Affidavit of Judith Wessler
Public Court Documents
November 27, 1996
65 pages
Cite this item
-
Case Files, Campaign to Save our Public Hospitals v. Giuliani Hardbacks. Affidavit of Judith Wessler, 1996. c8c4c455-6835-f011-8c4e-0022482c18b0. LDF Archives, Thurgood Marshall Institute. https://ldfrecollection.org/archives/archives-search/archives-item/5f64013f-cfc2-4157-8400-d6ba0b2b67a6/affidavit-of-judith-wessler. Accessed February 22, 2026.
Copied!
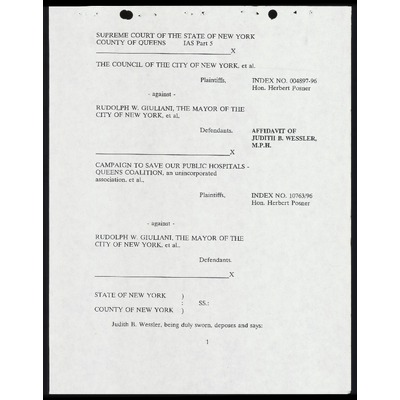
SUPREME COURT OF THE STATE OF NEW YORK
COUNTY OF QUEENS IAS Part 5
X
THE COUNCIL OF THE CITY OF NEW YORK, et al.
Plaintiffs, INDEX NO. 004897-96
Hon. Herbert Posner
- against -
RUDOLPH W. GIULIANI, THE MAYOR OF THE
CITY OF NEW YORK, et al,
Defendants. AFFIDAVIT OF
JUDITH B. WESSLER,
M.P.H.
X
CAMPAIGN TO SAVE OUR PUBLIC HOSPITALS -
QUEENS COALITION, an unincorporated
association, et al.,
Plaintiffs, INDEX NO. 10763/96
Hon. Herbert Posner
- against -
RUDOLPH W. GIULIANI, THE MAYOR OF THE
CITY OF NEW YORK, et al.,
Defendants.
X
STATE OF NEW YORK )
: SS.:
COUNTY OF NEW YORK )
Judith B. Wessler, being duly sworn, deposes and says:
1
1. I am a health policy analyst with knowledge of and expertise in
health policy and problems of access to health care. I have worked on health
care issues in New York City since 1970 as a health policy analyst, health
educator, and health advocate, and have counselled, taught, and written
publications on access to health care at the Health and Hospitals Corporation
("HHC") and the private hospitals in New York City (the "City"). I have
professional experience in reviewing policies and systems, assisting people in
gaining access to care, and teaching and writing about both how the public and
private systems work and how patients can use them. Specifically, I served as
Health Policy & Medicaid Specialist with the Children’s Defense Fund -- New
York Office from 1992 through 1995. during which time I worked to expand
comprehensive health services for children. I previously held the positions of
Senior Health Policy Analyst in the Office of the Manhattan Borough President
(1990 - 1991). Director of Health Advocacy with the Community Service Society
(1988-1990). Health Advocacy Coordinator for Community Action for Legal
Services (CALS) (1979-1988). among others. I received a B.A. from Boston
University and a M.P.H. from Columbia University.
2 In the past year I have reviewed publicly available documents
relating to the City’s plan to privatize the public hospitals, including the Report
of the Mayor's Task Force. the Offering Memoranda regarding Queens,
Elmhurst and Coney Island Hospitals. and the Letter of Intent signed by HHC,
2
- : : : > A f
r - » #
the City and PHS. I have also reviewed the draft Sublease ("the Sublease") of
Coney Island Hospital to Primary Health Systems - New York, Inc. ("PHS-NY")
and an outline of the contract agreement between HHC and Primary Health
Systems - New York, Inc. for the transfer of Coney Island Hospital.
3; This affidavit, first, provides an overview of HHC’s mission and the
ways in which HHC and private facilities differ with regard to access to care for
the indigent. See 11 4-14. In the second part of the affidavit I focus on the ways
in which the arrangements detailed in the Sublease depart from HHC’s historic
commitment to guaranteeing access to health care regardless of ability to pay.
See 19 15-39.
The Unique Mission of the Public Hospitals
4. Since 1992 I have served on the Coordinating Committee of the
Commission on the Public's Health System. an unincorporated association
established in 1991 in response to an announcement by Mayor Dinkins of the
formation of a blue ribbon commission to study the public hospital system.
Members of the Commission believed that meaningful analysis of the quality and
efficiency of health care delivery in the public hospitals could not consider HHC
facilities in isolation but should. instead. have focused on the respective
responsibilities and roles of the public and private sector. In 1996, for example,
HHC paid private medical centers nearly five hundred million dollars for their
services as affiliates of the public hospitals. yet the City Hospital Visiting
3
v
- : : ; » ;
r b Ld
Committee has found that the private affiliates have been responsible for
problems of low produciiviiy and high cost at HHC facilities.
5. Since 1991, the Commission has held multiple public hearings in
communities in Manhattan, the Bronx, Brooklyn, and Queens, many of which I
have attended. At these hearings community residents have spoken in support of
a public system. On numerous occasions individuals who were themselves
uninsured or whose families were uninsured spoke of their experiences being
turned away from the private system for non-emergent care and emphasized the
need for places to go for care that have no regard for a patient’s ability to pay.
6. HHC facilities operate in ways that are essential to the health of
New York City residents and particularly the City’s 1.9 million uninsured and
other medically indigent residents. HHC facilities provide a disproportionate
share of services to the uninsured and those people insured through the
Medicaid program. as well as to immigrants and to people who other hospitals
often do not want to treat -- prisoners. addicts, psychiatric patients, people living
with AIDS. tuberculosis, other chronically ill individuals and the homeless.
Coney Island Hospital's 450 bed complement, for example, includes 60
psychiatric beds.
7. In addition, public hospitals provide a large amount of care made
available for conditions that are expensive to treat, such as burn patients or
victims of life threatening trauma or crime. Six of the City’s 15 Trauma Centers
4
v < x » ’
T i” s
approved by the 911 Evaluation Unit are at HHC facilities. A seventh was
recently approved for Coney Island Hospital based on an demonstration of
medical need in the surrounding communities.
8. According to the Coney Island Hospital Offering Memorandum. in
1995 more than 87.8% of outpatient visits to Coney Island were made by
participants in public programs, i.e. Medicaid or Medicare, or by patients
categorized as "self-pay," the vast majority of whom are uninsured. Medicaid
patients alone account for 53.1% of outpatient visits. Similarly, participants in
public programs and "self-pay" patients account for 87.6% of inpatient discharges,
with Medicaid patients alone comprising 65.3%. The majority of Coney Island’s
net patient service revenue flows from Medicaid and the bad debt and charity
pools.
9, The particular services provided by HHC facilities respond to
community health needs and are critical to addressing these needs. For example,
HHC facilities play a unique role in meeting the health care needs of persons
living with HIV in the City. Despite the fact that a number of the not-for-profit
hospitals in the City are designated AIDS centers and receive higher levels of
reimbursement for treating persons with AIDS, last year HHC provided 51% of
hospital-based clinic visits to persons with AIDS in the City and 37% of inpatient
care stays. Moreover. the public hospitals treat a disproportionate number of
certain categories of AIDS patients. such as the drug dependent and women with
HIV/AIDS.
10. Similarly, it was HHC that responded to the tuberculosis crisis that
hit many of the City’s poor communities in the early 1990s, quickly developing
special programs such as the directly observed therapy program and new
outreach efforts.
11. HHC facilities operate in ways that are distinct from the private
sector, even from the not-for-profits. Most significantly, HHC facilities not only
provide emergency care without regard to a patient’s ability to pay, but also offer
non-emergent inpatient and outpatient services on the same basis. In contrast,
while federal law prohibits all facilities with emergency rooms from turning
patients away from an emergency room without first screening and, if necessary,
stabilizing the patient, private facilities are otherwise under no similar obligation
to provide services to those who lack adequate insurance coverage. Uninsured
people in cities with public hospitals are significantly more likely to receive
hospital care than those who live in cities with no public facilities.
12. Uninsured and underinsured patients who are treated at private
hospitals across the City experience difficulty obtaining medications and follow
up care. Many can afford neither the prescribed medications nor follow up visits
at an office or a clinic. As a result. for the most part HHC facilities have
maintained outpatient pharmacies. despite their cost. HHC now charges a
processing fee for prescriptions which can be forgiven if the patient is unable to
pay. Moreover, HHC facilities have aimed to offer comprehensive outpatient
care, again treating patients with no regard for ability to pay. While at
Community Action for Legal Services, for example, I developed and conducted a
telephone survey of public and private hospital clinics to investigate the degree of
difficulty uninsured patients experience in scheduling appointments and found
that (a) many private hospitals would not accept uninsured patients in their
clinics at all and (b) at those clinics that accepted the uninsured, uninsured
patients had a more difficult time scheduling timely appointments.
13. To the extent that a few voluntary, not-for-profit hospitals in New
York City have opened their doors to greater numbers of uninsured or
underinsured patients, they have experienced both financial difficulties and many
of the performance problems shared by HHC. Indeed, the survival of some of
the voluntary hospitals that have shared the cost of caring for the uninsured with
HHC 1s uncertain. Despite their similarities, however, these not-for-profits still
do not operate in a manner consistent with HHC’s mission. For example, they
generally seek to minimize unreimbursed patient care, whether or not such care
is needed by community residents. To whatever degree the operations of these
particular not-for-profits can be analogized to the public hospitals, they cannot be
seen as illustrative of how a private, for-profit corporation would behave. The
officers of the voluntaries serve the mandates of their institutions as directed by
their boards of directors or trustees but do not manage the facilities in a manner
' 4
: : « x ’ = 1 ‘ y
consistent with the interests of shareholders.
14. As public institutions, HHC hospitals and clinics are also subject to
freedom of information and sunshine laws, and their fundamental operating
decisions must be made in public. Thus, community residents and others who
rely on health care services have the opportunity to become involved in decision-
making. This is a unique and important feature of public facilities. HHC
provides care to everyone regardless of the limited and shrinking number of tax
levy dollars available, whereas under the Sublease PHS-NY would have only a
limited obligation to provide indigent care.
Questions and Concerns Regarding the Sublease to PHS-NY
Access to Care for the Uninsured and Underinsured
15. The Sublease does not guarantee that PHS-NY will treat everyone
who needs care regardless of ability to pay. The Sublease does not even require
that PHS-NY treat a specific number of uninsured patients. To the contrary,
Article 28 of the Sublease establishes a cap on PHS-NY’s obligation to serve the
indigent and defines PHS-NY's level of obligation in terms of dollar amounts.
Sublease at 74. 75. These provisions represent a complete departure from
HHC's practice of seeing all patients without regard to insurance status or ability
to pay and contravene HHC's mission.
16. In particular. PHS-NY is required to absorb the costs of care only
up to a specified "trigger point." The trigger point will be established annually
r
x x ¥ * 7 v 3
based on HHC’s audited charity care expense for Coney Island Hospital's most
recent fiscal year inflated annually and multiplied by 115%. Sublease at 75.
After the "trigger point" is reached, HHC will be obliged to reimburse PHS-NY
for costs incurred above the trigger point ("excess incurrence") for one year.
Sublease at 75. Although the City has represented that it will reimburse HHC
for such outlays, questions remain as to how such expenditures will be budgeted
and what impact they might have both on HHC’s annual budgeting process and
on the allocation of funds among HHC'’s other facilities.
17. After the first year of reaching the trigger point, the Sublease
explicitly permits PHS-NY to "manage access to health care in such manner as it
may deem appropriate so as to avoid ‘Excess Incurrence™ of indigent care if
indigent care costs exceed PHS-NY's cap in any given year. Sublease at 75.
HHC facilities cannot similarly "manage access to care." This provision is clearly
at odds with the mission of the public hospitals.
18. The Sublease also explicitly states that HHC cannot require PHS-
NY to provide indigent care if the trigger point is met: "[N]othing herein shall
give Landlord [HHC] the right to require Tenant [PHS-NY] to provide Indigent
Care in excess of such amount." Sublease at 75.
19. PHS-NY could inflate the reported cost of indigent care by
outsourcing services. thereby more easily meeting the "trigger point" while
treating fewer indigent patients. Currently HHC clinics and emergency rooms
9
x £ g y gs » Ld
post set charges along a fee scale for services. These are all-inclusive charges.
The Sublease does not prevent PHS-NY from outsourcing such services as
radiology, lab work, and pharmaceuticals and then charging separately for each.
PHS, Inc., outsources services in its Cleveland hospitals.
20. The City and HHC’s current projections of the number of uninsured
patients reliant on Coney Island Hospital for care and, thus, its analysis of the
likelihood that HHC will be required under the Sublease to reimburse PHS-NY
for indigent care, are erroneous and underestimate the impact of recent changes
in federal Medicaid eligibility. For example, Appendix A of the SEQRA Report,
attached to the Turbow Affirmation, states that 66% of the immigrants in Coney
Island Hospital's primary catchment area are refugees and thus remain eligible
for Medicaid under the Personal Responsibility and Work Opportunity
Reconciliation Act of 1996. Appendix A at 10. Yet the analysis fails to calculate
the impact of the Act on the one-third of immigrants who might no longer be
eligible.
PHS-NY's and PHS. Inc.’s Track Records in Service to the Indigent
21. The track records of PHS-NY and PHS, Inc. do not provide any
basis for concluding that this transaction will ensure continued access to care for
the indigent. First, PHS-NY is a for-profit corporation established in June, 1996
for the purpose of subleasing Coney Island Hospital. PHS-NY has never
operated any other hospital and it has no institutional track record. PHS, Inc.,
10
r .
L$ k y Ld
" x
itself only incorporated two years ago, and its reputation thus far is largely based
on two hospitals, St. Alexis and Deaconess, acquired in Cleveland within the past
two years. The little documentation available indicates that PHS, Inc. is, at best,
ill prepared to accept responsibility for Coney Island Hospital's indigent patient
population.
22. Coney Island Hospital is 450 bed facility operating with an
occupancy rate of nearly 90%. The Hospital annually receives more than 300,000
outpatient department visits, and discharges 17,000 to 18,000 patients from its
inpatient services. It serves a diverse, multi-lingual community and maintains
residency programs in internal medicine, general surgery, orthopedics, urology,
pedidivics obstetrics, gynecology and anesthesiology, ophthalmology, and
osteopathy. PHS, Inc., has never operated a comparable institution. St. Alexis
and Deaconess are both relatively small hospitals with much lower occupancy
rates. few salaried physicians. and no residency programs. Neither St. Alexis nor
Deaconess offer the type of extensive clinic system relied upon by Coney Island
patients. Coney Island Hospital receives more than 60,000 emergency room visits
per year. a figure almost twice as high as that at St. Alexis and Deaconess
combined.
23. PHS. Inc.’s performance in Cleveland raises substantial questions
about its commitment to providing access to care for the uninsured. According
to data provided by PHS for the years 1993 through 1996, total levels of
11
r
w S J 1 4
" 3
uncompensated care have dropped significantly since PHS, Inc., assumed control
of St. Alexis and Deaconess. A November 7 report by New York City
Comptroller that relies on figures supplied by PHS shows significant declines in
the amount of care provided to the uninsured working poor and the total
uncompensated care after PHS assumed control of St. Alexis and Deaconess.
See Report of the Comptroller of the City of New York, Attached as Appendix
A.
24. Documentation provided by PHS and HHC’s own initial reviews of
PHS’s current operations in Cleveland raise a number of additional unresolved
questions about both PHS’s commitment to serving the poor and the degree to
which PHS diverts resources to administrative costs and profits. According to
Dr. Walid Michelen, HHC'’s Senior Vice President for Medical & Professional
Affairs, who visited PHS hospitals in September, 1996, he had been informed
that these two hospitals "subtly" turned away indigent care patients. See
September 16, 1996 Memorandum from Walid Michelen, Attached as Appendix
B. In addition, HHC staff have raised concerns regarding PHS’s practice of
discontinuing and outsourcing services, its policy in Cleveland of taking 30% of
net revenues for profit and overhead. exclusive of systems, and the possibility that
PHS. Inc.. plans to transfer Coney Island Hospital after consummating the
transaction with HHC.
12
7
y
1 1
Services Accessible to the Indigent
25. The Sublease would allow PHS-NY to significantly alter the number
and types of services available to the indigent at Coney Island Hospital and does
not require either that such decisions comport with community health needs or
that PHS-NY guarantees continued access to these services.
26. In particular, the Sublease distinguishes between "Core" services and
"Non-core" services. Under Article 28 of the Sublease, PHS-NY must continue
to provide core services, including "Emergency Medicine, Medicine,
Obstetrics/Gynecology, Pediatrics, Psychiatry, Rehabilitation Medicine and
"nn General Surgery," "to substantially the same degree as provided by Coney Island
Hospital on the day prior to Commencement Date." Sublease at 67-68. By
contrast, the Sublease would allow PHS-NY to change the ways and means of
delivering "non-core" services (which include dental care, cardiology, urology,
endocrinology. ophthalmology. orthopedic surgery, podiatry, anesthesiology, oral
surgery. cardiac cath, pharmacy. surgical subspecialties and all other services not
listed as "core") at PHS-NY’s "reasonable discretion." Sublease at 68.
27. PHS-NY can thus make changes, including the closure of a non-core
service or the transfer of the non-core service to another site or provider, without
any effective limitation. Before closing or transferring the department, PHS-NY
must only give HHC notice. providing HHC with the opportunity to provide
input. The Sublease grants HHC no recourse should PHS-NY reject HHC’s
13
: » : ‘ X ¥
! » ’
recommendations.
28. The Sublease would allow PHS-NY to transfer responsibility for
performing inpatient and outpatient "non-core" services off-site to other
providers, including its affiliates, Brooklyn Hospital and New York University
Hospital, without any assurance that these providers will accept referred patients
without regard for ability to pay. Neither the Sublease nor any other publicly
available document provides any assurance regarding the accessibility of services
to the uninsured if patients are referred to private providers (i.e. doctors, private
practices or other private hospitals).
29. PHS-NY could, therefore, close or greatly reduce "non-core" services
‘that are crucial to community health but costly to provide. Such services might
include. example, care for the chronically ill. for diabetics, asthmatics or persons
living with AIDS. Such decisions would be inconsistent with HHC’s orientation,
which prioritizes the provision of public health services and places emphasis on
primary care.
30. Moreover. the list of "core" services contained in the Sublease
specifies the categories by department. not services. Available documentation
contains no list of services by department. Thus, it is unclear, for example, which
of Coney Island Hospital's 90 out-patient clinics (including, allergy, asthma,
diabetes. cardiac rehabilitation. out-patient surgery. hearing, geriatrics continuing
care. pre-natal. alcoholism. and family planning clinics, for example) PHS-NY
14
. x
L A y
» }
will continue to provide.
31. The Sublease would allow PHS-NY to change the ways and means
of delivering even "core" services and to alter the services offered within the
enumerated departments. PHS-NY could, after proceeding through a
notification and arbitration process, even close a "core" department without
getting HHC’s approval for reasons related to changes in government
reimbursement mechanisms, for example. Sublease, at 68.
32. By requiring only that PHS-NY provide care in the core service
areas to substantially the same degree as provided on the day before the hospital
changes hands, the Sublease also fails to provide a meaningful baseline for
measuring whether services are being reduced. A meaningful baseline would
reflect services provided during at least the most recent year, if not a longer
term. Moreover. the Sublease would allow reductions in services from current
levels as long as they are made by HHC prior to the transfer to PHS-NY.
Impact on Ability of the HHC System as a Whole to Fulfill its Mission
33. The Sublease and publicly available documentation fail to address
the impact of the loss of Coney Island Hospital to the HHC system and to
HHC's ability to carry out its mission throughout the City. The City has stated
that HHC will benefit from PHS-NY's payments for the purchase of Coney
Island Hospital. due at the time of closing. The City has offered no analysis, on
the other hand, of the costs of withdrawing Coney Island Hospital from the HHC
15
r
' « }
M %
system. In the past three to five years, HHC has been reorganizing to take
advantage of the benefits of its position as a multi-site system with purchasing
power and multiple points of entry. With the health care financing and delivery
system experiencing tremendous change and, particularly, with the growth of
managed care, the viability of HHC as a whole may be affected by the disposition
of HHC’s Coney Island facility. Already, following the announcement that
Coney Island would be privatized. Coney Island was removed from HHC’s
Brooklyn/Staten Island Network and has realized little benefit from HHC’s
recent efforts to network.
34. The Sublease also fails to specify whether PHS would participate in
HHC’s managed care program, Metroplus, and, thus, whether low-income
Metroplus enrollees would maintain continuity of care should they require
services in Southern Brooklyn.
Provisions for Monitoring Access to Care
35. The Sublease does not provide for effective outside monitoring or
the involvement of other city agencies. It instead puts monitoring in the hands of
a new community advisory board and HHC. Sublease at 69-72. These bodies do
not have the capacity to perform effective oversight to ensure that PHS-NY
continues to provide access to care.
36. In addition. community advisory boards at HHC facilities currently
have responsibility for oversight over planning and budgeting, areas that affect
16
’
¥ | |!
» L
access to care and the types of services provided. These responsibilities are not
included under the Sublease.
37. HHC does not appear to have the necessary staff to audit access to
care by PHS-NY. Indeed, audits performed by the New York City Comptroller
have found that HHC’s Harlem, Queens and Elmhurst Hospitals have not done
an adequate job of monitoring their affiliation contracts. Available documents
provide no evidence that HHC is reorganizing to expand and strengthen its
capacity for effective monitoring.
38. Moreover, the Sublease grants HHC limited ability to do effective
monitoring. HHC would have no authority to conduct surprise visits, nor to
observe the hospital's operations outside of normal business hours. Moreover,
most monitoring will be performed through the review of PHS-NY’s statistical
reports. Although the Sublease states that HHC may review PHS-NY’s books
and records, it does not require HHC to do so, much less at a regular interval.
39. The Sublease contemplates that HHC will monitor PHS-NY’s
performance and. where necessary. pursue arbitration to address problems but
fails to provide for the costs of monitoring and arbitration, including the costs of
legal fees. Such expenditures. as well as payments made to reimburse PHS-NY
for care provided above the trigger point. could divert needed resources away
from the HHC system.
17
’
! i 3
. 1)
Dated: New York, New York
November 27, 1996
SY b Wpsolon
JUDITH B. WESSLER
Sworn to before me this
27th day of November, 1996
Bn J (2
NOTARY PUBLIC
DENNIS D. PARKER
Notary Public, State of New York
No. 4972619
Qualified in Westchester
Commission Expires Oetober 1,
18
EXHIBIT A
: »
TELEPHONE: (212) 669-7396
FAX: (212) 669-3637
THE CITY OF NEW YORK
OFFICE OF THE COMPTROLLER
OFFICE OF POLICY MANAGEMENT
MUNICIPAL BUILDING, ROOM 517
NEW YORK, N.Y. 10007-2341
ALAN G. HEVESI
COMPTROLLER
ANALYSIS OF FUNDAMENTAL ISSUES THAT HAVE YET TO
BE RESOLVED
Whether The Hospital Will Serve Everyone Who Needs Care
Regardless of Ability To Pay
A The sublease does not guarantee that PHS-NY will see everyone who needs care
regardless of ability to pay.
The sublease does not require that PHS-NY see a specific number of uninsured
patients.
In his 10/30/96 presentation to HHC board, PHS’ Chair rejected David Jones’
request that these requirements be inserted into the sublease.
The sublease requires only that PHS-NY spend a certain amount on “charity care.”
The terms protect PHS-NY, by limiting its liability. But they do not guarantee that
the hospital will continue to carry out the mission of a public hospital
1. PHS-NY is required to provide care only up to a specified “trigger point.”
The trigger point will be established at closing based on HHC’s audited
charity care expense for Coney Island Hospital’s most recent fiscal year,
multiplied by 115% and inflated annually.
The sublease does not specify how PHS will calculate its charity care
expense. However, according to other documents, they will be calculated
on the basis of PHS-NY'’s fee schedule, rather than its actual costs. The
- State Environmental Quality Review statement says that PHS’ “charity care
expense” is the “difference between the charges [that PHS would normally
levy] and the portion for which the patients would be responsible.” In
other words, PHS is calculating its charity care as the amount of the
“discount” from its “normal” fee schedule.
3. PHS-NY could increase its “charity care expense” even if it treated fewer
indigent patients.
a. One way would be by increasing its fee scale.
b. Another would be through creative accounting. “Unbundling” is an
example of creative accounting. “Unbundling” means charging
separately for each part of what would normally be considered a
single service -- e.g., instead of charging for giving a TB skin test,
the hospital might give separate charges for the office visit at which
the TB test was “planted” and for the second office visit for
“reading” the test. This normally leads to higher charges.
4 The sublease explicitly says that PHS-NY can deny care if its charity care
expenses rise above 115% of the amount during HHC’s last year of
oeprating Coney Island Hospital. “Nothing herein shall give landlord
[HHC] the night to require tenant [PHS-NY] to provide indigent care in
excess of such amount.” After exceeding the trigger, PHS-NY “shall have
the night to manage Access to health care in such manner as it may deem
appropriate so as to avoid Excess Incurrence in the future.” HHC
facilities do not have that night.
5 It is possible that PHS-NY will automatically have greater “charity care
expenses” than HHC simply because it is calculating charity care expense in
a different way.
a. As indicated before, PHS-NY will estimate its charity care
expense on the basis of the money it is losing, in comparison to
what it would charge if those patients were paying paying “full
price,” according to PHS-NY’s fee schedule. “Charity care
expense” is the expense of forgone charges (including profit).
b. HHC appears to be calculating its own charity care expenses in a
different way: based on HHC’s actual costs, as reported on the
state’s institutional cost report form, not the fee schedule. Is this
true?
Cc If so, then PHS-NY would have higher charity care expenses simply
because it is using the fee schedule, while HHC is using costs. Fees
are normally higher than costs.
'State Environmental Quality Review, Appendix A, Full Environmental Assessment Form,
Part III, page A-7, released to HHC board on October 31, 1996.
2
’
’
[] L
’ NM
6. Eligibility for “charity care” will be based on PHS-NY’s own charity care
policy statement. PHS-NY’s policy statement (“New York City Charity
Care Guidelines”) was distributed to the HHC board on 10/31/96. The
statement includes the following provisions:
a. Uninsured “patients with annual incomes exceeding 150% of the
Federal Poverty Guidelines adjusted by the New York City wage
index will be expected to pay full charges.” In 1996 dollars,
someone will have to pay full charges if:
(1) single, annual income over $17,416;
(2) 2 person household, annual income of over $23,311;
3) 4 person household, annual income of over $35,101
b. Patients with incomes between 100% and 150% of the New York
City-adjusted federal poverty line will be eligible for the sliding
scale. The sliding scale is 20% of normal charges, up to 10% of
annual income.
C. The final group consists of patients with income below the New
York City-adjusted federal poverty line. These patients must make
the minimum payment -- $200 for inpatient care, and $20 for most
adult outpatient care. In 1996 dollars, this would include patients
who are:
(1) single, with annual income below $11,611
(2) two person household, income below $15,541
3) four person household, income below $23,400
d. Medicaid and Medicare patients have to pay some or all of the
difference between PHS-NY’s charges and the amount that
Medicaid and Medicare will cover. The amount of the “balance
billing” is based on the above guidelines.-- i.e., pay all of the
balance if income is more than 150% of poverty line, and 20% if
between 100% and 150%.
E. As discussed in a later section, the sublease does not establish an effective
monitoring procedure for monitoring the indigent care obligations.
F. PHS’ own data shows that it has poor track record in providing indigent care.
1. At 10/21/96 hearings of the New York State Assembly Committees on
Health, Corporations, and Labor, PHS presented estimates of the costs of
providing indigent care at its Cleveland hospitals. The estimates cover the
years between FY93 and FY96. PHS’ tables are attached.
*The guidelines appear to have been toughened in the course of the negotiations. It
appears that there was an earlier version of this policy, in which the cut-off for paying full charges
was 200% of the federal poverty line, rather than 150%
3
Ld
’ i \
[] -
\
2 The Comptroller’s Office prepared a new analysis of PHS’ indigent care
track record, using the numbers from PHS’ own testimony. The analysis
takes into account PHS’ criticism of the Comptroller’s prior analyses.
a. PHS said that 1995 data should not be used because PHS did not
operate the hospitals for that entire fiscal year. We did not
previously have 1996 numbers. Now that we do, we are using the
1996 numbers, rather than the 1995 numbers.
b. PHS also claimed that one of the 1994 numbers is much too high,
though they have not provided another, more accurate number. We
are now reducing the impact of the higher number by averaging the
data for 1993 and 1994.
c. We now compare the 1993 - 1994 average to 1996, so there is a
clear comparison between the most recent period before PHS took
over and the period when PHS was completely in control and had
some time to institute improvements.
d. The results are shown in the attached table. The table shows that,
even after we give PHS every benefit of the doubt, there is still a
big drop in care for the uninsured working poor (those above the
poverty line who generally do not have any health care insurance).
At St. Alexis, care dropped by 30%. At Deaconess, it dropped
39%.
e. The table also shows a drop in total uncompensated care. This
includes not only the working poor (those above the poverty line),
but also the most destitute (those who are below the poverty line).
For total uncompensated care, the drop at St. Alexis was 17% and
47% at Deaconess.
f In other words, even after taking into account PHS’s new
information, there are still substantial questions about what PHS
has done with the two Cleveland hospitals. And these declines may
well be understated because there is reason to believe that the data
for 1993 and 1994 understate the amount of care that was actually
provided.
G. During his visit to Cleveland, HHC’s Medical Director was told by persons outside
of PHS that Deaconess and St. Alexis do turn people away but “that they do so
subtly.” 3
September 16, 1996 memorandum from Walid Michelen, HHC Senior Vice President for
Medical and Professional Affairs, to LaRay Brown, HHC Senior Vice President for Corporate
Planning and Behavioral Health.
PHS refuses access to other pertinent data.
1. The Ohio Hospital Association has trend data on “payer mix,” indicating
the amount of care to people who are “self-pay” (which usually means
“uninsured”), as well as those who have Medicaid. St. Alexis and
Deaconess were participating in this data consortium long before the
change in ownership. This provides another way to evaluate whether PHS
reduced indigent care.
The Ohio Hospital Association will not provide such access without PHS’
approval. The Comptroller’s Office and the State Assembly have both
requested access to these data. But PHS has not given the approval for the
Ohio Hospital Association to do so.
There are unresolved questions about the impact of proposed changes in Coney
Island Hospital’s emergency room.
L. Due to their lack of regular care, indigent patients often enter a hospital
through the emergency room. Coney Island Hospital has over 60,000
emergency room visits a year -- almost twice as much as Deaconess and St.
Alexis combined. In its meeting with the Comptroller’s Office, PHS
expressed dissatisfaction with the number of Coney Island patients who
are admitted through the emergency room. How does PHS plan to change
this?
In its meeting with the Comptroller’s Office. PHS also expressed a desire
to rebuild or reconfigure Coney Island’s emergency room. on the grounds
that it is too crowded. How does it plan to do so? Will it be designed to
make the emergency room work efficiently or to make it uncomfortable
and hence reduce the numbers going to the emergency room.
»
’
1 1
]
[]
II. Whether The Hospital Will Provide The Services The
Community Needs, Or Only Those Services That Are Profitable
A. The sublease does not define specific community needs that PHS-NY is supposed
to meet, nor any external arbiter of what those needs are
1. Various outside bodies -- including the City and State Health Departments
and the City Comptroller -- have access to objective health planning data,
dealing with the prevalence of specific health problems, (e.g., HIV/AIDS,
alcoholism, asthma, heart disease and tuberculosis). But the sublease does
not even mention data on patient needs, let alone obligate PHS-NY to take
them into account.
ag The CAB is supposed to provide input on needs. But, as explained below,
in the section on monitoring, the CAB’s input is not binding, nor does the
CAB have to be representative of the community.
B. The sublease does not specify the particular services that PHS-NY must provide.
1. Attached is a list of Coney Island Hospital's 90 out-patient clinics and the
number of visits at each of them during each of the last ten years. For
example, there is information on clinics for family planning, allergies,
asthma, diabetes, cardiac rehabilitation, out-patient surgery, hearing,
geriatrics continuing care, pre-natal care, and alcoholism, among many
others.
2. The sublease does not provide information on which of these clinics will
operate. or at what level.
3. The sublease does not provide a meaningful baseline for measuring whether
these services are being reduced. A meaningful baseline would take several
years into account. However, the baseline stated in the sublease is the day
before the change in ownership
a. This might not reflect the level of service during the most recent
year, let alone the longer term trend.
b. After visiting PHS’ Cleveland hospitals, HHC staff said that they
were told that reductions of nursing staff were “done prior to the
PHS takeover within 90 days of the deal being signed.” For
‘Undated September 1996 memorandum by Jean Leon, HHC Senior Vice President for
South Brooklyn/ Staten Island network.
example, as part of the agreement with Deaconess, 225 employees
were dropped two months before PHS acquired the hospital.’
The main requirement about services concerns the continuation of seven
departments, which are considered “core” departments. These departments are:
emergency medicine, medicine, obstetrics/gynecology, pediatrics, psychiatry,
rehabilitation medicine, and general surgery. The sublease does not indicate what
specific services these departments will provide. PHS-NY can change the specific
services at its own “reasonable discretion.” But “reasonable” is not defined. The
only material constraint is that these particular departments are supposed to keep
operating, and to do so at “substantially the same degree” as on the day prior to
the PHS-NY’s takeover. “Substantially the same degree” is not defined either.
PHS-NY can close one of the “core” departments without getting HHC’s
approval. Before it closes such a department, PHS-NY must give HHC 90 days
advance notice. HHC can object. But, if it does, PHS can appeal to an outside
arbiter. The grounds for appeal would be if PHS-NY could argue that the closure
is a reasonable response to “changes in health care practices, changes in the health
care needs of the Coney Island community,” or “fundamental changes in
government reimbursement mechanisms, or other fundamental changes which
materially affect the delivery of health care services.” Those conditions are not
clearly defined.
1. The arbiter’s decision is final.
The arbiter is “the C.P.R. Panel of Distinguished Neutrals.” The acronym is
not defined. However, it may stand for Center for Public Resources, a
competitor of the better known American Arbitration Association. Who
are they and why were they chosen?
The arbitration process is itself poorly defined. Article 33 leaves open
whether the arbitration process will be governed by “federal or state rules
regarding court proceedings or rules set forth by private arbitration
organizations, including the Center.” Why is this left open?
Why is there an arbitration process in the first place? Why doesn’t HHC
have more power in defining the services that it wants its vendor to
provide? If the vendor does not want to provide those services, shouldn’t
the contract be voided?
HHC has even less influence over changes in other departments. In all the other
departments -- which are not considered “core” departments -- PHS-NY can
make changes (including closure) without any effective limitation (e.g.. to have the
*Raquel Ayala, HHC Vice President for Corporate Affairs, September 1996 report on
Cleveland due diligence visit.
. a
» 1 1
1 LJ
.
service provided by referring patients to another site, or by bringing in different
doctors). The departments where it has such discretion include cardiology.
urology, pulmonary care, pharmacy, dentistry, podiatry, oral surgery,
anesthesiology. endocrinology, ophthalmology, orthopedic surgery. and special
hematology. :
1. Before closing one of these “non-core” departments, PHS-NY has to give
HHC a chance to provide input. But there is no requirement about how
much advance notice to give.
2 PHS-NY is free to reject HHC’s input, without HHC having any recourse,
even to an arbiter.
’
’ 1 \
v []
III. Whether PHS’ Performance Will Be Effectively Monitored
A. The sublease does not make provision for effective, outside monitoring. It puts
monitoring in the hands of a new Community Advisory Board and HHC. But, as
shown below, these bodies are not in a position to perform effective and independent
oversight.
B. The sublease specifically drops reference to the authority of the City Comptroller.
1. No provision is made for the City Comptroller to verify PHS-NY’s
estimate of its indigent care costs by auditing and inspecting PHS-NYs
books, records, papers and files. Prior versions of the sublease had this
provision, but it has been removed from the current version.
2. PHS-NY is required to give HHC and the Community Advisory Board copies
of reports prepared by or for accrediting bodies or New York State. However,
the contract does not state that it is required to give these reports to other City
agencies -- such as the City Health Department, the City Comptroller or the
City Council. The same is true of its periodic “report cards,” which will
include statistics related to indigent care.
C: The new Community Advisory Board (CAB) does not have to be representative of the
community.
lL. The sublease calls for the creation of an entirely new Community Advisory
Board. There is no requirement that the existing community advisory board
have any continuing role, nor that any of its members be appointed to the new
CAB. The existing Board is, in effect, abolished.
2. Six of the CAB’s 12 members will be appointed by PHS-NY itself.
3 Only two seats are set aside for representatives of local community planning
boards and the Borough President. But the immediate catchment area has three
community planning boards -- 11, 13, and 15. No process is stated for which
community planning boards will be excluded.
4 The other four members will be appointed by the Mayor and HHC.
D. The Community Advisory Board (CAB) will not be provided with the means to be
good monitors.
]. Main responsibility is defined as publicizing the indigent care obligation and
providing a grievance mechanism. Members can make suggestions, but the
suggestions are not binding.
2. The CAB will not be given access to PHS-NYs insitutional cost reports and
9
other records of whether PHS-NY is meeting its indigent care obligations.
PHS-NY is not required to meet with the CAB more than four times a year.
Representatives of HHC, the City and PHS-NY are permitted to attend its
meetings, but “in no event shall the Community Advisory Board be deemed
hereunder a public body.” In other words, the CAB does not have to comply
with open meeting laws.
No specific time frame is defined for how soon the CAB must be established.
The sublease does not provide for the CAB to be given any staff, technical
assistance, or budget.
Most monitoring will be by HHC. But HHC will have limited ability to do effective
monitoring.
PHS must give HHC “access to Hospital and related facilities during regular
business hours upon reasonable request.” But HHC does not have authority to
conduct surprise visits, nor to observe the hospital’s operations outside of
normal business hours.
The sublease circumscribes the scope of the information HHC can request.
It must be operating or financial information and PHS-NY has to agree that
it is “reasonably needed to allow [HHC] to determine whether [PHS-NY]
has performed its service obligations and the indigent care obligations.”
PHS-NY has 30 days to provide the information.
The Comptroller’s audits have found that HHC’s Harlem. Queens and
Elmhurst Hospitals have not done an adequate job of monitoring their
affiliation contracts. How can we expect HHC to do a better job
monitoring PHS, when its position toward PHS is far weaker than its
position toward its affiliates?
Most monitoring will be through the review of PHS-NY ’s statistical reports.
The sublease says that HHC may review PHS-NY’s books and records.
But it does not say that HHC has to do so -- e.g., twice a year, or at some
other stated interval
HHC does not appear to have the necessary auditing staff. Does the City
plan to provide HHC with additional funds to hire additional staff or to
contract with an independent auditing firm? How much? What reason is
there to believe that HHC will have either the means -- or the motivation -- to
conduct aggressive monitoring once Coney Island is removed from HHC?
10
Even if HHC does find problems, its ability to enforce the contract is severely
limited. It is unfortunate that HHC’s authority over PHS-NY is so much less than
other agencies’ authority over their own vendors.
1, There is no recourse if HHC finds problems with the quality of care, unless
the problems are so great that the hospital loses its accreditation.
As discussed in the prior section, HHC would have very limited influence
over changes in services.
The sublease does define an enforcement process for violations of the
indigent care obligations, or if the hospital is in danger of losing its
accreditation. However, the process is so complex and lengthy that it may
not be workable. Enforcement would require HHC to go through all of the
following steps, and ultimately go to court.:
a. issuing a written notice of deficiency
b. meeting with PHS-NY
C. commissioning an independent third party audit to confirm the
alleged deficiency
d. giving PHS-NY further opportunity to correct the problem or deny
the deficiency
e. if PHS-NY still denies the deficiency, ask outside arbiter to hold
hearing to resolve whether the deficiency exists
f appoint an on-site monitor to observe the correction of the
deficiency
g. after the monitor has been in place for at least six months,
determine whether problem has been corrected; if not, notify PHS-
NY and meet again
h. seek further arbitration and/or take legal action
Section 28.04 (h) specifically states that HHC does not have any other
recourse for problems in indigent care, or services.
HHC 1s not given authority to impose fines for poor performance. PHS-
NY is not required to post a performance bond. from which HHC could
readily collect fines.
11
Will PHS Improve The Quality of Care?
A. The quality of care requirement is minimal. The only requirement is that PHS-NY
comply with the State’s regulatory requirements and that the hospital continue to
be accredited.
HHC is supposed to monitor PHS-NY by using statistical information, provided by
PHS-NY itself. Some specific indicators are mentioned in the contract, but most
of them are related to the quantity of care, not the quality. The only measure
related to quality of care is waiting time.
PHS has not negotiated an agreement for the provision of any specific number or
type of doctor -- neither with the hospital’s current affiliate (University Medical
oup), nor with Brooklyn Hospital, one of the proposed new affiliates. How can
the City even judge the quality of care without knowing where PHS will get the
doctors and what they will do? Will there be an agreement for physician services
before HHC is asked to approve the sublease, and will affected groups be able to
review it before HHC votes?
It is hard to make any meaningful evaluation of whether PHS-NY will improve the
quality of care in the absence of a clear statement about the specific services to be
provided, and without any written agreement between PHS-NY and a medical
affiliate about the number of doctors it will provide.
There are outstanding issues about the quality of care provided at PHS’ Cleveland
hospitals and their relevance for Coney Island Hospital.
E The main objective evidence that PHS improved the quality of care in its
Cleveland hospitals is that St. Alexis recently received a score of 93 from
the Joint Commission on the Accreditation of Health Care Organizations --
up from 90 in the Joint Commission’s prior review. But Coney Island
currently has a rating of 97. Is there any evidence that PHS hospitals
provide better care?
At her 10/24/96 briefing of the HHC board, Maria Mitchell said that PHS
will fare better in the next report of Cleveland Quality Choices than in the
last. But no evidence was provided. At his 10/31/96 presentation to the
HHC board, the director of Cleveland Quality Choices presented selected
data from the next report. The data showed no significant improvement
PHS Vice President Sussman told the Comptroller’s Office that there is an agreement
with Brooklyn Hospital, but that the agreement has to do with more general matters -- for
example, cooperation in strategic planning. There is no agreement at all with current doctors.
12
from the prior report -- e.g., at St. Alexis, the hospital’s ranking on
whether intensive care patients die was still worse than before the change in
ownership.
How have the PHS hospitals scored on the reports of the specialty
societies, such as the American College of Obstetrics, Academy of
Pediatrics, and American College of Surgeons? What is the evidence that
their evaluations have improved since PHS took over?
The Coney Island Hospital Community Advisory Board (CAB) was
scheduled to go to Cleveland to evaluate PHS hospitals for itself. But the
City cancelled the visit. Will the CAB have the opportunity to make such a
visit before the sublease is signed? If the CAB’s evaluation is negative, will
the deal be cancelled?
Frequent mention has been made of PHS’ 33 quality of care indicators.
What are they? How are they different from the ones Coney Island
already uses? What does PHS do with this data that is different from what
Coney Island does with its own data? When HHC staff visited Cleveland,
why did they find it “difficult to determine the structure used to monitor or
corrective action taken.”’?
PHS states that it uses these indicators to track its facilities on a regular
basis. Will PHS make this data public?
What specific steps has PHS taken to improve quality of care at its other
hospitals? How are these steps different from what Coney Island Hospital
is already doing?
The main improvement that has been mentioned by PHS or the City is that
PHS will invest in improving Coney Island Hospital’s physical plant, but
PHS said that it would not develop a capital plan until it takes the hospital
over. The specific capital improvements that have been mentioned are ones
that will improve the hospital’s financial position by making it more
attractive to potential patients, without necessary improving the quality of
care -- eg., building an atrium at the entrance, planting more shrubs,
improving the elevators, and converting six patient rooms into two and
four patient rooms. Most of these proposals are in the hospital’s existing
capital plan. Moreover, the amount PHS has commited to spend ($25
million over five years) is less than the amount needed -- $117 million,
"Undated September 1996 memorandum by Pete Velez, HHC Senior Vice President for
Queens network.
13
according to J.P. Morgan’s analysis.®
PHS also said that it would increase the amount of outpatient care. But
HHC staff who have visited the Cleveland hospitals pointed out that these
hospitals “provide few outpatient services at the hospital site,” “the activity
in the emergency department is extremely light,” and the hospitals “are not
comparable to Coney Island Hospital in scope of services, volume of
outpatient and emergency room workload or diversity of patients.”'°
Concern was expressed over whether PHS’ management information
systems are sufficient to manage the volume of outpatient care at Coney
Island Hospital." For example, the system “is inpatient oriented with little
emphasis on outpatient” [care] and it “does not have an appointment
booking system.”!?
*J.P. Morgan, Report to the City of New York Concerning the Privatization of: Coney
Island Hospital, Elmhurst Hospital Center; Queens Hospital Center, March 1995.
Velez, op cit.
"’LaRay Brown, HHC Senior Vice President for Corporate Planning and Behavioral
Health, “Summary of HHC Senior Management Staffs’ Site Visit Reports,” September 1996.
'"HHC Assistant Vice President for Corporate Reimbursement Peter Klemperer,
September 13, 1996 memorandum to HHC Senior Vice President Rick Langfelder.
“Summary of September 13, 1996 site visit to PHS/Integrated Health Computing, Inc.,
Wayne, Pa.
14
V. Whether Other HHC Facilities Will Be Adversely Affected
A The deal may endanger the tax status of bonds that were used to finance
improvements at Coney Island Hospital. An IRS determination that the City had
violated IRS regulations might make it more costly for HHC to finance capital
improvements in the future.
Ls In order for outstanding HHC bonds which financed improvements at CIH to
remain non-taxable, the change is use of the hospital must comport with
established IRS standards. Where those standards are not precisely met, as in
the case here, an alternative use of the lease proceeds may - or may not- be
acceptable to the IRS. The Comptroller’s Office has cautioned the City that
before it proceeds with the lease, it should seek a definitive ruling from the IRS
that HHC’s plans will result in the continued non-taxability of the outstanding
CIH debt. The City, however, intends to close the deal right away without a
ruling in hand. .
2. The IRS may ultimately rule against the City, determining that the City has
violated IRS regulations. One of the consequences of such a determination
might be that it would be more costly for HHC to finance capital improvements
at other HHC facilities in the future.
B. Misleading statements are being made about how Coney Island’s operating losses affect
the rest of the HHC facilities.
1 At its October 31 meeting, the HHC Board was given a document saying that,
in FY95, Coney Island Hospital had an operating loss of about $11.5 million.
The document goes on to say that eliminating Coney Island’s losses will
improve “the fi,nancial picture for HHC systemwide. >”
2 $9,034,000 of the $11.5 million is the amount that HHC charged off to
Coney Island Hospital, to cover the costs of running HHC as a whole
3 The Offering Memorandum says that the hospital made a profit of almost $10.4
million in FY 95, prior to deducting the cost of depreciation, interest, and the
allocations of costs from the Central Office.
C. In his 10/24/96 comments to HHC Board, Deputy Mayor Mastro said that $17 million
of the payment for Coney Island’s outstanding capital debt would be made available to
"*One page leaflet, titled “Benefits for HHC and the City.”
“We say “almost” because we reduced the estimated profit by taking out the $181,000 tax
levy contribution.
15
Ld
¥
®
.
.
HHC to reinvest in the capital needs of other HHC Hospitals. What assurances are
there that the funds will be used toward HHC’s capital costs, rather than for cash
flow or operating expenses, or that it will not be offset by other reductions in City
support?
D. HHC may be harmed by provisions of the sublease that require HHC to help PHS-NY
manage the costs of providing indigent care.
1. The sublease requires HHC to reimburse PHS-NY for the cost of providing
indigent care beyond the 115% “trigger point” during the first year in which
such costs are incurred. In its 10/24 briefing, the HHC board was told that the
City would sign a side agreement with HHC, under which the City would
reimburse HHC if HHC had to pay for excess care. The City has not provided
copies of any such side letter and, in any case, it is not clear that such a letter
would be readily enforceable. If the City intends to make this payment, why
doesn’t the sublease state that the City -- the “fee holder” -- would reimburse
PHS-NY’s excess costs? If HHC does bear these costs itself, then it has no
choice but to take the money from other HHC hospitals.
2 The sublease also says that if, PHS-NY is about to reach the trigger point -- or
if it has reached that point already, HHC will be informed and will work with
PHS-NY to manage those costs. Other than paying PHS-NY, HHC’s only
other feasible option is for HHC to transfer indigents to other HHC facilities.
3. At the same time, HHC is prohibited from competing with PHS-NY for the
neighborhood’s insured patients.
E. HHC gets substantial sums from Medicaid and Medicare in response to appeals of
reimbursement decisions concerning services provided in prior years. How will future
proceeds from future “rate appeals” be apportioned between HHC and PHS-NY?
F. The costs of monitoring are to be borne by HHC (the “landlord”), rather than by the
City (the “fee holder”). Has the City estimated the likely cost -- e.g., for contracting
with an independent auditor, or hiring additional HHC staff?
G. Disagreements between HHC and PHS-NY are to be resolved by using an outside
arbiter and, if necessary, going to court. Has anyone estimated how much HHC will
have to pay for arbitration costs or court costs?
H. According to a memo from HHC staff, * PHS’ president “claims that the city has
agreed to ‘relocate’ unionized staff that will be downsized to other facilities in the
'*September 16, 1996 memorandum from Walid Michelen, HHC Senior Vice President for
Medical and Professional Affairs, to LaRay Brown, HHC Senior Vice President for Corporate
Planning and Behavioral Health.
16
¥
[ Ll
[
A
corporation.” Is this true? Given the layoffs at the other HHC facilities. doesn’t this
simply increase the number of layoffs at the other HHC facilities? Doesn’t this simplv
shift PHS’ severence costs to other HHC facilities?
L The administration is making questionable claims about other hospitals getting more
money from the free care/ bad debt pool.
1. Mana Mitchell told the Comptroller’s Office that the City would save $7.5
million from a portion of the hospital’s Medicaid-funded reimbursement for
free care/bad debt for services rendered at Coney Island Hospital. This portion
comes from two particular pools of money, called the Supplementary (SUPP)
pool and the Supplemental Low Income Program Adjustment (SLIPA) pool.’
The City pays the $7.5 million into the pool, and the Federal government
provides a matching share.
2. These funds are available only to governmental hospitals. Coney Island
Hospital would no longer be eligible because it would no longer be a
governmental hospital. Therefore, the $7.5 million would be a real savings.
3. Mana Mitchell contends that the City would transfer the $7.5 million to other
HHC hospitals.
a She said that the City has authority to pay $7.5 million in liey of its pool
payments as an addition to HHC’s subsidy.
b. If thus 1s true, HHC would not have any recourse if the City did not do
SO.
C The City says that HHC no longer needs a subsidy,” even though the
City has paid $44.7 million subsidy so far this year and the cash subsidy
to HHC in the fiscal 1997 adopted financial plan is:
(1) 1997: $51.3 million
(2) 1998: $117.2 million
3) 1999: $113.2 million
4) 2000: $124.7 mullion
“Maria Mitchell gave this estimate during a September 6, 1996 briefing of the
Comptroller’s staff.
'"Mastro, op cit.
17
VI. Whether PHS Is Making A Credible Long-Term Commitment,
Or Whether It Will Pull Out When It Becomes Profitable To Do
So
A. There have been widespread concerns -- including by HHC staff who have visited
Cleveland" -- about whether PHS-NY has a long-term commitment to running the
hospital, or whether its ultimate goal is to make the hospital profitable and then sell it to
another health care entity -- perhaps a larger for-profit hospital chain.
]. The sublease permits this to happen. Within broad limits, Articles 10 and 11
give PHS-NY the right to sell its interest in the lease, transfer control, or sublet.
Section 10.01 (e) requires that PHS-NY notify HHC 60 days before the
effective data of the assignment, transfer, or sublease. HHC has 30 days to
object, but only on very limited grounds -- e.g., that the property is being
assigned to a criminal -- 10.01 (f).
If this does happen, what are the protections for HHC and the community?
Why should PHS have the right to sell its interest to someone else? Shouldn’t
the facility revert to HHC?
Why 1s PHS-NY’s capital commitment only for five years, and at a level ($25 million,
plus $5 million a year in routine maintenance) that is less than the $117 million that is
needed, according to J.P. Morgan's analysis."
PHS-NY was formed this June, the day before the letter of intent was signed. Asa
separate entity, PHS-NY could go bankrupt without the bankrupcy affecting the
position of PHS, the Delaware Corporation. In the event that this occurs, what are the
protections for the City?
Durning the 10/31/96 briefing of the HHC Board, the Mayor’s Office testified that the
City has investigated the background -- including a Vendex check -- of the two
individuals who are listed as officers or shareholders of PHS-NY, but not the rest of the
individuals and corporations that are shareholders or officers of PHS, the Delaware
"*In his September 13, 1996 memorandum to HHC Senior Vice President Rick Langfelder,
HHC Assistant Vice President for Corporate Reimbursement Peter Klemperer said that he
believes that it is “ultimately true” that PHS wants to strengthen its hospitals in order to “sell them
at a large profit.” He added that this won’t harm anyone “as long as the contract we sign protects
HHC and the community against any negative effects of a sale.” He did not say whether he
believes that the contract does in fact provide such protection.
"J.P. Morgan, Report to the City of New York Concerning the Privatization of: Coney
Island Hospital, Elmhurst Hospital Center; Queens Hospital Center, March 1995.
18
FJ
K ; N t
® :
1]
Corporation.
1; Both of the PHS-NY shareholders and officers are also officers or shareholders
of PHS, the Delaware Corporation. These are Robert Fleming and Michael
Sussman. Robert Fleming is Chairman of PHS-NY and also President of PHS,
the Delaware Corporation. Michael Sussman is President of PHS-NY and also
a Vice President of PHS, the Delaware Corporation.
Why didn’t the City also perform a background check on the rest of the officers
and shareholders of PHS, the Delaware Corporation?
In the 10/24/96 briefing of the HHC Board, Maria Mitchell said that PHS-NY will
make a security deposit of $750,000. Where does the sublease state this requirement
and the conditions surrounding the use of the deposit?
VII. Whether The City Got The Best Possible Deal
A. The State Attorneys-General of Ohio and Michigan have raised concerns that for-profit
entities do not pay fair market value when they acquire not-for-profit hospitals. In the
case of Coney Island Hospital, what was the basis for determining that $48 million
(Deputy Mayor Mayor Mastro’s estimate of the hospital’s outstanding debt) % is a fair
price?
1. Where is the document where PHS-NY states exactly what it will pay? The
sublease says that PHS-NY will “pay Debt Service Rent in the amounts and on
the dates specified in the Debt Service Rent Schedule attached hereto,” but the
schedule is not attached to the copies given to the HHC board. Deputy Mayor
Mastro said that the amount of outstanding debt is approximately $48 million 2!
but other documents mention a variety of numbers, ranging from a high of $50
million® to a low of $45 million.” What is the price?.
According to Coney Island Hospital’s audited balance sheet (attached to the
Offering Memorandum), the net value of plant and equipment by themelves
were worth $59 million in FY95. The market value of the land is another
$18.9 million, based on a 43% real estate equalization rate on a NYC
Department of Finance assessment of $8.6 million.. The total is roughly $78
million -- $30 million more than the $48 million stated by Deputy Mavor
Mastro.
The discrepancy would be even greater if we also included the value of the
hospitals’ current and projected revenues. For example, the hospital’s FY95
audited net patient service revenue was $221 million.
Did J.P. Morgan ever prepare an analysis of Coney Island Hospital’s market
value? What number did they come up with, and what was the basis by which
they arrnived at that estimate?
What were the offers that were rejected, and what were the dollar values of
those offers?
Were the losing bidders given an opportunity to match PHS’ offer; i.e., a “best
®Daily News, October 31, 1996, page 39
*'Daily News, October 31, 1996, page 39.
ZL etter of Intent, June 26, 1996, page 2.
PState Environmental Quality Review, Appendix A, Full Environmental Assessment
Form, Part III, page A-3, released to HHC board on October 31, 1996.
20
Ld
x ' '
&® !
. .
and final offer?
7 What is the evidence that other for-profits were given a fair chance to make
competing bids?
What arrangements have been made for PHS-NY to pay local taxes?
1. For the purposes of real estate valuation, the New York City Department of
Finance currently assesses the land and hospital building at $51 million. The
real estate tax would be over $2.3 million dollars a year. In prior drafts, the
sublease required PHS-NY to make a payment in lieu of taxes, in the amount it
would have paid were it paying real estate taxes. In the current draft, no
mention is made of such a payment. Will PHS-NY have to pay real estate
taxes, or make an equivalent payment?
2 As a corporate entity, what other taxes will PHS-NY have to pay? What taxes
will they be relieved from paying?
Subject to broad limits, Article 11 gives PHS-NY authority to mortgage the property.
What is the legal basis for a “leasee” to get a mortgage? Has the City estimated the
money that PHS-NY could earn bv mortgaging the property and then investing the
proceeds? Will the City, as landlord. get a share of those earnings?
The New York City Economic Development Corporation (EDC) was the lead entity in
negotiating this agreement. EDC’s main job is attract and retain business by offering
economic incentives. Did the EDC or the City offer PHS any incentives beyond the
apparent abatement of real estate taxes? What is their monetary value?
The hospital has a variety of concession agreements, covering services such as the
parking lot, the coffee shop, the gift shop, vending machines, and TV rentals.
Together, the most recent concession contracts are worth over $7 million. Does HHC
or the City retain any rights to these commissions, or to commissions from the
concessions?
21
VIII. Whether The City Will Save Money
A. J.P. Morgan estimated that, in the first five years, the deal would save the City
approximately $20 million a year. In a September 19, 1996, letter, we raised questions
about the specific elements of this estimate, and asked that J.P. Morgan provide further
explanation. Maria Mitchell promised that J.P. Morgan would respond but it has not.
¥ How is it possible for the City to save $20 million or more a year on one HHC
hospital when the City’s total subsidy for all 17 HHC facilities is only $51
million (according to the City’s adopted budget), and is expected to fall to
approximately $45 million (according to HHC officials), and when the
administration is now telling the press that HHC no longer needs a City
subsidy?%*
2 How does J.P. Morgan reconcile its estimate of savings due to loss in
operations ($5 million a year)® with the independent audit attached to the
Offering Memorandum? The independent audit estimates that, in 1995, the
City’s tax levy contribution to operations was only $181,000.%
3. Why does J.P. Morgan count the entire cost of capital maintenance and the
principal on outstanding capital debt as a savings, when most of this will be
recouped through Medicaid and Medicare reimbursements? Doesn’t it make
more sense to count only the portion that is not reimbursed?
4. On what basis are the capital savings being estimated? Are they based on
HHC’s actual spending or on the basis of projected needs? Are they based
on the amount that PHS-NY is projected to spend? If HHC is not actually
spending all that money, why is it all counted as a savings?
a. According to a document distributed at an October 31, 1996 HHC
board meeting, “HHC’s FY 1995 capital plan for Coney Island
Hospital totaled $15.3 million in projected five-year spending for
new projects.”
b. Yet, a document distributed at October 24, 1996 board meeting,
#Deputy Mayor Mastro said that, “for the first time in its 26-year history, the Health and
Hospitals Corp. can pay its own way without a city subsidy, generating its full $3.2 billion
budget” (Daily News, October 31, 1996, page 39).
*Maria K. Mitchell, “Testimony to New York State Assembly Joint Committee Hearing
on The Privatization of Coney Island Hospital,” August 13, 1996.
KPMG Peat Marwick, Independent Auditor’s Report, “Statement of Revenue and
Expenses,” line titled, “Funds appropriated by the City of New York for Operations.”
22
LJ
1 » t L]
.
p .
titled “Benefits for HHC and the City” lists the saving from
avoiding future capital liabilities as $50 million -- the entire amount
of PHS’ five year commitment ($25 million in capital
improvements plus an additional $5 million a year in routine capital
maintenance).
5. In addition, there appears to be double-counting. In one part of the
October 24 statement of benefits, the repayment of $48 million of existing
capital debt is listed as one of the savings. Later, separate mention is made
of “$17 million of the initial payment available for qualified HHC capital
expenses.” But isn’t the $17 million part of the $48 million?
6. How did J.P. Morgan calculate the amount the City would no longer have
to pay into the indigent care pool? Why would the City save from pool
payments when most of these contributions are part of the City’s Medicaid
share and, therefore, payable regardless of whether the patient is going to a
hospital operated by HHC? Are they just talking about SLIPA and the
supplemental pools -- the portions of free care/bad debt pool for which
public hospitals are the only ones eligible??’
B. To what extent does the administration’s estimate of possible savings take into
account the offsetting loses -- eg., loss of hospital revenues, the net value of
hospital assets, additional payments when the cost of indigent care exceeds the
trigger point, the matching federal funds that were “pulled down” when the City
made its contribution to the portion of the free care/bad debt pool that Coney
Island can no longer collect (SLIPA and SUPP pools), and the continuing financial
Liabilities stated elsewhere in this memo -- including the potential for additional
interest payments if the IRS rules against the way the City is retiring Coney
Island’s existing capital debt?
C The sublease requires HHC to pay PHS-NY for PHS-NY’s “excess” costs during
the first year when the cost of indigent care exceeds 115% of Coney Island
Hospital's prior costs. But, when HHC’s own facilities face a similar “excess,”
the City does not increase HHC’s own subsidy.
]. Isn’t this itself a cost increase?
2. The sublease states that HHC is liable only for indigent care costs beyond those
for which state reimbursement is available. PHS-NY is eligible for
reimbursements from the main part of the State’s “free care” pool -- though not
from other elements (SLIPA and SUPP pools). However, the State is reducing
*’See supra, for explanation of SLIPA and SUPP pools.
23
LJ
1 { x
M
the total size of its free care pool. How will this affect HHC’s liability for PHS-
NY’s “excess” costs?
In her 10/24/96 briefing of the HHC board, Maria Mitchell said that the City
would sign a “side letter” with HHC, promising to compensate HHC for such
payments. What is the City’s estimate of the likely costs of keeping this
promise? What is HHC’s protection against the City offsetting this payment
through a reduction in the City’s overall subsidy?
What are the labor-related costs for which the City will still be liable?
1.
2
3.
4.
Unemployment and other severence costs?
Pension rights for employees who have participated in the New York City
Employees Retirement System?
Post-retirement health benefits?
Vested vacation and sick leave?
Coney Island Hospital currently provides free care for prisoners, and for the work-
related needs of police and fire fighters. Will PHS-NY continue to do so?
1.
2
Will there be a separate charge to the City? At what cost?
The City pays higher rates for employee health insurance when employees incur
more insurance costs. HHC saves the City on employee health costs when it
treats uniformed officers for free. Will PHS-NY bill City health insurance
when they take care of the work-related needs of police officers, fire fighters
and other uniformed officers. If so, what is the estimated impact on the City’s
employee health insurance costs?
The final sublease may leave the City liable for other costs, for which it was not liable
in prior drafts. What is the potential financial cost of the City or HHC of:
lL. Hazardous or toxic wastes found on the premises (current draft removes
protection of the City from Section 17.04);
Latent or patent defects in the hospital (protection of City removed from
Section 17.03).
Medical malpractice. Section 7.09 (d) is titled “medical malpractice,” but the
content is left blank. Section 19.01 (d) indicates that PHS-NY will indemnify
HHC and the City against any liabilities related to accidents and injuries which
occur in, on or about the premises. This clearly covers trips and falls. But is
this sufficient to cover medical malpractice liability, which is not specifically
included in the list of liabilities for which PHS-NY must indemnify HHC or the
24
Ld
L \ ' EE
t
.
IX. What Is The Evidence That The City Has Adequately
Investigated PHS’ Background?
A. In its meeting with the Comptroller’s Office, PHS promised to provide a list of the
documents that PHS has provided the City in response to the City’s “due diligence”
investigation. But PHS has not done so yet. Will the City or HHC provide such a list
itself?
B. What specific numbers does HHC have concerning trends in indigent care at PHS’
Cleveland Hospitals, beyond the data that we brought to HHC’s attention, from
institutional cost reports? For example, what data did HHC collect concerning trends in
the hospitals’ payer mix?
C. According to one of the documents in the HHC Board’s briefing book (“Responses To
Issues Raised At The Joint Public Hearing”), City investigators conducted “detailed
research” on indigent care at PHS-owned hospitals and found that “indigent care
provided by PHS-owned facilities was at least equal to and in some cases greater than
the level of charity care provided by prior owners.” What is the evidence to support
this conclusion?
D. What specific reports did HHC examine from the Ohio Health Department? From
medical specialty societies? May we have copies?
E May the Comptroller’s Office have a copy of the Joint Commission’s report on its
August 1996 visit to St. Alexis?
F. What are the findings of any investigations into the background and financial interests
of corporate and individual stockholders in PHS, the Delaware Corporation? HHC
staff said that HHC checked the background of PHS-NY’s two shareholders, but not
the background of the larger group (about 15) which owns shares of PHS, the
Delaware corporation. Why wasn’t the larger group subject to a background check?
May we have a copy of the report on Fleming and Sussman?
G. What is the evidence of PHS-NYs financial ability to carry out the terms of the
agreement?
H What are the names of the hospitals owned by American Health Care Management
dunng the ime when PHS managers were with AHCM. For which of these hospitals
does the City have independent assessments of trends in the quality of care, and the
level of indigent care? Which of these assessments will be made available? For
example, does the City have copies of California Health’s Department’s information on
indigent care at AHCM's East Los Angeles hospital?
26
M
t ( [}
be
:
»
X. Why Is The Administration Trying To Rush This Agreement
Through When PHS Is Not Yet Ready To Carry Out Its
Contractual Obligations and There Are Still Outstanding
Questions About the Legality of the Transaction?
A. In its 10/7/96 meeting with the Comptroller’s Office, PHS indicated that it did not yet
have a business plan, a capital plan, nor a clinical plan. In his 10/31/96 presentation to
the HHC board, the PHS Chairman said that PHS has a “vision,” but will not develop a
business plan until it is in control of the hospital. Without these plans in hand, how can
the City realistically judge their financial feasibility, or the likely quality of care?
1. How can the City judge the quality of care without knowing the specific
services that will be provided?
2. How can the City judge the likely quality of care when PHS does not yet know
what doctors it will have; for example, they do not have an agreement with the
physicans that currently staff the hospital. Will HHC require that there be such
agreements prior to approving the sublease? Will they be made public? Is
there a written agreement between PHS and its projected affiliate, Brooklyn
Hospital? Will this be made public prior to approving the sublease?
5. Many hospitals -- both public and private -- are experiencing severe financial
pressures. Without knowing PHS-NY” business plan, how can the City be
confident that it will not go bankrupt? PHS says PHS-NY will increase the
hospital’s revenue by attracting more insured patients, but other providers are
competing for the same patients, and many of them are in networks that are far
bigger that PHS.. How can the City evaluate whether PHS-NY will win out,
without knowing its business plan (eg., marketing strategy)?
a Does PHS have a track record of expanding the patient base at its other
hospitals?
b. Why do PHS’ Cleveland hospitals have an occupancy rate of less than
50% (compared to 90% at Coney Island),?® while also providing
relatively little out-patient care.?
4. At the 10/24/96 briefing of the HHC board, Maria Mitchell said that PHS-NY
needs the HHC board’s vote in order to raise the money to finance their offer.
What is the evidence that PHS-NY has the financial ability to carry out their
offer? Does this depend on PHS-NY mortgaging the hospital -- a practice that
the sublease will permit?
%Qctober 19, 1996 memorandum from James R. Dumpson to HHC Board of Directors,
titled “Summary Report of my Visit to PHS, Inc.
*Brown, op cit, and Velez op cit.
27
Ll
hd : »
L
.
B. The sublease states that PHS-NY will contract with PHS, the Delaware Corporation, to
manage the facility and that PHS will be the guarantor of the indigent care obligations.
However, on October 31, the City’s Law Department told the HHC board that there is
not yet a contract between PHS and PHS-NY. When will there be one? Will the HHC
board review it prior to agreeing to the sublease?
C, PHS said that it will negotiate with the existing unions. But it has not yet reached an
agreement with them. In her 10/24/96 briefing of the HHC Board, Maria Mitchell said
~ that the agreement will not go into effect until a labor agreement is reached. But we
did not find any such stipulation in the sublease. Where is there a written agreement
stating this stipulation?
D. Several law suits have been filed, challenging the legality of this transaction. In prior
versions of the sublease, it was stated that the sublease will not go into effect while
legal actions are pending. But this stipulation does not appear to be in the current
version. Why not? Will the HHC Board be asked to vote on an agreement without a
definitive judgement about the legality of the agreement?
E, What provision has been made to deal with the fact that HHC is subleasing the property
for a period that is longer than its own lease? The City leased the hospital to HHC 26
years ago (on June 16, 1970), for a period of 99 years. In 1996, the lease has 73 more
years to run. By what authority can HHC give PHS-NY a sublease that will run, with
renewals, for 198 years?
28
L]
é | |
[
[]
XI. Have All Agreements Been Made Public?
A The HHC board has been given copies of the sublease. However, the
administration has made statements about terms which are not in the sublease such
as the conditions for closing the sublease, and the amount of financing PHS-NY
payments must obtain. Are the terms stated in other documents? If so, which
ones? Will these be made publicly available before the board votes?
B. Are there other written agreements between PHS or PHS-NY and HHC, the
Economic Development Corporation, or with other City agencies? Will they be
made public before the board votes?
**One place it did so is in October 24, 1996 document for HHC board, titled “Coney
Island Hospital Privatization: Transaction and Board Process.”
29
INDIGENT CARE LEVELS AT
rE or
DEACONESS HOSPITAL
fry Ot
1993 - 1996 ny oie he seb!
ls/zr [6
» 93 Y ss Bi periiminaryl
Deaconess
Charges
Gen Asst 510,658 348,610 401,642 267,785
Other Charity __ 236.801 583.021 69.337 _168.144
< 100% Poverty
747,459 09% 931,631 1.1% 470,979 0.6% 435,929 0.7%
> 100% Poverty
152.723 02% 3.432.480 4.1% 170.964 02% 1.592.951 2.3%
- Total Indigent
: 905,184 1.1% 4,364,111 33% 642,943 08% 2,028,880 31%
Hospital Total Charges. 30704395 __82980370 __ 729.028.8610 _ 61994.144
Estimated Cost
<100% Poverty 496,026 555,269 472,034 180,911
Soir 104.669 2,045.822 172.349 _ 661.075
INDIGENT CARE LEVELS AT
FR om
ST. ALEXIS HOSPITAL PHS TESTimown
1993 - 1996 PNY S As senb!
|e / 2 / 14
93 wh 9 Sie {prodiminnry}
0 2,814,926 2,931,456 1,536,978
__2.888365 9. _ 2222608 456.191
2,888,365 6.0% 2,814,926 5.2% 5,154,064 96% 1,993,169 4.3%
2715411 3% 2.842680 32% 252.569 0.3% 1.424.578 22%
5623,776 11.6% 5,657,606 10.4% 5,406,633 101% 3,417,747 10% o!
48.354.747 54183390 531.783.2290 44079002 oils
1,689,557 1,667,148 2,530,574 1,600,515
1.600.086 1.683.586 124,008 1.143.936
OBNEY ISLAND HUSH IAL
CLINIC VISITS - FY 1967 THRU FY 1997 IsT uy
~N
]
len)
!
a SMS : FY1oe7 UY 1s6s FY19589 FYI FYISS1 FY 152 FY DO FYI99¢ FYI9S PYDS JME JMOL
cob CLINIC TOTAL TOTAL TOTAL TOTAL TOTAL TOTAL TOTAL TOTAL TOTAL TORAL FYI? EXT TORY :
Tp) .
g -l
S 840 ABORTION 2252 2085 1508 1178 "is "oe 0 * » 0 ] * fi
838 ADOLES. OUTARE - GRADY
15 “2 ” % Oo i
2 " 825 ADULT EVE. & WEEKEND oon 004 610 7 1 1 1045 292 1.714 1.519 8 2.281 -
- 083 ALCOHOL $8502 14.462 12008 11655 12158 105% 11205 10951 11,058 0,502 1.089 7m
wn 884 ALCOHOL CLINIC SERVICES
250 1,049 14 we
Tr 001 ALLERGY 4300 4333 42771 4246 441 4p 5308 5100 4541 3.947 “ne 3,050 |
ve) 629 AM-SURG. PRE-ADMIT 28 742 738 1181 1618 1388 1.761 $83 2.313 i
p 604 ARTHRITIS 1043 1733 1085 1717 15201 1513 16% 1683 1788 1,500 393 1,559
@76 BREAST SURGERY 307 1061 1100 148 1404 1717 2077 2100 2,12 2178 or 2015 i!
© 807 CARDIAC 062 1505 1843 167 2025 168 2128 1824 1851 157% 414 1843
on 871 CARDIAC REHAB. 0 405 75 858 ws 21 1 440
oii . 854 CARDIOVASC. IMAGING
3 1 0 0 [] 0 |
~ 857 CAT SCAN $80 1085 1128 1,008 1,008 0 0 0 0 0 o 0
976 CD 4 MONITORING 1 4 0 [| [|] o .’ 0
¥ 757 CDATP - DAY CARE : 12008 15837 21,146 20081 30767 30,008 2347 177 0 027 sit 2543
o 758 COATP-OP VISITS 153 3609 4030 3256 1847 479 13315 10,145 9,852 2829 8,050
860 CHC - FAMILY PLAN. 191 oe hh 146 125 a 7 42 15 1 ¢
758 CHC -GYN 1.028 853 69 1435 2 1,109 909 1805 1833 24 Te 2205
929 CHC - MED 6245 6083 08580 8070 838 1M TAR 7350 T7013 8,525 2492 0.007
803 CHC - PED 3585 387 4,05 3677 3004 2028 2.440 3017 3489 176 pad 2,760
814 CHC - POD (NON ROUTINE) 0 0 0 C3 468 433 405 408 485 we a3 250
” 728 CHC - POD. (ROUTINE) 0 0 0 32 12 8 3 52 4a n 3
Ln 796 CHC - WELL BABY 843 338 355 1,185 684 1220 nr 402 n 3 1 4
3 924 CHC HIV PRE-COUN NOT.
4 L 4
| 816 CHC HIV PRE-COUNNO T.
2 o 0 # 0
\0 842 CHC-OBS 843 361 808 a4 858 1,079 0s 7] 142 007 1464 a7
Oo 715 CHC-CD 4 MONT {SATI) 0 1 0 0 0 0 0 0
! 658 CHC-COMP HIV EV(SAT) 0 a 1 0 0 0 0 0
* 684 CHC-DENTAL COMPLETE 50 2241 1102 2726 3118 4088 5479 $309 1279 8,043
~ 688 CHC-DENTAL ROUTINE 3457 0 0 0 0 q 0 0 # 0
3 890 CHC-DENTAL-IN PROG 2140 4368 4703 1% LW 142 108 o79 pat 4
- 685 CHC-DENT. MPLANTY 4 3» 0 0 ° » 0
Oo 720 CHC-DRUG IMMUN (SAT) 0 0 0 0 0 * ’ 0
ro 837 CHCPOST CONT-NEG
12 4 102 7 14 158 » 341
' 936 CHCPOST CONT-POS 1 5 5 12 3 3 1 4
a. 663 CHC-PRECOUN TEST(SAT 4 4 75 125 1 v4) 1 400 [
3 633 CHEMOTHERAPY V
58 pot *" 185 12s 500 :
S 920 CHEST - TB 087 815 856 s18 ©@5 1448 2458 2114 2315 1,870 “0 1.781
680 CHEST BURGERY an 358 27e i. “Us S02 abe 870 7 ei we 813
\ 610 CHEST-NON TB 227% 2333 2513 2827 2880 3403 2635 2886 2,079 2,776 e12 2420
917 CiH FAM PLN HIV CSL-NT
1 » % i]
831 CiHH- OTHER HIV COUN-NT
45 Lv. 797 Hh 254
815 CIHHIV PRENAT COUNNT
18 308 261 Eo 188
872 COMP - HV EVAL 2 0 0° 0 » 0 ® 0
005 CONTINUING TREATMENT 10,024 1225v 11917 11820 11107 8742 7020 9044 10821 10714 ey 2.630
'
ON
EY
IS
L.
ME
D
Q
LUNE IDLANU NUDE iw
CLINIC VISITS -FY 1987 THRU FY 1997
n
o5T ssT |
2 sms Fyasss FYises FY 16s TY 1990 FV FY192 FYI FY1994 FY 995 JYDPS6 IOS 3 MOS :
L CODE CLINIC TOTAL TOTAL TOTAL TOTAL TOTAL TOTAL TOTAL TOTAL TOTAL TOTAL WY ed EXT Pe FY i
H
0° ga3 CYSTOSCOPY a Sn ow a Ms "es Mt. WN oa? J 148 P= |
> 615 DERMATOLOGY 2723 3080 2677 3150 3478 33% 2815 4374 A231 1 3920 b
o 894 DEVEL EVAL 1701 2ue 1350 1840 1.341 1420 1298 1323 1304 1,085 "me 674 H
Z- 817 DWMBETIC na aon 563 470 pa 543 441 438 52 7 3 29 s
5 037 DIABETIC 0 0 rT 115 "0 25 152 101 157 134 n Cy
pee 878 DRUG IMMUNIO THERAPY
0 y 0 1] » 0
> 631 EAR, NOSE, THROAT 3508 3748 3635 4048 IIR 4044 4583 4332 468 4204 1.497 4.7149 :
4 500 EMP VISITS{OTH CLIN) 3101 3301 567 ° 0 0 # 0 0 0 ¥ [] |
935 EMPLOYEE HEALTH 7015 0382 $5803 S42 755 7507 1903 9428 8978 5,629 1.008 ey
620 ENDOCRINE 1018 1152 1353 1078 1.134 1314 1472 175 1.484 1,411 ns 1,498 ;
0 892 EYE 1383 1200 1367 MB 3M 4947 4854 474 0018 5121 1412 5,002
wid 928 FAMILY PLANNING - CiH RES 673 453 7 308 200 126 1584 198 1002 428 1,000
< 896 FAM PLN-POST COUN-NE
7 a a9 A 2 a4 . 0
oN 970 FAM PLN-POST
0 5 12 @ 6 $ A ] '
+o 969 FAM PUN-PREC 8 TEST
s [3] 0 a4 45 19 3’ 12 :
3 624 GASTRO-INTES 4560 1486 1568 1758 1.008 1900 2118 22 2507 2,305 3 2511 i
600 GENITAL - URINARY 338 3288 3414 3633 31568 3827 4020 4831 5808 6002 L572 8237 :
855 GERWTRIC ALCOHOL
: 1.72 1778 2 ] 1] °
881 GERIATRICS CONT. TREAT. 2004 S958 7587 7898 7510 7.100 7613 7005 sas 2,007
822 GYN - ENDO 2 0 2 1 0 12 a 250 385 101 3 12
827 GYN - SCREENING 12 276 n 1 = 1 3 1 4 0 0
829 GYN - TUMOR 1244 1361 1420 1725 1.908 1572 g76 1319 1455 1.450 a 1,058
go 628 GYN- WALK N » 102 9 "2 129 302 157 (44 1.243 74 1404
vie 830 GYNECOLOGY 9231 9295 9275 0682 687 8670 10340 11002 11548 WSN 2p18 10,375
Ln 748 GYNAUROLOGY
@ 51 15 ~
3 704 HEAD - NECK 63 39 02 100 a 118 302 1 As an 02 405
— 708 HEARING 77 1.127 638 600 499 538 752 21 861 750 154 611
9 627 HEMATOLOGY 3425 2784 3810 3841 4385 48% sp13 ©6856 7608 7883 1898 150 ;
© 628 HEMODIALYSIS 2318 2748 2.078 1.957 a 3oh 1.830 2088 3 oe 8 1797
™ 832 INFECL DIS. 262 395 8 11 1 0 : TN 218 863
Jy 636 MED RECEPT (SHORE Y) 848 483 285 Le 414 ET = 3s 0 0 » °
634 MEDICINE PRIMARY CARE ~~ 54253 52008 48843 45502 4380 44501 42767 44.107 48.785 Wwr20 1201 47.848 :
> 958 MENT HLTH GRP COULAT.
3 0 0 1) 0
| 902 MENTAL HYG. 11402 9569 9400 OM7 8360 0.877 11202 11,118 11087 11,084 ass 12,045
- 671 MH CLN COLLAT.-ADULT
1 7 19 0 * 0
712 MINOR SURGERY 107 61 s6 54 7” a 14 75 ha “w 21 8
gs 641 NEUROLOGY s762 1428 1678 1730 1805 1.834 1953 1630 1344 1322 w 1,501
= 941 NUCLEAR MED. 973 Poa 789 1,009 041 1492 1200 1249 1,403 1420 243 064
841 OBS - HIV COUNTEST
2613 248 150 + +
848 08S - POST PART -CH 877 711 a7 $18 wy 2 941 681 ase ho. Ht 778
. 849 OBS - PRENATAL 9437 10071 10,108 11.771 10805 0026 10908 11,435 10,008 8,367 ax 8.616
wr 853 OBS - PREN TEENPREG
1 0 0 ¥ 0
= 851 OBS - sag 1138 1.113 1,352 1701 1742 1.501 1,384 1,200 m 1,679
: 852 OBS - WALK IN 10 28 50 74 7 51 nh 12 * C] 0
Er 614 OBS INTIAL VISIT - CHC 80 310 rig! 168 1S 2% 33 21 62 55 4 *
“u -
i
102288 PROLNVS WKI
oO
(GR)
LCOUNEY ISLAND SDI ba.
:
CLINIC VISITS - FY 1987 THRU FY 1997
: i
3
1; isT ;
S sms FY1967 FY ISS FY 136 FY 990 FY 191 FY1992 FY 198 DY (199% PV 1995 FY 19% 300% IMO :
AQ CODE cLNC TOTAL TOTAL TOTAL TOTAL TOTAL TOTAL TOTAL TOTAL TOTAL TOTAL rom TTY :
LQ
3
3 611 OBS INTIAL VISIT -CH 191 (7 S77 152 1050 1837 154 1408 1.108 tas ioe 1,085 i
’ 877 OCCUP. THER. 2928 2883 2712 200 2088 2793 2381 27M 4.5% 4,000 NL 3002 :
o 716 ONCOLOGY 1534 1742 1551 1939 1947 2181 1.500 1 5 120 * ° !
< 717 OPHTHALMOLOGY 731 e452 e652 S0¥ ABT3 49T 4AB8 4714 AWM 5.440 1.287 $027
© 719 ORTHOPEDICS 318 ©6344 0006 6828 807% 7043 0355 70% 1.500 7.77 1.004 8.308 y
¥ 765 PED - ADOLES. ape 2686 138 877 1224 1723 18 02 2548 3,087 "i 3,029 :
©O 907 PED - MENT. HYG. 4242 4812 484 ANN 4364 4142 3447 1820 1,363 0 (3 [1] :
» 797 PED - RENAL mn" 10 2s 71] 251 21 248 224 190 - m ’
791 PED - SCREENING
797 1063 1620 17080 2230 2613 24060 1,931 1,505 ar 1.004 t
782 PED - WALKIN “or 872 “oe 765 540 3 804 1200 1,408 41 1870 ;
7H 808 PEDIATRICS se? 632 6100 4871 S7® 858 od24 7318 A715 a8 180 7008
- 916 PEDS M H NEPTUNE
190 2000 230 3532 A 373
pi 888 PEDS MHCLN.-COLLAT
25 han 74 12 ° 0 :
851 PEDS SCHL MH PS188
43 1% 108 apa ” 357 :
4 908 PEDS SCHL Mii PS288
70 278 22 1.084 zr S04
fa 909 PEDS SCHL MH PSX20
55 14 150 290 20 115
771 PED. ALLERGY 71 422 513 hla 816 we ™ 555 a7 7 73 200
774 PED. CARDIAC 162 216 249 248 3 £114 297 341 42 ns as 37
781 PED. ENDOCRINE 200 237 180 180 210 333 34S US 21 us 1 m
787 PED. GYN 0 0 0 0 [7] 212 273 357 302 300 [1 1
788 PED. HEMATOLOGY 323 345 381 3 395 kT) 527 654 23 539 128 S08
0 793 PED. NEURO. 294 363 380 398 429 455 457 sn 457 ps , an
tH 788 PED. NIC ae7 801 1097 o7é 1.108 1114 1189 1385 1.20 1.581 2 2,071
ks 808 PED. WELL BABY 3908 4035 4420 433% sees 45271 4m 41® 3.670 2676 it 2,412
4 932 PED. (EVEN. +WK END) 4181 4040 4088 3546 340 2965 3100 1718 2435 2,142 are 1.085
0 722 PERWPHERAL VAS. DIS. 1648 1564 1,215 o77 830 637 ang 544 A 2 1]; 208
oo 872 PHYSIO - THER. 8534 10821 8884 7647 7548 7308 7527 es 7185 6.624 3.521 13,900
; 723 PLASTIC SURGERY 1255 1316 1248 13% 1459 1502 ted) 2030 1.079 2,064 es 2492
662 PODIATRY 6620 ©6455 4702 633 5134 4862 7031 7507 2245 8.044 2484 9.055
~ 725 PODIATRY (ROUTINE) ase 5.149 e282 4122 S51 10 4802 2333 4344 0255 2.204 410 1827
' 875 POST COUNSEL NEG
4 28 67 78 298 05 108 ia
- 974 POST COUNSEL POS
1 2 11 14 3M 30 7) 40
= 873 PRE COUNSEL & TEST
" w od 138 1 tM "3 o47
vin 062 PRENATAL POST COUNN
3% 25 283 199 =] 782 "7 742
961 PRENATAL POST COUN-P
1 2 4] Ss 2 5 2 (1
ai 960 PRENATAL PREC & TEST
«Q 738 981 1048 I. 843 240 952
2 850 PREN. - HOGH RISK 478 79 850 7 20 1407 1839 213 1.01 244 e108 2444
635 PRIMARY CARE RESID. CIN 071 4991 5532 4442 0488 7505 7230 7838 7, 5,082 1370 5.435
728 PROCTOLOGY 03 612 841 ard a4 842 905 1.153 1,047 1.134 y £1 wt
910 PSYCH - DAY CARE 3448 3704 3548 4202 3612 2070 1.474 a 0 0 [] 0
i 580 PSYCH - OFF SITE 4612 S534 0 a 0 (1) 0 0 0 . *
wl 660 PSYCH. ADULT 3950 4835 4168 4428 5004 A850 5740 4TI3 485 5.230 1,840 8.145
ha 978 RAD. DIAG 2005 3782 3752 3906 ad412 S538 5000 7568 7AM 7.557 1.582 887
873 REHAB 4224 4350 4253 4001 3048 4153 437 47 4S 4822 1,189 4,683
A 649 RENAL 730 ans 775 a19 508 55 SQ 633 LS Hd “.e 1]
—
.
ta
A
192288 PROLNVISWIC
RD)
- QONEY (SLAND HOSH IAL
CLINIC VISITS - FY 1987 THRU FY 1987
ak wy
il PY987 FY158 FY1580 FYI9%0 FY 1991 PV 33 BY IMG FYI DV 1988 FYes 30008 El
CODE CLIC TOTAL TOTAL YOTAL TOTAL TOVAL TOTAL TOTAL TOTAL TOTAL TOTAL NYP EXT TONY
733 SCOLIOSIS ha 20 PX] " FA 13 7 ¢ 12 & 1 4
933 SCREENING 5700 5431 380 53%8 $292 G40 0007 ad TAL (Rig 184 0.204
25 SPECIAL MEDICAL CLINIC 1,740 1675 180 1433 1343 1421 139 188 1270 Le Yd 1,400
735 SPEECH 55 153 1873 1,220 is 28 "es T90 1202 “oe 2 "»
730 SURGERY 430 3818 3550 3W4 337 388 3654 3718 4115 - 37a ol 80
045 ULTRASOUND 3955 5031 5408 5509 4684 4785 5007 5.84 4.0% Len Lue AM
657 WOMENS ALC PROG. 1 SIM Gd A300 4390 1.997 RR 1801
TOTAL 200,000 310,985 312670 34170 32821 IAIN 332443 NA M48 BE MSE acd
Jc
t
24
°9
6
®
N
o
.
0
0
S
P
.
0
S
w
i
ie
s
i
e
m
a
eo.
0.
s
e
r
u
m
E
E
me
m
§
OS
s
fg
©
w
«b
o
SU
P
CE
C
—
—
—
-
s
i
®
@w
me
ce
c
o
c
m
m
e
REVISED ANALYSIS OF INDIGENT CARE COSTS AT PHS HOSPITALS IN CLEVELAND,
BEFORE AND AFTER BEING PURCHASED BY PHS (FY95)
TAKING INTO ACCOUNT PHS’ COMMENTS, AND UTILIZING PHS’ LATEST NUMBERS,
WHICH PHS PRESENTED IN ITS 10/21/TESTIMONY TO NYS ASSEMBLY, 10/21/96 *
GROUP RECEIVING WHETHER OHIO | REIMBURSED HOSPITAL
UNCOMPENSATED CARE PERMITS UNDER
HOSPITALS TO OHIO S Deaconess St. Alexis CHARGE THOSE | HOSPITAL
PATIENTS CARE :
ASSURANCE | Average of | Costsin | Percent | Average of | Costs in Percent
PROGRAM Yearly FY96* Change | Yearly FY96 Change
Costs, Costs,
FY93 and FY93 and
FY9%4 FY9%4
Income Above Federal Poverty Yes No $1,075,246 | $661,075 | -39% $1,641,836 | $1,143,936 | -30%
Line **
Income Below Federal Poverty No Yes $525,648 | $180,911 | -66% $1,678,353 | $1,600,515 | -5%
Line, or Receiving Ohio General
or Disability Assistance
Total Uncompensated Care -- - $1,600,894 | 841,986 | -47% $3,320,189 | $2,744,451 | -17%
SOURCE: Table attached to testimony of Steven Volla, Chairman and Michael Sussman
Health, Urban Health, Corporations, and Labor.
*The dollar amounts are what the hospitals reported (FY93,FY94) or expect to report (FY96) to the Ohio Department of Human Services in order to quality for partial state reimbursement. They do not include the cost of hospital services to Medicaid patients. Under Ohio law, recipients of General Assistance and Disability Assistance are covered only for physician services, not for hospital charges. For further explanation, see text. FY’96 is PHS projection, not yet reported to State of Ohio. FY’95 is excluded because responsibility split between PHS and pnor owners and because PHS said that
they did not write off FY95 debt until FY96.
**Due to changes in Ohio’s reimbursement formula, hospitals are now more likely to report all the costs of uncompensated care to people above the poverty line than they were in 1993. For that reason, these numbers probably understate the size of decline in services to the uninsured
, Vice President, Primary Health Systems, Inc, October 21, 1996, at New York State Assembly Joint Hearings of Committees on
working poor.
EXHIBIT B
EW YORK 43 HEALTH AND HOSPITALS CORPORATION
125 Worth Street - Room 507 « New York « New York 10013 '.. SEP23 1956
212.788.3848 Fax: 212.788.3681
: )
Walid Michelen, MD
‘a Senior Vice President
Gon & Professional Affairs
LaRay Brown
Senicr Vice President
Corporate Planning & Behavioral Eealth
Walid Michelen, M.D. (WYW
September 16, 1996
PHS SITE VIS!
Y. Mt. Sinai
Since this hospital was acquired by PHS in April, it is too
early for PHS to have rad any significant impact on its
operations.
II. Saint Alexis
PHS took over thie hospital about two years ago. Since that
time they have rebuilt an outpatient onceolegy unit and an
endoscopy suite. They plan tc rebuild the emergency room and the
operating roomisoon. 73RHS has laid off 150 FTE's and contracted
out laundry, dietary, and pharmaceutical services.
Their JCAHO survey was two months ago. They received a 93,
their highest score ever. They have a very good QA/PI plan in
place. However, it has performed worse than expected in
important areas such as pat.ent satisfaction, mortality, and
length of stay in the 5/16/96 report of the Cleveland Health
Qual.ty Choice (CHQC). It shculd be noted that the report's most
recent date of findings is 9/95, cnly one year after PHS took it
over. Because this report's analysis is much more outcome
oriented than the Joint Commission, its findings are troubling.
We should attempt to get some preliminary data from CHQC from
more recent periods.
St. Alexis spends about $1.2 million on ‘charity care", as
Per the CEO. They claim not to turn anyone away. Others claim
TOTAL P.21
. .
z p 3 [J ; ‘ L
1
-
a 3
that they do so subtly. It would rake more investigations to
determine what is really the case.
All the medical staZf is voluntary. Most receive a small
stirend from the hospital. Orne physician's income, at a hospital
clinic, is guaranteed. There are not housestaff, Thre physicians
I spoke with favored the PHS take over. They are satisfied with
the company, especially with the investments thev have dore.
They clearly see an improvement ir their ability tc render
patient care since PHS took over.
III. Deaconess
This hospital was bought by PHS about 18 months ago. Since
then the hospital has been reorganized.
Most of the physicians on staff are in private practice and
admit patients to Deaconess, as it St. Alexis. The medical by -
laws very much protected these physicians, and were exclusionary.
PHS did away with the by-laws and invited all physicians to
reapply. The vase majority of them did. PHS also contracted out
radiology, pathology, and the emergency room physicians. I did
not speak with any of the physicians.
Their last JCAHC survey was in 1994, before the PHS
purchase. However, their CHQC report was similar to St.
Alexis's. The recommendations are the sane.
es Sh TTI Ge |
My comments on uncompensated :.gcare are the same as those om -=
St. Alexis. - Lisiihd vids
IV. Overall
It 1s clear that PHS's approach is to downsize based on
their standards and then to interfere as least as possible with
the operations of the hospital. Some improvements are made. It
is clear that consolidations will increase, especially in
clinical areas, now that Mt. Sinai has joined the syscem.
During the visit we learned that PHS sees the Coney Isiand
Acquisition as its way to get a foothold on the New York market.
Its president claims that the city has agreed to "relocate"
unionized staff that will be downsized to other facilities in the
corporation.
Given the above, and other findings, the following issues
should be considerec:
*We should discuss the segue of redeplcyment with the city.
HAC should nct bear ti2 cost of PHS downsizin
*Can PHS handle a fhespital with so many unions?
*Can PHS handle such 2 ~culcurally diverse paiient and staff
population? :
*It is highly likely that PHS will exceed the indigent care
cap. Will the patients be sent tc King's, turned away? Wi.l the
city ask HHC to pay for the cost of the care exceeded by the cap?
WM/ep
cc: Luis R. Marcos, M.C.
Ty 57 nhs GREASE Hn
Rt Ba ies 2 AQ EST:
= leg em Fm GLINTES
TOT&L P.B2
Ld
:
t
"
SUPREME COURT OF THE STATE OF NEW YORK
COUNTY OF QUEENS IAS Part 5
wn a te en 2 X
THE COUNCIL OF THE CITY OF NEW YORK, et al.
Plaintiffs, INDEX NO. 004897-96
Hon. Herbert Posner
- against -
RUDOLPH W. GIULIANI, THE MAYOR OF THE
CITY OF NEW YORK, et al,
Defendants. REPLY AFFIRMATION OF
RACHEL D. GODSIL
mm X
CAMPAIGN TO SAVE OUR PUBLIC HOSPITALS -
QUEENS COALITION, an unincorporated
association, et al.,
Plaintiffs, INDEX NO. 10763/96
Hon. Herbert Posner
- against -
RUDOLPH W. GIULIANI, THE MAYOR OF THE
CITY OF NEW YORK, et al.,
Defendants.
a a a i ee nn ee me nm a ne x
STATE OF NEW YORK )
COUNTY OF NEW YORK po
Rachel D. Godsil, Esq. hereby affirms that the following is
true under the penalty of perjury:
1. I am an attorney duly authorized to practice in the State
of New York. I am Assistant Counsel to the NAACP Legal Defense and
Educational Fund, Inc. I submit this reply affirmation in response
to the Court’s request, made during a conference call had with
plaintiffs’ and defendants’ counsel on November 12, .1996, for
further submissions with respect to the issue of the legality under
# :
+ . ’
i [}
-
the HHC Act of defendants’ plan to sublease Coney Island Hospital
to a for-profit corporation. I make this affirmation in support of
plaintiffs’ motion for summary judgment and in opposition to
defendants’ motion for summary judgment. The facts set forth below
are within my personal knowledge or are based upon information
obtained from books and records of New York City, the New York City
Health and Hospitals Corporation ("HHC"), and the New York City
Economic Development Corporation ("EDC"), or © other public
documents.
2. Attached hereto as Exhibit A is a copy of the By-Laws for
the Health and Hospitals Corporation ("HHC").
3 On September 5, 1996, a Michigan Circuit Court held that
it violated the state’s not-for-profit laws for a not-for-profit
hospital to merge with a for-profit health conglomerate. Attached
hereto as Exhibit B is a copy of Kelly v. Michigan Affiliated
Health Care System, Inc., September 5, 1996 Court Ruling, Honorable
James R. Giddings, Circuit Court for the County of Ingham, State of
Michigan.
4. In San Diego Hospital Ass’n et. al, California Attorney
General Daniel Lungren concluded that the transfer of two not-for-
profit hospitals into a for-profit entity violated the Articles of
Incorporation. A copy of a November 8, 1996 letter from Attorney
General Lungren to John F. Walker, Jr. is attached hereto as
Exhibit C.
5. The transcript of the September 13, 1985 Board of
Estimate Hearing concerning the sublease of the R&S Building at the
. I
[N A
: 4
[
-
Bellevue Hospital Center addressed in Campaign Plaintiffs’
Supplemental Memorandum of Law submitted to the Court on November
19, 1996 was found at the Municipal Library on November 20, 1996.
I provided defendants’ counsel with a copy of the transcript on or
about November 22, 1996. A copy of the September 13, 1985 Board of
Estimate Hearing is attached hereto as Exhibit D.
Dated: New York, New York [
November 30, 1996 | (4
RACHEL D. GODSIL, ESQ.
Dated: New York, New York
November 27, 1996
JUDITH B. WESSLER
Sworn to before me this
27th day of November, 1996
NOTARY PUBLIC
18
SUPREME COURT OF THE STATE OF NEW YORK COUNTY OF QUEENS
DBR ae i te ep LE Sg LS Tg ie
Plaintiffs, INDEX NO. 004897-96
- against -
RUDOLPH Ww. GIULIANI, THE MAYOR OF THE CITY OF NEW YORK, et al,
Defendants. SECOND SUPPLEMENTAL AFFIRMATION OF
3 :
RACHEL D. GODSIL WITH EXHIBITS; AFFIDAVIT OF JUDITH B. WESSLER
i i Caled wl do BB Th A EY Cb Re X WITH EXHIBITS
, 4
CAMPAIGN TO SAVE OUR PUBLIC HOSPITALS - ®
QUEENS COALITION, an unincorporated oe
association, et al.,
Plaintiffs, INDEX NO. 10763/96
J
- against -
§
RUDOLPH Ww. GIULIANI, THE MAYOR OF THE CITY OF NEW YORK, et al.
WP
Defendants.
Rin Se Sebo dif uf ain Tk Ta Kh Sk RAT Nt x
KENNETH KIMERLING
PUERTO RICAN LEGAL DEFENSE & EDUCATION FUND, INC. 99 Hudson St., 14th Floor
New York, N.Y. 10013
‘
(212) 219-3360
+ ra
ELAINE R. JONES
pry
Director-Counsel Loh
NORMAN CHACHKIN :
MARIANNE L. ENGELMAN LADO
¥ &-
RACHEL D. GODSIL oa
NAACP LEGAL DEFENSE & EDUCATIONAL FUND, INC. 99 Hudson St., 16th Floor
New York, New York 10013
(212) 219-1900
dn,
BARBARA OLSHANSKY
CENTER FOR CONSTITUTIONAL RIGHTS
po :
666 Broadway, 7th Floor
:
New York, New York 10012
(212) 664-6464
ATTORNEYS FOR PLAINTIFFS