old and the paint is in poor condition.
4 Q. Now, do you know the numbers of Medi-Cal eligible
5S children who live in old housing, as you define it?
6 A. No.
7 Q. Have you ever made an attempt to determine that?
8 A. No.
4 Q. Has there ever been any inquiry, as far as you know,
10 to determine that?
11 A. No.
12 Q. Do you have any assumptions with respect to that?
13 A. The issue is broader than Medi-Cal eligible
14 children.
15 Q. Which issue?
16 A. The issue would be: looking at any child, regardless
17 of their Medi-Cal eligibility, for risk of exposure.
18 Q. My question is: Has there ever been any inquiry or
19 attempt to determine how many kids, who are Medi-Cal
20 eligible, live in old housing, as you defined it?
21 A. No.
22 Q. With respect to the "behavior problems, * as you
23 described it, to your knowledge how many kids, who are
24 Medi-Cal eligible, exhibit such behavior problems?
25 A. I do not know.
26 Q. Has there ever been any attempt to find out?
27 A. I don’t know.
8 ,e JE Ah Ee eh
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
C C
a useful thing to do?
A. May I go off the record?
MR. ROSENBAUM: Sure.
(Whereupon a discussion was held
off the record.)
THE WITNESS: No, I have not made that
suggestion.
MR. ROSENBAUM: Q. In 1991, do you know how
many children, who are Medi-Cal eligible and who saw
providers, who lived in an environment, as you described
it, regarding exposure to lead?
A. No.
Q. Or with respect to any of the other factors that you
mentioned, do you know, for 1991 or 1990?
A. No.
Q. Any area?
A. No.
Q. Has there been any attempt to find out that
information?
A. I do not know.
Q. Were Medi-Cal providers, in 1990, specifically
directed to ask questions regarding environment?
A. The directives in Medi-Cal guidelines gave them some
guidelines for assessing exposure to lead.
Q. But that’s not quite my Question.
Were they specifically directed to ask
questions regarding environment?
A. In the Medi-Cal guidelines, they were requested to
30
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
Pa f N
Vain
1
" ‘®
through your department or any department, to your
knowledge, ever attempted to determine just how well the
program is doing with respect to identifying kids with
elevated blood lead levels?
A. No.
MR. VAN WYE: Wait. Do you know, or not, to
your knowledge?
THE WITNESS: Not to my knowledge, actually,
would be better.
33
te
A
n
Ea
A
0
A
S
A
i
n
s
NTE /AA9.Q151 CAL WEST REPORTERS FAX 916/442-1310
Q. Do you regard the way you carry out your duties and
responsibilities to be governed by the State Medicaid
Manual?
A. Yes.
Q. In your experience, do you know of any time when the
State Medicaid Manual directives have not been followed?
A. I can only answer for the EPs -- the portion of that
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
manual that we have responsibility for.
I'm not aware of any times.
Q. You regard that as your controlling regulations,
directives; is that right?
A. They are guidelines.
Q. And you regard them as controlling what you do; is
that right?
A. Yes.
Q. Now, going back to the EPSDT law as defined in the
regulations -- HCFA transmittals. What's your
understanding of what the law requires in terms of exposure
to lead?
A. Assessment of the risk of a child being exposed to
lead and testing those children determined to be at risk.
Q. Has that ever been communicated to providers, that
that’s the purpose of the law, to your knowledge?
A. I'm not sure that we interpret it to providers as
the law.
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
28
Q. Do you have an understanding, Miss Range, as to
whether or not a child can be suffering from lead toxicity
and not be symptomatic?
A. Yes.
Q. What's your understanding?
A. That symptoms may not be demonstrated during very
high levels.
0. Why is that?
A. I do not know. I’m not sure anyone does.
Q. Can you give me an example of levels of lead
toxicity at which a kid would not be necessarily
symptomatic?
A. At 25 to S50.
Q. What about below 25?
A. Probably not, or they would be very subtle.
Q. When you say “very subtle," what do you mean by
that?
A. Probably symptomatology that would not be identified
as resulting from lead.
Q. Can asymptomatic lead toxicity be determined without
use of some sort of blood test?
A. Would you repeat that?
Q. Yes. Can the asymptomatic lead toxicity that you’ve
been telling me about, can that be determined without the
use of some sort of blood test?
MR. VAN WYE: I Object to the question and
direct the Witness not to answer, because that legally
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
Pan 3 Poi
ey
¢ ® 1
1 calls for a medical conclusion, and she’s not a medical
2 doctor.
3 MR. ROSENBAUM: Q. Well, do you have any
4 understanding whether or not that can exist, in the
s carrying out of your duties?
6 A. Yes.
7 Q. What's your understanding?
8 A. That it can exist.
) Q. That is for the reason that you told me earlier; is
10 that right?
11 A. There would be no symptoms, or there would be
12 symptoms.
13 Q. Is that true of children at all ages?
14 A. I do not know.
D 1s Q. What about children below age five?
16 A. Yes.
17 Q. Can you tell me for 1991 or 1990, or any period of
18 time, the number of children in the EPSDT program who have
19 been identified as suffering from lead toxicity?
20 A. No.
21 Q. Has any inquiry been made to determine that?
22 A. No.
Q1A/447-Q181 CAT. WFST R¥FPORTERS FAY Q16/442-1310
QD
Q. Do you know how many of the children you're talking
about were identified in terms of their exposure to lead,
as part of the EPSDT program?
A. No.
Q. Do you know what percentage?
A. No.
Q. Has there been any attempt to find that out?
A. No, not that I know of.
Q. Are you aware of any studies of exposure to lead in
Oakland or Wilmington or Compton or other communities
throughout California?
A. Yes.
Q. And who conducted those studies?
A. I believe the Lead Program did. Dr. Goldman’s
program.
Q. Do you have any responsibilities with respect to
those programs?
A. No. :
Q. Have you seen the results of any of those studies,
or --
A. I've read the report.
Q. - And do you know how the screening was accomplished
in those programs?
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
~~
f hy
—
A.
Q
A.
Q
nih #
6
ey Pre
‘® ;
I believe it was house-to-house.
Do you know if blood-level tests were administered?
Yes.
Do you know what percentage of children who were
interviewed or looked at were tested by blood-level tests?
A.
Q.
The numbers of children?
Percentage of all the kids that they looked at. Do
you know what percentage of them had blood-level tests
administered?
A.
them.
I remember reading the percentages; I cannot quote
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
es
Y
=
"
MR. ROSENBAUM: Q. Let me show you what was
marked in the Gregory deposition as Exhibit 3. And we've
made it part of this deposition, as well.
That’s a November 26th, 1986, program letter.
Can you just quickly take a look at that?
A. Yes.
0. Did you have anything to do with the drafting of
that?
A. Yes.
Qo. What was your involvement?
A. Getting it out.
Q. Did you do the primary drafting?
A. One of my staff did, in consultation with Dr. Goldman
and Dr. Gregory.
Q. Let me show you what’s marked as Exhibit 2.
Did you have anything to do with the drafting of
that?
A. Yes.
Q. What was your involvement?
A. I essentially wrote this letter, and Dr. Kizer added
Aa. few. things,
ww
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
pn eg Sp
Q. Did you make any attempt to summarize what was in any
HCFA transmittals regarding that?
A. No.
Q. Any reason why not?
A. Yes. Because our providers do not read long letters,
and I was trying to keep it short and simple.
; = Eel Te
A
Q. On the first page, where it says, "There is concern
that many children are not being screened"?
Yes.
Did you write that?
No. Our branch chief wrote the cover letter.
And you approved it, I take it?
We all approved it, yes.
What is the basis for that statement?
Just that.
What was the information that caused you that
concern?
A. Our figures of the testing, and the article.
Q. What would it be about the figures regarding testing
that would cause you concern that many children are not
being screened?
916/442-9151 CAT, WEST REPORTERS FAY 916/442-131n
os.
~ ” >
® ® 44
A. The areas in which the testing is being done or not
being done.
Q. What sort of figures would you expect to see that
would remove that concern that many children are not being
screened?
A. That in areas where we suspect there is older
housing, that we would have a higher level of tests.
Q. Like what?
A. Oakland, areas of Los Angeles, San Francisco.
Q. When you say "a higher level of testing," what do
you mean by that? What number are you thinking about, 80
percent, 90 percent?
A. I don't know. I haven’t developed a percentage.
Q. Has there been any talk about what sort of numbers
one would expect?
A. No, not that I am aware of.
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
Q
— aaa Staaalad A adhe aus aaa
-
MR. ROSENBAUM: Let me have marked as Exhibit 7
a several-page document, "State Medicaid Manual," dated
July 1990. It’s transmittal number 4.
[Whereupon Deposition Exhibit 7
was marked for identification.)
Q. Have you seen this before?
A. I don’t recollect this one.
Q. Do you know how, if at all, the July 1990
transmittal differed from any of the earlier transmittals
with respect to the EPSDT program and screening for lead?
A. I believe it was an attempt to clarify it.
Q. Do you know how it clarified it?
A. It clarified more of the testing, as I remember.
Q. Do you know specifically what changes, if any, were
made?
A. No.
Q. Now, you told me before, regarding the impact of
State Medicaid Manuals, I take it that you would regard
this transmittal as governing the performance of your
responsibilities; is that right?
A. These are guidelines.
QO. But, I take it, with respect to them as guidelines,
you would take them as controlling the way you carried out
your duties; is that right?
A. Yes.
Q. And looking at page 5-15, do you see the portion
that says -- do you have that in front of you? There's a
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
Re a. () ~~
{% §
A
» 47
bracket portion. Do you see where it says, "Screen all
Medicaid eligible children ages 1-5 for lead poisoning"?
A. Yes.
Q Now, do you regard that as a guideline for you?
A. Yes.
Q. and when you say you regard it as your duty to
screen all Medicaid eligible children ages one through five
for lead poisoning --
A. Yes.
Q. -- is that being done?
A. Providers are requested or guided to assess all
children for risk of lead burden.
Q. So, your answer to my question is "yes"?
A. Yes.
Q. The next sentence says, "Lead poisoning is defined
as an elevated venous blood lead level." Then there’s more
specifics.
Do you see that?
A. Yes.
Q. Do you regard that as a definition that governs the
conduct of your duties and responsibilities regarding lead
poisoning?
A. Yes.
Q. When the first sentence uses the phrase “lead
poisoning,” that’s what you understand to mean “under
these regulations” -- is that right? -- under these
Medicaid Manual provisions?
A. That I understand to mean the referral level.
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
Q. My question is a little bit different. My question
is: When you see in the first sentence, “lead poisoning,"
is the definition in the second sentence, you believe, to
be applied to the first sentence, that says, "lead
poisoning"?
A. I'm not understanding your question.
Q. When you see the words "lead poisoning" that appear
in the first sentence?
A. I don’t see the two as necessarily together, if
that’s what you mean.
Q. You don’t see that where "lead poisoning" is defined
in the second sentence that necessarily applies to the
first sentence; is that right?
A. Yes.
Q. How do you define lead poisoning in the first
sentence?
A. That children should be screened for risk of lead
poisoning. And lead poisoning itself is defined as a
venous blood level of that 25 micrograms per deciliter.
Q. Now, directing your attention to the third sentence:
"In general, use the EP test as the primary screening test."
Do you see that?
A. Yes.
Q. Do you regard that as what the program should be
doing? |
A. No.
Q. - Why is that?
~ We have been told the EP test is not a good test for
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
lead burden.
Q. You have been told that there are other blood-level
tests that are preferable; is that right?
A. Yes.
0. How has the Federal Government told you that the EP
test should not be used as the primary screening test?
A. That document says that [indicating].
Q. You’‘re referring to the CDC document; is that right?
A. Yes.
Q. But my question to you is: Has HCFA ever told you
that the EP test should not be used as the primary
screening test?
A. No.
Q. Now, prior to this February 1991 document, Exhibit
6, had the Federal Government or any branch or body or
agency of the Federal Government ever said to you that the
EP test should not be used as the primary screening test?
A. The Lead Program, but not the Federal Government.
Q. When you say “the Lead Program,” what do you mean by
that?
A. Dr. Goldman.
Q. Have Medi-Cal providers been told, at any point in
your tenure, that the EP test should be used as the primary
screening test?
A. Yes, we had told them.
When were they told?
. In 1986 they were told by this [indicating].
And they were told that -- you're referring to
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
Exhibit 3?
A. Yes.
Q. Where were they told that?
A. On page 26.
Q. Can you show me on page 26 what you are interpreting
to mean that the EP test should be used as the primary
screening test?
A. In essence, they were given the option of the EP --
Q. Read to me what you’‘re referring to.
A. "It is strongly recommended that if lead poisoning
is suspected, a venous macro blood sample (5 ml.) be drawn.
If this is not possible, four capillary tubes of blood may
be drawn: one for FEP, one for blood lead, and two extra
in case of clotting or breakage."
First, “Only those with an FEP of 35 micrograms per
100 ml. of blood or greater should have a blood lead
level.”
Q. And in Exhibit 2, were providers specifically told
that they should use the EP test as the primary screening
test?
A. Exhibit 2?
Q. Yes.
A. I believe this letter stressed more doing the venous
blood test, when the child was suspected to be at risk.
Q. So, is it now the position of the department that the
primary screening test should be the venous blood test?
A. ‘ives,
Q. You're telling me that’s been communicated to
nac aan Ana CY ~aew PYRE AT TT, TRV As Feo
3 provider
s?
(
2 A. Not officially
.
3 Q. why 1s that?
A. we're waiting
for the communica
tion about the
in referral
level.
and then we'll tell them that th
test iS not sensitive
enough tO rest for the 10 to :
milliliter
microgram
level.
Q. you're experience
d. and based on your unders
Miss Range. is it possible
to find out if 2a child 1}
poisoning
without
conducting
some sort of blood te
11 A. No.
12 Q. why is that?
oS
13 A. you may suspect it. put the plood level te
confirm
jt, which ig true of many tests.
Q. Has there ever been any investiga
tion. to
xnowledge:
ro determine
the extent t© which prov
administe
ring one blood 1evel test or another of
eligible
children
that they see? That is, has ¢
gone out and said, “You told me the EP test is
gcreening
test, and let's find out how many doc
using it as a primary screening
test"?
MR. VAN WwyYyE: I'm going to object
the Witness dot to answer.
That's clearly going tO second anc
jssues. The one we're dealing with is the fi
MR. ROSENBAUM:
Q. When you see
wprimary"
in this cransmittal
. which we've ™
Exhibit
y 2 what do you understan
d the word »
6 ala
cAL WEST REPORTERS
FAX S
percent of the time?
That that woul
e -- EPS would be the
A.
4a be -- 1 believe
th
would bP
14
1S used.
16 Q. you mean that should be the presv
17 right?
18 A. 1 guess. 1 believe SO-
19
Can we 9° off the record?
20
MR. ROSENBAUM:
Yes.
21
(whereupon
2 discussion
wa:
22
off the record.)
23
: MR. ROSENBAUM:
pack on th
24 Q. what's your understanding
as
1evated EP
25 children
can have 2 very ©
26 | what you said.
MR. VAN wyE: I presume 1
understan
ding?
~yr WEST REPORTERS
l
!
in this instance,
it's. a pre-test
for
Q. what do you mean when you say wpre-te:
A. well, it will identify
children
with
jc’s elevated,
they must be re-tested;
they
venous plood 1ead test on chem. It does NO
mean the child is 1ead-burde
ned.
Q. When you say wadditiona
l test," you
A. The blood 1ead test.
10 Q. when you S€€ in this rransmitta
l th |
11 general,”
what do you understand
that to 2 |
primary
test |
~
O
h
o
O
ww
O
o
10
11
12
3
14
15
16
17
18
18
20
21
22
23
24
25
26
27
28
\
— hn
= 2
® 3
MR. ROSENBAUM: Q. Just your understanding?
A. The EP test will be elevated with anemia. It may
not mean the child has a lead burden.
0. And that’s why what you’‘re saying is it’s important
that the primary screening test be the venous blood level
test; is that right? The other blood level test?
A. That will be the recommendation, I understand, from
CDC.
Q. And the department --
A. I only assume that would be the recommendation.
Q. Of whom?
A. Of CDC, the department.
Q. But that’s the position of the department -- is that
right? -- as you understand it?
A. Currently, either the EP or blood lead test may be
done. The provider has the option to do either test or
Q. When?
A. When the provider deems the child is at risk, or
whenever the provider wishes to do the test. The provider
has the option to do the test at any time that they wish to
do it.
Q. Do they have to request prior approval?
A. No, they do not.
Q. Have there ever been any regulations or directives
that have indicated they have to have prior approval?
A. No.
Q. Would that be an inappropriate request, to require
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
nN
7 : uy — <s a v ad TAR Teg wey REF he aE |
tems c—
\
- - - -- —— tn nr
nv In terms of ‘the risk factors that we altel SEE :
AF 3
has there been any determination as to adequacy of ‘those. 2
risk factors in determining whether or not a: Floated ri
-— on
PT a
test should be administered? How good are those factors in °
determining whether or not a blood test should be
administered? : :
MR. VAN WYE: Again, we‘re moving well into --
MR. ROSENBAUM:
understand your objection.
question here.
MR. VAN WYE:
MR. ROSENBAUM:
please.
If I move much farther, I can 4
I'm just asking a predicate
Would you rephrase the question?
Can you repeat my question,
[Whereupon the record was read back.)
THE WITNESS:
MR. ROSENBAUM:
looked into that?
A. No, I do not.
I do not know.
Q. Do you know if anybody has
Q. In terms of what does ‘take place, are providers
8 J. 3
ly 0
directed to ask specific questions with respect to exposure
to lead?
- -
-
te BLL
-
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
May I look at this [indicating]?
They are given examples here in the medical
guidelines of sources of lead that should be looked at when
doing a history -- a health history of the child and
family.
Q. You're referring to page 26 of --
A. The medical guidelines.
Q. And this is Exhibit 3 you were looking at; is that
right?
A. Yes.
Q. My question is: Are they directed to ask specific
questions?
A. They are not given specific language.
a. ———— ——— + ll tin si el ee i ® ®
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
28
MR. ROSENBAUM: Q. Now, as you see it, if
providers get a certain set of answers to whatever
screening that they do, are they then supposed to
administer a blood level test?
A. They have not been directed yet to ask specific
questions.
Can a y .
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
Q.
Miss Range, have you spoken to anyone in the Federal
Government regarding the state’s compliance with EPSDT
concerning lead?
A. Yes.
How many different persons have you spoken with?
Two..
With whom have you spoken?
Edna Ray and Bess Hiscok.
Spell the last names, please.
H-i-s-c-0-k, I think.
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
‘® ( A 43
‘ 0. Did you speak to one before the other, or both at
( 2 the same time?
3 A. Yes, Edna Ray first.
4 Q. Tell me approximately when you spoke to her.
S A. Two or three weeks ago.
6 Q. How did that happen? Were you asked to do it by
7 counsel?
8 A. No, I was asked to do it by a branch chief.
9 Q. Who asked you? |
10 A. Dr. Cumming.
11 Q. He's the person above you; is that right?
12 A. Yes.
13 Q. You placed a call to Miss Ray; is that right?
14 A. Yes.
¢ 18 Q. What did you say to her?
16 A. There were several issues we discussed besides this
17 one, clarification on the federal requirement. But we felt
18 we were in compliance with the federal, and she indicated
19 she felt we were in compliance.
20 Q. Who is Edna Ray?
21 A. The EPSDT coordinator.
22 Q.. Did you provide -- or through your talking to her --
23 send her any documents or documentation or any materials at
24 all?
25 A. I did not.
26 Q. Has anybody?
; 27 A. I do not know.
C 28 Q. Have you subsequently?
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
® i» 60
A. No
Q. Have you sent Miss Hiscok or anybody any materials?
A. I have not sent any.
Q. Do you know if anybody has?
A. I do not know.
Q. Did she ask you any questions?
A. I do not recollect.
Q. What did you say to her, as best you can recall?
A. Our procedure.
Q. What did you say your procedure was?
A. To do a good history on the child, in determining
their risk, and test when a risk was indicated -- do a
blood lead test when risk was indicated.
Q. Did she ask you questions about how often you were
administering these blood tests?
A. I do not remember.
Q. Did she ask any questions about what "when
indicated" meant?
A. No.
Q. Or what "risk®™ meant?
A. No.
Q. Did you have any discussion about any of the HCFA
transmittals? ;
A. I do not recollect any discussion.
Qs Did you say anything else beyond what we just now
discused?
A. We discussed the statewide conference. We discussed
other things that were happening in the program that were
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
® o 61
1 not related to lead.
Anything else about lead?
No, not that I remember.
Did you speak with Michael Quinn?
Frequently. I work with him.
Did you speak with Charles A. Woffinden?
No.
Have you ever spoken with him?
Have I met him?
Have you ever spoken to him about lead?
No.
Have you heard that Mr. Quinn spoke with Edna Ray?
I do not know.
oo
)
9
2
.
0
0
0
>
O
F
S
OO
»
O
O
5
0
Have you ever had discussions with Mr. Quinn about
4 15 this case?
16 A. Yes.
17 Q. Have you had discussions with him about whether the
18 state is in compliance with HCFA requirements?
19 A. No.
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
ne RT paaliia Seah aoa asl
Q. Now, this letter you are on the CC, this letter I'm
referring to, Exhibit 4?
Yes.
And did you get it on or about April 11th?
I believe it was later than that.
A week later?
I'm out of the office, and it’s difficult to tell
without checking the check-in date when it actually
arrived.
Q. Did you at any point notice any inaccuracies in this
letter?
Let me put it in front of you.
A. It was a, quote, “July ‘90 transmittal"?
Q. Yes.
A. Yes, we do not require that all Medi-Cal children
are screened through the requirements of the EP test.
Na on i
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
@
@
Q. Then, you had another conversation with another
individual?
A. Bill Hiscok.
Q. When was that one with Mr. Hiscok?
A. Tuesday.
Q. Three days ago?
A. Yes.
Q. Who initiated that?
A. I initiated the conversation in terms of the EP
test ;
Q. Did you call him, or did he call you?
A. We met at a meeting.
Q. What did you say to him?
That we were being advised not to use the EP test.
And did you also say to him that therefore this
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
A oo Ty ~~ £
@ p 65
letter was inaccurate in that regard?
—
A. That we were requesting first the assessment of risk
for children, and then testing with a blood lead test those
children at risk.
What did he say to you?
He seemed to indicate that was fine.
Q
A
QO Did he say it was fine?
A Not in so many words.
Q Did he ask you any questions regarding how you
assess for risk?
A. No.
Q. Did he ask you any questions in terms of how many
kids of the total number of Medi-Cal eligible kids that
were being seen by providers were receiving some sort of
blood lead level test?
A. No.
Q. Did he ask you any questions in terms of kids 1 to
5, how many of those kids were getting blood tests?
A. No.
Q. Did he say anything else about the administration of
the program or what you are doing beyond what you told me?
A. It was a very brief conversation.
Q. Like 30 seconds?
A. Two minutes.
Q. Can you think of anything else that was said beyond
what you told me?
A. Not on this subject. -
916/442-9151 CAL WEST REPORTERS FAX 816/442-1310
é
2
Q. Going back to what we’ve marked as Exhibit 7 -- let
me show you on the same page, where it says "“F. Vision and
ari cre "
Do you see that?
A. Yes.
Q. Now, do you regard "screens," as used in "F" as the
identical meaning as what you just told us with respect to
the first paragraph on the same page; that is, that
history?
A. You would as part of a history determine what the
patient perceives as visual or hearing problems, yes.
Q. My question may be a little different.
Are you saying that here [indicating], where
they say, "you may include vision and hearing screens,"
that what they are specifically and only referring to is a
history?
A. For the first three years of life, you essentially
rely primarily on a history for vision and hearing, with
————
(a »
El
some observation of the child, because prior to that time,
it is difficult, at least, to do a vision test.
Q. But my question to you is "F" doesn’t refer to
different ages; it doesn’t say "up to three, one protocol,
and after three, another protocol."
My question to you is: When you see the word
"screens" in "F," do you take that to mean only taking a
history?
A. No.
70
wn
a
p
—
—
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
Dd \S
la -
For kids over three years old, does EPSDT, in
construing vision and hearing screens, regarding this
transmittal, mean only to ask a history?
A. Vision and hearing are not dependant upon
environmental problems, and so they are not externally
caused -- solely externally caused. So that a vision
problem could be present that would have no environmental
cause, which is not true of lead.
. So, the answer is "no."
You mean, here "screens" means an --
A. Actual test.
Q. -- actual test. Is that right?
A. Yes.
Q. Now, turning to the next page where it says, "Dental
Screening Services."
Do you see that?
A. Yes.
Q. Do you interpret the word "screen," here, in terms
of dental screening, to mean only taking a history?
A. No, it involves looking in the mouth.
916/442-9151 CAL WEST REPORTERS FAX 916/442-1310
EXHIBIT K
IN THE UNITED STATES DISTRICT COURT
FOR THE NORTHERN DISTRICT OF CALIFORNIA
pt * HL ¥ pa
ERIKA MATTHEWS, et al
Plaintiff,
vs. No. Civ. No. C-90-3620 EFL
KENNETH KIZER, et al
Defendant.
N
s
”
Na
t”
N
i
N
u
”
N
t
?
N
w
w
a
w
t
?
“w
i
“o
it
®
COPY
pions * ¥ Lines
Deposition of
MARIDEE ANN GREGORY, M.D.
Friday, May 3, 1991
--000—-
Reported by: Cynthia Bynum Palmer, CSR No. 3556
CAL WEST REPORTERS
801-12th Street, Suite 600
Sacramento, CA 95814
(916) 442-9151
NREPORTERS/ FAX (916) 442-1310
Q. Okay. And Doctor, as I understand from your
resume here, you are Chief of California Childrens
Services branch of the State Department of Health
Services?
A. Yes, I am.
Q. And can you just very briefly tell me what your
duties and responsibilities include?
A. I oversee the operation of the California
Childrens Service branch and in that role I supervise
medical professionals as well as administrative
professionals. I am the person that gets called upon
also to make medical judgments in terms of eligibility
CAL WEST REPORTERS/916-442-9151
AT
or benefits for cases in which there is a problem or
it's not real clear to other medical consultants or
county consultants.
J
Okay. Do you know Ruth Range?
Yes, I do.
Do you have any working relationship with her?
Yes, I do.
What's that?
I serve as the medical consultant for the
CAT, WEST REPORTERS/916-442-9151
TR
3 wn
10
Child Health and Disability because they do not have a
physician on staff. Ruth Range is the Regional
Operation Chief and usually is the person that's
involved with dealing with the interface between my
program, for example, or for looking at ~-- at medical
issues.
Q. And have you worked with her on any matters
relating to lead?
A. Yes, I have.
Q. And what have those matters included?
A. Basically I was involved in the drafting of the
program letters that have gone out with respect to lead
in the last I believe four or five years.
CAL WEST REPORTERS/916-442-9151
A. The expertise that I have is that of a
0
Jd
O
O
pediatrician and I don't have any special expertise in
9 the area of lead. I have not done any writing as far as
10 published any articles or any research.
11 Q. Would you consider yourself an expert in the area
12 of lead or lead toxicology?
13 A. I would not consider myself as an expert.
CAL WEST REPORTERS/916-442-9151
x
~
~
C
h
19 MR. ROSENBAUM: Q. Do you want to modify your
20 answer?
21 A. Yes. When I was the Chief of Maternal and Child
22 Bealth at the Riverside County Health Department -- and
23 I don't recall exactly the timeframe of it, somewhere in
24 the late '70s and early '80s -- we did do a special
25 project on -- at Riverside County Health Department that
26 was funded by the State Department to look at the
27 incidence of lead and we did pretty much a universal
28 screening study at that time.
CAL WEST REPORTERS/916-442-9151
(&
V ®
Q. Okay. Did you have any specific ely Bl
with respect to that program?
A. Well, basically I was the lead person for the
county at that time.
Q. Okay. But with respect to that specific program,
did you run the universal screening program?
A. Yes.
Q. And how was that universal screening
accomplished?
A. We had -- we used the FEP and screened every
child that came through our CHDP clinics at that time.
Q. And why did you do that?
A. We did that as under the direction -- it was a
special study that was funded by the State
Department of Health Services.
Q. Okay. When you say FEP, you mean cap F, cap E,
cap P, right?
A. Yes.
Q. Were you directed to use the FEP methodology?
A. We were directed and provided equipment to do it.
Q. Did you use any other methodology for screening?
A. No. That was the screening method.
CAL WEST REPORTERS/916-442-9151
MR. ROSENBAUM: OQ. Do you know what those
letters stand for?
A. Early periodic screening, diagnosis, and treating}-
treatment.
Q. Do you have some relationship to it?
A. Yes, I do have some relationship to its
Q. What's your relationship?
A. The relationship -- I have several. One is that
I serve as a medical consultant to the California
CAT. WFST REPORTERS/916-442-9151
"
E
E
T
S
E
TO
R
W
o
m
O
y
W
n
10
11
12
13
14
15
16
17
18
19
20
2]
22
23
24
25
26
27
28
Q. Now, you told ne ust a few BomEnte 290 that one
of your relationships to EPSDT is you superintend some
of the diagnosis and treatment of individuals who have
been screened under that program. Is that correct?
A. I wouldn't quite use the word "superintend."” I
would say that the program that I'm the chief of
provides funding for diagnosis and treatment for
children that have been identified at the -- in the
screen as having potentially an eligible condition under
my program.
Q. Okay. Thank you.
Now, regarding the treatment aspect of that, in
the past year -- well, let's start since January 91, the
past several months. Do you know how many children in
the state of California have been treated for matters
relating to exposure to lead under this program?
A. No.
Q. Bave you ever made any inquiry to find out?
A. I have in the past looked under the ICD-9 codes
for lead to see if there were children that were covered
by my program. There are --— data that we have is like
two years old, so I don't have any idea what is going on
currently.
Q. When you say your data is two years old, what do
you mean by that?
A. The data of the children that are served under
the California Childrens Services program is not
"fr ANMODPC OTE _AAD-QT RT
= hy
4 EN Y
24
key-entered and available to me as state-wide data.
It's -~- it's data that's like '88, '89 right now.
0. Okay. Do you have any data for '90 or '91
regarding the number of kids who have been treated under
this program for lead?
A. No. Not yet.
Q. Has anyone made any inquiry to find that out?
A. It -- it simply isn't available yet.
Q. Okay. Is it available by area or region?
A. The data comes in on a face sheet from the
counties and then it has to be key-entered and then
analyzed and given to us in a report.
Q. And that hasn't been done?
A. No.
Q. But the data is somewhere in Sacramento. It just
hasn't been collated, printed out, whatever. Is that
right?
A. It's somewhere in the system.
Q. Okay. To your knowledge, has there been any
discussion or inquiry about, well, how many kids are we
treating in '90 and '91 for exposure to lead?
A. No.
Q. Now, you told me diagnosis and treatment. If I
asked you the same questions with respect to diagnosis,
do you also not know how many persons -- how many kids
have been diagnosed for exposure to lead in '90 and '91?
A. That's correct.
Q. You don't know that?
CAL WEST REPORTERS/916-442-9151
(,
vo
B
E
TW
BU
5
0, Pigs
A. It's the same data we're looking at. 2
Q. Okay. Do you know when that data is going to be
prepared?
A. For this year, it would be probably next year or
the year following.
Q. Okay. And just so we are talking the same
language when you talk about diagnosis:how do you define
"diagnosis"?
A. Diagnosis is when we're trying to determine
whether or not the child has a CCS eligible condition.
Q. And what is a CCS eligible condition?
A. There are a large number of conditions that are
eligible for the CCS program. They --
Q. For lead I mean. I'm sorry. Let me start my
question over. I apologize for for cutting you off. In
terms of lead --
A. Yes.
Q. -- what -- first of all, what does CCS mean?
A. California Childrens' Services.
Q. Okay. And what does it mean in terms of CCS
eligible for treatment with respect to lead?
A. For lead poisoning it would be that the child has
a lead level that's high enough that would require
treatment.
CAL WEST REPORTERS/916-442-9151
CQ
S
I
O
y
N
d
W
N
a
# v,
Do you know for '90 and -- and/or '91 how many
screenings were done for lead in the state of California
under your program?
A. No screenings were done for lead under my
program.
Q. Do you know how many screenings were done under
the EPSDT program?
A. No, I do not.
Q. Have you ever made any inquiry to find out?
A. No.
Q. Have you ever been involved in any discussion
involving the number of screenings or whether it was
believed to be an adequate number or anything like that?
Put aside the conversation with the lawyers.
A. I don't recall whether I've been in any
discussions. I know there have been things written. I
have been aware of the fact that the director was
concerned about the number of -- of lead screenings that
have been done and it was part of the articles that went
in the letter that went out to all the CHDP providers.
Q. Have you yourself ever expressed any opinion
regarding the number of screenings that have taken
place?
A. Not in public.
CAL WEST REPORTERS/916-442-9151
©
~
~
O
N
Un
p Pe
Q. What about privately? 2
A. I don't recall exactly if I have or I have not.
Q. What about generally? Do you recall?
A. No.
Q. Have you ever had any discussions with
Kenneth Kizer regarding the number of screenings?
A, No.
Q. Or any of the persons whom you told me were above
you?
A. No.
Q. And you told me you're generally aware of -- is
it Mr. Kizer or Dr. Kizer?
A. It's Dr. Kizer.
Q. Dr. Kizer. That he's been concerned about the
number of screenings?
A. Yes.
Q. And what's your understanding of what his concern
is?
A. My understanding of what his concern is is
reflected in the policy letter that went out in March.
Q. Do you know what the basis of his concern is
beyond anything that was written in that March 12
letter?
A. Well, in the letter itself, it quotes I think
from the study that was done.
Q. Okay. Did you go back -- besides the letter and
the sources referred to in the letter, do you have any
other independent knowledge of the concerns, any
CAL WEST REPORTERS/916-442-9151
concerns regarding the number of screenings taking place
in California?
Ww
N
N
A. Not specific to California, no.
fo
m
o
o
~
N
o
n
:
(
28 ly
CAL WEST REPORTERS/916-442-9151
® ®
1
2
4 k
5
6 Q. Did you make any recommendations regarding the
7 March letter?
8 A. No, I did not because it had been written by the
9 Director. | :
10 Q. Did you independently form any judgments as to
11 whether or not there are an adequate number of
12 screenings taking place in California under this
13 program?
: 14 A. No, because I don't remember how many screenings
< 15 that they have right now.
16 Q. Do you know how many were done in '89 or '88 or
17 187 or '862
18 A. No.
19] Q. Do you know how many treatments were done in any
20 of those years?
21 A. No.
22 Q. How many diagnoses?
23 A. No.
24 Q. Have you made any inquiry to find out many
25 diagnoses or screenings or treatments were made in those :
26 years?
E 27 A. No.
hr i 28 Q. Any reason why not?
CAL WEST REPORTERS/916-442-9151
ov,
® »
32
A. Mainly because it's not usually within the sphere
of what my responsibilities are on a day-to-day basis.
That is the responsibility of the other program to keep
track of what's going on within it.
Q. Okay. Regarding the EPSDT program in general,
Doctor, could you tell me, please, what you understand
to be the purpose of that program?
A. The program was established by President Johnson
as a result of a concern of the large number of draftees
that ended up coming in and not being eligible for
medical services because of having certain conditions
that could have been prevented if they had been picked
up earlier in terms of screening and so he established
the EPSDT program to try to reassure that kids got in
and got screened for potentially handicapping conditions
that could, if had been caught earlier, have been
prevented.
Q. And when you say potentially handicap conditions
that could be caught earlier or prevented, what do you
mean by that?
A. They are conditions that would respond to
treatment if -- if diagnosed earlier.
Q. And when you say "prevented," you mean prevented
in the sense of becoming serious or harmful to an
individual or more harmful for a child? Is that what I
understand that to mean?
A. Yes. I think that's basically correct.
Q. Okay. When you told me several moments ago that
Q. Doctor, regarding the EPSDT program as you've
just outlined it for me, could you tell me, please, what
your understanding is as to the purpose of the EPSDT
program as it relates to determining physical or mental
illnesses or conditions resulting from exposure to lead?
A. The purpose of the EPSDT program is to screen for
conditions, number one. Number two, if it appears on
the screening, which is only a preliminary step, that
the child may have a condition that needs treatment,
then this program is obligated to provide referrals and
follow-up for diagnosis and treatment.
Q. Okay. Now, when you say screen for conditions,
could you tell me what you mean when you use the word
"conditions"?
A. A condition could be a -- an abberation from what
one could -—- would consider as to being healthy or
normal.
Q. And what I'm interested in, Doctor, is for the
state of California in your department what do you
consider an abberation in the way you've just used that
CAL WEST REPORTERS/916-442-9151
5
B
E
E
S
rd
F-
N
o
o
=~
OO
un
ov,
b
1
35
term?
A. A deviation from normal.
Q. What is a deviation from normal with respect to
exposure to lead as your department considers it?
MR. VAN WYE: Well, let me ask a clarifying
question. Are we talking about objective manifestations
or are we talking about heightened blood lead levels?
MR. ROSENBAUM: I don't know. And I think --
wait. You asked me a question and I'll give you an
answer. All I want to know is what the doctor means
when she uses certain words.
Q. I am not using the words. I'm just saying you've
used some words, you've told me if I understand you
correctly, Doctor, that the purpose of EPSDT regarding
lead is to screen for conditions. Then I asked you what
you meant by nconditions" and you said abberation from
normal. Am I understanding you correctly?
A. Well, when we're talking about a condition, we're
talking about a medical problem that could result in the
child not being able to function as well or being ill or
potentially die.
Q. All right. And what I want to know is for your
department what does that mean in terms of lead? When
|}
does that abberation exist? when does that condition
exist?
A. I can't speak for the Department --
Q. Okay. Tell me -~-
A. -- because I'm not fully the Department.
CAL WEST REPORTERS/916-442-9151
00
N
N
a
Ou
277,
') od y
Q. Well, what's your understanding of what the
Department -- strike that.
Does the Department have a position so far as you
know as to when that abberation exists with respect to
exposure to lead?
A. I -- I do not -- I honestly do not know what -- I
would say that the position -- official position is the
one in -- which has already gone out in terms of policy
letters.
Q. You have to help me understand this, Doctor. I
want to know what you understand, if anything, is the
Department's position as to when an abberation exists
with respect to exposure to lead. When does a condition
exist with respect to exposure for lead as you've
defined those words? Does the Department have any
specific position that you can articulate for me?
A. I think that it's an area in which there is a lot
going on right now and I would not want to state what
the Department's official position is.
CAL WEST REPORTERS/916-442-9151
Q. You've told me -- I'm not trying to get you to
say anything but the truth here and what you understand
to be the position of the Department.
You've told me that it is the purpose of the
EPSDT program as you understand it regarding exposure to
lead that -- that you all are supposed to screen for
conditions. Then you defined "conditions" for me and
you used the word "abberation."®
Now, sitting here today what I'm asking you is do
you know what "conditions" or "abberation"™ means?
CAT, WFQT RREPOARTFRGS/QT1RA-449-0Q0181
CO
w
y
O
y
A
N
PA 3
What's the Department's position? &
Q. I'm asking do you know what the Department®”s
official position is or even if there is an official
position?
A. I don't know.
Q. Okay. Now, let me show you what's been marked as
Exhibit 2, the March 12, 1991, document and ask you to
please take a look at that.
Now, having that document in front of you, can
you tell me what the Department's official position is
regarding what conditions are being screened for?
A. No. I don't think it clearly articulates what --
Q. Do you know any document that does?
A. I don't know of any document that clearly
articulates what the Department's official position is
CAL WEST REPORTERS/916-442-9151
£7 ZO,
39
at this time. No, I 40 not.
Q. Thank you.
Are you familiar with the phrase "lead toxicity?
hy Yes.
Q. Can you define what your understanding of that
phrase means?
A. Lead toxicity means when lead produces some sort
of adverse effect.
Q. When you say "adverse effect," what do you mean
by that?
A. Some kind of diminution of the health.
Q. Okay. Is it your view -- strike that.
Can you cite me any professional literature or
opinion of any expert that supports that definition?
A. No.
Q. Is that the official position so far as you know
of the Department of Health Services as to what "lead
toxicity" means?
A. I don't know what the official position is.
Q. Have you ever made any inquiry to find out?
A. No.
Q. When you say "diminution," I don't want to
misrepresent your word. You said diminution of -- what
)
were the words you used please?
A. Lead toxicity occurs when the amount of lead that
the child has in some way has adversely affected their
health.
Q. Okay. And does that mean, Doctor, that lead
CAL WEST REPORTERS/916-442-9151
wo
~
N
oO
Ou
»
s
a
Ww
W
WO
10
11
12
13
14
15
16
17
18
19
20
2]
22
23
24
25
26
27
28
40
toxicity necessarily must be symptomatic?
A. It -- the question of lead -- symptomatology can
be real subtle, as if you don't have a problem. If you
don't have any kind of manifestation at all, it would be
difficult to say that there's an adverse effect on the
health.
Q. I don't want to put words in your mouth, but I
think then you're saying that if there aren't any
symptoms that are demonstrated then it's not possible to
be suffering from lead toxicity. Am I understanding you
correctly?
A. It depends on what you're screening and what you
"mean in terms of "symptoms," because there may be subtle
things that aren't terribly obvious.
Q. Such as what?
A. Such as subtle mental problems or learning
disorders.
Q. Can you give me any specific examples?
A. A diminution of IQ, for example, may not be
particularly obvious on an initial examination.
Q. Why is that?
A. Because the screening examination per se does not
do a very precise test of measuring intellectual
function.
Q. Why is that?
A. Because it is simply a screening test and in
order to measure intellectual function requires more of
a detailed evaluation.
(
Q. Sure. Can children below the age of five -- is
it possible for them to have lead toxicity, be suffering
from lead toxicity and be asymptomatic, if you know?
A. It is possible that on a screen that you would
not be able to identify a symptom.
Q. But would that mean the person's not -- could not
be suffering from lead toxicity? |
A. It is possible on the screen that you might not
find anything because of the -- of the type of screen
that's being done.
Q. Okay. And when you say "on the screen,” what do
you mean by "the screen®?
A. The -- of the -- the screen that is the routine
tvpe of screening that is done under the EPSDT program.
CAL WEST REPORTERS/916-442-9151
Q. Do you have an opinion as to the number of kids
with lead toxicity who aren't picked up by screeners
under the California prgrant
A. I don't have any opinion.
Q. Do you know the number of kids under the EPSDT
program who have been screened and been found to be
suffering from lead toxicity?
CAL WEST REPORTERS/916-442-9151
* Q
No, I do not.
Have you ever made any inquiry to find out?
No.
Do you know if anybody
I don't know.
What about in specific communities like Oakland
Wilmington or Compton? Do you know if any monitors
kids with lead toxicity have taken place?
A. I know they were the three areas I think that
were involved in the lead study that the Department did.
Q. And do you know the results of that study?
A. I can't off the top of my head give you the
percentages.
Q. Okay. Do you know how the screening was done in
those programs?
A. I don't recall exactly how they were done.
Q. What's your best understanding?
A. My best understanding is that they use blood
lead.
CAL WEST REPORTERS/916-442-9151
Ee
® » |
1
2
3
4
5 Q. Do you know why blood leads were done in those
6 communities as part of that special program?
7 A. Whenever you're assessing or truly trying to
8 evaluate whether a child has a lead problem, you to have
9 do blood lead.
10 Q. Why is that?
11 A. You can screen using other things, but blood lead
12 is the definitive test.
13 Q. Why is that?
14 A. Because the problem is lead.
( 15 Q. So explain. I'm just --
16 A. I mean how more direct can you get? If you --
17 except a blood lead?
18 Q. Okay.
19 A. If the problem is lead poisoning and you're
20 wanting to know how much lead is there, the best way to
2) find out is measure how much lead is there.
22
23 |
24 |
25 Q. Okay. Were all kids as part of the special |
26 program in Oakland and Compton and Wilmington given
£ 27 blood lead so far as you know?
\. 28 A. I don't know. To the best of my recollection, as
CAL WEST REPORTERS/916-442-9151
Ng .
47
1 -- and it's been sometime since I read the study --
that's the best of my recollection, that if you're going
to really assess whether or not the child truly has
lead, the final thing that you must do is the blood lead
because you're assessing the amount of lead that's in
the body. It makes sense that you would measure the
lead.
BD
~
~
h
n
W
N
N
pt
v
i
CAL WEST REPORTERS/916-442-9151
re es —
) J
A !
Let's mark this two-page document -- can you tell
me, there's an April 11, 1991, date. Did you put that
date on it or did that come --
MS. SLAUGHTER: That came on it I think.
MR. VAN WYE: Standard federal practice.
MR. ROSENBAUM: Okay. Let's mark this document
as Exhibit 4 and then I'm happy to take a break.
MR. ROSENBAUM: Back on the record.
Let me just ask you, have you gotten any other
correspondence from the feds besides this one?
MR. VAN WYE: No. My understanding is that we
received that from the feds in response -- we made
inquiries of the federal government, of course, and they
concur with our policy. They wrote us this letter in
response. There had been responses, correspondence or
discussions going back and forth and we understand that
there is -- the feds intend to follow up the letter
because that, obviously, is premised on a slight
misunderstanding. In fact, Linda may speak to it.
MS. SLAUGHTER: Okay. That's my understanding
too, is that they -- that the letter is not reflective
of what the Department is doing and that they were --
CAL WEST REPORTERS/916-442-9151
0
~
N
O
N
WU
»
a
s
Ww
y @
58
that they were going to send a clarifying letter or do
some follow-up and send us another letter now that they
understand what the Department is really doing.
MR. ROSENBAUM: What did they think the
Department was doing?
MS. SLAUGHTER: Well, if you read the letter, on
the second page it says -- on the second page, the top
paragraph, it says what they think the Department is
doing.
MR. ROSENBAUM: And you're referring to the
sentence that says "As we understand it, the State's
instructions to provide EPSDT services require that all
MediCal-eligible children ages one to five are to be
screened for elevated blood level -- blood lead levels
through the performance of an FEP test." Is that what
you mean?
MS. SLAUGHTER: Yes.
MR. ROSENBAUM: And the state is not doing that?
MS. SLAUGHTER: Yes. :
MR. ROSENBAUM: Do you know what that clarifying
letter is going to say in sum or substance?
MS. SLAUGHTER: My understanding was that it was
going to say we understand that our earlier letter, that
paragraph, did not -- did not accurately reflect what
the Department is -- what the Department's procedures
actually are; however, we still leave it to the
Department -- to the states to determine how they will
do a screen is my understanding of what it's going to
CAT. WFRCGT REFPNRTFRS/QTIA-4492-0Q71R
n
n
H
s
W
N
i $
59
say.
MR. ROSENBAUM: Have you had contact with
Mr. Woffinden or anyone else?
MS. SLAUGHTER: I did speak to him, yes.
MR. ROSENBAUM: Did you ask him or somebody in
his office initially to write this letter for a
statement?
MS. SLAUGHTER: I did not ask him to write that
letter. no
MR. ROSENBAUM: Do you know how this letter
happened?
MS. SLAUGHTER: I think that our clients asked
the federal government if they thought we were in
compliance and that they said that they thought we were
in compliance and they asked them that. could they tell
us in writing that they thought we were in compliance.
and that letter is in response to that request.
CAL WEST REPORTERS/916-442-9151
* ®
1
2
3
4
5 2
6 MR. ROSENBAUM: Q. Doctor. in this etter
7 there's a mention of a state Medicaid manual. I take it
8 you know what the state Medicaid manual is?
9 A. Yeah. I know what the state Medicaid manual is.
10 Q. Okay. And again, I don't mean to refer to this
11 letter. but tell me generally what your understanding of
12 what the state Medicaid manual is.
13 A. Well, my understanding is that it in general
: 14 contains information with respect to the Medicaid
© 15 program as administered in the State of California...
16 Qe ii. Okay.
17 i W And it's broad, covers all areas of Medicaid.s
1 20 To your knowledge, does the state
A ar taont of Health Services make use of the state
20 Medicaid manual?
21 A. To my knowledge. I think jthey do.
CAL WEST REPORTERS/916-442-9151
Q. And do you know in your experience of any
4
instructions that have been included within the state
Medicaid manual that haven't been complied with by the
Department of Health Services?
A. No.
So far as you know. they are complied with as
CAL WEST REPORTERS/916-442-9151
Va > %
1 fully as possible?
6 4
2 A. Yes.
CAT, WEST REPORTERS/916-442-9151
e
Q. Okay. And I take it based on your earlier
answers that you would regard whatever instructions or
directions or guidelines that are in that Medicaid
manual with respect to lead as what the state is
supposed to do. Is that right?
A. Yes.
Q. Okay. And do you remember the contents of any of
these provisions from the state Medicaid manual as
relating to lead?
A. In general. yes, I do.
CAI. WEST REPORTERS/916-442-915]1
15 Can you tell me with certainty that you saw these
16 paragraphs before today?
17 A. Not with certainty.
CAL WEST REPORTERS/916-442-9151
—
|
EY
8 Q. Are providers provided any specific directives as
9 to what questions ought to be asked?
10 A. Not to my knowledge.
19
CAL WEST REPORTERS/916-442-9151
’ ;
IA
MR. ROSENBAUM: OQ. To your knowledge has there
been any discussion about well. we should formulate some
specific questions that providers should ask?
A, Not that I can specifically recall.
CAL WEST REPORTERS/916-442-9151
Ww
N
A
D
~
3
,
OO
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
17
Q. Do you knew. Doctor, the number of
MediCal-eligible children who live in older housing?
A. No. I do not.
Q. Do you know the percentage of MediCal-eligible
children who live in older housing?
A. No.
Q. Do you -- has the Department so far as you know
or your branch of the Department conducted any inquiry
to determine the number of children who live in older
housing? And I'm getting that phrase from page 52 of
the California Physician article.
A. I know that my branch has not conducted that
study. Whether the epidemiology studies did that in
terms of their study. I think they alluded to something
like that in the article. but whether or not -- what
they did in terms of that. I have no way of knowing.
Q. Okay. Have you ever made any inquiry to find
out?
A. No. I did not.
Q. Have you ever made inquiry to find out the
numbers of MediCal-eligible children who live in older
housing?
A. No.
Q. Do you know specifically whether anybody has?
A. I don't know that.
Q. Has there ever been any discussion that that
CAL WEST REPORTERS/916-442-9151
ro 7
. »
1 would be a useful or a good thing to do?
2 A. 1 don't -- I don't know that.
3 Q. ‘When you see "older housing" in the portion of
4 the California Physician article that your pointing me
5 to. how do you understand -- what do you understand the
6 word "older" to mean?
7 A. An older housing to me would be something that's
8 over 20 years old.
9 Q. Okay. And when this -- I'm reading this from
10 this paragraph you pointed me to. "having large numbers
1} of children under the age of six." What do you
32 understand "large numbers" to mean in this context?
13 A. Would you please state what that context is?
14 0. Sure. Sure. Reading from the paragraph you
( 15 pointed me to at page 52 of the California Physician
16 article. "So far DHS has targeted screening efforts to
11 areas defined as high risk. that is. areas containing
18 older housing. having large numbers of children under
19 the age of six" and so on, and I'm asking you is what's
20 your understanding of what -- of what "large numbers of
21 children under the age of six" means.
22 A. In the context of that I can't -- I don't know
23 what they meant.
24 Q. Okay.
25 A. It's an -- that was a determination that was made
26 by whoever did the study.
27 Q. Okay. Do you know whether or not there have been
\. 28 any inquiries by your branch to determine the numbers of
CAL WEST REPORTERS/916-442-9151
0
~
~
O
O
Rp ro
| »
aw, Ae) children who live in families with 3
large numbers of children under the age of six?
A. My branch is the California Childrens Services
program and it is not responsible for the EPSDT program
and it would not be appropriate for my branch to make
that kind of an inquiry.
Qe. Do you know if anybody has done that in the State
of California?
A. I don't know.
Q. When you see -- reading still from page 52 having
large -- having -- strike that -- "having relatively
large number of ethnic minorities." what did you
understand that phrase to mean?
A. I would think that that would be a census track
in which there are a lot of Hispanics. Asians.
Afro-Americans.
Q. And when you say "large number." what do you mean
by that? More than 15 percent?
A. A significant number. Again. that's a -- in the
context of that article. I'm not sure what they meant by
"large."
Q. Okay. When you -- when you saw this article. did|
you make any inquiry as to what they meant by "large"?
A. No. I did not.
Q. Now. reading further down here. "Between .5 and 1
percent of children tested in Oakland and Los Angeles
neighborhoods had blood lead levels greater than 24
MCG/DL. and 19 percent of Oakland-studied children and 5
CAL WEST REPORTERS/916-442-9151
HEY,
4 y
: »
percent of Los Angeles and Sacramento-studied children
80
had blood lead levels greater than 14 MCG/DL."
Now. when you saw those numbers. did that concern
you at all in terms of the adequacy of the EPSDT
program?
A. Y! -- I'm -- that's a --
MR. VAN WYE: Hold on. Again, --
MR. ROSENBAUM: Let me restate that.
MR. VAN WYE: We're getting beyond --
MR. ROSENBAUM: I don't think we are. but I'm
happy to restate that.
Q. Was there any discussion between you and
Ruth Range or anybody else regarding these numbers. the
19 percent number and the 5 percent number that I
mentioned?
A. There was no discussion concerning those numbers.
no.
CAL WEST REPORTERS/916-442-9151
EXHIBIT L
(4 S. Hrc 101-36%
HEALTH CARE COVERAGE FOR CHILDREN : ——
HEARING ...
COMMITTEE ON FINANC
&" E UNITED STATES SENATE
Lg ONE HUNDRED FIRST CONGRESS
Ra
FIRST SESSION
2
re
l
be
R
o
HP
JUNE 20, 1989
3
2 i;
3
ONE” WEEK
Lec
Printed for the use of the Committee on Finance
U.S. GOVERNMENT PRINTING OFFICE
WASHINGTON : 1990
For sale by the Superintendent of Documents, Congressional Sales Office
US. Government Printing Office, Washington, DC 20402
22
Research does indicate that there is a positive response by physi-
cians when States have increased reimbursement and improved
claims processing, eligibility determinations, and scope of services.
The problems of professional liability affect access to care by all
women, not just those insured through public programs. Increas-
ingly, obstetricians and gynecologists, as well as family physicians,
are no longer providing maternity services. To address access for
the Medicaid population, we must encourage all physicians to con-
tinue the practice of obstetrics.
One proposal that could affect the willingness of physicians to
provide obstetric care will soon come before this committee, and
that is the inclusion of liability costs in the new Medicare reim-
bursement rates under the resource-based relative value scale. If
not done properly, this could actually lead more physicians to stop
providing care.
Congress should increase funding for the Maternal and Child
Health Block Grant. Clinics funded through MCH block grants are
a critically important source of prenatal care for low-income
women.
Finally, we urge the committee to support an increase in the cig-
arette excise tax. Smoking during pregnancy increases the risk of
miscarriage, of pre-term delivery, and of stillbirth. Smoking is thus
an important preventable contributor to adverse pregnancy out-
comes.
As one of the members of this committee, Senator Moynihan,
will recall from the visit he paid us at the Health Science Center at
Brooklyn, we also cannot ignore the major impact of this country’s
drug abuse and AIDS problems on having good pregnancy out-
comes.
ACOG commends this committee, and particularly its chairman,
for all of the efforts you have made on behalf of pregnant women
and their children. Much progress has been made. Much remains
to be done. And we at ACOG look forward to working with you,
Mr. Chairman, in that regard.
are prepared statement of Dr. Schwarz appears in the appen-
ix.
The CHAIRMAN. Thank you very much.
Our next witness is Ms. Kay Johnson, director of the health divi-
sion, Children’s Defense Fund.
Ms. Johnson, we are pleased to have you.
STATEMENT OF KAY A. JOHNSON, DIRECTOR, HEALTH DIVISION,
CHILDREN'S DEFENSE FUND, WASHINGTON, DC
Ms. JounsoN. Thank you.
Mr. Chairman and members of the Finance Committee, I am
Kay Johnson, director of the health division of the Children’s De-
fense Fund, and on behalf of CDF I would like to thank you for this
opportunity to testify today regarding programs that promote the
health of children.
For more than 15 years our efforts to improve programs and poli-
cies for children have included extensive work on ensuring access
to care for low-income children and their families.
23
. I would like to commend you, Mr. Chairman, for holding this
hearing to focus attention on key publicly funded maternal and
As you know, for millions of low-income
families, lack of access to needed health care has become a serious
threat. Erosions in income, family health insurance, health status,
have led to widening cracks in our health care system.
While my written testimony discusses at greater length the size
lem and the barriers to health care services which
exist, in the interest of time I would like to summarize my recom-
mendations and submit m complete statement for the record.
The CHAIRMAN. That wi 1 be done.
Ms. Jounson. Toda I will discuss reforms in the two key pro-
ams, Medicaid and [itle V, which are of particular relevance to Before 1 move to the discussion of these key publicly-funded
health programs, I would like to begin by restating our position in
Md support of the dependent care tax credit proposal.
“
ne t week, CDF testified before this committee regarding this
initiative. We view the expansion of the dependent care tax credit,
2- designed to help low-income families with children offset the cost of
of health insurance coverage, as one important component of an over-
Js all effort by the members of this committee to ensure access to
t health care for children. Specifically, we view the tax credit initia-
if tive as a complement to, a though in no way a substitute for, your
efforts to expand Medicaid.
n, For low-income children and women, Medicaid is the primary
at source of health care financing. In 1987 more than 11 million chil-
did dren under age 18 received services paid for by Medicaid. Children
it- comprised about 50 percent of all recipients, and they accoun
for only about 15 percent of all expenditures. Medicaid paid for ma-
n, ternity care for approximately one-half million births that year,
en nearly one in every six United States births.
ns The recent reforms in Medicaid have the potential to dramatical-
u, ly affect access to care for low-income pregnant women, infants,
and the youngest children; however, if we are to ensure health care
n- access, even for all poor children and pregnant women, Congress __
and the States must take additional steps to improve Medicaid in x
number of ways. Among these are the following eligibility expan
vi- sions: ;
Medicaid coverage should be provided to all pregnant women and
infants with family incomes below 185 percent of the Federal pov-
erty level, and I am pleased to note that nine members of this com-
N, mittee support such an expansion.
Second, the Medicaid program should be expanded to cover all
r children. Currently, we have millions of school-age children m who are without coverage and who are forced to go without needed
Yor medical and dental care. Provisions for such coverage have been in-
in troduced by Senator Bradley and supported by many members of
he the committee. a
| In addition, Medicaid eligibility for near-poor children over age 1
li. | should be phased in over the coming years.
oil In addition to eligibility reforms, Federal support should be
available to States to allow them to make structural improvements
in their Medicaid programs. For example, policies should be en-
24
acted which improve and simplify enrollment procedures through
modifications to resource tests, eliminations of unnecessary distinc-
tions between groups of children, requirements that States review
and redetermine eligibility before benefits are terminated, guaran-
teed annual enrollment periods, and improvements to presumptive
eligibility programs.
Reforms also are needed to enhance provider participation. CDF
supports protections for disproportionate-share hospital providers,
improvements to Medicaid reimbursement for community health
centers, efforts to ensure the provision of primary and outpatient
treatment services for children with mental health conditions, and
the study of provider reimbursement rates to allow us to plan for
further reforms in that area.
All of these reforms are included in legislation now pending
before Congress and have the support of one or more members of
this committee. In addition, as we know, President Bush has made
Medicaid a priority in the area of low-income pregnant women and
children expansions, and has worked with Senator Dole to intro-
, duce legislation which would expand such coverage.
CDF also supports the proposed reforms in the preventive health
component of Medicaid, the Early and Periodic Screening, Diagno-
sis, and Treatment Program, also known as EPSDT. EPSDT is the
most important publicly-financed preventive child health program
over Fuscted by Congress, and the benefits that it offers are unpar-
alleled.
We appreciate the interest that the chairman has shown in im-
"proving the EPSDT program through the Maternal and Child
ealth Act of 1989. There also should be improvements to the Title
V Maternal and Child Health Block Grant Program, particularly
in the areas of increased accountability, priority to all of the three
target groups within the program’s mission, and increased flexibil-
ity to demonstrate and replicate new models of care.
We are very pleased that so many members of this committee
have made a commitment to improving the health of mothers and
children. We know that you believe, as we do, that we must make
preventive investments now to ensure the health and security of
our population in the future.
Thank you.
ae prepared statement of Ms. Johnson appears in the appen-
ix.
Senator ROCKEFELLER. Thank you very much, Ms. Johnson.
OPENING STATEMENT OF HON. JOHN D. ROCKEFELLER IV, A US.
SENATOR FROM WEST VIRGINIA
I will start with a question for Dr. Schwarz.
On page 4 of your testimony you talk about low reimbursement
rates as one of the reasons why physicians don’t participate in the
Medicaid program, and you specifically mention West Virginia's re-
imbursement rate. I want to tell you there has been an update on
that; we are doing better than you indicate in your testimony. We
are up to $600, and I think that ought to be reflected.
This goes back to the question I was asking the GAO person. I
have been torn in my mind, because I was Governor of West Vir-
a
n
ad
OS
P
p
e
p
p
d
Dd
BA
Bu
d
BR
oP
Bo
OA
SN
oh
bd
ob
OB
oO
a
d
d
h
o
d
F
E
A
A
n
p
u
t
25
gh ginia for 8 years and we really have tried to push hard on expand-
ne- ing Medicaid benefits and doing more than is required by the law.
ew When services or income eligibility are optional, we go beyond
an- that, and we need to, because we are a poor State.
ive It just seems to me, on balance—and I am not asking you a ques-
tion so much, Dr. Schwarz, as I am talking to myself—that the
DF child health initiatives contained in Senator Bentsen’s bill and
rs, also, of course, in Senator Bradley's bill, are so compelling that
Ith even States like West Virginia, that have massive financial prob-
ant lems and too many poor children have to do better. We have to do
nd better. I am not sure how we can afford to do better, but we have
for got to find a way to do better.
So, I want to cosponsor this bill, and I am very proud to do it,
ng even as I am proud of what West Virginia, against unbelievable fi-
of nancial odds, been doing. But still, we have to do better. %
de Nevertheless, I want to set the record straight in terms of gs
nd own testimony.
I do have a question. There have been a lot of articles about the
scarcity of doctors delivering babies, and there has been a lot of
talk about malpractice. Would you clarify something for me? Is it
th i more a matter of where it is that those doctors are racticing, that
he there is a shortage in some areas? Are there, in fact, fewer OB-
wn GYNs in this country practicing today than there were 10 years
ar- ago? Or is that they are practicing in certain areas and not practic-
ing in others? It relates not only to malpractice and the effect of
in that, but also hy the substance of the argument that there
ild aren't enough O Ns.
tle Dr. Schwarz. Senator, in my own State of New York where we
rly have surveyed obstetricians and gynecologists, it is not that they
oe are dropping the practice entirely, although some are retiring ear-
il. lier than they had anticipated, but many are dropping obstetric
ractice as a part of their practice of medicine, and others are lim-
oe iting the number of high-risk pregnant women that they take care
of in their practices.
” All of that leads to a reduced number of providers available
of That is most acute for the Medicaid population, but in the Ure )
rural areas of New York, there are counties with no obstetrici g
gynecologists, or at least no obstetrician-gynecologists who are pro-
5. viding obstetric services. So, I think the data is real.
Senator ROCKEFELLER. You have spoken of New York. I am
asking on a national basis.
Dr. ScHwARz. I think surveys would indicate, also, on a national
basis similar trends—that is, to retire early, for those physicians B approaching retirement; to give up obstetric practice but continue
necologic practice. In our testimony we have shown the differen-
tial insurance rates. For example, in States like Florida the differ-
nt ential is just enormous for those who provide obstetric care and
ne those who don't.
e- So I think these trends are national by our survey information.
n Senator RockxrELLER. Thank you.
fe [The Jrovare) statement of Senator Rockefeller appears in the
appendix.
I nator ROCKEFELLER. Senator Chafee”
r- | Senator CHAFEE. Thank you, Mr. Chairman.
194
OUTREACH
Any effort to provide increased funding for a variety of outreach activities for
pregnant women would be welcome by states. Enhanced funding would provide in-
centive for those states that have not yet undertaken such activities, and would
allow the many states that have begun such efforts to build upon, and expand exist-
ing programs.
INPATIENT DAY LIMITS/ REIMBURSEMENT
I am pleased to say that many states have moved to unlimited inpatient days
under Medicaid and have capitated payment systems that account for catastrophic
costs resulting from biowiiikt v 3 lengths of stay, which addresses part of the concerns
of disproportionate share hospitals.
States a disproportionate share payment is an appropriate public policy for
hospitals that have a commitment to serving the poor. However, states that contin-
ue to have a cap on inpatient hospital days are concerned about efforts to further
eliminate that cap for older children served in disproportionate share hospitals.
States believe there are equity considerations involved in such a mandate. Eliminat.
ing amount and durational limits for one specific subset of the total Medicaid popu-
lation indicates that one population is more inportant than another within the
same program. There is also concern about the effects such a mandate might have
on access to inpatient services in a geographic area. In addition, there are also cost
considerations that will impact the program as a whole.
881 CHILDREN AND MEDICAID ELIGIBILITY
Related to children’s health and the Medicaid program is the issue of SSI eligibil-
ity. States have a growing concern for SSI children who loose Medicaid eligibility in
particular months when their parents may have income in excess of SSI standards
due to i lar pay periods. ile the children are reinstated in the program sev-
eral weeks later, this temporary discontinuance of coverage can have substantial ad-
verse impacts. There are also agency administrative considerations involved in re-
moving a child from the rolls, and then reinstating them several weeks later. States
fully support any efforts this Committee would undertake to allow consideration of
annualized income for SSI eligibility where an irregular pay period would result in
temporary termination.
SUMMARY
In summary I would say that states, in general, are ually izant of the Job.
lems and need for change. States have been making good faith efforts to expand and
expedite eligibility, increase outreach, and educate about wellness to combat in-
creased infant mortality. We remain unconvinced, however, that mandating further
incremental expansions and reporting requirements at this time constitutes a realis-
tic solution. Further mandates at this time will have significant implications for the
whole of the Medicaid population in different states.
The APWA has given the issue of access to health care serious consideration over
the past two years and has published a set of proposals for broader reform. We are
aware that our proposals do not constitute the ultimate resolution to all the health
care problems, but we believe they are a substantive place to start.
I would like to stress that states want to work together with Congreesional lead-
ers and their staffs to develop a set of viable pro Is based on what we, together,
know at this point. It is clear that something n to be done.
Our system of governance is based on federal/state partnership. That partnership
must be evaluated, in the context of the Medicaid program, and built upon in order
turn our nation’s health care situation around.
Thank you for the onportunity to testify today.
PrEPARZD STATEMENT OF KAY JOHNSON
Mr. Chairman and Members of the Committee: My name is Kay Johnson, and I
am the Director of the Health Division of the Children’s Defense Fund (CDF). On behalf of the CDF, I want to thank you for this opportunity to testify today regard-
ing programs which promote the health of children. CDF exists to provide a strong
and effective voice for the children of America who cannot vote, lobby, or speak for
themselves. We pay particular attention to the needs of low income and minority children. For more than 15 years, our efforts to improve programs and policies for
195
children have included extensive work on reforms in the Medicaid and Title V Ma-
ternal and Child Health Programs. ;
I want to commend you, Mr. Chairman, for holding this hearing today to focus
attention on our key publicly funded maternal and child health programs. For mil-
lions of low income families, lack of access to adequate needed health care has
become a serious threat. Erosions in family income, health insurance, and health
status have led to widening cracks in our health care system which the current pro-
grams have been unable to fill.
While my written testimony discusses at greater length, the size of this problem
and the barriers to-health care services which exist for children and families, in the
-interest of time, I will briefly summarize the recommendations it contains. Howev-
. er, I would like to submit a complete written statement for the record.
I. WHAT\2® THE EXTENY OF HEALTH INSURANCE COVERAGE FOR CHILDREN PREGNANT
WOMEN?
In recent years, the problem of uninsuredness has been growing. Children are es
pecially likely to be uninsured as a group—representing approximately one-third ok,
the more than 37 million uninsured Americans under age 65." As a result of re,
tions in coverage under employer-based health insurance plans and reduction
Federal and state public insurance programs for low-income children, fewer chil-
dren today have health insurance coverage.
Poor children, whose (amilies generally lack the means to pay for health care ex-
penses “out-of-pocket” are among those most likely to be uninsured.
* Between M80 and 1985, the proportion of children under age 18 covered by em-
ployer imsurance fell by 6 percert<«from 64.6 percent to 60 6 percent). Among poor
children under age 18, the proportion privately covered declined by onequarter,
from 16.9 percent to 12.8 percent.?
* In 1986, nearly one out of every 5 children in families over 11 million nation-
wide—had no health insurance, public or private.’ (Table 1)
* By 1986 nearly one-third of all poor children were completely uninsured. This
translates into 4 million poor children nationwide. While an estimated 1 million to
1.5 million children have been added to the Medicaid program since 1986, the re
maining 2.5 million to 3 million lack the key to access to health care—insurance.
* In 1986, more than 4 out of every 10 children in employed poor families had no
health insurance public or private. (Table 2, Figure 1) These children have tradition-
ally been left outside of the scope of the Medicaid program and, increasingly, their
families lack employar-based dependent coverage.
In fact, the absence of health insurance, public or private, is most clearly seen in
low income working families. Children in low income working families are less
likely to have access to employer-based family coverage, and yet nonetheless are ya.
likely to be eligible for Medicaid. Many children in such families could be classi
as “near-poor’ (with family incomes between 100 and 200 percent of the Fede
poverty level).
* In 1986, nearly 3 out of 10 children in near-poor families had no health insur-
ance. (Table 2A, Figure 2)
* In that year, just over half of near-poor children-had private, employer-based
health insurance coverage. Moreover, among this group, the full cost of the chil-
dren’s premiums was covered by the employer or union in only 32 percent of the
cases
The best way to ensure that a child will begin life as healthy as possible, is to
ensure the health of the mother during pregnancy through prenatal care. Women of
childbearing age need access to health care, especially during a pregnancy. Yet in-
adequate health insurance coverage acts as a barrier to health care for women.
* Among women of childbearing (15-44 years), 9.5 million had no health in-
surance, public or private, in 1985. If women who have some health insurance but
lack adequate maternity care coverage were included, then over 14 million women
were completely unprotected against the cost of maternity care in 1985.4
While recent Federal changes in Medicaid ensure coverage of all poor pregnant
women beginning in 1990, millions of near-poor women continue to be uninsured or
underinsured. These women, generally young, married, and in a employed family
with an annual income of just under $20,000, are most typical of those who Nive
birth today.*
196
Il. WHAT IS THE RELATIONSHIP BETWEEN INSURANCE STATUS, HEALTH CARRE UTILIZATION,
AND HEALTH BTATUS?
Study after study has shown that health insurance is a significant determinant of
health care utilization. The uninsured use substantially fewer services than their
insured counterparts, even when health status and the need for services is taken
into account.® Research also has shown that even among the poorest families, pub-
licly-funded health care coverage can bring health care utilization up to average
levels.”
e National survey data reveal that low-income uninsured children have a lower
likelihood of, and a significantly lower average of, visits to physicians. When adjust-
ed for health status, uninsured children remain most likely to have no physician
visits in a re
* Even biol children with identified disabilities whe icipate in special edu-
cation pregrams, lack of health insurance has been fo $0 be associated with re-
duced access to necessary health care.®
e However, r children with Medicaid coverage are far more likely than unin-
sured poor children to have a regular source of health care and te visit a ph
in a year. Medicaid recipient children use services in a pattern similar to that to
their affluent, privately insured counterparts.'®
e Uninsured low income women are less likely to receive care early in pregnancy
and are twice as likely to receive late or ro prenatal care.!!
At the same time, research indicates the extent to which adequate access to
health care is critical to maternal and health and saves money by preventing unnec-
essary illness, disability, and death.
Maternity care, beginning with prenatal care in the critical first three months of
pregnancy and continuing threugh the birth of a child, can dramatically improve
maternal and infant health. An infant born to a women receiving no prenatal care
is more than 3 times more likely to die in the first year of life.'* Prenatal care can
save $3 for every $1 invested.'® Yet each year, millions of infants are born to
women who did not receive early care.
* In 1986, about one in four babies nationwide was born to a mother who did not
benefit from early care. (Table 3)
* In that year, only 68 percent of all births occurred among mothers whose prena-
tal care could be considered adequate, even in terms of timing and frequency of
visits.
* That year marked the seventh in a row in which the trend in receipt of late
(beginning after the sixth month) or no prenatal care worsened or showed no im-
provement. In 1986, 70,000 infants were born without benefit of any prenatal care.'®
The Institute of Medicine of the National Academy of Sciences reports that “fi-
nancial barriers—particularly inadequate or no insurance and limited personal
funds—were the most important obstacles reported in 156 studies of women who re-
ceived insufficient care.” !* From New York City to Oklahoma City, these studies
document the financial barriers which keep women from receiving early and ade-
quate prenatal care.
Immunizations, beginning in the first months of life, can eliminate the death and
disability that can Fa from now- foventable, childhood diseases such as measles,
mum rtussis (whooping ), diphtheria, tetanus, polio, and meningitis.
Childhood i immunizations save $10 for every $1 invested.!” Inadequate immuniza-
tion levels lead to outbreaks of preventable disease. However, between 1980 and
1985, immunization levels for our nation’s infants and toddlers eroded substantial-
ly.'® (Table 4, Figure 3)
. In 1985, the proportion of infants younger than one with at least one dose of
polio or diphtheria, tetanus, and pertussis ( ) vaccine was lower than in 1980.
Among all nonwhite infants, the proportion receiving at least one dose of polio vac-
cine fell by more than 20 percent, while the proportion receiving at least one dose of
DTP vaccine fell nearly as sharply.
e Because the 1985 DTP immunization status of children who had reached age
one showed some improvement, it appears that some families may have delayed im-
munizations and ‘caught up’ later. This places many infants at unnecessary risk
for preventable disease.
* Two-year-olds experienced erosion in immunization status in each vaccine cate-
govy. The overall pattern indicates a significant decrease in the immunization status
0 two-year-olds.
Comprehensive primary and preventive care for children can detect and treat a
wide range of health conditions before ‘they become serious. Screening for lead poi-
197
soning, learning disabilities, vision impairments, and dental health needs can
reduce the co uences of these health problems. Children who receive comprehen
sive primary health care have annual health costs 7 to 10 percent lower than those
who do not. However, many children do not receive such preventive care. :
« In 1986, as a result of inadequate access to health care, poor children were con-
siderably more likely than affluent children to have had a routine physical in the
previous year.'®
« National surveys indicate that poor children are at least 3 times more likely
than affluent children to have never had a physician visit (5.4 percent and 1.6 per-
cent, respectively).*®
We understand how to keep most children healthy. We know that every child
needs health care. Good medical care begins before a child's birth with comprehen-
sive prenatal care. It continues throughout childhoed, with care for a child's preven-
tive, acute, and chronic health care needs.
No child—whether the need is for immunization, treatment for a strep throat,
dental care, hospitalization, medicines, or eyeglasses—should go without health care
because a family cannot afford it. No pregnant woman shouid be denied prenatal
care because she does not have enough money to pay for it.
The current gaps in insurance Soversie and medical care among chigha are
costly in both human and fiscal terms. aternity and pediatric services een
found not only to be effective but also to be a remarkably cost-effecti ype of
health care investment. Our highly sophisticated medical system can offer preven-
tive or remedial care for most child health problems. Yet a series of events have left
our children vulnerable to preventable childhood disease, disability, and death.
11. WHAT POLICY REFORMS ARE NEEDED TO IMPROVE THRE ADEQUACY OF PUBLICLY-
FUNDED PROGRAMS PORILOW INCOME FAMILIES, ESPECIALLY CHILDREN
In recent years, Congress has<aken steps to improve access to health care for
pregnant women, infants, and wehildren. These _preventive investments inchude
changes in key maternal and child. health programs such as Medicaid, the Title V
Maternal and Child Health Block Grant, Community and Migrant Health Centers.
childhood immunization, and health manpower programs. I will discuss reforms in
the two programs, Medicaid and the Title V Maternal and Child Health Block
Grant, which are of particular relevance to the work of this Committee.
A. Medicaid
For low income children and women, Medicaid is the primary health care financ-
ing program.
e In 1987, more that 11.6 million children under age 18 received services paid for
by Medicaid. Children comprised 50 percent of all recipients.
* Despite its pork , Medicaid still failed to reach all poor children in 1987
Furthermore, chil account for only approximately 15 percent of the total ex-
penditures.
™\
o Medicaid paid for maternity care‘for approximately one-half million 3 Ahat
year—nearly one in every six U. 8. births.
Moreover Medicaid is a unique in its mission to serve a broad range of]
medically indigent individuals an families. It is the only publicly funded health
program sufficiently elastic to permit the development of both a rationalized mater-
nal and child. bealth system and a.basic system of long term care for the elderly and
disabled. The most notable aspect of the Medicaid reforms we have witn over
the past five years is precisely that they have been responsive to the needs of many
categories of program beneficiaries, not just one or two. This unified and incremen-
tal approach to health policy development is a sound and sensible one. CDF strongly
supports this unified approach.
et despite recent improvements, the Medicaid program continues to fall far
short of fulfilling its mission to address the health care needs of r Americans
Over 50 percent of all poor Americans, and between one-third and one-half of our
poor children did not qualify for Medicaid last year. Strict eligibility rules, difficult
enrollment procedures, limitations on benefit packages which vary widely from
state to state, and low provider participation levels together create significant bar-
riers to access.
Because of the size and scope of the program, recent reforms in Medicaid have the
tential to dramatically affect access to care for low income pregnant women, in-
ants, and the you children. However, if we are to ensure health care access
even for all poor dren and pregnant women, Congress and the states must take
198
additional steps to improve Medicaid in a number of ways. These include the follow-
ing:
1. Eligibility Expansions
* Medicaid coverage should be provided to all pregnant women and infants with
family incomes below 185 percent of the Federal poverty level. Expansion of eligi-
bility to all pregnant women and infants with family incomes below 185 percent of
the , Br fon poverty level will make coverage available to approximately two-thirds
of all uncovered mothers and infants.
* The Medicaid program should be expanded to cover all r children. There is
no magic which protects children over age 6 from acute and chronic health condi-
tions. Currently, millions of school age children are without coverage and are forced
to go without needed medical and dental care. This type of neglect can lead to
school failure and preventable disability. A phased-in mandatory ex ion of Med-
icaid coverage could lead to a one-third reduction in the number of uninsured chil-
dren. Moreover, states should be given the option to cover all poor children begin-
ning in FY 1990.
* Medicaid eligibility for near-poor children over one should be phased-in
over the coming years. The families of near-poor children are more likely to be
working, but without employer provided coverage and unable to afford private cov-
erage for their children. As a result, these families need access to publicly-funded
goyerags Provisions for such coverage are included in S. 839 as introduced Ly Sena-
tor Bra , ;
o Allow states the option of extending Medicaid to children In non fedecuily
funded foster care placements with family incomes below 100 percent of the Fed-
eral poverty level. Many children in non-federally funded foster care nonetheless re-
ceive Medicaid because their incomes and resources do not exceed the AFDC guide
lines. However, a handful of children (for example, children receiving Social ri-
ty Survivors’ benefits) have income slightly over the AFDC eligibility level but
under the Federal poverty level. These children currently cannot qualify for Medic-
aid. States that do not opt now to extend Medicaid to-all poor children under 18,
nonetheless might elect to provide coverage to this subclass of poor children. S. 949
as introduced by Senator Riegle proposes to extend coverage to this group.
* Prohibit * ion 209 Si states from denying medical assistance to SSI
qualified children with disabilities. Between 6 and 7 states that are socalled “Sec
tion 209 (b)” states present] Sategorically exclude disabled children from their Med-
icaid programs, even though they meet SSI standards and would be eligible for cov-
erage as adults. We believe that correcting this problem is virtually no-cost, since so
few children are affected.
8. Administrative Reforms
Federal support should be available to states to allow improvement of their Med-
icaid programs in a number of ways. For example, policies which improve and sim-
plify enrollment procedures or enhance provider participation will allow more preg-
nant women, infants, and children to receive cost-effective primary and preventive
health services.** Moreover, these are low cost initiatives which make Federal and
state eligibility expansions meaningful for families at the local community level.
* Modify resource and asset tests to allow more poor pregnant women and chil-
dren to become eligible. for Medicaid. Low income working families need basic
household goods and automobiles which allow them to travel to work. They should
not be penalized for having such resources. We support the elimination of punitive
resource tests for pregnant women and children in low income families.
* Eliminate the distinction between “qualified” children and “poor” children. As
mandatory eligibility for poor children expands, there is little reason to retain a
SDETouD class of very r children known as “qualified” children (Section
1905(nX2)). This situation leads to confusion at the Federal, state, and local level.
* Require states to redetermine eligibility for children enrolled in the program
before benefits can be terminated. The Family Support Act of 1988 contains impor
tant protections specifying that before Medicaid benefits can be terminated in the
case of affected families the eligibility for continued benefits of the children in the
household must be redetermined to ensure that they do not remain continuously eli-
gible under another classification. As Medicaid eligibility for children is expanded,
the need for redetermination protections also grows.
* Structure an option for guaranteed annual enrollment periods which aliow
_ children to be continuously enrolled in Medicaid. The on n, off-again nature of
Medicaid enrollment not only creates a barrier for the family seeking access to
ventive and primary health care, it also discourages providers from accepting Med
199 $0
icaid program porticipants, Annual enrollment periods would be a big step toward
llow-
reducing these barriers. :
* Improvements and expansions to the presumptive eligibility programs. Cur-
rently, states have the option to extend presumptive” or temporary eligibility to
with pregnant women through a network of qualified providers. We recommend expan-
ligi- sion of this option to allow infants and children to benefit from such systems. Re-
at of ports from acroes the country document the tragedies which have resulted from
rirds delays in children’s eligibility determinations
. vide protections for the disproportionate share hospital providers furnish-
re is ing extended inpatient services to children. Consistent with 1988 amendments,
ndi- which allow an adjustment in payment for hospital services for infants, dispropor-
roed tionate share hospital facilities should be provided with adjustments to reimburse
d to ments in the case of children younger than 18.
Med- e Improve Medicaid reimbursement for providers meeting the requirements of
chil- Section 330 and 329 of the Public Health Service Act. The network of more than
gin- 500 federally funded community and migrant health centers who furnish primary
care to all poor and publicly insured patients in their communities are now using
d-In millions of dollars in scarce Federal discretionary funds to defray the gap between.
> be the cost of care furnished to Medicaid beneficiaries and the amount Medicaid ay )
cov- ally pays. We estimate that in 1988 this “gap” amounted to about $45 million —s? ;
ded cient funding to serve more than 400,000 additional low income persons. Senator
ona- Chafee has introduced legislation (S. 1199) with provisions designed to close this gap.
« Improve the capacity of Medicaid programs to ensure the provision of pri-
all mary and outpatient treatment services for children with mental or developmental
Fed- illness or conditions. Many such children routinely receive services in clinical set-
y re- tings where there is a range of Professionals skilled in the diagnosis, evaluation, and
ide- treatment of these types of health problems. However current law does not allow a
uri- clinic to be reimbursed if it is directed by a non-physician licensed practitioner (such
but as a poychiologiat or psychiatric social worker). We recommend that an exception to
dic- this rule be made for clinics serving children with developmental or mental health
18, needs.
949 3. The Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) Pro-
gram
vin EPSDT is the most important publicly financed preventive child health program
lod ever enacted by Congress. The benefits it offers are unparalleled. Yet, except for a
Ov. single sentence, the statute is virtually silent regarding the structure and content of
» 50 the health benefits included in the p . Moreover, the terminology used in the
current definition of EPSDT is extremely outdated.
Mr. Chairman, we appreciate the interest you have shown in improving the
EPSDT program through plans for legislation to codify, clarify, and expand the
od- scope and depth of the program. The x in i elements of EPSDT reform are essen-
im- tial and would remedy problems which have plagued the program for more than
og- decade. )
iv » Codification of the current EPSDT regulations. The Medicaid statute curren
only refers to EPSDT in one sentence. This program and the protections it provides
are too important to be left to the rulemaking process alone.
hil e Clarification of the independent nature of the four basic components of
sic EPSDT. These include: (1) health and developmental examinations, diagnostic pro-
ald cedures, and treatment; (2) vision examinations and treatment; (3) assessment, diag-
ive nostic and treatment services for hearing problems; and (4) preventive and restora-
tive dental care.
As » Expansion of the range of d tic and treatment services which may be
a provided to a child following an EPSDT assessment. States have long had the
on option to provide an enhanced benefit package to children with conditions disclosed
el. by an EPSDT assessment. Creating a national benefit kage, which would allow
. providers to deliver a broadened range of diagnostic and treatment services deemed
~ medically pecesary through their assessment, would be a giant step forward.
hue e Clarification that families can elect to receive either some or all of the compo-
he nents of an EPSDT assessment and treatment program. There currently is wide
1i- spread confusion around the issue of whether providers are allowed to provide only
a portion of EPSDT screening and treatment. Since few providers are capable of fur-
nishing all elements of the assessment, in many communities no provider is willing
to offer EPSDT-quality services. It also keeps out of the program scores of highly
qualified providers specialized in one or more aspects of the program. Finally. any
other inte tion contradicts years of Federal policy Sook hi state administra-
tion of E and Federal rulings. “
7
2
s
&
200
B. Title V Maternal and Child Health Block Grant
For over 50 the Title V Maternal and Child Health programs have served
America’s mothers, infants, and children. As the only Federal health program ex-
clusively focused on maternal and child health, Title V serves as a cornerstone of
our public health system. Each year, the rovides maternity care to hun-
dreds of thousands of pregnant women and preventive and primary care to millions
of children. In addition, from the beginning, Title V has included in its mission serv-
ices for children with special health care needs.
However, as with all programs, periodic revisions are necessary to keep the pro-
gram in step with the times. We hope that this Committee will-make improvements
to Title V in the following areas: :
* Increased accountability: Improvements in fhe planning and reporting procees-
es, as well as creation of a state level advisory board, would allow Title V programs
to better document unmet need and program success. ‘
* Commitment to all three target groups within the programs mission: Materni-
ty and infant care, primary and preventive health care for children, and services to
children with special health care needs are all priorities in maternal and child
health. While it may be easier at times to document the problem of infant mortali-
ty, children need health care throughout childhood. Moreover, millions of regnant
women, infants, and children live in medically underserved areas where y a pub-
licly funded progreny like Title V is likely to reach them, even if they have a Medic-
aid card. It is essential that the program place emphasis on service to all three
groups.
° Flexibility to demonstrate new models of care and replicate models on a na-
tionwide basis: Title V has a special advantage in that it contains a provision for
funding special projects of regional and national significance (SPRANS). The oppor-
tunities to test the advantages of home visiting programs, new genetic screeni
and treatment systems, techniques for better serving children with special heal
care needs in the community, and other models are essential to the development of
a better system of care for all mothers and children.
OONCLUSIONS
We are very pleased that so many members of this Committee, eluding the
Chairman, have made a commitment to improving the health of mothers and chil-
dren. Likewise, we are pleased that President Bush has made Medicaid coverage for
low income pregnant women and children a priority. We know that you believe as
we do that society “should ensure that the basic needs of vulnerable Americans do
not go unmet,” *3 that we must make preventive investments now to ensure the
health and security of our population in the future. ;
REFERENCES
1. Chollet, D., Uninsured in _the United States: The Nonelderly Population Without
Sealeh Insurance, (Employee Benefit Research Institute, Washington, D.C.), October,
2. National insurance statistics for 1980 and 1985 are based on published data
from the U.S. Census Bureau, calculations by CDF.
8. These and other 1986 national insurance statistics for children are based on un-
published data from the U.S. Census Bureau, calculations by CDF.
No flan Guttmacher Institute, Blessed Events and the Bottom Line, (New York,
b. Ibid.
6. Butler, J., Winter, W., 8 , J., et al, “Medical Care Use and Expenditure Among Children and Youth in United States: Analysis of a National Probability Sample,” Pediatrics, 76:495-507, 1985.
7. Newacheck, P. and Halfon, N., “Access to Ambulsion Care Services for Eco- nomically Disadvantaged Children,” Pediatrics, 78:813-819, 1985.
8 Indurance Coverage
. Rosenbach, M. ‘and Ambula Medical Care of Low- Income Children, United States, 1980,” Nationa! Medical Utilization and Ex- pesditure Survey, (DHHS Pub. No. 85-20401, National Center for Health Statistics),
'9. Singer, J., Butler, J., and’ Pal , J., “Health Care Access and Use Myssk Handicapped Students in Five Public Systems,” Medical Care, January, 1
10. Rosenbach, op.cit. i
11. Alan Guttmacher Institute, op.cit. hy 12. Healthy People: The Surgeon General's Report on Health Promotion and Die ease Prevention, D Pub. No 70-56071 (Hyattsville, MD) 1979.
le
.
’
201
13. Institute of Medicine. Preventing Low Birthweight, (National Academy Press,
rved Washington, DC) 1985.
2 ex- 14. Hughes, D., Johnson, K., Rosenbaum, 8., and Liu, J., The Health of America’s
ve of Children: Maternal and Child Health Data Book, 1989, (Children’s Defense Fund,
hun- Washington, DC) 1989.
lions on 15. Ibid.
serv- gr | 16. Institute of Medicine. Prenatal Care, (National Academy Press, Washington,
RB, DC) 1987.
pro- HE ke 17. Office of Technology Assessment, Healthy Children: Investing in the Future,
ents a (U.S. Congress, Washington, DC) 1988.
3 18. Johnson, K., Who's Watching Our Children's Health: The Immunization Status
of America’s Children, (Children’s Defense Fund, Washington, DC) 1987.
19. Dawson, D. and Adams, P., “Current Estimates from the National Health
Interview Survey, United States, 1986,” Vital and Health Statistics, Series 10, No.
164, (DHHS Pub. No. PHS 87-1592, National Center for Health Statistics), 1987.
20. Ibid.
21. Hughes, et al. Children’s Defense Fund, op.cit.
22. Rosenbaum, S., Testimony before the U.S. House Energy and Commerce Com- ™
mittee, Subcommittee on Health and the Environment, regarding Provider Partici-
pation in the Medicaid Program, February 8, 1989.
23. Bentsen, L., Interview published in Hospitals, May 5, 1989.
EXHIBIT M
|. MEDICARE and MEDICAID
NUMBER 596 OCTOBER 5, 1989
—EXTRA EDITION—
Omnibus ~~
Budget Reconciliation Act
of 1989 -
H.R. 3299
Report of the
House Budget Committee
September 20, 1989
9
A
T
T
Explanation of the Energy and Commerce ;
and Ways and Means Committees
Affecting Medicare-Medicaid Programs
CCH Special 1
4 Extra copies of this Extra Edition are available from Commerce
Clearing House, Inc., 4025 W. Peterson Ave. Chicago, Illinois
60646. Price: 1-4 copies, $5.00 each; 5-9 copies, $4.75 each; 10-24
copies, $4.50 each; 25-49 copies, $4.00 each.
COMMERCE. CLEARING, HouseE, INC..
TULIALALLLL LRA AR ARR AR AAR WR AW AALRALRR ANAL AL ARR ALARA ALARA ARRAY SANNA La
Setting the standard since 1913
4025 West Peterson Avenue Chicago, inois 60646
-
a
a
Sr
. aii a Se Ra -
:
7 o
%
4 :
: H te
:
- o »
: . CE Dh A - * .
Sia oy ~ . = .« » - vv. = ee 3
39%
: cient time for a mother to make the transition from welfare to a
{ job that offers health insurance coverage for her and her children.
To further encourage welfare families to work. the Committee
bill would allow the States, at their option, to extend the current
“3. month transitional coverage period for 2n additional 12 months
: or 3. 6. or 9 months, as the Brace elects). Thus, a State could offer
a working welfare family a total of 24 months of transitional Med-
caid coverage (12 mandatory, 12 optional). Under the bill, the
structure of the current mandatory benefit would remain un-
changed. Thus, States could. at their option, impose the same
income-related premium during this optional 12-month period that
they are allowed to impose during the 2nd mandatory 6-month
period. The Committee bill would also repeal the sunset.
The Committee bill would also make some technical corrections
to current law. It clarifies that Medicaid transition coverage termi-
nates at the close of the first month in which the {amily ceases to
include a child. whether or not the child is a dependent child under
part A of Title IV, or would be if needy. The Committee bill also
clarifies that families who, prior to April 1, 1990, are receiving
Medicaid extension coverage under the current law 9-month provi-
sion are entitled to continue receiving this extension coverage after
that date until their 9-month coverage period expires.
a
P
R
E
p
w
s
E
P
n
d
e
.
S
e
w
Section 4213—Early and periodic screening, "diagnostic, and treat
ment services
(a) In general. —Under current law, States are required to offer
early and periodic screening, diagnostic, and treatment (EPSDT)
services to children under age 21. States are required to inform all
Medicaid-eligible children of the availability of EPSDT services, to
provide (or arrange for the provision of) screening services in all
cases when they are requested, and, to arrange for (directly or
: through referral to appropriate agencies or providers) corrective
treatment for which the child health screening indicates a need.
The EPSDT benefit is, in effect, the nation's largest preventive
health program for children. Each State must provide, at a mini-
mum, "0h following EPSDT services: assessments of health, devel-
opmental, and nutritional status: unclothed physical examinations;
‘mmunizations appropriate for age and health history; appropriate
vision, hearing, and laboratory tests; dental screening furnished by
direct referrals to dentists, beginning at age 3; and treatment for
vision. hearing, and dental services found necessary by the screen-
ing. These services are available to children under EPSDT even if
they are not available to other Medicaid beneficiaries under the
State's plan.
The EPSDT benefit is not currently defined in statute. In the
view of the Committee, as Medicaid coverage of poor children ex-
pands, both under current law and under the Committee bill, the
EPSDT benefit will become even more important to the health
status of children in this country. The Committee bill would there-
fore define the EPSDT benefit in statute to include four distinct
elements: (1) screening services, (2) vision services, (3) dental sery-
ices, and (4) hearing services. Each of these service elements would
have its own periodicity schedule that meets reasonable practice
standards. These items and services must be covered for children
SUD
Ppr
y
y
|
2
a
b
c
u
m
®
fare to a
children
mmittee
current
. months
4.¢ offer
1ak Med.
bill. the
ain un-
@ same
“10d that
b-month
“rections
‘e termi-
‘eases to
'd under
bill also
eceiving
h provi-
ge after
d treat-
to offer
PSD
orm all
ices. to
5 in all
ctly or
“rective
ced.
ventive
1 mini-
devel-
ations:
priate
ned by
‘nt for
-creen-
ven if
=r the
in the
en ex-
ll. the
health
there-
1Stinct
i serv-
would
-actice
tldren
399
even if, under the State Medicaid plan, they are not offered to other groups of program beneficiaries. Under the Committee bill. screening services must, at a mini- mum. include (1) a comprehensive health and developmental histo. ry including assessment of both physical and mental health deve]. opment. ‘2; a comprehensive unclothed physical exam. (3) appro- priate immunizations according to age and health history, (4) labo- ratory tests including blood lead level assessment appropriate for age and risk factors), and (3) health education (including anticipato- rv guidance. The Committee emphasizes that anticipatory guid- ance to the child (or the child's parent or guardian) is a mandatory element of any adequate EPSDT assessment. Anticipatory guidance includes health education and counselling to both parents ang chil- dren.
Under the Committee bill, vision services must, at a minimum, include diagnosis and treatment for defects in vision, includin eye- glasses. Dental services must, at a-minimum, includesrelief o pain and infections, restoration of teeth, and maintenance of dental health. Hearing services must, at a minimum, include diagnosis and treatment for defects in hearing, including the provision of
necessary, these controls must be consistent with the preventive thrust of the EPSDT benefit. For example, States may not limit dental care to emergency services only, Mitchell v. Johnston, 701 F. 2d 337 (5th Cir. 1983).
The Committee bill also clarifies the periodic nature of EPSDT
The Committee bill also requires States to provide screening services at intervals other than those identified in their basic perio- dicity schedule, when there are indications that it is medically nec- essary to determine whether a child has a Physical or mental ill. ness or condition that may require further assessment, diagnosis, or treatment. These interperiodic screening examinations may occur even in the case of children whose physical, mental, or devel- opmental illnesses or conditions have already been diagnosed. if there are indications that the illness or condition may have become more severe or has changed sufficiently, so that further examina- tion is medically necessary. The Committee emphasizes that the de- termination of whether an interperiodic screening is medically nec- essary may be made by a health, developmental, or educational professional who comes into contact with a child outside of the
$7.3
a
PR
So
a
n
400
health care system (e.g. State early intervention or special educa-
tion programs, Head Start and day care programs. WIC and other
nutritional assistance programs). As long as the child is referred to
an EPSDT provider. the child would be entitled to an interperiodic
health assessment (or dental. vision, or hearing assessment) or
treatment services covered under the State plan.
These same considerations apply with respect to vision, dental,
and hearing services. all of which must be provided when indicated
as medically necessary to determine the existence of suspected 1ill-
nesses or conditions. For example, assume that a child is screened
at age 5 according to a State's periodicity schedule and is found to
have no abnormalities. At age six, the child is referred to the
school nurse by a teacher who suspects the child of having a vision
problem. Under the Committee bill. the child can—and should—be
referred at that point to a qualified provider of vision care for full
diagnostic and treatment services,"and the State must make pay-
ment for those services, even though the next regular vision exam
under the State's periodicity schedule does not occur until age 7.
While States may, at their option, impose prior authorization re-
quirements on treatment services, the Committee intends that, con-
sistent with the preventive thrust of the EPSDT benefit, both the
regular periodic screening services and the interperiodic screening
services be provided without prior authorization.
The Committee notes that Medicaid-eligible children are entitled
to EPSDT benefits even if they are enrolled in a health mainte-
nance organization, prepaid health plan, or other managed care
provider. The Committee expects that States will not contract with
a managed care provider unless the provider demonstrates that it
has the capacity (whether through its own employees or by con-
tract) to deliver the full array of items and services contained in
the EPSDT benefit. The Committee further expects that. in setting
payment rates for managed care providers, the States will make
available the resources necessary to conduct the required periodic
and interperiodic screenings and to provide the required diagnostic
and screening services.
The Committee bill clarifies that States are without authority to
restrict the classes of qualified providers that may participate in
the EPSDT program. Providers that meet the professional qualifi-
cations required under State law to provide an EPSDT screening,
diagnostic, or treatment service must be permitted to participate in
the program even if they deliver services in school settings, and
even if they are qualified to deliver only one of the items or serv-
ices in the EPSDT benefit.
(b) Report on the provision of EPSDT.—In order to assess the ef-
fectiveness of State EPSDT programs in reaching eligible children.
the Committee bill would require the States to report annuaily to
the Secretary, in a uniform form and manner established by the
Secretary, the following information. broken down by age group
and by basis of eligibility for Medicaid: (1) the number of children
receiving child health screening services; (2! the number of chil-
dren referred for corrective treatment (the need for which is dis-
closed by the screening); and (3 the number of children receiving
dental services. These reports would be due April 1 of each year
(beginning with April 1, 1991) and would apply to services provided
~~
oy 2 SB -
. -
-’
or special educa-
s. WIC and other
hild 1s referred to
> an interperiodic
g assessment’ or
to vision, dental,
d when indicated
> of suspected 1l]-
child 1s screened
e and 1s found to
referred to the
f having a vision
—and should —be
sion care for full
must make pay-
ular vision exam
:cur until age 7.
authorization re-
.ntends that. con-
benefit, both the
2riodic screening
iren are entitled
+ health mainte-
r managed care
ot contract with
nstrates tha: it
sees or by con-
les contained in
: that. in setting
rates will make
equired periodic
Jired diagnostic
Jut authority to
v participate in
2ssional qualifi-
'SDT screening,
0 participate in
>I settings. and
> "lems Or serv-
2 assess the ef.
ble children,
2rt annuziiy to
32.sned by the
. D¥ age Zroup
cer of children
umber of chil-
r which is dis-
idren receiving
+ of each year
rvices provided
101
during the Federal fiscal year endin g the previous Senter ner 30 (beginning with FY 1990).
4
Section 4)! —Extension of payment provisions for medical neces. Sary services in disproportionate share hospitals
(a) Coverage of medically necessary services for children. — Under current law, States may impose reasonable limits on the amount. duration, and scope of covered services. However, effective July 1, 1989, States are prohibited from imposing any fixed durational limit on Medicaid coverage of medically necessary inpatient hosp- tal services provided to infants under age 1 by disproportionate share hospitals. As of January, 1989, according to the Nationa] As. sociation of Childrens’ Hospitals and Related Institutions, 12 States imposed durational limits on inpatient hospital services tor chil. dren (Alabama, Alaska, Arkansas, Florida, Kentucky, Louisiana, Mississippi, Missouri, Oregon, Tennessee, Texas, and West Virgin. 1a). Ny x %
The purpose of the current law exception to fixed durational limits is to prohibit States from using arbitrary length of stay limi- tations (e.g., 20 days per year) to reduce payments for medically necessary services provided by hospitals, including many public and childrens’ hospitals, that serve a disproportionate number of low-income patients. The Committee bill would extend this current law prohibition to any fixed durationa} limits on payment for inpa- tient services provided to ¢thildren under age 18 by disproportionate share hospitals. The requirement is effective for inpatient hospital services furnished on or after July 1, 1990.
(b) Assuring adequaie payment for inpatient hospital ser: ices for children in disproportionate share hospitals. —Under current law, States may reimburse hospitals for inpatient services on a prospec- tive basis. If they choose to do so, States must, effective July 1, 1989, provide for an outlier adjustment in payment amounts for medically necessary inpatient services provided by disproportionate share hospitals involving exceptionally high costs or exceptionally long lengths of stay for infants under 1 year of age. According to the National Association of Children’s Hospitals and Related Insti- tutions, as of January, 1989, a total of 44 States pay for inpatient hospital services on a prospective basis; only 17 of these do not make outlier adjustments for high cost or long-stay cases (Ala- bama, Alaska, California, Colorado, Connecticut, D.C., Florida, Kentucky, Mississippi, Missouri, Nevada, New Hampshire, New Mexico, Oklahoma, Tennessee, Texas, and Washington). The Committee bill would extend this current law requirement to cases involving children from age 1 up to age 18. States that pay for inpatient hospital services on a prospective basis would be re- quired to submit to the Secretary, no later than April 1, 1990, a State plan amendment that provides for an outlier adjustment in payment amounts for medically necessary inpatient services pro- vided by disproportionate share hospitals after July 1, 1990. involv- ing exceptionally high costs or exceptionally long lengths of stay for children age 1 up to age 18.
gH IY
f
e
r
c
e
n
n
B
a
y
C
O
N
Y
h
e
r
e
c
A
N
m
e
@
A
P
M
P
N
y
e
EXHIBIT N
PN .
o- P@YU-352601
state medicaid manual Department of Health
and Human Services
Pant 5 — Early and Periodic Screening, Gnawa Administration
Diagnosis, and Treatment
(EPSDT)
Transmittal No. 3 Date
APRIL 1990
REVISED MATERIAL REVISED PAGES REPLACED PAGES
Table of Contents 5-1 (1 p.) 5-1 (1 p.)
Sec. 5010 - 5350 5-3 - 3-55(38 pp.) 5-3 - 5-39(37 pp.)
NEW IMPLEMENTING INSTRUCTIONS—EFFECTIVE DATE: APRIL 1, 1990
This transmittal provides guidance on $§§6403(a), (d) and (e) of OBRA'89 relating to
early and periodic screening, diagnostic and treatment services under Medicaid.
The cited subsections amended §51902(a)(43), 1905(a)(4XB) and added a new
§1905(r) to the Act.
The primary purpose of the amendments is to incorporate into the statute existing
regulatory requirements found at 42 CFR 440.40(b) and Part 441, Subpart B.
However, $6403 does make certain changes as follows:
0 modifies the definition of screening services by including appropriate
blood lead level testing and health education;
0 requires distinet periodicity schedules for screening, dental, vision and
hearing services and requires medically necessary interperiodic
screening services;
0 adds a new required service component of "other necessary health care,
diagnostic, treatment and other measures described in section 1905(a)
to correct or ameliorate defects and physical and mental illnesses and
conditions discovered by the screening services, whether or not such
services are covered under the State Medicaid plan."; and
0 clarifies that nothing in the Medicaid law permits limiting EPSDT
providers to those which can furnish all required EPSDT diagnostic or
treatment services or as preventing qualified providers which can
provide only one such service from program participation.
Changes have been made throughout the manual to accommodate the modifications
discussed above.
In addition, §56403(b) and (C) included requirements relating to annual reporting
requirements and development of EPSDT participation goals, respectively. This
material will be included in a future manual issuance.
HCFA-Pub. 45-8
®
CEAPTER V
EARLY AND PERIODIC SCREENING, DIAGNOSTIC AND TREATMENT (EPSDT) SERVICES
Introduction
OVRIVI@Wen snr venus cnsnrnsveneces 830060000920 000000000000 cee 5010 $-3
Program Requirements and Methods
Basic Requirement S.c eres cesvnsorecvcssnssionesovarsionss vs 5110 5-5
Informing Pamilies of EPSDT tg ber PEER RENE RE ie 5121 S-7
EPSDYT Service ReqQuirementlesecssnecseissvenrnscerensrsvne 5122 S-9
Screening Service Delivery and Content. .ceeeeceeoeseeoses $123 $-10
Minimum Standards and Requirements. .cveeeeecscscsoennes $123.1 5-10
Screening Service CoNteN.sssveersntseneneseress sevens 5123.2 S-11
DIAGNROSLS And MreAtBeN estas srtceersrsrvceveserrseseses 5124 S-17
PeriOBICItY SOBBAUIEs certs cstrtterssrenssssesrvasesse esse 5140 5-20
Transportation and Scheduling AssistanCe..ceeeeeecsscoess 5150 5-23
Utilization of Providers and Coordination with Related Programs
Referral for Services Not Covered Under Medicaid......... 5210 5-25
Uti1123t0N Of ProviBerssseesssessceessovesversscressesos 5220 5-26
Coordination with Related Agencies and Programs..c.coevees 5230 $=-27
Relations With State Maternal and Child Health
BEOUTAMBesnernvssevnsssrssnensaetssenseessoeesensa 5230.1 S=-28
Other Agencies and ProgramB.svessscrscernscoscesesessnse $230.2 5-30
CONLINUING CAL@eennvrreessnsnovternsnessesnscneossessseees 5240 $-33
Administration
Program Monitoring, Planning, and BvaluatioN.eeceececeeos. 5310 S$=-3%
Information Needs and Reportingeiceccecsceccenccccasneees $320 S-38
Administrative Information Requirements. ..ceececcccees $320.1 S-38
Records or Information on Services and Recipients..... $320.2 S-38
TIRE line EB nncecantvsrsstssesesrtsvres st etasesceersrnsees $330 $-45
ReimbUL SERENE ecreonrsrrssstsntrsvervrssssrosesseosiesosee 5340 S-51
CONE Ident IA Yr eeerrnnsnstsnnssnesnennssressvrrserresee $350 §=-5§
Rev. 3
5-1
® EARLY AND PERIODIC SCREENING, 04-50 DIAGNOSTIC AND TREATMENT SERVICES 5010
Introduction
EE ———————————
5010. OVERVIEW
= A. Early and Periodic Screening, Diagnostic and Treatment Benefit.—Early and periodic screening, diagnostic and treatment services (EPSDT) Is a required service under the Medicaid program for categorically needy individuals under age 21. The EPSDT benefit is optional for the medically needy population. However, if the EPSDT benefit is elected for the medically needy population, the EPSDT benefit must be made available to all Medicaid eligible individuals under age 21,
B. A Comprehensive Child Health Program,.--The EPSDT program consists of two, mutually supportive, operational components:
0 assuring the availability and accessibility of required health care resources and
0 helping Medicaid recipients and their parents or guardians effectively use them,
These components enable Medicaid agencies to manage a comprehensive child health program of prevention and treatment, to systematically:
; © Seek out eligibles and inform them of the benefits of prevention and the health services and assistance available,
0 Help them and their families use health resources, including their own ~ talents and knowledge, effectively and efficiently,
0 Assess the child's health needs through initial and periodic examinations and evaluation, and
© Assure that health problems found are diagnosed and treated early, before they become more complex and their treatment more costly, Although "case management” does not appear in the statutory provisions pertaining to the EPSDT benefit, the concept has been recognized as a means of increasing program efficiency and effectiveness by assuring that needed services are provided timely and efficiently, and that duplicated and unnecessary services are avoided,
Sg C. Administration.--You have the flexibility within the Pederal statute and regulations to design an EPSDT program that meets the health needs of recipients within your jurisdiction. Title XIX establishes the framework, containing standards and requirements you must meet.
Rev. 3 3 $-3
3 EARLY AND PERIODIC sc@ xine, 0490 DIAGNOSTIC AND TREATMENT SERVICES 5110
Program Requirements and Methods
5110. BASIC REQUIREMENTS
[MoBRA 89 amended §§1902(aX43) and 1905(aX4XB) and created §1905(r) of the Social Security Act (the Act) which set forth the basic requirements for the program. Under the EPSDT benefit, you must provide for screening, vision, hearing and dental services at
health care, You must also provide for medically necessary screening, vision, hearing and dental services regardless of whether such services coincide with your established periodicity schedules for these services. Additionally, the Act requires that any service which you are permitted to cover under Medicaid that is necessary to treat or ameliorate a defect, physical and mental illness, or a condition identified by a screen, must be provided to EPSDT participants regardless of whether the service or item is otherwise :
The statute provides an exception to comparability for EPSDT services. Under this . exception, the amount, duration and scope of the services provided under the EPSDT
reasonably achieve their purpose. The amount, duration, or scope of EPSDT services to recipients may not be denied arbitrarily or reduced solely because of the diagnosis, type of illness, or condition. Appropriate limits may be placed on EPSDT services based on medical necessity.
/
Rev, 3 5-5
I's
» EARLY AND PERIODIC sci@uine,
DIAGNOSTIC AND TREATMENT SERVICES $121
5121. INFORMING FAMILIES OF EPSDT SERVICES
04-30
A. General Information.—Section 1302(aX43) of the Act requires that the State plan provide for informing all eligible Medicaid recipients under 21 about EPSDT. The intent of the statute is to allow flexibility of process as long as the outcome is effective, and is achieved in a timely manner, generally within 60 days.
The informing process, which may begin at the intake interview, extends to no later than 60 days following the date of a family's of individual's initial eligibility determination, or of a determination after a period of ineligibility, A combination of face-to-face, oral and written informing activities is most productive, :
The regulation requires you to assure that your combination of written and oral informing methods are effective, Use methods of communication that recipients can clearly and easily understand to ensure that they have the information they need to utilize services to which. they are entitled, © HCFA considers "oral" methods to Include face-to-face informing by eligibility case workers, health aides and providers as well as public service announcements, community awareness campaigns, audio-visual films and film strips.
It is effective and efficient to target specific Informing activities to particular "at risk" groups. For example, mothers with babies to be added to assistance units, families with infants, or adolescents, first time eligibles, and those not using the program for over 2 years might benefit most from oral methods, : : $e, > >
B. Individuals to Be Informed, —
}
or determined eligible after a period of ineligibility if they have not used EPSDT services for at least 1 year. Use a combination of written and oral methods, generally within 80 days following the date of the eligibility determination,
Families that go on and off the rolls do not have to be informed more than once in a 12-month period.
0 There is no distinction between title IV-E foster care families and others. For title IV-E foster care individuals, informing must be with the unit receiving the cash
cases, there are changes in foster parents, institution administrators, or responsible social workers. It Is to the individual's benefit that informing be done initially, not only with the unit receiving the cash assistance, but with parties who have legal authority over or custody of the individual,
Rev. 3 . 5-7
eS EARLY AND PERIODIC SCREE(@G,
5121(Cont.) DIAGNOSTIC AND TREATMENT SEWRVICES 04.99
—
Informing about EPSDT encourages appropriate planning for the health needs of children.
When informing foster parents or administrators of institutions encompass all title [V-E
foster care Individuals in their care. Inform institutions or homes having a number of ( individuals annually or more often when the need arises, such as when changes in
administrators, social workers or foster parents occur. If an individual is rotated through
foster care homes, inform the responsible parties at the homes, unless previously done
within the year for other foster care individuals. Annual contact establishes a
relationship with the facilities to resolve any problems arising.
Fo o Inform a Medicaid eligible pregnant woman about the availability of EPSDT
services for children under age 21 (including children eligible as newborns). A Medicaid
eligible woman's positive response to an offer of EPSDT services during her pregnancy,
which is medically confirmed, constitutes a request for EPSDT services for the child at
birth. For a child eligible at birth (i.e., as a newborn of a woman who is eligible for and
receiving Medicaid), the request for EPSDT services is effective with the birth of the
child. The parent or guardian of an infant who is not deemed eligible at birth as a
|__newborn must be informed at the time the infant's eligibility is determined.
C. Content and Methods.—
o Use clear and nontechnical language, provide a combination of oral and
written methods designed to inform all eligible individuals (or their families) effectively
describing what services are available under the EPSDT program; the benefits of
preventive health care, where the services are available, how to obtain them; and that
necessary transportation and scheduling assistance is available.
[Inform eligible individuals whether services are provided without cost. States may impose
premiums for Medicaid on individuals (i.e., pregnant women and infants) whose family
income exceeds 150 percent of Federal poverty levels as described in §3571 and, for
medically needy participants, may impose enrollment fees, premiums or similar charges
|_for participation in the medically needy program.
o
n
0 Provide assurance that processes are in place to effectively inform
individuals, generally within 60 days of the individual's Medicaid eligibility determination
and, if no one eligible in the family has utilized EPSDT services, annually thereafter.
o Utilize accepted methods for informing persons who are illiterate, blind,
deaf, or cannot understand the English language. For assistance in developing appropriate
procedures, contact agencies with established procedures for working with such
individuals, e.g., State or local education departments, employment security offices,
handicapped programs.
o You have the flexibility to determine how information may be given most
appropriately while assuring that every EPSDT eligible receives the basic information
necessary to gain access to EPSDT services.
5-8 3 Rev. 3
® EARLY AND PERIODIC SCREENING, 04-90 DIAGNOSTIC AND TREATMENT SERVICES 5122
S122.
The EPSDT benefit, in accordance with §1905(r) of the Act, must include the services set forth below. The frequency with which the services must be provided is discussed in §5140.
EPSDT SERVICE REQUIREMENTS
A. Screening Services.—Screening services include all of the following services:
0 A comprehensive health and developmental history (including assessment of both physical and mental health development);
© A comprehensive unclothed physical exam;
© Appropriate Immunizations according to age and health history;
o Laboratory tosis (including lead blood level assessment appropriate © age | and risk); and , EE Sag:
0 Health education (including anticipatory guidance).
Immunizations which may be appropriate based on age and health history but which are medically contraindicated at the time of the screening may be rescheduled at an appropriate time. : ;
B. Vision Services.—At a minimum, include diagnosis and treatment foe defects in vision, including eyeglasses. : .. i Se i
Nn
C. Dental Services.—At a minimum, include relief of pain and infections, | restoration of teeth and maintenance of dental health. Dental Services may not be limited to emergency services. g ® hn
D. Hearing Services.—At a minimum, include diagnosis and treatment foe defects in hearing, ne: hearing aids.
E. Other Necessary Health Care.—Other necessary health care, diagnostic services, treatment and other measures described in §1905(a) of the Act to correct or ameliorate defects, and physical and mental illnesses and conditions discovered by the screening services.
F. Limitation of Services.—The services available in subsection E are not limited to those included In your State plan.
0 Under subsection E, the services must be "necessary . . . to correct or | 2nelicente defects and physical or mental Qllnesses or conditions « +o" and the defects,
Rev. 3 5-9
EARLY AND PERIODIC SCREE ga G,
512) DIAGNOSTIC AND TREATMENT SSVICES 04-90
illnesses and conditions must have been discovered or shown to have increased in severity
by the. screening services. You make the determination as to whether the service is
necessary. You are not required to provide any items or services which you determine are
not safe and effective or which are considered experimental.
A 0 42 CFR 440.230 allows you to establish the amount, duration and scope of
services provided under the EPSDT benefit. Any limitations imposed must be reasonable
and services must be sufficient to achieve their purpose (within the context of serving the
needs of individuals under age 21). You may define the service as long as the definition
comports with the requirements of the statute in that all services included in §1905(a) of
the Act that are medically necessary to ameliorate or correct defects and physical or
mental illnesses and conditions discovered by the screening services are provided.
0 All services must be, provided in accordance with both §1905(a) of the Act
and any State laws of general applicability that govern the provision of health services.
Home and community based services which are authorized by §1915(c) of the Act are not
included among the other health care under subsection E because these services are not
included under §1905(a) of the Act.
5123. SCREENING SERVICE DELIVERY AND CONTENT
5123.1 Minimum Standards and Requirements.—
A. State Standards.--Set standards and protocols which, at a minimum, meet the
standards of §1905(r) of the Act for each component of the EPSDT services, and maintain £
written evidence of them. The standards must provide for services at intervals which
meet reasonable standards of medical and dental practice and be established after
consultation with recognized medical and dental organizations involved in child health
care. The standards must also provide for EPSDT services at other intervals, indicated as
medically necessary, to determine the existence of certain physical or mental illnesses or
conditions. The intervals at which services must be made available are discussed in
§5140.
B. Services.—
o Provide an eligible individual requesting EPSDT services required screening
services listed in §5122. This initial examination(s) may be requested at any time, and
must be provided without regard to whether the individual's age coincides with the
established periodicity schedule. Sound medical practice requires that when children first
enter the EPSDT program you encourage and promote that they receive the full panoply
of screening services available under EPSDT,
o It is desirable that a parent or other responsible adult accompany the child
to the examination. When this is not possible or practical, arrange for a followup worker,
social worker, health aide, or neighborhood worker to discuss the results in a visit to the
home or in contacts with the family elsewhere.
5-10 Rev. 3
®» EARLY AND PERIODIC SC (@F NING,
0430 DIAGNOSTIC AND TREATMENT SERVICES 5123.2
C. Who Screens/Assesses?—
© Examinations are performed by, or under the supervision of, a certified Medicaid physician, dentist, or other provider qualified under State law to furnish primary medical and health services. These services may be provided within State and local health departments, school health programs, programs for children with special health needs, Maternity and Infant Care projects, Children and Youth programs, Head Start programs, community health centers, medical/dental schools, prepaid health care plans, a private practitioner and any other licensed practitioners in a variety of arrangements,
© The use of all types of providers is encouraged. Recipients should have the greatest possible range and freedom of choice. It is required, in the case of title V, and encouraged, in the case of the primary care projects (i.e., community health centers), that maximum use be made of these providers. Day care centers may provide sites for examination activities, Encourage cooperation when and where other broad-based assessment programs are unavailable, ' ::
0 Providers may not be limited to those which have an exclusive contract to perform all EPSDT services. Service providers may not be limited to either the private or puble sector or because the provider may not offer all EPSDT services or because it | sfters only one service. Assure maximum utilization of existing resources to more effectively administer and deliver services.
Medicaid providers who offer EPSDT examination services must assure that the services they provide meet the agency's minimum standards for those services in order to be reimbursed at the level established for EPSDT services.
5123.2 Screening Service Content,— Bea - o 3 - yo . . an ae bE)
y ra © ’ Sn in : rp)
s A. Comprehensive Health and Developmerital History.—Obtain this ‘Information from the parent or other responsible adult who is familiar with the child's history and include an assessment of both physical and mental health development, Coupled with the |_physieal examination, this includes: ie oh 2
1. Developmental Assessment.—This includes a range of activities to determine whether an individual's developmental processes fall within a normal range of achievement according to age group and cultural background. Screening for developmental assessment is a part of every routine initial and periodic examination.
Rev, 3 : s-11
‘@ FARLY AND PERIODIC scret fo, 5123.2(Cont.) DIAGNOSTIC AND TREATMENT SERVICES 04
Developmental assessment is also carried out by professionals to whom children are referred for structured tests and instruments after potential problems have been identified by the screening process. You may build the two aspects into the program so that fewer referrals are made for additional developmental assessment,
-90
8. Approach.—There is no universal list of the dimensions of development for the different age ranges of childhood and adolescence. In younger children, assess at least the following elements:
o Gross motor development, focusing on strength, balance, locomotion;
© Fine motor development, focusing on eye-hand coordination;
0 Communication skills or language development, focusing on expression, comprehension, and speech articulation;
0 Self-help and self-care skills;
0 Social-emotional development, focusing on the ability to engage in social interaction with other children, adolescents, parents, and other adults; and
0 Cognitive skills, focusing on problem solving or reasoning.
As the child grows through school age, focus the program on visual-motor integration, visual-spacial organization, visual sequential * memory, attention skills auditory processing skills, and auditory sequential memory. Most school systems provide routines and resources for developmental screening,
For adolescents, the orientation should encompass such areas of special concern as potential presence of learning disabilities, peer relations, psychological/psychiatrie problems, and vocational skills,
b. Procedures.—No list of specified tests and instruments is prescribed for identifying developmental problems because of the large number of such instruments, development of new approaches, the number of children and the complexity of developmental problems which occur, and to avoid any connotation that only certain tests or instruments satisfy Federal requirements. However, the following principles must be consider ed:
© Acquire information on the child's usual functioning, as reported by the child, parent, teacher, health professional, or other familiar person.
3-12
Rev, 3
a
> EARLY AND PERIODIC SEE ENING,
0490 4 DIAGNOSTIC AND TREATM SERVICES
5123.2(Cont.)
© In screening for developmental assessment, the examiner
incorporates and reviews this information in conjunction with other information gathered
during the physical examination and makes an objective professional judgement whether
the child is within the expected ranges. Review developmental progress, not in isolation,
but as a component of overall health and well-being, given the child's age and culture,
o Developmental assessment should be culturally sensitive and valid.
Potential problems should not be dismissed or excused improperly on grounds of culturally
appropriate behavior. Do not initiate referrals improperly for factors associated with
cultural heritage.
0 Programs should not result in a label or premature diagnosis of a
child. Providers should report only that a condition was referred or that a type of
diagnostic or treatment service is needed. Results of initial screening should not be
accepted as conclusions and do not represent a diagnosis,
o Refer to appropriate child development resources for additional
assessment, diagnosis, treatment or follow-up when concerns or questions remain after
the screening process.
2. Assessment of Nutritional Status.—This is accomplished in the basic
examination through:
0 Questions about dietary practices to identify unusual eating habits (such
as pica or extended use of bottle feedings) or diets which are deficient or excessive in one
or more nutrients,
o A complete physical examination including an oral dental examination.
Pay special attention to such general features as pallor, apathy and irritability.
0 Accurate measurements of height and weight are among the most
important indices of nutritional status.
© A laboratory test to screen for iron deficiency. HCFA and PHS
recommend that the erythrocyte protoporphyrin (EP) test be utilized when possible for
children ages 1-5. It is a simple, cost-effective tool for screening for iron deficiency
Where the EP test is not available, use hemoglobin concentration or hematocrit.
0 If feasible, screen children over 1 year of age for serum cholesterol
determination, especially those with a family history of heart disease and/or hypertension
and stroke.
Rev. 3 . 5-13
a EARLY AND PERIODIC SCREENS. 5123.2(Cont.) (DIAGNOSTIC AND TREATMENT $ CES 04-90
If infor mation suggests dietary inadequacy, obesity or other nutritional problems, further assessment is indicated, including:
© Family, socioeconomic or any community factors,
0 Determining quality and quantity of individual diets (e.g., intake, food acceptance, meal patterns, m
and utilization of food assistance programs)
dietary
ethods of food preparation and preservation,
0 Further physical and laboratory examinations, and
© Preventive, treatment and follow-up services, including dietary counseling and nutrition education.
B. Comprehensive Unclothed Physical Examination:~Includes the following:
1. Physical Growth.—Record and compare the child's height and weight with those considered normal for that age. (In the first year of life head circumference measurements are important), Use a graphic recording sheet to chart height and weight over time,
2. Unclothed Physical Inspection.—Check the general appearance of the child to determine overall health status. This process can pick up obvious physical defects, including orthopedic disorders, hernia, skin disease, and genital abnormalities. Physical inspection includes an examination of all organ systems such as pulmonary, cardiac, and gastrointestinal,
qd
C. Appropriate Immunizations.—Assess whether the child has been immunized ( against diphtheria, pertussis, tetanus, polio, measles, rubella, and mumps, and whether booster shots are needed. The child's immunization record should be available to the provider. When an immunization or an updating is medically necessary and appropriate, provide it and so inform the child's health supervision provider.
Provide immunizations as recommended Dy the American Academy of Pediatrics (AAP) and/or local health departments.
D. A iate Laborator Tests.—Identify as statewide screening requirements, the minimum Si tests or analyses to be performed by medical providers for
= 1. Lead Toxicity Screening.—Where age and risk factors indicate it is medically appropriate to perform a blood level assessment, a blood level assessment is | mandatory.
TE Rev. 3
M [
EARLY AND PERIODIC SCREENING,
07-90 DIAGNOSTIC AND TREATMENT SERVICES 5123.2(Cont.)
Screen all Medicaid eligible children ages 1-5 for lead poisoning. Lead poisoning is
defined as an elevated venous blood lead level (i.e., greater than or equal to 25
micrograms per deciliter (ug/dl) with an elevated erythrocyte protoporphyrin (EP) level
(greater than or equal to 35 ug/dl of whole blood). In general, use the EP test as the
primary screening test. Perform venous blood lead measurements on children with
elevated EP levels.
Children with lead poisoning require diagnosis and treatment which includes periodic re-
evaluation and environmental evaluation to identify the sources of lead. fhe
: oe
2. Anemia Test.—~The most easily administered test for anemia” bh ‘a
microhematocrit determination from venous blood or a fingerstick.
2
3. Sickle Cell Test.—Diagnosis for sickle cell trait may be done with sickle cell
preparation or a hemoglobin solubility test. If a child has been properly tested once for
sickle cell disease, the test need not be repeated. :
4. Tuberculin Test.—Give a tuberculin test to every child who has not received
one within a year, “ait
5. Others.—In addition to the tests above, there are several other tests to
consider, Their appropriateness are determined by an. individual's age, sex, health
history, clinical symptoms and exposure to disease. These include a urine screening,
pinworm slide, urine culture (for girls), serological test, drug dependency screening, - stool
specimen for parasites, ova, blood, and HIV screening. ii oF al
E. Health Education.—Health education is a required component of screening
services and includes anticipatory guidance. At the outset, the physical and dental
assessment, or screening, gives you the initial context for providing health education.
Health education and counselling to both parents (or guardians) and children is required
and is designed to assist in understanding what to expect in terms of the child's
development and to provide information about the benefits of healthy lifestyles and
practices as well as accident and disease prevention.
F. Vision and Hearing Screens.—Vision and hearing services are subject to their own
periodicity schedules (as described in §5140). However, where the periodicity schedules
coincide with the schedule for screening services (defined in §5122 A), you may include
vision and hearing screens as a part of the required minimum screening services,
1. Appropriate Vision Screen.—Administer an age-appropriate vision
assessment. Consultation by opthalmologists and optometrists can help determine the
type of procedures to use and the criteria for determining when a child should be referred
for diagnostic examination,
2. Appropriate Hearing Screen.—Administer an age-appropriate hearing
assessment. Obtain consultation and suitable procedures for screening and methods of
administering them from audiologists, or from State health or education departments,
Rev, 4 5-15
» »
EARLY AND PERIODIC SCREENING, :
$123.2(Cont.) DIAGNOSTIC AND TREATMENT SERVICES 07-90
G. Dental Screening Services.——Although an oral screening may be part of a physical examination, it does not substitute for examination through direct referral to a dentist. A direct dental referral is required for every child in accordance with your
periodicity schedule and at other intervals as medically necessary. Prior to enactment of OBRA 89, HCFA in consultation with the American Dental Association, the American Academy of Pediatrics and the American Academy of Family Practice, among other organizations, required direct referral to a dentist beginning at age 3 or an earlier age if determined medically necessary. The law as amended by OBRA 89 requires that dental services (including initial direct referral to a dentist) conform to your periodicity schedule which must be established after consultation with recognized dental organizations involved in child health care, N
0 Especially in older children, the periodicity schedule for dental examinations is not governed by the schedule for medical examinations. Dental examinations of older children should occur with greater frequency than is the case with physical examinations. The referral must be for an encounter with a dentist, or a professional dental hygienist under the supervision of a dentist, for diagnosis and treatment, However, where any screening, even as early as the neonatal examination, indicates that dental services are needed at an earlier age, provide the needed dental services,
o The requirement of a direct referral to a dentist can be met in settings other than a dentist's office. The necessary el¢ ment is that the child be examined by a dentist or other dental professional under the supervision of a dentist, In an area where dentists are scarce or not easy to reach, dental examinations in a clinic or group setting may make the service more appealing to recipients while meeting the dental periodicity schedule, If continuing care providers have dentists on their staff, the direct referral to a dentist requirement is met. Dental paraprofessionals under direct supervision of a dentist may perform routine services when in compliance with State practice acts.
o Determine whether the screening provider or the agency does the direct referral to a dentist. You are ultimately responsible for assuring that the direct referral is made and that the child gets to the dentist's office in a timely manner.
5-18
Rev. 4
EXHIBIT O
MEDICAID
Early and Periodic Screening
Diagnosis Treatment for
Individuals Under 21
— Guidelines
CE ® Medical Services Administration
DEPARTMENT OF HEALTH, EDUCATION, AND WELFARE @ SOCIAL and REHABILITATION SERVI
€
DEPARTMENT OF HEALTH, 9... AND WELFARE "»
SOCIAL AND REHABILITATION SERVICER
WASHINGTON, D. C.
REGULATION:
MAINTENANCE
INSTRUCTIONS :
INQUIRIES TO:
PROGRAM REGULATION GUIDE
MSA-PRG-21
June 28, 1972
STATE AGENCIES ADMINISTERING APPROVED MEDICAL
ASSISTANCE PLANS
Medical Assistance Manual: Services and Payment
in Medical Assistance Programs - Amount, Duration
and Scope of Medical Assistance - Early and
Periodic Screening, Diagnosis, and Treatment
SRS PR 40-11(C-4), 45 CFR 249.10(a)(3) and (b)(4)
(11), Barly and Periodic Screening, Diagnosis, and
Treatment of Eligible Individuals Under Age 21
This material provides guidelines on the regulation
pertaining to the requirement for early health care
for young Medicaid recipients.
The requirements were effective February 7, 1972
Interim Program Regulation Guide, MSA-PRG-13,
December 22, 1971.
1. Remove MSA-PRG-13 (Interim) from Part 5S of the
Medical Assistance Manual.
2. Insert the attached pages in Part 5 of the
Medical Assistance Manual.
3. Post receipt of PRG
SRS Regional Commissioners.
A.olo BY
Qreee Commissioner
Medical Services Administration
TABLE OF CONTENTS
Introduction . .
Summary of Basic Provisions
Coverage « «
Case Finding .
Screening «
Diagnosis . .
Treatment « ¢« oo o o
Interagency Cooperation
APPENDIX
A Amendment to 45 CFR 249.10(a)(3) (b)(4) (11):
36 F.R. 21409, November 9, 1971
Bibliography
MSA- PRG- 21
6-28-72
0 "
Medical
Assistance
—— Manual
Services and Payment in Medical Assistance Programs
Early and Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 21
5.70-10 legal Background and Authority
A. Title XIX of the Social Security Act, as amended, Section
1905(a) (4) (B),
B. 45 CFR 249,10(a)(3) and (b)(&4)(i1); 36 F.R. 21409,
November 9, 1971 (See Appendix A for text).
C. SRS Program Regulation 40-11(C-4), dated November 9, 1971.
5-70-20 Implementation
A, Introduction
The 1967 amendments to title XIX of the Social Security Act added a
requirement to Medicaid that was intended to direct attention to the
gi importance of preventive health services and early detection and
L treatment of disease in children eligible for medical assistance.
This corresponded to a similar amendment to title V of the Act, Through
this amendment Congress intended to require States to take aggressive.
steps to screen, diagnose and treat children with health problems.
Congress was concerned about the variations from State to State in the
rates of children treated for handicapping conditions and health problems
that could lead to chronic illness and disability. Senate and House
Committee reports emphasized the need for extending outreach efforts to
create awareness of existing health care services, to stimulate the use
of these services, and to make services available so that young people
can receive medical care before bealth problems become chronic and
irreversible damage occurs,
Although health assessment may be carried out by an individual prac-
titioner in solo practice, the complexities of physical and mental health
problems and the rapid expansion of medical and psychological knowledge
and technology usually will require the efforts of several health special-
ists working closely together if a complete evaluation of an individual's
health status is to be accomplished. For the most effective implementation
(:
MSA- PRG- 21
6-28-72
2
5-70-00 p. 2 3 8
Medical —
Assistance -
Manual
Part 5. Services and Payment in Medical Assistance Programs
5-70-00 Early and Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 21
5-70-20 A, Introduction (Continued)
of the regulation, comprehensive screening services with provision for
continuity of care through diagnosis and treatment are necessary. The
State agency should encourage and work toward the development, on a
State-wide basis, of screening and diagnostic services so that young
people who are eligible for Medicaid services will have access to a
coordinated, integrated evaluation process and health care system,
Where such integrated programs do not presently exist, the Medicaid
agency shculd enlist the help of the professional health associations,
individual practitioners, medical and dental schools and institutions
that train other health practitioners, and the many official and volun- :
tary health agencies in the State to provide the services needed to carry a \
out the program, The efforts of all of these groups, and others, will be 5
urgently needed if the goals of early casefinding and diagnosis, as well
as prompt and effective treatment, are to be realized.
Implementation of the regulation will necessitate an examination of the
extent of the screening services needed by the young Medicaid population.
Within any given population, individuals will differ greatly in their
need for health care and medical services. Among children, some may never
have seen a physician, and no assessment has been made of their state of
health, These children should be drawn into a screening process to be
followed by diagnosis and treatment, as necessary. Other children have
apparent or obvious health problems but are not receiving treatment, They
may need more definitive diagnostic studies and subsequent treatment, but
screening might be unnecessary. Other young Medicaid recipients may
already be receiving preventive and health assessment services in child
health clinics or may be under the care of health practitioners. For this
group it may be necessary only to make certain that an assessment of their
complete health status has been made, and they are receiving the needed
care, :
Within the context of this regulation, the words, screening, diagnosis,
treatment, early and periodic are defined as follows:
MSA- PRG- 21
6-28-72
5- 70- 00 Pe 3
Medical
Asslstance
Manual
Services and Payment in Medical Assistance Programs
Early and Periodic Screening, Diagnosis, and Treatment of
2.
3.
Eligible Individuals Under Age 21
A. Introduction (Continued)
Screening is the use of quick, simple procedures carried out among
large groups of people to sort out apparently well persons from those
who have a disease OT abnormality and to identify those in need of
more definitive study of their physical or mental problems.
Diagnosis is the determination of the nature or cause of physical or
nental disease or abnormality through the combined use of health.
history, physical, developmental and psychological examination, and
laboratory tests and X-rays. Although, in some instances, 8& presump-
tive diagnosis may be made at the time of screening, it will usually
be necessary to refer the patient to the appropriate practitioner or
medical facility for definitive evaluation. :
Treatment means physician's or dentist's services, optometrist's or
audiologist's services, hospital services (inpatient and outpatient),
clinic services (both comprehensive health services centers and
specialized clinics); laboratory and X-ray services; prescribed drugs,
eyeglasses, hearing aids, prosthetic and orthotic devices; physical
therapy, occupational therapy, speech pathology and audiology services;
rehabilitative services; and any other type of medical care and
services recognized under State law, to prevent, correct or ameliorate
disease or abnormalities detected by screening and diagnostic procedures.
Early means, in case of a family already receiving assistance, a8 early
as possible in the child's life; or as soon as a family's eligibility
for assistance has been established.
. .
Periodic means at intervals established for screening by medical, dental
and other health care experts at appropriate periods of time to assure
that disease or disability is not incipient or present, Some procedures
should be done annually, some every two or more years, and the frequency
of others will depend on the child's age. Health experts in the State
should be consulted for assistance in establishing periodicity.
5-70-00 p. 4 (@ is | |
Medical ll _“§—h"n GPA : 4 (
Assletanc® |
Manual AMR
AT LEE U WIV Wo ree ran
Part 5, Services grid Paymant in Medical Assistance Progrems
5-70-00 Early and Periodic Screening, Disgnosig, and Treatment of
Eligible Individuale Under Age 21
5-70-20 B. Summary of Basic Provisions
This section deecribas briefly the major provisions of the EPSDT* regu-
lation and is followed by a more detailed discussion of some aspects of
the progran,
1, Under this regulation, a State agency must provide for an asseszement
of an individual's physical and mental health, The State agency,
through consultation with health experts, should determine the specif:
health evaluation procedures to be used and the mechanisms needed to
carry out thes screening program,
At a minimum, screening should include: a health and developmental
history (physical and mental); an assessment of physical growth;
developmental assessment; inspection for obvious physical defects; C
ear, nose, mouth end throat inspection (including inspection of teeth
and gums); screening tests for cardiac abnormalities, anemia, sickle
Gell trait, lead poisoning, tuberculosis, diabetes, infections and
other urinary tract conditions; and assessment of nutritional
status and immunization status. An assessment cf this nature is
necessary to identify individuals with potential or apparent physical
or mental health and development problems requiring diagnosis and,
possibly, treatment. Further discussion of screening will be found
in Section E7,
2.. The State agency must provide for diagnostic services for individuals
found, through the screening process, to be in need of further diagnos-
tic study.
3. The State agency must provide any treatment within the amount, duration,
and scope of its State plan, needed by an individual who has received
- screening or diagrostic services. In addition, if the State plan does
not otherwise include eyeglasses, hearing aids, other treatment for
visual and hearing defects, and dental services as described under Gl
of these guidelines, such services must be made available to individuals
eligible for EPSDT services,
—
*For brevity, the letters EPSDT will be used hereafter in the guidelines to (
designate 'early and periodic screening, diagnosis, and treatment,"
#
S- 70-00 Pe 5
- ; Medical
Assistance
— Manual
Part 5. Services and Payment in Medical Assistance Programs
5-70-00 Early and Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 21
5.70-20 B, Summary of Basic Provisions (Continued)
4, All States have been required to provide EPSDT since February 7,
1972.
5. The program must include all eligible individuals under age 21,
but a State may implement the regulation by starting with children
under six years, as a minimum, provided that it has submitted a
plan to the Regional Office for phasing-in other age groups and by
June 1, 1973 is offering EPSDT services to all Medicaid eligibles
under 21. ‘'Phasing-in" applies only to age groups; services may
not be added one or two at a time under this requirement since
the purpose of EPSDT is to evaluate and treat the whole child.
6. The State agency must have an outreach program to inform AFDC
( families and other eligible individuals about the screening program
and to encourage them to take advantage of this service. Trained
indigenous workers often are most strategically located to reach
families and to inform them about the program, :
7. The State agency must seek out and develop agreements with facili-
ties and practitioners throughout the State that can provide screening
and diagnostic services for early casefinding purposes. To the
extent they are available, existing programs for early casefinding
should be used. When screening and diagnostic services throughout
the State are insufficient to meet the needs of the Medicaid program,
the development of additional centers should be encouraged, This
will require contacts with such groups as medical and dental societies,
other practitioner organizations, medical schools, State and regional
or local health departments, programs for mothers and children under
title V of the Social Security Act, OEO neighborhood health centers,
developmental disability agencies, university affiliated facilities,
day care centers, school health programs, rehabilitation agencies and
voluntary health programs,
#
TSA- PRG- 21
6- 28-77
5-70-00 p. 6 PA »
\
Medical
Assistance
Manual
Part 5. Services and Payment in Medical Assistance Programs
5-70-00 Early and Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 21
5-70-20 B, Summary of Basic Provisions (Continued)
8.
9.
10.
33,
12,
Procedures should be established to facilitate reporting of findings
and referral from the screening center, Effective referral and
follow-up mechanisms will require a close working relationship among
the provider of screening services, the State agency and the local
welfare department, Prompt transmittal of the results of the
screening procedures is necessary so that diagnostic studies and
treatment can be instituted without delay. Children found, during
the screening process, to need immediate medical attention should
be referred promptly,
EPSDT represents an exception to the requirement for comparability
of services under title XIX. A State may provide EPSDT services for o
individuals under ‘21 years of age without providing similar services
for those over 21. -
Payment, where appropriate, for screening, diagnostic, and treatment
services should be made in accordance with Federal regulations per-
taining to payment for services provided under the Medicaid program,
Further discussion of payment for services provided under the au-
spices of other agencies is in Section H2 of these guidelines.
The State agency may impose utilization controls on the use of the
EPSDT program and on expenditures under the program so long as the
controls do not prevent an eligible individual from having access
to the minimum provisions of the EPSDT effort,
A required monthly reporting form has been developed by which the
State agency will submit to SRS summary data on early and periodic
screening, diagnosis, and treatment provided during the report month,
including the following information:
number of children screened; number of children
referred for diagnosis and/or treatment of eye
problems, hearing deficiencies, dental problems,
sickle cell anemia, lead poisoning, and "all
other" conditions, C
MSA- PRG- 21
6-28-72
5-70-00 p. 7
Viedical
Assistance
Manual
Part 5, Services and Payment in Medical Assistance Programs
5-70-00 Early and Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 21
5.70-20 B, Summary of Basic Provisions (Continued)
These data are to be provided for two distinguishable groups of
children-- those under 6, and those 6-21. Data systems should be
established to enable response to additional data requests con-
cerning referral for diagnosis and/or treatment of various con-
ditions as may be specified by the Social and Rehabilitation
Service from time to time, However, as a minimum it is expected
that records will be kept which distinguish referrals on the
basis of the six classifications listed above. In establishing
its record system, each State should seek to meet two major
objectives:
A a. development of records which will establish a health
\ care history for each child which details screening
tests provided, conditions uncovered, results of
diagnosis, and services rendered (by condition) so
that costly and unnecessary repetition of screening
and diagnostic procedures will not occur, and appro-
priate medical treatment will be facilitated; and
b. development of a data base which will allow for de-
tailed analysis of the costs and benefits of the
screening program in terms of: cost of screening,
conditions uncovered, treatment received (by condition),
cost of treatment, and treatment needed but not avail-
able under the State plan. :
To meet these objectives, establishment of an individual health
record on each child is necessary. It is expected that SRS will
require, on an annual basis, for a sample of children covered under
the program, this detailed information in order to establish base-
line data on the health needs of low-income children, and to
evaluate the costs and effects of the program.
>
MSA- PRG- 21
6-28-72
5-70-00 p. 8 é
Medical
Agslastance
Manual
Part 5. Services and Payment in Medical Assistance Programs
5-70-00 Early and Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 21
5-70-20 B, Summary of Basic Provisions (Continued)
13. The State agency should publicize the EPSDT program in a variety
of ways to reach eligible and potentially eligible individuals and
casefinders such as caseworkers, public health nurses, teachers,
pharmacists and community groups attached to churches, schools,
health and recreation centers, etc, All media such as posters
flyers, pamphlets, radio, TV and newspaper announcements should be
used, Information should be given about whom the program is intended
to serve, its goals, and specifics about where to go and what to do
to have a child screened, The messages should be simple, clear and
free of administrative jargon. In areas in which English 1s not the
first language spoken in low-income homes, bilingual announcements
should be made. : C
C. Coverage
1, The EPSDT requirement applies to all individuals under 21 (or ini-
tially, under 6 years of age) who are determined to be eligible for
Medical Assistance, This includes recipients of financial assistance -
AFDC, AB, and APTD, :
If the State plan includes the following classifications of eligibles,
these individuals must be included in the EPSDT program: (a) children
in foster homes or in private institutions for whom public agencies
are responsible in whole or in part; (b) children in unemployed father
families; (c) all financially eligible individuals under 21, without
regard to categorical relationship; and (d) children in families that
would be eligible as AFDC families, but who have not applied for
assistance.
If the State plan includes services under 1905(a)(4) for medically
needy individuals, such individuals must also be included in the
EPSDT program, The State has the option of beginning with medically
needy children under age six if it is unable from the outset to make
the services available to all medically needy persons under 21,
MSA- PRG- 21
6-28-72
5-70-00 p. 9
AS
Medical
Assistance
Xx
Manual
Part S. Services and Payment in Medical Assistance Programs
5-70-00 Early and Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 21
5.70-20 D, Case Finding
1. To actively seek out eligible individuals for the EPSDT program, the
State agency should develop procedures: (a) to inform parents that
these services are available for their children, and when and where
they are provided; (b) to make sure that they understand the nature
and purpose of the screening program; (c) to enlist the help of
other community agencies in casefinding activities; and (d) to assure
that families are helped, if they need such assistance, to obtain
transportation to the screening center and for diagnostic studies
and treatment, The title XIX agency must assure the provision of
transportation when necessary.
i 2. The primary targets for these outreach efforts are individuals under
21 in families who are applying, and have been determined eligible,
; for public assistance or medical assistance and the same age group in
families presently receiving such assistance.
3, A variety of outreach methods should be used primarily at the local
level in the community close to the people the program is trying to
reach, :
Bilingual materials and interpreters should be used as indicated by
the population served. Among the outreach mechanisms that can be used
are:
a. Where group intake meetings are held, availability of EPSDT
services should be stressed. This can be a brief explanation,
essentially to alert applicants, because these sessions must
cover much material and applicants usually have more overriding
concerns at this point of intake, ~
e
a
b. A written, simple explanation of the EPSDT program should be
sent out to each family as soon as possible after eligibility
has been established.
| Co MSA- PRG-21
6-28-72
5-70-00 p. 10 » | »
Medical Niiva i
Assistance |
Manual
Part 5, Services and Payment in Medical Assistance Programs
5-70-00 Early and Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 21
5-70-20 D, Case Finding (Continued)
c, Similar interpretation should be given to families ‘presently
receiving public assistance, There should be a variety of
opportunities for contact with them, These include a written
explanation of the EPSDT program sent with the monthly check,
an explanation of the services by the eligibility worker when
reestablishing eligibility, discussion with the family by a
caseworker who may be helping the family with other problems,
or a visit by an outreach worker from the county welfare de-
partment, health department or other community agencies coopera‘-
ing in the EPSDT program, .
screening program, they can seek further information from the
public assistance worker, the medical assistance unit, case
aides employed by the welfare agency, health department or OEO,
or from a caseworker in the service programs. The State agency
should assure that arrangements are made for assistance to
families on a local level in obtaining and using services under
the EPSDT program. Some families will need help: (1) in under-
standing the importance of preventive health services and early
diagnosis and treatment, (2) in overcoming their fears of doctors
and other aspects of medical care, (3) in mobilizing themselves
to make use of a health service for which they may feel no
pressing need; and (4) in arranging for transportation, baby-
sitting services or other services to enable parents to bring
children to the screening center or to other providers of health
services, Parents who are burdened with other family problems
and financial stress may not be able to make much effort to seek
screening examinations for their seemingly well children.
d. Families should be told that if they have questions about the
e. Consent of the child's parent or guardian should be obtained before
screening or other health services are provided. In accordance
with Section 1907 of the Social Security Act, no person eligible
for services under title XIX may be compelled to undergo any
medical screening, diagnosis or treatment if the person (or, in
the case of a child, his parent or guardian) objects to such services
on religious grounds, C
MSA- PRG-21
6-28-72
5-70-00 p. 11
Medical
Assistance
Manual
Services and Payment in Medical Assistance Programs
Early and Periodic Screening, Diagnosis, and Treatment of
5-70-20
1.
2.
3.
Eligible Individuals Under Age 21
E. Screening
Although screening should be performed under the supervision of a
physician, dentist, optometrist, audiologist or other health care
specialist, or with consultation from such persons, the carrying .
out of interviews, observations and tests that can constitute the
screening process may not require their presence during screening.
Nurses, trained health aides, laboratory technicians and trained
volunteers can conduct the screening activity. yo
Screening, as defined in these guidelines (5-70-20-A),1i8 intended
to be carried out with large groups of individuals under 21 and is
not generally a service provided on a one-to-one basis. There may
be communities where the size of the Medicaid population under age
21 does not lend itself to a group screening approach. In these
areas, health assessment on an individual basis or of small groups
of children by a physician or nurse may be necessary to accomplish
the objectives of the regulation,
The services of a broad spectrum of health personnel and facilities
will be necessary if the eligible population is to be screened and
diagnosed and if periodic screening is to be done at appropriate
intervals. Programs or agencies that may be suited to provide health
screening are State and local health departments, school health pro-
grams, Crippled Children's Services, Maternity and Infant Care projects,
Children and Youth projects, Head Start and Health Start programs, .
neighborhood health centers under OEO or other auspices, and day care
centers, Other participants to provide screening services may be
found among clinics, hospitals, medical, dental and optometric schools,
voluntary health agencies, developmental disability projects, prepaid’
health care plans and other groups of practitioners in a variety of
HMO arrangements.
The screening process as a mechanism to maintain an individual in good
health through early casefinding cannot be a "one shot" event if it is
to be effective, Screening should be done periodically between birth"
and 21 years. Screening procedures should be repeated at intervals for
MSA- PRG-21
6-28-72
5. 70-00 p. 12 . i»
fMMedical
Agglstance
Manual
Part Se Services and Payment in Medical Assistance Programs
5-70-00 Early and Periodic Screening, Diagnosis, and Treatment of
5-70-20
Se
6.
Eligible Individuals Under Age 21
BE, Screening (Continued)
at least certain tests if incipient disease or illness is to be found,
Advice on intervals between screening tests should be sought from
public health specialists and other medical and dental experts within
the State, Other resources for such guidance will be found in the
bibliography in Appendix B. eS Pa?
Although most tests should be repeated at intervals, some procedures
will need to be done only one time or will be limited to an age group,
For example, properly done scréening for sickle cell trait will need
to be done only one time for Negro children, while all children,
especially those living in old delapidated buildings or in urban or
rural slums, should be screened periodically for lead poisoning between
one and six years of age, For children over six years lead. poisoning
screening needs to be done only when medically indicated.
Principles related to confidentiality of information must be observed
in the EPSDT program, and reports of the screening results and of
other health services provided should not be made available to individ-
uals outside the screening program or the title XIX agency without the
consent of the parent, guardian or, if appropriate, the person between
16 and 21 years of age who has received screening or other health
services, :
When screening services are provided in ‘schools and in other settings
serving children from public assistance families and from families
not on public assistance, careful procedures should be observed so
that individuals eligible for Medicaid are not singled out and publicly
identified as recipients of Medical Assistance. ek
It is desirable that a parent or other responsible adult accompany
the child to the screening center, but when this is not possible or
practical, arrangements should be worked out by the title XIX agency,
~ the screening center, and a follow-up worker (social worker, health
aide, neighborhood worker,- etc,) to discuss the results in a visit to
the home or in contacts with the family elsewhere, ” #2 :
MSA-PRG-21
6-28-72
5-70-00 p. 13
Medical
Assistance
Manual
Part 5, Services and Payment in Medical Assistance Programs
5.70-00 Early and Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 21
5.70-20 E. Screening (Continued)
7. It is recommended that the elements described below be fncluded as
the minimum content of this program to prevent disease, chronic
{1lness and disability and to detect incipient physical and mental
health problems, In planning for fnclusion of these procedures,
appropriate professional consultation should be utilized.
(NOTE: In the interest of possibly mandating a minimum
package of screening procedures, SRS is conducting
further consultation with authorities in the field
of child health, If this consultation leads to the
conclusion that such mandating is supportable .
according to substantial professional judgment, an
appropriate revision of these guidelines will be
tgsued, Until such time, however, the elements
described below should be regarded as the minimum
recommended components of a screening program)
a. History. Obtain an adequate health and developmental history
(e.g. a check-sheet) from the parent or other responsible
adult who is familiar with the child's health history. This
could be done at the time of the screening visit or prior to
the screening appointment through a form sent to the parent
for completion, In some situations, a home visit by the
public health nurse, caseworker or health aide may be necessary
to re-emphasize the importance of bringing the child in for
screening and to help the parent complete the health history
sheet, Some parents will be able to provide the information
with minimal or no assistance, Others will need considerable
help in providing data that are adequate to determine if a
child has health problems, Such information is essential to the
screening procedure, In addition, pertinent social information
provided by the caseworker or eligibility worker should be made
available to the screening center staff, :
MSA-PRG-21
6-28-72
Se p. 14 & ®
Medical AAS
Assistance
Manual sh
Part 5, Services and Pgysent in Medical Assistance Programs
5-70-00 Early end Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 1)
5-70-20 E, Screening (Continued)
b, Physical Growth. Record the child's height and weight and -
compare his measurements with those considered normal for
children of his age. In the first two or three years of life,
head circumference measurements are important, A graphic
recording sheet should be used to chart height and weight,
c. Developmental Assessment, Information from the parent or other
person who has knowledge of the child's development, observation
of the child, and talking with the child can all be useful in
assessing the individual's development, A test such as the
Denver Developmental test can also be used for this purpose,
This part of the screening procedure should include assessment
of eye-hand coordination, gross motor function (walking, hopping, C3
climbing), fine motor skills (use of hands, fingers), speech
development, self-help skills (dressing, eating, personal care),
and behavioral development, : ¥
d. Unclothed Physical Inspection, Check for obvious physical
defects including orthopedic disorders, hernia; skin disease,
genital abnormalities, and other deviations that are readily |
observable. Physical inspection includes a heart examination,
It could be accomplished through an examination with a steth-
oscope or a cardiac scan, along with observation of the child's
color and history of difficulty in breathing.
e. Ear, Nose, Mouth and Throat Inspection. Inspect the ears, nose,
mouth and throat for evidence of obstructions or pathological
conditions and for general assessment of child's dental condition.
Extensive dental screening is unnecessary since almost all
children have some dental problems and definitive dental diagnosis
and treatment will usually be necessary, This inspection, however,
will provide an opportunity to observe the individual's teeth and
gums, 3
MSA- PRG- 21 £4
6-28-72
5-70-00 p. 15
+5 Medical
Assistance
IAI AY
Manual
Part 5. Services and Payment in Medical Assistance Programs
5-70-00 Early and Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 21
5-70-20 E. Screening (Continued)
£. Vision Testing. Administer a vision screening test appropriate
to the child's age. Consultation by ophthalmologists and
optometrists can be of help in determining the type of tests
to be used and the criteria for determining when a child should
be referred for diagnostic examination.
g. Hearing Testing. Administer a hearing screening test appropriate
to the child's age. Consultation on suitable tests for screening
and on methods of administering the tests should be obtained from
audiologists or from State health or education departments.
: h. Anemia Test. The most easily administered test for anemia is
( a microhematocrit determination from venous blood or a finger-
stick, This should be dcne on all children or, if possible,
a hemogloblin concentration which will give a more accurate
determination of anemia should be done.
i, Sickle Cell Test. Check all Negro children for sickle cell trait,
This may be done with a sickle cell preparation or a hemoglobin
solubility test, If a child has been properly tested once for
sickle cell disease, he does not have to be tested again,
i j. Tuberculin Test. Give a tuberculin test to every child who has
not had one within one year.
k. Urine Screening. Carry out a rapid urine screening on all
children for the presence of sugar, albumin and bacteria.
1. lead Poisoning Screening. It is not possible to identify which
children may have had undue exposure to lead-based paint and other
sources of lead poisoning, except by determination of blood- lead
levels, Therefore, all children between the ages of 1-6 should be
periodically screened for lead poisoning. Children 6 and over should
MSA- PRG-21
6-28-72
H
N
i
1
'
1
t
5-70-00 p. 16 4 »
Medical
Agslgtance
Manual
Part 5. Services and Payment in Medical Assistance Programs
5-70-00 Early and Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 21
5-70-20 E, Screening (Continued)
be screened when medically indicated. The principal source
of ¢thildhood lead poisoning is lead-based paint, but pollution.
of the environment from such things as burning lead batteries
and repeated exposure to fall-out particles of lead that get
into the soil and are ingested by a child may also result in
lead poisoning, Early identification and prompt treatment
of symptomatic and asymptomatic (over 80 mg/100 milliliters
of whole blood) cases can prevent the serious sequelae of
lead poisoning, such as mental impairment, mental retardation
and involvement of the central nervous system, Venous or
capillary blood samples may be used, depending on local
laboratory facilities,
m. Nutritional Status. Physical and laboratory determinations ( :
carried out in the screening process will usually yield
information useful in assessing nutritional status, Of par-
ticular importance are measurements of height, weight, head
circumference and hemoglobin concentration or hematocrit, A
child having any detectable nutritional deficiencies should
be referred to a nutritionist or public health nurse for
consultation,
n, Immunization Status. The screening program presents an
~ excellent opportunity to ascertain a child's immunization
status, a major tool in preventing disease and disability.
During the screening process, assess the child's immunization
status; i.,e., whether he has been immunized against diphtheria,
pertussis, tetanus, polio, measles, rubella, and mumps, and
whether he is in need of booster shots, When it is available,
the child's immunization record should be brought to the
screening center, If immunization or updating of immunization
ie needed, provide the immunization or updating at the screening
center or make sure it is done through the facilfty or provider
to whom the child goes for child health supervision.
~ MSA-PRG- 21 Cc
6-28-72 :
5-70-00 p. 17
Medical
Assistance
Manual
Services and Payment in Medical Assistance Programs
Early and Periodic Screening, Diagnosis, and Treatment of
5- 70-20
8.
9.
10.
Eligible Individuals Under Age 21
E. Screening (Continued)
In addition to the basic screening procedures described in section
E7 above, there are several other screening tests that should be
considered. Their appropriateness will be determined by the
individual's age, sex, health history, clinical symptoms and exposure
to disease. Among the procedures that could be included in the
screening process are a cardiac scan (if not done in the course of
physical inspection), chest x-ray, blood pressure, pinworm slide,
urine culture (for girls), serological test, drug dependency
screening, and stool specimen for parasites, ova and blood. When
it is required for admission to school, a child should have a
smallpox vaccination,
Because the AFDC caseload is an ever-changing one and families have
varying periods of eligibility for AFDC, many AFDC children will
not be eligible for continuous health supervision under the Medicaid
program. The periodicity and continuity of screening will be affected
by the individual's eligibility for the title XIX program if the
screening center is only used for Medicaid recipients, The screening
cycle may be interrupted by the family's loss of eligibility for
assistance, It is essential that this factor be considered in
establishing a screening program and, when feasible, to provide the
screening service through a program where continuity of care is
possible, For example, such continuity could be achieved through
child health clinics in local health departments if they serve children
up to age six, Children and Youth projects, Maternity and Infant Care
projects (1f the child continues into a Children and Youth project),
a Head Start program, or a school health program,
Although the regulation is intended to include all eligible
individuals under 21, States whose fiscal problems or limited medical
resources make it impossible initially to serve the entire age range
up to 21 may begin with those under six years, These States must
describe, in the State plan amendment provided for EPSDT, the
schedule for phasing in such services by age groups. 1f a State
has to phase in an EPSDT program, it is encouraged to phase in
5-70-00 p. 18 lr ®
Medical
Aselsiance
Manual
Part Se Services and Payment in Medical Assistance Programs
5-70-00 Early and Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 21
5-70-20 E, Screening (Continued)
1.
2.
3.
gradually by extending the services to other age groupings within
the under 21 population so that by 7-1-73, the services will be
available to all those under 21 years, For example, additional
age segments (6-12, 12-18, 18-21) could be added at three-month
intervals, The State agency may determine the size and sequence
of age groups six years and over, in accordance with the particular
needs of young people in the State, If a State has good health
coverage for elementary school children, it might wish to focus
EPSDT, after screening the children under 6, on older individuals
from 16 to 21, In any case, by July 1, 1973 the EPSDT program
must be available to all eligible individuals under 21.
F, Diagnosis i C
When screening tests indicate the need for further evaluation of
an individual's physical or mental health, diagnostic studies, as
necessary, must be done. Referral for diagnosis should be made
without delay, and there should be follow-up to make sure that
the individual receives diagnostic evaluation, :
Regardless of the limits of treatment under the State plan, every
individual found to have a possible health problem should be
referred for diagnosis, Until a diagnostic examination has been
done and recommendations for treatment made, it may not be known
whether such treatment is included under the State plan,
Diagnosis can be accomplished in several ways, The family may
wish to have the child examined by the family physician or by
another physician of its choice. Or the individual can be referred
to a Maternity and Infant Care project, a Children and Youth project,
Crippled Children's Services, a neighborhood health center, a
comprehensive health services center, a rehabilitation center, a
hospital out-patient department, or to any other practitioner or
facility qualified to evaluate and diagnose a young person's
health problens,
MSA- PRG-21
6-28-72
5-70-00 p. 19
x 41y 1
Medical
1¥ Aga Assistance
+X
Manual
Part 5S. Services and Payment in Medical Assistance Programs
5. 70-00 Farly and Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 21
5-70-20 PF. Diagnosis (Continued)
4, Unlike other health needs, dental problems are so prevalent that
most individuals will need diagnostic evaluation and some treat-
ment. The examination, diagnosis and treatment planning must be
the responsibility of legally qualified dental practitioners and
their auxiliary personnel,
5. Diagnosis can usually be accomplished on an out-patient basis, but
some diagnostic procedures may require the use of in-patient
facilities, Where in-patient servicés are necessary to complete
the diagnosis, they should be provided as part of the diagnostic
services, :
6. In many cases when treatment is recommended, the necessary care
g can be covered within the amount, duration and scope of treatment
& available under the State plan. To assure that the individual
- receives necessary treatment, the Medical Assistance Unit should
be informed of the recommendations resulting from the diagnostic
study. Some families will necd assistance in arranging for treat-
ment even when it is included under the State plan, For treatment
not available under the Medicaid program, referral help should be
given to the family by the Medical Assistance Unit, the caseworker,
public health nurse, health aide, or some other person who may be
able to assist the family in finding treatment resources outside
the Medicaid program, For AFDC families, such help is a specific
requirement in the regulation related to "Service Programs for
Families and Children," (45 CFR Section 220,24). For AB and
APDT recipients, similar social services are available if a State
elects to provide social services under those plans; "Service
Programs for Aged, Blind, or Disabled Persons," (45 CFR Section
222.44), Joint planning by the title XIX agency and service
agency should include assistance to families in following-up on
recommendations and obtaining needed care.
G., Treatment
1. Treatment may be limited to the amount, duration, and scope of the
State plan, except that even if not otherwise included in the State
MSA- PRG- 21
6-28-72
pn a
A "a = M i
Pon { . : {
i 8 : i
. Sa 70- 00 Pe 20
Medical
Agselstance
Manual
Part 5, Services and Payment in Medical Assistance Programs
5-70-00 Early and Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 21
5-70-20 G. Treatment (Continued)
plan, eyeglasses, hearing aids, and other treatment for visual and
hearing defects, and dental care to maintain dental health must
As a minimum, the dental services that must be provided include
emergency services, preventive services and therapeutic services
for dental disease which, if left untreated, may become acute
dental problems or may cause irreversible damage to the teeth or
supporting structures, Other therapeutic services for dental
disease should be provided as rapidly as the availability of
resources permits, Dental services include:
a. Emergency Services: Emergency dental care services 4
are those necessary to control bleeding, relieve pain, “
eliminate acute infection; operative procedures which
are required to prevent pulpal death and the imminent
loss of teeth; treatment of injuries to the teeth or
supporting structures (e.g., bone or soft tissues
contiguous to the teeth); and palliative therapy for
periocoronitis associated with impacted teeth, Routine
restorative procedures and root canal therapy are not
considered emergency procedures,¥
b. Preventive Services: Preventive dental services include:
1, Instruction in self-care oral hygiene
procedures (provided individually or in groups).
2, Oral prophylaxis (cleaning of teeth), necessary
as a precursor to the application of dental
caries preventives in areas where such applications
are indicated (provided in groups or individually),
or oral prophylaxis independent of the application
of caries preventives for patients 10 years of
age or older."
*Based on definition of emergency services approved by the Council on (
Dental Health of the American Dental Association,
MSA- PRG-21
6-28-72
S- 70-00 Pe 21
— Medical
Assistance
— Manual
Services and Payment {n Medical Assistance Programs
Farly and Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 21
Treatment (Continued)
c. Therapeutic Services: Therapeutic Services include:
1. Pulp therapy for permanent and primary teeth.
2. Restoration of carious (decayed) permanent and
primary teeth with silver amalgam, silicate cement,
plastic materials and stainless steel crowns.
Scaling and curettage.
Maintenance of space for posterior primary
teeth lost prematurely.
Provision of removable prosthesis when masticatory
function is impaired, or when existing prosthesis
{s unserviceable, or in instances when esthetic
considerations interfere with employment or
social development,
Limitations in State plans on the amount, duration, and scope of
medical and remedial care an
ross purposes
with Congressional intent to prov
and young people in their early years to give them optimum opportunity
for full, productive lives, free from disabling conditions. It
should be reemphasized, therefore, that this regulation makes it
possible, regardless of State plan limits which are otherwise
applicable, to provide to eligible individuals within the EPSDT
age group any needed medical and remedial service that can be
included under any provision of Section 1905(a) of the Social
Security Act for individuals under the age of 21.
Federal financial participation is available to any State that
elects to provide Fealth services for the EPSDT group beyond the
amount, duration, and scope limits of the State plan for individuals
21 years of age or older,
|
MSA- PRG-21
6-28-72
5-70-00 p. 22 & No
Medical
Assistance
Manual
Part 5. Services and Payment in Medical Assistance Programs
5-70-00 Early and Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 21
5-70-20 G. Treatment (Continued)
3. If a State provides services in added amount, duration and scope
for individuals under age 21, it is not required to make the same
services in the same amount and duration available to individuals
over 21 years.
H. Interagency Cooperation
1. It is anticipated that the State agency will have to draw upon the
resources of many health programs and providers to implement this
regulation, As already indicated, programs such as Maternity and
Infant Care projects, Children and Youth projects, Crippled
Children's Services, developmental disabilities projects, child health
clinics, Head Start, Health Start, neighborhood health centers under 3
OEO or other auspices, school health programs and other health care {
programs have screening and diagnostic facilities and, in some
instances, provide treatment,
2. Where appropriate, the State agency should pay for services provided
through these and similar prograns, just as it pays individual
providers of service under its State plan, in accordance with the
provisions of 45 CFR 250,30. In general, the title XIX agency
should pay for any screening, diagnostic and treatment services
provided to an individual within the amount, duration, and scope
of the State plan, including those additional services required
under the EPSDT regulation, Factors that will have a bearing on
whether the services are paid for by title XIX funds include the
administrative arrangements of the program that provides the
services (e.g. whether a fee schedule has been established,
whether such services are available to individuals in the community
without chargé, whether the clinic staff is paid on a salaried or
: fee- for- service basis, etc.); the problems in estimating the cost
for an individual Medicaid recipient when the program provides care.
to many non-Medicaid patients; and the administrative complexities
of determining costs when some items of treatment are included in
a State title XIX program and others are not,
MSA- PRG-21 (
6-28-72
5-70-00 p. 23
TT a : Medical
£08 1 - Assistance
7} ee Manual
Part 5. Services and Payment in Medical Assistance Programs
5-70-00 Early and Periodic Screening, Diagnosis, and Treatment of
Eligible Individuals Under Age 21
5-70-20 H, Interagency Cooperation (Continued)
3, Written interagency agreements between the State title X1X agency
and providers of services under this regulation are essential as
a mechanism to provide a clear, mutual understanding of arcas of
responsibility, services provided, referral arrangements, arrange-
ments for payment, and other elements that contribute to smooth
working relationships between agencies.
4, The interagency agreements should be developed in accordance with
SRS Program Regulation 40-19; 45 CFR 251,10 - "Interrelations with
State Health and State Vocational Rehabilitation Agencies and with
title V Grantees." Further elaboration of this regulation will be
issued as guidelines,
MSA-PRG-21
6- 28-72
EXHIBIT P
y -.. este er —— ———— a —
Depcriment of Health
and Human Services
state medignid manual ®
@ Part 5 — EMy and Periodic ScreShing, ina"
Diagnosis, and Treatment
(EPSDT)
Transmittal No. 2, : oo APRIL 1368
ou! r 4 A 13 NN =
NEW MATERIAL PAGE NO. qv. )' REPLACED PAGES
Lideg
Table of Contents, Part 5 5-1 (1 page) _
Sec. 5010 - 5450 5-3 - 5-39 (39 pages) 5-1 (1 page)
MANUALIZATION — EFFECTIVE DATE: Not applicable.
This transmittal introduces Part 5: Early and Periodic Screening, Diagnosis, and Treatment
(EPSDT). It contains EPSDT program guidelines and implements §51902(aX43) and 1905(a)(4 XB)
of the Act, including revisions enacted by P.L. 97-35, the Omnibus Budget Reconciliation Act
of 1981, and P.L. 37-248, the Tax Equity and Fiscal Responsibility Act of 1982.
Discard previously issued Program Regulation Guides (PRG), Field Staff Information and
Instruction Series (FSIIS), Policy Interpretation Questions (PIQ), Action Transmittals
(AT), and Information Memoranda (IM) concerning EPSDT.
) Changes and additions to the EPSDT guidelines will be issued as Part 5 revisions.
Forward requests for additional copies of this part, or for a change in the distribution
list to: 4
liealth Care Financing Administration
Printing and Publications Branch, OMB
377 East High Rise Bldg.
6325 Security Blvd.
Baltimore, MD 21207
This transmittal obsoletes ATs: 75-50, 76-86, 78-2, 78-59, 79-101, 80-80, and also, IMs 78-46
and 79-3. on
1A
HCFA-Pub. 45-5
he
A
a
g
e
Xi
ah
In
a
a
S
S
wi
a
i
BO
I
R
t
e
A
E
R
a
A
pT
o
h
Sn
SEN
A
PR
ao
t
TR
IE
UR
S
D
ARR
R
R
BE
a
I
S
i
A
A I
L
I
A
t
he
BR
DS
ER
SE
2
A
S
S
Ea
¥
04-88 EARLY AND PE
iss—— =
3. Approp@e Vision Testing, - Administ an age-appropriate vision
assessment. Consultation by opthalmologists and optometrists can help determine the
type of procedures to use and the criteria for determining when a child should be referred
for diagnostic examination,
RIODIC SCREENING, DIAGNOSIS AND TREATMENT 0122(Cont.)
4. Appropriate Hearing Testing, - Administer an age-appropriate hearing
assessment, Obtain consultation and suitable procedures for screening and methods of
administering them from audiologists, or from State health or education departments.
5. Appropriate Laboratory Tests. - Identifying as Statewide screening
requirements the minimum laboratory tests or analyses to be performed by medical
providers for ° particular age or population groups. Physicians providing
screening/assessment services under the EPSDT program use their medical judgement in
determining the applicability of the laboratory tests or analyses to be performed. If any
laboratory tests or analyses are medically contraindicated at the time of
screening/assessment, provide them when no longer medically contraindicated. As
appropriate, conduct the following laboratory tests:
a. Anemia Test. — The most easily administered test for anemia is a
microhematocrit determination from venous blood or a fingerstick.
b. Sickle Cell Test. — Diagnosis for sickle cell trait may be done with
sickle cell preparation or a hemoglobin solubility test. If a child has been properly tested
once for sickle cell disease, the test need not be repeated.
c. Tuberculin Test. — Give a tuberculin test to every child who has not
received one within a year,
d. Lead Toxicity Screening. — All EPSDT eligible children, ages 1-5
should be screened for lead toxicity, using the erythrocyte protoporphyrin (EP) test as the
primary screening test. Children with any elevated EP (greater than, or equal to, 50
micrograms per deciliter of whole blood) should receive a blood lead test. Children with
both an elevated EP and an elevated blood lead (greater than, or equal to, 30 micrograms
per deciliter) require diagnosis and treatment, which includes environmental
epidemiologic services to identify the source of lead, and periodic re-evaluation.
e. Others. — In addition to the the tests above, there are several other
tests to consider. Their appropriateness are determined by an individual's age, sex,
health history, clinical symptoms and exposure to disease. These include a urine
screening, pinworm slide, urine culture (for girls), serological test, drug dependency
screening, and stool specimen for parasites, ova and blood.
6. Dental Screening Services. - Although an oral examination may be part of a
physical examination, it does not substitute for examination through direct referral to a
dentist. The judgement that dental treatment is or is not necessary can only be made by
a dentist, It is the intent of the regulation not to disrupt continuous, comprehensive
dental care situations, but rather to encourage and develop them,
Rev, 2 5-11
EXHIBIT Q
a
OF HEALTH, EDUCATION, AND WELFARE
Social and Rehabilitation Service olor ouan al a
American Academy of Pediatrics
% a SCREENING
CHAPTER 21. SCREENING FOR INCREASED LEAD ABSORPTION
1. Purpose and Rationale. The purpose of screening
for increased lead absorption is to prevent death
and disability from lead poisoning. This can be ac-
complished by identifying children who have absorbed
an undue amount of lead from their environment, re-
ducing their exposure to lead and medically removing
already absorbed lead from certain children who have
ill effects or are in danger of developing ill effects.
It is estimated that more than one hundred children
die each year from lead poisoning and several hundred
more have permanent brain injury following recovery
from symptomatic lead poisoning. It is likely, but
not certain, that thousands of other children may suffer
various degrees of brain damage from lead poisoning
which never produces obvious symptoms and thus is un-
noticed or unreported.* Once acute symptoms have
developed, presently available treatment is not fully
effective in preventing death or brain damage.
The major cause of symptomatic lead poisoning in chil-
dren is repeated ingestion over several weeks or
months of paint chips or putty chips containing lead
pigment from old and deteriorating homes. Such
* The prevalence of renal and peripheral nerve
damage from lead poisoning in children is unknown,
but such damage has been reported in adults.
187
ingestion occurs almost exclusively in children
between ages one and six years who live in, visit
or obtain day care in buildings which contain
loose or peeling lead-pigment paint. At least
ten percent of children between ages one and six
live in such circumstances. Surveys of such chil-
dren indicate that from 15 percent to more than 50
percent, depending on the community, have absorbed
sufficient lead to produce blood lead levels well
above those found in non-exposed children. 1In
some children dust, dirt and automobile exhaust
fumes account for a part of this increased absorp-
tion. Exposure to these sources alone rarely if
ever causes symptomatic lead poisoning, but it may
reduce the amount of ingestion of paint necessary
to cause symptoms. If children with undue absorp-
tion can be identified through screening and
separated from the source of lead, both sympto-
matic and silent lead poisoning can be prevented.
2. Identifying Children To Be Screened. All chil-
dren between ages one and six who live in poorly
maintained buildings built before 1950, who visit
relatives, friends or babysitters in such buildings
or who obtain day care in such buildings should be
screened, unless careful epidemiologic surveys have
shown that lead poisoning is not a problem in the
community. Any child known to be exposed to other
sources of lead, such as industrial lead fumes,
should also be screened. Children with unexplained
gastrointestinal symptoms, central nervous system
symptoms or anemia should also be tested for undue
lead absorption, but such testing is considered a
part of the diagnosis of these conditions, not part
of screening as such.
3. Frequency of Screening in Susceptible Children.
Children at risk should be screened at least yearly
SCREENING
beginning at their first birthday or during the
months of May, June and July following their first |
birthday. (Blood lead levels are higher and evi-
dence of intoxication more frequent in the summer J
months.) If possible, children should be screened A
two or three times a year (perhaps in March, June
and August) until age three, One to three is the
most susceptible age period, and it is possible for
a child in this age group who has had a normal
screening test to develop irreversible damage from
lead poisoning in less than one year.
children who have negative screening tests through-
out the second and third years of life probably do
not live in an environment which permits excessive
exposure to lead. Similarly, four- and five-year-
olds who are normal at first testing probably have
avoided the risk of lead ingestion. Retesting of
these children, unless their environment is changed,
is much less important than testing younger chil-
dren at risk. Children with normal or slightly
elevated lead levels who are no longer exposed to
lead hazards (because of a move to newer housing,
for example) need not be retested.
4. Methods for Use in Screening for Undue Lead
Absorption.
a) Blood lead determinations
Currently the most widely accepted method
of screening for undue lead absorption is
the blood lead determination* using
* Other methods, including urine lead levels,
urine coproporphyrins and urine delta amino
levulinic acid (ALA), have been proven to be
inadequately sensitive.
SCREENING
atomic absorption spectrophotometry,
anodic stripping voltammetry or the
dithizone method.
All these methods require meticulous attention to
the method of obtaining the blood sample, complex
special laboratory equipment costing many thousands
of dollars, highly skilled laboratory technicians,
and continuing expert supervision of laboratory
methodology. These can best be achieved by having
all blood samples tested in a few centralized well-
supervised laboratories.
The particular laboratory method chosen is much less
important than the skill, training and supervision
of those who perform the laboratory determination.
Planning for blood lead testing in EPSDT programs
should be carefully coordinated with testing already
taking place in the community, region or state so
that a minimal number of laboratories can serve all
programs.
Dust and dirt on the skin of children can contain
sufficient lead to contaminate the blood sample,
producing laboratory values which greatly overstate
the blood lead levels. Similarly, needles, syringes,
glassware, cotton swabs and disinfectants used to
obtain or to transport blood samples can contain
sufficient lead to give falsely high readings.
For this reason, blood samples must be obtained
by persons trained and supervised in careful
cleansing of the skin site from which blood will
be obtained. all disinfectants, needles, syringes
and glassware used in obtaining samples must be
certified as lead-free by the laboratory respon-
sible for blood testing.
Because of the risk of contamination during sample
collection and limitation in the precision of
laboratory measurements of lead, duplicate deter-
minations should be performed on each blood sample
tested. When capillary blood 1s used, two tubes
should be submitted and tested. Even with good
quality control, the precision of the laboratory
test is about i5 micrograms of lead. Thus a lab-
oratory report of 40 micrograms indicates a "true"
level between 35 and 45 micrograms. Two successive
determinations with values of 40 and 48 may repre-
sent laboratory variation rather than any change
in the status of the child. All persons who inter-
pret blood lead level reports must keep this im-
precision in mind, or they may make faulty
conclusions.
Any child with a blood lead level over 40 micro-
grams/100 ml should have a confirmatory blood
lead determination. Children with a blood level
of over 50 micrograms/100 ml should be evaluated
at the time the second blood sample is obtained
for the presence of any symptoms and for evidence
of metabolic effects of lead toxicity.
b) Free erythrocyte protoporphyrin tests
(FEP) .
Because of their recent introduction,
tests for blood protoporphyrin have
been less widely used and accepted than
have blood lead tests. However, as a
screening test, the FEP test has several
potential advantages over blood lead de-
terminations. The test is simple and
rapid and is unaffected by lead contamina-
tion of the skin or glassware. It can
be performed in most hospital laboratories,
or even with portable equipment. Re-
sults can be reported within less than
an hour so that follow-up can begin im-
mediately. The duplicate or triplicate
determinations necessary to achieve
SCREENING
SCREENING
accuracy in blood lead determinations
are not necessary for FEP determinations.
The FEP has been found to identify cor-
rectly all children with blood lead
levels over 50 micrograms/100 ml, the
children who may need immediate treat-
ment. Its low cost makes frequent re-
peated testing of high-risk children
more feasible.
The disadvantage of the FEP test is that a pro-
portion of children with blood lead levels between
40 and 60 micrograms/100 ml, who may have undue
absorption of lead and thus need protection
against further ingestion, will have normal FEP
values. (The proportion will vary with the FEP
level chosen as the cut-off point between normal
and abnormal values.)
Also children with iron deficiency have elevated
FEP levels, and in some communities a high pro-
portion of children with positive FEP tests will
have iron deficiency anemia rather than elevated
blood lead.
whichever test is chosen for initial screening,
laboratory facilities for blood lead determina-
tion must be present to evaluate and manage
children with positive screening tests. Simi-
larly, it is highly desirable to have the capa-
bility of performing the FEP test, since it is
an excellent measurement of the toxic metabolic
effects of lead. F
l
a
3
a
a
Di
r
a
ei!
In communities or regions in which laboratory
facilities for blood lead testing are adequate,
the blood lead determination may be the best
current choice for screening. In communities
in which blood lead testing facilities are cur-
rently inadequate, use of the FEP test can permit
p
i
n
d
d
A
EE
immediate screening of a large number of sus-
ceptible children, and the limited blood lead
testing capacity can be used for confirmation,
treatment and follow-up. If current research
should indicate that children screened as nor-
mal by the FEP method are truly of very low
risk, all screening programs could substantially
reduce their costs by using this method.
1f the FEP test is used as the first screening
test, all children with a positive screening
test (level for positive to be determined by
testing lab) should have an immediate blood
lead determination and should be evaluated and
treated, if necessary, for iron deficiency.
When this blood lead determination is above
40 micrograms/100 ml, the child should be eval-
vated and managed in the same way as a child
who has had two blood lead levels over 40
micrograms/100 ml. When the blood lead level
is below 40, repeat screening should be sched-
uled at the appropriate interval.
5. The Meaning of a Negative Screening Test.
A child with a blood lead level under 40 micro-
grams/100 ml on initial or confirmatory testing,
or a child with a negative FEP test, probably
has not yet absorbed enough lead to be at im-
mediate risk of developing clinical lead poison-
ing. He or she should be retested at periodic
intervals according to age and residence (see
Section 3). The child's parents should be made
aware of the sources of lead in the environment
and of steps they can take to prevent undue
exposure.
6. Follow-up of a Positive Screening Test. Any
child with repeated blood lead levels over 40
193
SCREENING
SCREENING
micrograms/100 ml or who has symptoms or meta-
bolic tests suggesting lead intoxication should
immediately be evaluated by a physician or
clinic specially equipped to evaluate and treat
lead poisoning. Such a physician must be well
versed in the symptoms and signs of lead intoxi-
cation, must have access to reliable laboratory
facilities and must have effective working re-
lationships with organizations capable of inves-
tigating homes for lead intoxication hazards as
well as with authorities empowered to enforce
housing codes. Children with blood lead levels
between 40 and 50 micrograms can often be well-
managed by their own physicians or clinics using
protocols developed in conjunction with the lead
poisoning specialists.
The precise nature of this evaluation and the
criteria for removing children from their homes
and for treating them with chelating agents are
not currently standardized and are subject to
rapid change with the development of new knowl-
edge and technology.
At a minimum, all children with confirmed positive
tests should:
be evaluated for clinical signs or
symptoms of lead intoxication
be tested for metabolic evidence of
lead intoxication
have their environment investigated for
possible sources of lead exposure
be separated from any potential sources
of further lead exposure
be tested repeatedly to ensure that
separation from sources of lead is effective.
a L
e
ee
current methods for such evaluation, testing and
prevention are described in the reference materi-
als listed at the end of this chapter.
It may be necessary for a screening program to
survey all physicians, hospitals and clinics in
its region to identify those with the necessary
interests and capabilities so that referrals can
be effective.
7. Costs of Screening Procedures and Screening
Programs. Finger prick blood samples can be ob-
tained by volunteers, aides, technicians, nurses
or physicians. Non-professional workers need
only a few hours of training. Such persons can
collect 10 to 15 samples per hour.
Blood samples, properly preserved and sealed, can
be mailed or transported to a central laboratory
at little cost.
The cost of the laboratory determination of blood
lead depends almost entirely on how efficiently
expensive equipment and technicians are used. .In
laboratories processing as many as 50,000 samples
per year, the total cost can be less than one
dollar per determination, including equipment,
supplies, personnel and clerical costs. With much
lower volumes the cost can be as high as $5 to $10
or more per determination. Regional or statewide
planning of laboratory facilities is clearly
desirable.
The cost of medical follow-up and management of
all children with an initial abnormal screening
test will probably not exceed $200 per child, though
the cost for some children, especially those who
require hospital treatment, will be much more. Be-
cause screening must be repeated several times for
SCREENING
SCREENING
children at risk, because a large proportion of
children tested are likely to require either re-
testing or complete evaluation, and because each
test and evaluation is relatively expensive, all
screening programs must constantly re-evaluate all
aspects of their operation that can affect costs.
Otherwise, the costs can rapidly exceed the amount
spent on all other aspects of child health care.
The following questions must be asked:
- Is blood testing confined to children
who actually live in environments which
place them at risk?
Are blood samples obtained and tested with
methods that ensure the lowest possible
number of false positive and false nega-
tive tests? 1 _Are the following elements as economical
as is consistent with prevention of
damage to the children?
a) the criteria used for positive tests
b) the methods and criteria for evaluation
of children with positive tests
c) the criteria for hospitalization and
for chelation therapy.
Any unnecessary evaluation or treatment is costly
not only in money, but also in pain, inconvenience,
anxiety and possible side effects for the child
and the parents.
The greatest cost in the total program is the re-
habilitation of the housing in which the children
live. This cost is usually not borne by the screen-
ing program, but unless children are effectively
® » SCREENING
separated from their sources of lead, the other
costs of the screening and treatment programs will
be almost entirely wasted. A child with increased
lead absorption or lead poisoning who returns to
an unmodified home will almost certainly be poisoned
again, and the risk of permanent damage increases
with each episode. Much can be accomplished by
the family itself by frequent cleaning of floors,
window sills and other surfaces where dust collects,
and by covering hazardous painted surfaces with
wallboard or heavy contact paper.
Further Reading
For parents and lay groups:
Parents: Are Your Walls Poisoning Your Children?
U. S. Department of Health, Education and Welfare,
publication No. (HSM) 73-10009
Watch out for Lead Paint Poisoning. (Also avail-
able in Spanish) U. S. Public Health Service
publication No. 2147 (English) and DHEW publica-
tion No. (HSM) 72-5106 (Spanish)
For health professional personnel and program
planners:
Lin Fu, J.:Undue Absorption of Lead among Children -
A New Look at an Old Problem. New Eng. J. Med.
286:702-710, 1972 (Reprints available from Dr. Lin
Fu, Room 12-E 08 Parklawn Building, 5600 Fishers
Lane, Rockville, Maryland 20852)
Medical Aspects of Childhood Lead Poisoning.
Pediatrics 48:464, 1971
Chisolm, J. J.: Screening Techniques for Undue
Lead Exposure in Children: Biological and Practical
Considerations. Journal of Pediatrics 79:719-725,
1971
197
EXHIBIT R
9804
Findings of Fact
1. The amounts in controversy exceed
$10,000 for cost reporting periods ending
December 31, 1973, and December 31, 1974.
2. The provider, beginning in 1965, leased
its radiology department to a radiologist,
for a percentage of the radiology depart-
ment's gross revenues,
3. The lease provided that the hospital
would maintain certain specified equipment,
provide utilities and janitorial and mainte-
nance services and to bill those inpatients
who did not have health insurance.
4. The original lease has expired but the
arrangement continued on a month-to-month
basis during the December 31, 1973, and
December 31, 1974, cost reporting periods.
S. The provider treated the radiologists
payments and the radiology department's
costs as non-patient income and non-patient
costs for the cost reporting periods at issue.
6. The provider did not treat the pay-
ments received from the radiologists as an
offset to allowable costs in its Medicare cost
reports for the cost reporting periods end-
ing December 31, 1973, and December 31,
1974.
7. For the fiscal year ending December
31, 1973, the physician paid the provider
$64,671. The provider's expenses for the
X-ray department amounted to $19,210.
8 For the fiscal year ending December
1974, the physician paid the provider $63,72S.
The provider's expenses for the X-ray
department amounted to $23,319.
Conclusions of Low
1. The reasonable costs of the provider
are to be determined in accordance with
N @ 210 9
the methods specified in the Regulations
(Section 1861(v)(1)(A) of the Social Secus
rity Act, as amended, [42 USCA 1395x])).
2. The radiology department leased to
the radiologist by the provider constituted
a hospital department within the meaning
of 20 CFR 405.486(a), (b)(1), and (b)(2).
J. The provider's payments for some of
the radiology department's costs are oper-
ating expenses of a hospital department
within the meaning of 20 CFR 405.486(b) (1).
4. The operating expenses of the radiol-
ogy department paid for by the provider
are reimbursable hospital costs under 20
CFR 405.486(b) (1).
S. The payments made by the radiologist
to the provider for the radiology depart-
ment must be used to reduce the provider's
allowable costs reimbursable through the
hospital insurance program under 20 CFR
405.486(b) (1).
6. Offset of the radiologist’s rental pay-
ments to the provider's allowable costs is
required to assure that Medicare pays only
actual costs of services to its beneficiaries
under 20 CFR 405.402(a).
Decision
The decision of the Provider Reimburse-
ment Review Board that the portion of the
revenue from the radiologist exceeding the
hospital's costs of the radiology department
may not be used to offset allowable costs
of other departments of the hospital is
reversed.
This Constitutes the Final Administrative
Decision of the Secretary of Health, Educa-
tion, and Welfare.
§ 28,505 MEDICAID—EPSDT AND DETECTION OF LEAD POISONING
Information Memorandum, IM-77-32 (MSA), June 9, 1977. Subject: “New Technology
Available in the Screening and Detection of Lead Poisoning and EPSDT.”
Medicaid —EPSDT and detection of lead poisoning.—New technology, in the form
of relatively inexpensive instruments called “hematoflurometers,” has enable providers at
their own sites or at centrally located laboratories to detect lead poisoning and iron defi-
dency anemia inexpensively within 10 seconds. This technology has introduced a primary
screening test that can result in cheaper and more comprehensive testing for these condi-
tions under Medicaid's EPSDT program, and in a related reduction in the long-term care
(also Medicaid-financed) that Jead poisoning often causes. Therefore, it is recommended that
EPSDT screening should ideally include lead testing at least once for screened children
one through five years old because excessive exposure to lead in this age group has largely
irreversible effects on the development of the cental nervous system. As a2 minimam, in the
screening of EPSDT eligibles on a county or city basis, at least 10 percent but not less
than 100 children in the age one through five screen group should be tested for lead as an
indicator of this problem within this group. If this testing yields less than three percent
positive, the lead test should probably not be performed on a periodic basis but should be
performed selectively. In counties with less than 100 eligible in this age group, all of
these children should be tested. Bock reference: 114,551.
1 28,505 © 1977, Commerce Clearing House, Inc.
[Text of Memorandum)
This information transmittal was jointly
developed by the Division of Early and
Periodic Screening, Diagnosis and Treat-
ment (EPSDT) and the Division of En-
vironmental Health Services of the Center
for Disease Control (CDC) to provide our
endorsement of available new technology
for the detection of lead poisoning among
the EPSDT population. . ..
The Problems
All children should be considered at risk
for lead exposure since all individuals re-
ceive varying degree of exposure to lead in
their daily life. The impact of excessive
lead exposure to children 1 through § years
of life can and does have serious and largely
irreversible effects on the development of
the central nervous system. It may vary
from severe brain damage to relatively mild
neurologic disability and hyperactivity at
lower levels of exposure. Undue lead
absorption may also result in toxic effects
on the kidneys as well as bone marrow with
associated impairment of blood cell informa-
tion. Childhood lead poisoning costs money
for long term institutional care and increases
public assistance expenditures,
Risk
Most of the children with undue lead
absorption do not have overt symptoms of
the disease. The problem can only be de-
tected by screening the child for the disease.
Children who live in, or frequently visit,
poorly maintained housing units constructed
prior to the 1960's, are at greatest risk of the
disease. Unfortunately, the majocity of the
children served by the EPSDT Program are
in this high nsk group.
New Technology
Screening for undue lead absorption has
been recommended in A Guide to Screening
for the Eorly ond Periodic Screening, Diag-
nosis, ond Treatment Program Under Meds-
cad. Since its publication, there have been
considerable advances in technology and
information relating to undue lead absorp-
tion. In the past, screening, using blood and
lead determinations, was recommended as
the primary detection tool. Recently, how-
ever, a series of instruments have been
developed to allow a program to perform
erythrocyte protoporpyrin (EP) determina-
tions at the provider site or in a centrally
located laboratory. This test not only pro-
vides an indicator of the metabolic effects
of undue lead absorption, but also can be
Medicare and Medicaid Guide
New Dew:
pane nts 9805
used in determining if a child is anemic due
to iron deficiency. These instruments, called
“hematoflurometers”™ are relatively inexpen-
sive, require only a few drops of blood, and
optically analyze the specimen in less than
10 seconds. The EP is not subject to con-
tamination as is the micro blood test. If the
EP is negative (less than —60 ug/dl whole
blood), the program can rule out iron de-
ficiency and undue lead absorption. If, how-
ever, the test results are above —-60 ug/dl,
then the child should be fully evaluated for
iron deficiency anemia ond undue lead
absorption. With these advantages and low
cost per specimen analyzed, the erythrocate
protoporphyrin test would appear to be more
desirable as a primary screening test and
will result in significant long term savings
to the EPSDT Program.
Recommendations
In light of the data we have reviewed
from EPSDT programs and the CDC data,
it is obvious that programs which look for
children with undue lead absorption, find
children requiring medical attention. In
order to determine how much of a problem
there is in the 1 through § years of age
group, each State program should plan to
include lead testing procedures in their
screening requirement so that each child
is tested at least once. The providers should
carefully review the yield from the testing
to determine if the lead test should continue
on a penodic basis as determined by the
percentage of children found to have lead
problems.
The Center for Disease Control, Environ-
mental Health Services Division, has re-
leased a statement entitled Increased Leod
Absorption and Lead Poisoning in Young
Children, March 1975, which describes the
current recommendation for screening and
pediatric care for children with a lead
problem. Note that children with a blood
level of —30ug/dl ond EP —60ug/dl are
considered to have undue lead absorption and
require medical care. The CDC statement
discusses the interpretation of test results
in detail and has served as a guide to many
of our providers in the management of
children with lead problems.
Screening Eligibles
When screening eligibles on a county or
city wide basis, at least 10 percent but not
less than 100 children of the EPSDT-eligible
children screened ages 1 through 5 should
be tested for undue lead absorption as an
indicator of magnitude of the lead problem
1 28,505
EXHIBIT 3
bl
eC "en
/
|
|
i A GUIDE TO ADMINISTRATION,
DIAGNOSIS, AND TREATMENT
for the
Early and Periodic Screening, Diagnosis,
and Treatment Program (EPSDT)
“under
MEDICAID
by
Gerald Hass, M.D.
Mr. Melvin Scovell
Prepared by the American Academy of Pediatrics under Contract HSM 110-73-524, Health Services and Mental Health Administra- tion, U.S. Department of Health, Education and Welfare
d
a
h
HR ee en PFE ed
0 »
INTRODUCTION
In 1965, Congress enacted Title XIX of the Social Security Act (Medicaid) to increase the availability of medical care to persons who cannot afford it. It is a State administered program under which the Federal Government reimburses costs incurred by the States in providing medical care to low income “individuals and families. The Federal Government pays from 50 to 78 percent of the costs incurred by the States, based on the per capita income of the State.
| Medicaid recipients include persons and families receiving or entitled to receive cash assistance payments under the Social Security Act. In addi- tion, States may elect to pay for medical care provided to medically needy persons and families (individuals whose income equals or exceeds the State's standards under the appropriate financial assistance plan but is insufficient to meet their medical costs). Each State determines the extent of services offered and the eligibility of recipients. As a minimum, to quali- fy for federal reimbursement under Medicaid, States must provide inpatient and outpatient hospital services, laboratory and x-ray services, skilled nursing home services, physicians’ services, home health care services, and family planning services.
The 1967 amendments to Title XIX created the Early and Periodic Screen- ing, Diagnosis, and Treatment (EPSDT) program. They added a requirement to Medicaid directing attention to the importance of preventive health sery- ices and early detection and treatment of disease in children eligible for medical assistance. The amendment requires State Medicaid programs to arrange for the screening of children under 21 years of age for physical and mental defects, and to provide the necessary health care to correct or ameliorate the defects. They further stipulated that treatment for visual, hearing, and dental defects must be provided.
EPSDT was to begin in 1971. Because of the complexities of initiating this program, interim regulations issued in December 1971 were superseded in June 1972 by Program Regulation Guide MSA PRG-21.1 These regulations requested States to initiate EPSDT programs by February 7, 1972, for children under 6 years of age, and for all eligible children under 21 years of age by July 1, 1973.
“Program Regulation Guide," MSA-PRG-21, Department of Health, Education and Welfare, Social and Rehabilitation Services, Washington, DC 20201, June 28, 1972.
1
oy,
~~, Ca £
Public Law 93-603 added a penalty provision effective July 1, 1974, requir-
ing the Department of Health, Education, and Welfare to withhold 1% of a
State's Title IV-A Aid for Dependent Children (AFDC) funds if a State (a)
fails to inform the adults in AFDC families of the availability of child health
screening services; (b) fails to actually provide or arrange for such serv-
ices; or (c) fails to arrange for or refer to appropriate corrective treatment
those children identified by such screening as suffering illness or impair-
ment.
Lodind Zo. phi
Richard W. Olmsted, M.D.
Associate Director
American Academy of Pediatrics
RS Es
oo
Explaining the problems of sickle cell disease and trait can be difficult.
Well trained counselors who may be nurses or community aides may allay
needless anxiety. Families with sickle cell problems frequently need sus-
tained support, particularly if a family member has sickle cell disease.
Problems of transportation to medical care, repeated hospitalization, inter-
rupted schooling, and depression need to be faced and solved. Families
need help to cope with the fact that a child with sickle cell disease has a
shortened life expectancy. A child with sickle cell disease needs careful
and continous follow-up by a physician and supportive personnel in addi-
tion to access to a referral center for management of complications of the
disease.
Counseling and Follow-up:
Resources:
Children of school age handicapped by sickle cell disease may qualify for
education services through the State Department of Special Education. In
many states, organizations such as the Sickle Cell Foundation24 are active
in educational and supportive services for families with sickle cell disease.
Increased Lead Absorption?
In the United States, 2.5 million children 1 through 5 years of age are at
risk of undue lead absorption. Approximately 600,000 will be affected by
the disease, generally as a result of living in oid, deteriorated housing con-
taining lead-based paint. Prevalence is lower in suburban areas and may
be extremely low in areas with houses built after the 1950's and with little
exposure to industrial sources of lead. Classical symptomatic lead poison-
ing is generally not seen. Approximately 6,000 will develop neurologic
damage including slow learning, hyperactivity, and behavioral disorders
even though the child is asymptomatic.
Diagnosis:
All children 1 through 5 years of age should receive an ertyhrocyte proto-
porphyrin test. If the results are 60 u g/dl or more, the child should receive
24Contact the National Association for Sickle Cell Disease, Inc., 945 South Western Avenue, Suite 206,
Los Angeles, California 90006. Telephone: 213-731-1166.
Sop. cit., "A Guide to Screening,” Chapter 21
64
{ L
Pn
a blood lead test. if the blood lead is less than 0, 8 the child should
receive a hematologic evaluation to determine if the child is iron deficient
or suffering from another porphyria. However, if the blood lead is 30 ug/dl
or more. the child should be considered to have undue lead absorption.
Both the ertythrocyte protoporphyrin and blood lead tests can be per-
formed readily on a finger prick sample. In view of the known difficulty in
carrying out blood lead level determinations, only experienced, proficient
laboratories should utilized.
Referral:
Children Identified with undue lead absorption should be referred to re-
sources especially equipped to evaluate and treat the condition. Physicians
accepting these referrals should have experience with the management of
undue lead absorption and must have access to reliable laboratory and
hospital facilities.
Management:
The physician to whom the child is referred will probably undertake the
following steps:
1. Clinical evaluation for symptoms and signs of lead intoxication
2 Additional laboratory studies for evidence of lead intoxication
3. X-ray studies for evidence of lead lines in the long bones and ra-
dio-opaque material in the gastrointestinal tract
4. Treatment, if indicated, by chelation using CaEDTA (calcium diso-
dium versenate) or BAL (2,3-dimercaptopropanol) under close medical
supervision in the hospital. The physician supervising the care of the
child may determine that a mild lead intoxication could be followed
on an outpatient basis
5. Notification of the appropriate community agency (e.g., public
health department, housing authority, etc.) to initiate environmental
lead hazard identification and reduction services to protect the child
from additional exposure
6. Testing of other family or household members for undue lead ab-
sorption
7. Arrangement for continued pediatric follow-up
65
Counseling: ®
3
Families with children who have undue lead absorption need counseling to help them understand the nature of the threat of lead poisoning to a
A child with undue lead absorption is at risk of future developmental and intellectual handicaps. Follow-up is important to monitor the response to
education, housing inspection and lead hazard reduction services, legal services, screening, referral centers and hospitals, and community or State
In communities without intensive lead poisoning prevention programs, it may be necessary to establish such a program. Close coordination is re-
I
—
—
—
—
—
—
W
—
—
—
—
—
—
—
"a
EXHIBIT T
8 13232
beneficiaries to retain sccesa to t serv-
jces. Note—The bill also requires States
which cover hosploe services to pay hospices
an sdditional amount equal to at lesst 85%
of the rate that would have been paid by
the State to the nursing facility for & hos-
pice beneficiary,
MEDICAID COVERAGE OF RURAL HEALTH CLINIC
SERVICES
Present Law.—States are required to cover
services by facilities designated by the Sec-
retary as rural health care clinics if the
services are otherwise covered under the
State Medicaid plan. The State must pay
100 percent of the reasonable costs of the
clinic in furnishing the services. For services
that would be coversad as rural health elinic
services If furnished to a Medicare benefici-
ary. the State must follow the methods used
by Medicare in determining reasonable cost.
For other services, the State's determina.
tions are bound by any regulations the Sec-
retary may promulgate relating to tests of
reasonableness.
Committee Provision.—The Committee
bill provides that, for Medicald purposes, a
facility Is to be treated as as rural health
clinfe if it has been determined by the Sec
retary to meet requirements under the
Public Health Service Act for funding as a
community or migrant health center or a
provider of health care to the homeless. Re-
quires States to pay, for rural health clinic
services furnished to Medicaid beneficiaries,
100 percent of the reasohable costs of such
services as determined by the fiscal iInterme-
diary for Medicafe beneficiaries.
Cost-based provisions of this statute,
when applied to provider-based rural health
clinics, should serve as an incentive to re-
structure and maintain health care services
In rural areas. The Committee believes that
for private physi-
Present Low.—a. Coverage ef Pregnant
Women, Infants, and Children to Age 6. The
Medicare Catastrophic Coverage Act of 1988
(MCCA) requires States to offer Medicaid
coverage to pregnant women and infants
under one year old with family incomes
below 75 percent of the Federal poverty line
by July 1, 1888, and to those with family in-
comes below 100 percent of the poverty line
by July 1, 1980. The Omnibus Budget Rec-
oncilistion Act of 1887 (OBRA 87) permits
States to establish a higher income standard
for pregnant women and infants up to 188
percent of the poverty line, and also permits
States to cover children under age 2. 8, 4, §,
8, 1, or 8 (as selected by the State) who were
born after September 39, 1883, and whose
family income is below & State-established
income level which may be as high as 100
percent of the Pederal poverty level.
b. Coverage of Children to Age 19. States
must provide Medicaid for children recelv-
fing Aid to Families with Dependent Chil-
dren (AFDC) and may provide Medicaid to
children whose family income is within
APDC standards but who do not meet non-
financial criteria for AFDC.
¢e. Continuous Eligibility for Pregnant
Women, Infants, and Children. (i) Begin-
ning July 1, 1889, States have the option of
continuing coverage for a pregnant woman
through the end of the second full month
beginning after the end of the pregnancy,
even if the woman would otherwise become
ineligible during that period; the infant
born to the woman remains eligible for the
same period. (ii) Periodic redetermination of
eligibility for Medicald beneficiaries who are
not recefving cash assistance occurs at inter-
2 CONGRESSIONAL RECORD — SEZ "TE
vals determined by the State. (iff) An |
vidual who ceases to qualify for Medicaid
benefits on one basis may still qualify on
some other basis. For example, 8 family
that is no longer financially eligible for
AFDC (and hence for automatic Medicaid
benefits) might still be eligible for Medicaid
under a higher income standard used for
the “medically needy.” Under current law,
States are not required, when terminating
Medicaid eligibility in such a case, to deter-
mine whether the beneficiary might qualify
for benefits on some other basis. Instead,
the individual may be required to re-apply
for Medicaid benefits.
d. Coverage of Children Receiving 881
Benefits. States are ordinarily required to
provide Medicaid to any aged, blind, or dis
abled person receiving cash assistance under
the Supplemental Security Income (8S1)
program. However, section 208(b) of the
Social Security Amendments of 1972 (P.L.
92-603) provided that a State could use
more restrictive eligibility standards for
Medicaid than those used for 8SI if the
State was using those standards for Medic-
ald on January 1, 1972. As of 1989, there are
14 “Bection 209(b)” States, using criteria for
Medicaid for the sged, blind, and disabled
more restrictive than those used for 881
e. Mode! Application. States design thelr
own application forms for Medicaid bene-
fits.
f. Hospital Payment Protections. States
may establish durational limits on coverage
of Inpatient hospital services, but may not
impose these limits on medically necessary
services provided to children under 1 year
old In hospitals serving a disproportionate
number of low-income patients with special
needs. If the State pays for inpatient serv-
ices on a prospective basis (under which
payment rates are established in sdvance
and may not reflect the hospital's sctual
eosts for covered services), the State must
provide additional payment to dispropor-
tionate share hospitals for patients under 1
year old who are “outliers,” that is, who
incur exceptionally high costs or have long
hospital stays.
g. Codification of Adequate Payment.
States establish their own payment levels
for Medicaid services. Medicaid regulations
(42 CFR 447.204) provide that payments
must be sufficient to enlist enough provid-
ers 80 that covered services will be available
to Medicaid beneficiaries to st least the
extent that such services are available to
the general population.
h. Required Coverage of Nurse Practition-
er Services. States are permitted, but not re-
quired, to include as a Medicaid benefit
services of nurse practitioners within the
scope of their licenses under State law.
L Home and Community-Based Services.
Section 2178 of OBRA 81 permitted States
to obtain waivers of certain Medicaid re-
quirements in order to establish a home and
community-based service program for a de-
fined population (such as the aged or the
mentally retarded) of persons who would
otherwise require long-term institutional
care. Waiver programs must be approved
and periodically re-approved by the Secre-
tary and must meet certain requirements,
including tests of cost-effectiveness. So-
called “model” walvers are a separate cate-
gory of section 2178 waivers that allow
States to provide support services for dis-
abled children Hving at home who would re-
quire institutionalization without those
services and would, If institutionalized, be
eligible for Medicaid. Originally, the
number of children who could be served
under a model waiver was limited to 50.
OBRA 817, 88 modified by MCCA, prohibited
the Secretary from limiting coverage under
October 12, 1989
any section 2176 waiver Lo fewer than 200
persons.
J. Home Visitation Services. No provision
k. Farly and Periodic 8creening, Diagno-
sis, and Treatment (EPSDT). States are re-
quired to cover early and periodic screening.
dizgnostic, and treatment (EPSDT) services
for most groups of Medicaid beneficiaries
under age 21. Medicaid regulations provide
that EPSDT acreenings must inclode a
health and developmental history, 8 com-
prehensive physical, vision and hearing lest
ing, appropriate laboratory tests, and dental
screening for children over 3.years oid (or
over 5 years old, with the Secretary's ap-
proval). The regulations require that States
establish, tn consultation with medical and
dental organizations, a “periodicity sched-
ule” for acreenings, specifying services sp-
plicable at each stage of the beneficiary's
life. States must also provide treatment for
problems or conditions identified during
screening. The regulations provide thst, in
addition to any treatment services normally
covered under the State Medicaid plan, the
and vision and hearing
Jreasment, including eyeglasses and hearing
L Foster Children. Title IV-E of the Social
Security Act requires, ss a8 condifion of
foster care assistance grants to States, that
8 case plan be developed for each Federally-
assisted child placed in 8 home or instite-
tion, Including piuans for assuring proper
care and services.
m. Medicaid Coordination with WIC Pro-
gram. The Special Supplemental Food Pro-
gram for Women, Infants, and Children
(WIC) provides supplemental food and re
lated services to certain low-income mothers
and young children Although many persons
qualifying for WIC are 2ls0 eligible for Med-
icald, there fs currently no formal coordina
tion between the two programs.
n. Improving Public Health Coordination.
No provision. :
0. Use of Most Recent Data In Computing
Pederal Medicald Assistance Percentage.
The Federal matching percentages used for
Medicaid, AFDC, and other programs are
promulgated by the Becretary in October or
November of each year and take effect on
October 1 of the following year. The pér-
centage calculations are based on State per
capita income data, using the most recent
svailable dats.
p. Outreach as an Optional Service. States
may conduct outreach activities, but would
receive Federal funding st the 50 percent
administration matching rate. 2
qQ. Provider Reimbursement Demonstra-
tion. No provision.
r. Maternal and Child Health Bandbook.
No provision.
8. Annual Report by Secretary. No proxi-
sion.
t. Requirements of the Secretary. No pro-
vision.
u. Maternal and Child Health Services
Block Grant. The Maternal and Child
Health (MCH) Block Grant program, su-
thorized by Title V of the Social Security
Act, provides grants to States for a variety
of health programs, including direct provi-
sion of preventive and primary care services
to mothers and children, health screenings,
immunizations, and rehabilitation servicey .
for children with special health care rieeds
{formerly referred to as crippled children).
The permanent authorization for the MCH
block grant program is $561 million per
year; the appropriation for FY89 is $554
million. Of this amount, approximately 84%
is allocated to States; the rest is retained by
DHHS to support “special projects of re-
gionai and national significance” and to con-
duct research, training, and genetic 4d
screening programa
v. Buy-in Demonstration. No provision
w. Medicaid Caoversge of Community
Health Clinic Services. States are permitted,
but not required, to cover services in com-
munity and migrant health centers and pro-
viders of health care to the homeless receiy-
ing Federal grants under the Public Health
Services Act. States that cover such services
established their own reimbursement meth-
odologies.
X. MEDICAID TRANSITION FOR CERTAIN AFDC
FAMILIES
Present Law.—Section 406(h) of the Social
Security Act provides that families who
become ineligible for AFDC because of the
collection of child or spousal support pay-
ments are eligible for Medicaid for the four
month period beginning with the first
month of ineligibility. This provision ex-
pires on October 1, 1989 (Section 2((b) of
P.L. 88-3178).
Committee Provision.—a. Coverage of
Pregnant Women, Infants, and Children to
Age 6. The Committee bill requires States to
cover pregnant women and children under
age 6 with family incomes below 133 percent
“of the Federal poverty line, effective April.
+ 1, 1990.
‘b. Coverage of Children to Age 19. The
Committee bill permits States, effective
April 1, 1990, to extend Medicaid coverage
to children who are age 8 or over, but under
age 19, and whose family incomes do not
exceed a State-established level which may
be as high as 100 percent of the Federal
poverty line. .
¢. Continuous Eligibility for Pregnant
Women, Infants, and Children. The Com-
mittee bill requires all States, effective Jan-
vary 1, 1998, to continue eligiblity for preg-
nant women until the end of the second
month beginning after the end of the preg-
nancy. For children under 3 years old who
are not receiving cash assistance, States are
prohibited from conducting redetermina-
tions of eligibility more often than every 8°
months, regardless of any change in the
family’s circumstances. Effective on enact-
ment, States are prohibited from terminat-
ing the Medicaid eligibility of children
under 38 who lose AFDC or SSI benefits
until it is determined that they do not qual-
ify for Medicaid under any other category.
d. Coverage of Children Receiving 8SI
Benefits. The Committee bill requires all
States, effective January 1, 1890, to provide
Medicaid to persons under 18 who are re-
ceiving SSI benefits.
e. Model Application. The Committee bill
requires the Secretary to develop and make
available to States, by January 1, 1991, a
model uniform Medicaid application form
for applicants who are not receiving AFDC
and are not Institutionalized. Use of the
form by States will be optional.
f. Hospital Payment Protections. The
Committee bill requires States, effective
January 1, 1990, to waive durational limits
and provide outlier payments for medically
necessary inpatient services provided by dis-
proportionate share hospitals or children’s
hospitals to children under age 8, and for in-
patient services provided by any hospital for
children under age 1. The imposition of
dollar limits on Inpatient services for benefi-
claries under age 1 is prohibited. In the case
of services furnished to a child under 19 by
an out-of -State hospital, the State is re-
quired to pay at the rates paid by the State
in which the hospital is located, unless the
two States have agreed otherwise.
The Committee Is interested in alternative
methods for providing payment protections
for hospitals providing outpatient services
to infants and to young children, particular-
October 18, 1989 | i a RECORD — SEN/_E
ly in disproportionate share hospitals and
childrens’ hospitals, similar to those provid-
ed for Inpatient services in this bill
g. Codification of Adequate Payment. The
Committee bill incorporates the current reg-
ulatory requirements for provider remburse-
ment into the statute. The Secretary Is re-
quired to report to Congress, not later than
January 1, 1890, on the adequacy and timeli-
ness of States’ Medicaid payment for obstet-
rical and pediatric services, and on factors
that may delay payment to providers of
such services.
h. Required Coverage of Nurse Practition-
er Services. The Committee bill requires
States to cover under Medicaid services of
certified pediatric or family nurse practi-
tioners practicing within the scope provided
under State law, regardless of whether they
are under the supervision of or associated
with a physician or other provider.
{. Homé¢ and Community-Based 8ervices.
The Committee bill allows States to cover,
without a waiver, home and community-
based services for children who are under
age 18 and who have acquired immune defi-
ciency syndrome or are medically dependent
on a ventilator for life support, effective
January 1, 1990. With respect to section
2176 walvers granted or renewed on or after
January 1, 1900, the Secretary is prohibited
from limiting participants to fewer than
350.
It is the Committee's understanding that
addicted children living in foster care homes
or group homes are eligible for home and
community based services and home visiting
services as provided in this bill. :
j. Home Visitation Services. The Commit-
tee bill permits States to cover as a Medic-
aid service home visitation to medically
fragile pregnant women and tc infants in
the first 12 months of life who have medical
conditions that require life-sustaining medi-
cations or equipment or technologically as-
sisted feeding, effective January 1, 1990.
The Committee notes that, under current
Medicaid law, States can finance home visi-
tation services by lay visitors. States are au-
thorized to furnish “case management”
services to all or some groups of Medicaid
beneficiaries, on a Statewide or sub-State
basis. Under the expansions in eligibility in-
cluded under this bill, States will be able to
furnish case management services to a
larger group of women and children. Lay
visitors services are designed to promote
access to health care and appropriate use of
NECESSAry care,
k. Early and Periodic Screening Diagnosis
and Treatment. The Early and Periodic
Screening, Diagnosis and Treatment
(EPSDT) program was added to the Medic-
aid statute in 1967. Under EPSDT, all Med-
fcaid-eligible individuals under age 21 are
entitled to comprehensive preventive and
primary medical, dental, vision and hearing
screening, diagnostic, and treatment services
as well as immunizations, vision, hearing
and dental care even if not otherwise includ-
ed in a State's Medicaid plan. If the condi-
tions are discovered in a screen. Since its in-
ception, EPSDT, the nation's largest pre-
ventive health programs for low income
children, has provided comprehensive pre-
ventive health care for millions of children.
Children who participate in EPSDT have
been found to have annual health care costs
nearly 10 percent lower than children who
do not receive such services.
The EPSDT benefit package has never
been described in detail in the statute.
There have arisen questions regarding the
content of the program, as well as which
providers are qualified to furnish the
EPSDT screening and treatment. Addition-
ally, while states have always had the
option to do so, many still do not provide to
8S 13233
‘dren participating In EPSDT all care
and services allowable under federal law,
even if not otherwise included In the state's
plan.
The EPSDT has grown in importance as
millions of additional infants and children
have become eligible for Medicaid and as
other, complementary for children (such as
the 1988 early intervention amendments to
the Education for All Handicapped Chil
dren's Act) have been enacted. In order to
strengthen and clarify the scope of EPSDT
and its relationship to other programs for
children with special health care needs and
to encourage additional providers to partici-
pate in the program, the Committee bill
thus contains a series of amendments to the
Act.
General screening services. —the bill clari-
fies that the screening services required
under EPSDT include health examinations
provided at specified intervals described on
a State's periodicity schedule, which must
meet certain requirements. The bill also
clarifies that separate vision, hearing, and .
dental schedules that meet accepted stand-
ards of practice and are determined in con-.
sultation with appropriate professional or-
ganizations must also be established.
The Committee amendment also requires
states to cover screening services furnished
at intervals other than those formally identd-
fled on the State's physical, dental, vision
and hearing periodicity schedules when
there is reason to believe that a child suf-
fers from a physical or mental {llness or
condition that requires further assessment,
diagnosis and treatment. These interperi-
odic examinations may be triggered even In
the case of children who already have had a
physical, mental or developmental problem
diagnosed, if there is reason to suspect that
the {llness or condition has grown more
severe or has altered sufficiently so that
further examination is warranted.
No prior authorization may be required
for interperiodic screening and diagnostic
activities, just as none may be required for a
periodic exam and diagnosis. However, prior
suthorization may be required for treat-
ment services.
The Committee underscores that the de-
termination of medical necessity for these
“interperiodic” screens can be made by pro-
fessionals who come into contact with a
child through various channels. It is impera-
tive that a child's treatment not be delayed
until he or she is due for a periodic screen
So long as a referral (including a self refer-
ral in the case of health related providers
that are also EPSDT providers) is made to
an EPSDT provider, the child is entitled to
“interperiodic” health, dental, vision or
hearing assessment or treatment services
covered under the State plan.
Anticipatory guidance.—The Committee
bill clarifies that anticipatory guidance pro-
vided to the child or the child's parent or
guardian is a formal part of any good
EPSDT assessment. This guidance includes
health education and counseling to both
parents and children.
Vision, dental and hearing services. —The
Committee bill clarifies that, while part of
EPSDT, these services are independent of
the physical and developmental components
of the program in the sense that a physical
and developmental examination and refer-
ral are not mandatory prerequisites $0” ™-
vision, dental and hearing care. Moreover,
each of these services is to be governed by
its own professionally appropriate periodici-
ty schedule and is subject to its own Inter-
periodic screening rules. As with physical
assessments, no prior authorization is
needed for either a periodic vision, dental cr
hearing exam or an interperiodic exam. Re-
ME
AT
S
CER
a
Tee
Th
s
AN
e
n
,
yap
;
;
hy
E
y
A
g
p
-
'
a
pe
E
S 13234
fertrls (including self referrsls) can be made
{f an inlerperiodic assessment ls determined
to be medically DeCcessary.
covered Medicald service generally.
The Committee amendment would require
that states provide to children all treatment
{tems and services that are allowed under
federal law and that sre determined fo be
he il
H
i
l
lh fii
istrative expense.
The Committee amendment 8lso requires
the Secretary to report no later than by
July 1 of each year on the number of chil-
dren receiving EPSDT services by age and
by besis of eligibility for medical assistance.
L Fosier Childrern.— The Committee bill re-
quires, effective January 1, 1880, that case
plans for foster children include a health
care record that is provided to the foster
care provider before the child is placed (or
within 30 days after emergency placement).
The foster care provider must be notified of
the availability of EPSDT services. The
State must develop a health care plan for
the child, must ensure that the foster care
provider and easeworker understand their
-
0 rcnrovonn RECORD — sere
responsibilities with respect to the child's
health needs, and must periodically review
the plan to ensure that ii Is being adhered
to.
wm. Medicaid Coordination with WIC Pro-
gram.—The Committee bill Requires State
Medicaid plans to provide for coordination
between the Medicsid and WIC programs,
women,
availability of WIC benefits and to refer
such persons to the State agency adminis-
proved or denied within 90 days,
tary is required to report to Congress on the
results of the projects by March 1, 1992. Ap-
and other organizations, with the handbook
to be ready for field testing by July 1, 1890,
Field testing and evaluation is to be com-
pleted by June 1, 1991, after which the
handbook is to be distributed nationally to
all pregnant women and new families with
young children. The Secretary is to coordi-
nate distribution through public and private
agencies. Appropriations of $1 million are
authorzied for each year, FY 1891 through
FY 1893. 7
8. Annual Report by Secretary.— The Com-
mittee bill requires the Secretary to publish
annually, beginning January 1, 1891, s
report on the health status of children, in-
om
£
October 1%, 1989
cluding information from snnual State re-
ports (see item u, below) and statistics relat-
ing to child health and health services
The Committee is increasingly concernad
about the impact of the growing problem of
substance abuse during pregnancy. Recent
indications are that maternal and infant
mortality and morbidity may be rising as a
result of increased substance abuse during
pregnancy. A recent study by the House
Select Committee on Children, Youth and
Families found that hospitals are reporting
velop definitions of medically risk
children at high risk of medical
problems, and chil-
sultation with health care groups and
health insurers. The Secretary is also to de-
velop a model health benefit package for
pregnant women and children, including st
least primary care and catastrophic inps-
tient coverage. Reports on the definitions
and the benefit package are to be provided
to Congress by March 1, 1990.
x Maternal and Child Health Services
Block Grant —The Committee bill increases
the permanent authorization to $711 million
for FY 1990 and later years. The Federal
set-aside for special projects is fixed at 15
percent. In addition to other research, train-
ing, and special programs, the set-aside is to
be used to fund 3-year demonstrations of
ways to extend basic health insurance to
children not covered by other public or pri
vate programs. Demonstration programs
could be school-based plans or plans operat,
ed by hospitals or other non-profit entities.
They would have s& declining level of Feder-
al funding over the 3-year period, could
charge premiums to enrollees, but would be
prohibited from excluding applicants for
medical reasons or Imposing pre-existing
conditions or waiting periods.
The Committee intends that enrollees in
these demonstrations are treated no diffes-
ently than individuals enrolled in other in-
surance plans. Thus, it is recommended that
hy
i * Phr SY |
6» ’
'
+
Qvtobe 13, 1583
children. 3 the program de provided dent|-
firnttore Und I similar 1 nyture to that
used by other members of the organizations
apeesting the program.
The Cstourittee BilK requires States, Begin-
ning Jagusry I, 1900; ts ase at least 30 per
cant of thelr sllotmenty for services to ehil-
drea witht specikb hesth cure meeds and at
lest 8 percent for primary heslth services
projects for ohdldrem, the devslopment of
" service wet works ond case mmnegement pro-
grams for children with special heuith care
needs, and screening for sirdlecell anemia
and gther genetic diseases, A State's contri-
batiox te mmterrosd and child health pro-
gran must be at. least equal to the amount
provided bp the Stats in 196% For PY 1990
though. FY 1962 States are required to de-
velop a system of family centered communmni-
care for childrerr with special
hegith eare needs, guordinsting with Medic
ald snd othiey programs and providing a toll-
free hotline. on svailable medical and sup>
port services. The: Soeretary § required to
assist in developing these systems snd to
§oIapne national directory ef the States’
II-free numbers. Annual reports required
“from States are expanded to Include data on
© the extent to wiiich the State las met indi-
viduals’ needs; the nature of services provid-
ed. hesith statux outcomes, snd the
amounts of fundy devoted to the care net-
works foi chiltfterr with spefesd health carr
needs. Reports must aso Include & maternal
and child care needs assessment, including
plang for meeting identiffed needs sd a de-
scriptionr of Pow grant funds will be used’
under the pla In developing the omusl
meeds sssexsment and the community-based
care network, the Stxte ix required to work
fn: consuitatfor with x maternal and child
heaith advisory Doxrd. The board’ must also
£ review sod coomwments ory the
State's program of “one-stop shopping,™ mr
tegrated maternal and’ chfid hexdth service
delivery system coordinsting Medicaid,
MCE programs, and otter services.
It is the Committee's intent that the
new
mittee encourages Staies te eontinue plac.
ing a priorily on preventive and primary.
care beth for women and infants, and. fer
children and adoTeseenis. The Commities
notes that Slate allocatipns under the block
grant are intended to achieve the purpeses.
of Tille V of {he Social security Act, and
that resources for State agency overhead
should be efficiently allocated.
The sole of the Maternal & Child Health
Advisory Board created by the bill could be
stengthened {I other key agencies engaged
fn providing serwWces to children with special:
health care needs are also included, such as
the state lead agency administering early
intervention programs, the State mental re-
tardation/developmental disability agency,
and other groups.
The Committee notes that many States
have involved parent groups in developing
consolidated information systems for chron-
fcally inl children, and encourages similar in-
volvement as Slates undertake to imple-
ment similar requirements under this bill
The Committee has also included authar-
fty for a demonstration of home visiting
programs to high risk pregnant women and
infants, and hopes that sdequate funding
can be made available for this important ini-
tiative. The Committee also encourages the
Bureau of Materrml and Child Health to
fund diverse prajests: including those im
sparsely populated and hard to reach areas,
Applicants for funding in. these areas may
Biorsonat RECORD — sna @
require technical assistance to develop pro-
v. Buyin Demonstrations. —The Commit-
tee bill reqnimes the Segretary to enter into
egreements with several States to conduct
demonstrations. of alternatives for extend
ing Medicaid coverage, or altermative caver-
age, to pregnant women and children under
20 who are otherwise ineligible for nredicaia
and whose family incomes are below 185
percent of the Federal poverty level. Alter-
native coverage may include such options as
enrollment under employer plans, the
State's plan for its own empioyaes, a State
uninsured plan, or an HMO: If a project in-
cludes enrollment under employer plans, it
must require an emplayer contributian.
Projects must provide for premiums to be
charged to families above 100 percent of the
poverty level. The premium may be based
on a sliding scale or may be set at 3 percent
of family income. Demonstrations are ta
Begin by July P, 1990, and continue for
three years; unless the Secretary finds the
State noncompiant withr program require-
mentx Total Pederal Medicaid participation
fn the projects Is limited to $10 million in
FY90, $45 ndifion fn FYST, £55 million. in
FY32 and $10 millton in FY93. The Secre-
tary is required to submit sar interim evalua-
tion of the projects to Congress by January
P, 1992, ard x final report by January 1,
The Committee bill requires the Secretary
to enter into agreements with two States to
conduet demonstrations of alternatives for
extending Medicaid’ coverage, ar alternative
coverage, to individuals (including individ.
vals who are mediczily uninsurable or have
exhausted health insurance benefits) who
are inefigibie for Medicaid and whose family
[reomres are below 130 percent of the Feder-
af poverty’ evel. The Secretary may also
Impose am asset test, taking into account
those used ir other Feders! programs. Alter-
native coverage may include such options ss
enrollment under employer phans, Ne.
State's plan for its own employees, a State
uninsured plan, or ar EMO. If a project in-
cludes enrollment urrdder employer plans, ft.
must require amr emsployer contribution ard,
if the employer plan does not furnish alFf
RMedicafd benefits, the State must muke
those benefits avaflable to enrollees
Projects must provide for premiums to be
charged to families above 100 percent of the
poverty level, and tHe Secretary may also
require tRut plans on a sliding scale or may
be set at ¥ percent of family inconre. Dem:
omnstrations are to begin by July I, 1990, and
continue for three years, unless the Secre-
tary finds the State noncompliant with pro-
gram requirements. The Secretary 3 au-
thorized to waive the requirement that
State Medicaid plans operste: uniformly
throughout the State. Total Federal Medic-
afd participation in the projects is limited to.
$5 millon In each of FY%0 through FY92
The fs required to submit an th-
terinr evaluation of the prujects to Congress
by January 1, 1892, and a final report By
January 1, 199%.
w. Medicaid Coverage of Communily
Health Clinic Services.—The Committee bill
requires States to cover ambulatory services
and (Io sreas wilh a shortage of home
health providers) home health services pro-
vided by community health clinics. Commu-
nity health clinics Include Federally-funded
comnmunity and migrant health centers and
providers of health care to the homeless, as
well as providers that are not receiving Fed-
eral grant funds but meet the requirements
for community or migrant health center
funding. Payment for community health
clinic services must be equal to 100 percent
of the: facilities’ peasarmble costs for provid-
ing the services.
S 13235
z Medicaid Transition for Certain AFDC
Families —
Committee FProvtsiom.—The Cbmmillee
bill makes permanent the four month ex-
tension of Medicaid benefits.
Effective Dute.—Enactment.
INSTITUTIONS POR MENTAL DISEASE
Present Law.—Under current Medicahtd
Iaw, amounts expended by a State for the
eare of individuals between. the ages of 22
and 65 who are patients of an institution for
mental diseases (IMIX) ape not eligible for
Pederal matching funds. This exclusiom,.
which has been. effective since the begin
ming of the Medicaid program, was based
upon the judgment that it is the responsibil-
ity of the States to provide long-ternr care
for individuals residing in mental institu-
tons.
Federal firmancial assistance is available
far opatient psychiatric care furnished tv
general haspitais,.
The law defines my IND as a. hospital,
nursing facility, or ether institution of more:
thars 1& beds that is primarily engaged tm
the diagnosis, treatment, or cape of individ
uals with mental disease.
Current regulations provide that & deter-
minstiom as to whether an institution is am
EMD will be based uporr its “overad]l charac
ter.” One of the tests. for IMID status fis
whether more than 30 percent of an: institu.
tion’s patients have & mental disease requir-
ing inpatient treatment.
For a single facility that is under conmmen
administration: and contains a number of
separately licensed units serving Individoahe
with different needs, inclusion or exclusion
of patients in these affiliated units will obwyi-
ously affect whether the facilily exceeds
the 50 percent limit.
Commiilee Provision.—The Committee
bill: requires the Secretary of Human Serv-
fees (Segretary) to study and report to the
Congress by not later than October 1, 1988
on the appropriateness of continuing the
BID exelusion in light of changes in the de-
livery of mental health serviees since thre ex:
clusion was enacted.
The bill provides that any determination
by the Secretary (on or after June I, 1988)
that a facility is an TMB will not take effect
until October 1, 199%, if the facility meets
certain requirements: The requirements are
that: (1) as of June tL, 1989, the facility was
certified to provide both inpatient hospital
servicer and’ nursing facility services under
Medicaid and had more beds certified for
the provision of nursing facility services
than for inpatient hospital services, (2) the
gverage length of stay, in those units of the
facility primarily providing care for individ:
uals with mental disease, was 25 days or less.
far the facility's most recent fiscal year
ending before June 1, 1989, and (3) the facil-
ity was not formally and finally determined
to be ann IMD before June 1, 1888.
Effective Date.—Enactment.
NURSING HOME REFORM. DELAY IN EFFECTIVE
DATE OP FEBRUARY 2, 1988 FINAL REGULATION
Current Law.—On October 16, 1987, the
Secretary of Health and Human Services
(Secretary) published a notice of proposed
rulemaking (NPRM) specifying revisions in:
the requirements for nursing homes partici-
pating in Medicare and Medicaid ¢(52 Fed.
Reg. 38582), There was a period for public
comment on the NPRM.
OBRA 87, which became law on December
22, 1987, revised the requirements for these
facilities substantially. While some provi-
sions of the NPRM were similar to those of
the new law, the proposed rule did not re-
flect 8 number of changes made by the stat-
ute.
B
i
i
Pt i
g
ig
EXHIBIT U
B
T
T
S
D
U
D
V
I
C
E
vo
A
E
R
ro
ti
nii
oti
ndl
S
S
S
I
Ld
%. MEDICARE and MEDICAID
Part m NUMBER 603 DECEMBER 15, 1989
—EXTRAEDITION— >
Printed in U.S. A. All rights reserved.
Omnibus
Budget Reconciliation Act
of 1989
H.R. 3299
As Cleared by Congress
for the President
Explanation of the Conference Committee
Affecting Medicare-Medicaid Programs
CCH Special 3
COMMERCE. CLEARING. HOUSE, INC.. Rit a A SELF EUR NREE Ret vey beet trety MARTA JETT SAURTRRRR RS WALLA
Setting the standard since 1913 :
4025 West Peterson Avenue Chicago, linois 60646
Ln
‘=
NN,
Ngo *
ntinue
‘nefits
if the
1g the
ths of
ay re-
econd
‘nroll-
cover-
amily
ation
meet
re re-
AFDC
use
(C) EARLY AND PERIODIC SCREENING, DIAGNOSTIC, AND TREATMENT
Present law
States are required to cover ea nostic, and treatment
Physical exam, vision and hearing testing, ap-
propriate laboratory tests, and dental screening for children over 3
years old (or over 5 Jean old, with the Secretary's approval). The at States establish, in consultation with med. ental organizations, a * att schedule” fyi i e at each s
ate immunizations, and vision eyeglasses and hearing aids.
House bill (section 4213)
furnish only a Part of the EPSDT package from
participating in the program. uires States to report annually to
the Secretary, by April 1 after the end of each fiscal year i ning with ), on the number of children receivi DT
Screens, the number referred for follow-up treatment, and the
number receiving dental services, by age and basis of Medicaid elj-
gibility. Effective on enactment.
Senate amendment
No provision.
Conference agreement
agreement follows the House bil] ing modifications: (1) States are required to provide any service that a State is allowed to cover with Federal matching funds under Medicaid that is i required to treat a condition identified during a screen, whether or not the service is included in the State's Medic. aid plan; (2) the Sec i to develop, and every 12 Ronths thereafter, EPSDT participation goals for required to include data on the extent to
Be a —— in| Sonn wa + vm le ll =
454
which they comply with these goals in their annual reports to the
Secretary; and (3) the provision is effective April 1, 1990.
(D) EXTENSION OF PAYMENT PROVISIONS FOR MEDICALLY NECESSARY
SERVICES TO CHILDREN IN DISPROPORTIONATE SHARE HOSPITALS
Present law
(1) States may establish reasonable durational limits on coverage
of inpatient hospital services, but may not impose these limits on
medically necessary services provided to children under 1 year old
in hospitals serving a disproportionate number of low-income pa-
tients with fpecial n
(2) If the State pays for inpatient services on a prospective basis
(under which payment rates are established in advance and may
not reflect the hospital's actual costs for covered services), the
State must provide additional payment to disproportionate share
hospitals for patients under 1 year old who are “outliers,” that is,
who incur exceptionally high costs or have long hospital stays.
House bill (section 4214)
(1) Requires States to waive durational limits for medically neces-
sary inpatient services provided by disproportionate share hospitals
to children under age 18. Applies to payments for calendar quar-
ters beginning on or after July 1, 1990.
(2) Requires States with prospective payment systems to submit
to the Secretary, by April 1, 1990, a State plan amendment provid-
ing for payment adjustments for services provided by disproportion-
ate share hospitals after July 1, 1990, to children over age 1 but
under age 18 who are outlier cases.
Senate amendment
No provision.
Conference agreement
The conference agreement does not include the House bill.
(BE) REQUIRING ‘‘SECTION 209 (B)"’ STATES TO PROVIDE MEDICAL
ASSISTANCE TO DISABLED CHILDREN RECEIVING 8SI BENEFITS
Present law
States are ordinarily required to provide Medicaid to any aged,
blind, or disabled person receiving cash assistance under the Su
plementary Security Income (SSI) program. However, section 209(b)
of the Social Security Amendments of 1972 (P.L. 92-603) provided
that a State could use more restrictive eligiblity standards for Med-
icaid than those used for SSI if the State was using those standards
for Medicaid on January 1, 1972.
House bill (section 4215)
Requires all States to provide Medicaid to persons under 18 who
are receiving SSI benefits. Effective July 1, 1990.
Senate amendment
No provision.
EXHIBIT V
“u, a Health Care
¢ DEPARTMENT OF nef & HUMAN SERVICES » Financing Administration
Refer to. Region IX
MCD-P-EMR 75 Hawthorne Street
San Francisco, CA 94105
APR 11 1991
Mr. Michael Quinn, Research Manager
Child Health and Disability Prevention Branch (cD)
Data Management and Evaluation Unit
714 P Street, Room 708
Sacramento, California 95814
Dear Mr. Quinn: .
This is to confirm your discussion with Edna Ray regarding the
clarification of HCFA's guidelines on blood lead level testing
under the Early and Periodic Screening, Diagnosis, and Treatment
(EPSDT) Program relative to Section 6403 of the Omnibus Budget
Reconciliation Act of 1989 (OBRA '89).
The Federal statute at Section 1305 (r)(B)(iv) of the Social
Security Act mandates the provision of "laboratory tests (including
lead blood level assessment appropriate for age and risk factors)."
To assist States in implementing this and other provisions of OBRA
*'89, HCFA issued State Medicaid Manual (Part 5), Transmittal No.
3, dated April 1990. The guidelines in Section 5123.2 (D) (1) of
this issuance provided:
o Lead Toxicity Screening - where age and risk factors indicate
it is medically appropriate to perform a blood level
assessment, a blood level assessment is mandatory.
0 In July 1990, HCFA issued State Medicaid Manual (Part 5),
Transmittal No.4 and Section 5123.2.D.1 was clarified to
define lead poisoning ang recommended testing. It reads as
follows:
"Lead Toxicity Screening =- screen all Medicaid eligible
children ages 1-5 for lead poisoning. Lead poisoning is
defined as an elevated venous blood level (i.e., greater than
or equal to 25 micrograms per deciliter (ug/dl) with an
elevated erythrocyte protoporphyrin (EP) level (greater than
or equal to 35 ug/dl of whole blood). In general, use the EP
test as the primary screening test. Perform venous blood lead
measurements on children with elevated EP levels."
As we understand it, the State's instructions to providers of EPSDT services require that all Medi-Cal eligible children ages 'i-
5 are to be screened for elevated blood lead levels through the performance of an "FEP" test. Additionally, assessments for lead polsoning are required as a part of health examinations for children not in the 1-5 age group. Guidelines and/or Criteria for these assessments have also been issued to the EPSDT providers.
On the basis of this discussion, it appears that the State is in compliance with the minimum Federal requirements with respect to blood lead level screening. We will verify California's adherence to its stated policies and procedures in a forthcoming on-site review of the EPSDT Program. :
We hope that this information is responsive to your needs. Any questions may be directed to Edna Ray at (415) 744-3580.
Sincerely,
(ts or fon Chief
Medicaid Operations Branch
John Rodriquez, Deputy Director
Medical Care Services, DHS
Gordon H. Cumming, Ph.D., Chief «~
Ruth Range, Chief, Regional Operations ,CHDP
EXHIBIT W
oe on REC'D MAY 15 19%
DANIEL E. LUNGREN State of California
Attorney General DEPARTMENT OF JUSTICE
2101 WEBSTER STREET
OAKLAND 94612-3049
(415) 464-4200
San
(415) 464-1173
May 14, 1991
MARK D. ROSENBAUM
TION OF SOUTHERN CALIFORNIA
633 So Shatto Place
Dear Mark:
Erika Matthews, et al., vs. Kenneth Kizer
U.8.D.Cy N.D., CA, No. C-90-3620 EFL
During the two depositions which were conducted in
Sacramento on May 3rd we indicated that we anticipated a written
clarification of the Federal Government’s position vis-a-vis the
State’s lead screening/testing practices. Accordingly, I am
providing herewith a copy of Charles Woffinden’'s May 7, 1991,
letter to Michael Quinn.
Please call if you have any questions.
Sincerely,
DANIEL E. LUNGREN
Attorney General
E. VAN WYE
Deputy Attorney General
HEVhs
Encl.
cc: Jane Perkins, Esq., N.H.L.P. (w/encl.) re
=
“\ Dee’ = s \_“Hoalth Care
DEVARTMENT OF Ng SERVICES
# Financing Agmunstestion
a.
Rw’0. Region ix f
MCD-P-EMR Lh
KAY 7 1381 fay 3 FT 2/94 105
Mr. Michael Quinn, Research Manager
Child Health and Disability Prcveantion Branch (CHDP)
Data Management and Evaluation Unit
714 P Street, Room 708
Sacramento, California 95814
Dear Mr. Quinn:
The purpose of this letter is to correct the information you were perviously furnished in a letter dated April 11, 1991, Based on our most recent discussion with Linda Slaughter of the Department 3
of Health Services (DHS), our understanding of the States's lead
blood level assessment procedures was incorrect, AS we now
understand it, the State does not routinely perform the FEP test
for all children 1-5 years of age. A blood test for lead toxicity is performed when the need is indicated bY the patient's history and physical during an EPSDT screening, and the medical practitioner determines the type of lead blood level test that |{s
to be administered.
—
Lo
s
a
g
It appears that the procedures employed by the State basically comply with HCFA's guidelines governing lead toxicity screenings. The State Medicaid Manual provides that all Medicaid eligible children ages 1-5 be screened for lead poisoning, and a blood level [ assessment ls mandatory only when medically indicated by age and risk factors.
The Federal statute at Section 1905 (£)(1)(B)(iv) of the Social Security Act mandates the provision of "laboratory tests (including lead blood level assessment appropriate for age and risk factors).™ To assist States in implementing this and other provisions of OBRA '89, HCFA issued State Medicaid Manual (Part 5), Transmittal No. 3, dated April 1990. The guidelines in Section 5123.2 (D) (1) of this issuance provided:
*
o Lead Toxicity Screening - where age and risk factors indicate it is medically appropriate to perform a blood level assessment, a blood level assessment is mandatory.
o In July 1990, HCFA issued State Medicaid Manual (Part 5), Transmittal No.4 and Section 3123.2.D.1 was clarified to
It reads as
define lcad poisoning and recommended testing.
follows:
esr”
"Lead roxicity Scieening screen sll w eligible
Children ages 1-5 for leed puisoning. Lead poisoning is
detined as an elevated Venous blood level !{i.e., greater than
or egual to 23 micrograms por deciliter (uvg/dl) with an
elevated erythrocyte protoporphyrin (EP) level (greater than
or equal to 35 ug/dl of whole blood). In gencral, use the EP
test as the primary screening test. Perform venous blood lcad
measurements on children with elevated EP levels." (emphasis
added)
On the pasis of our most recent discussion, it appears that the
State is in compliance with the minimum Federal requiremcnts with
respect to blood lead level screening. We will verify California's
adherence to its stated policies and procedures in a forthcoming
on-site review of the EPSDT Program.
We hope that this information is responsive to your needs and we
regret any inconvenience that the earlier response may have caused.
Any questions may be directed to Edna Ray at (415) 744-3580.
Sincerely,
Y LJ
[oat adi
arles A. Wofifinden, Chief
Medicaid Operations Branch
cc: John Rodriquez, Deputy Director
Medical Care Services, DHS
Gordon H. Cumming, Ph.D., Chief
Ruth Range, Chief, Regional Operations, CHDP
i )
{
{