White v. Florida Hearing Transcript
Public Court Documents
August 21, 1969
Cite this item
-
Brief Collection, LDF Court Filings. White v. Florida Hearing Transcript, 1969. 1f3be5fe-c89a-ee11-be36-6045bdeb8873. LDF Archives, Thurgood Marshall Institute. https://ldfrecollection.org/archives/archives-search/archives-item/c4623ffd-f534-4ce2-b25f-c6cf122ac77f/white-v-florida-hearing-transcript. Accessed February 24, 2026.
Copied!
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
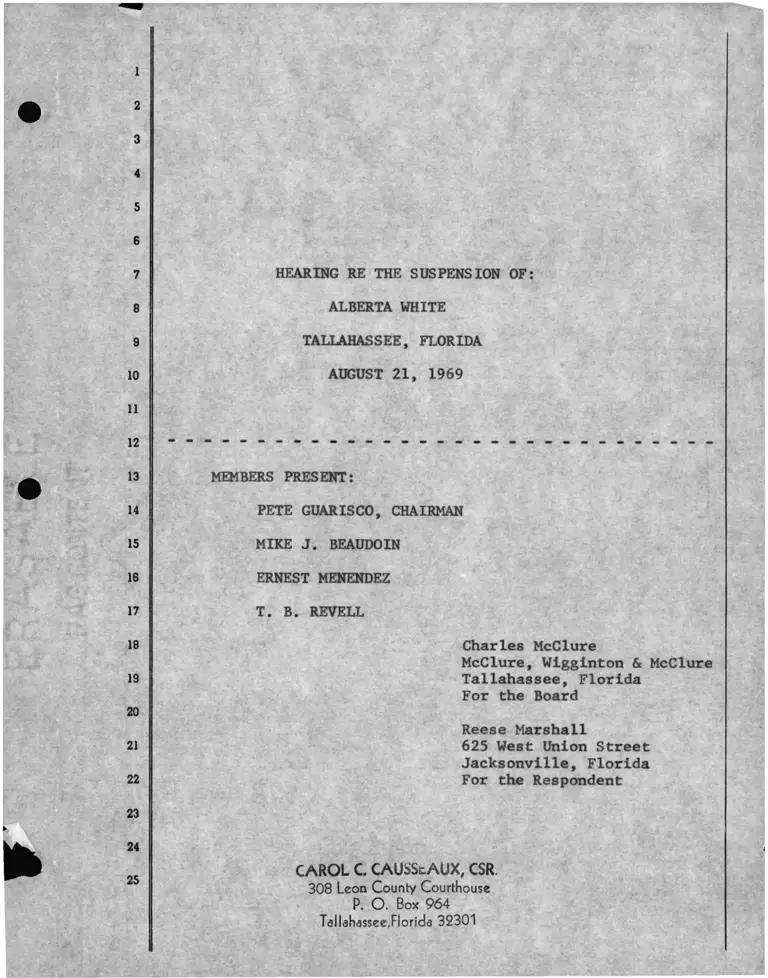
HEARING RE THE SUSPENSION OF:
ALBERTA WHITE
TALLAHASSEE, FLORIDA
AUGUST 21, 1969
MEMBERS PRESENT:
PETE GUARISCO, CHAIRMAN
MIKE J. BEAUDOIN
ERNEST MENENDEZ
T. B. REVELL
Charles McClure
McClure, Wigginton & McClure
Tallahassee, Florida
For the Board
Reese Marshall
625 West Union Street
Jacksonville, Florida
For the Respondent
CAROL C. CAUSScAUX, CSR.
308 Leon County Courthouse
P. O . Box 964
Tdllahassee,Florida 32301
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
NAME OF WITNESS
I N D E X
DIRECT CROSS REDIRECT RECROSS
JAMES N. TOOKS 19 53 76
E X H I B I T S
NO. & DESCRIPTION I.D. ADMITTED
1 - Notice to Mrs. White re hearing 18
2 - Notice of charges 18
3 - Notice from Mrs. White requesting hearing 18
4 - Cover letter from Supt. Ashmore 18
(Nos. 3 & 4 composite)
5 - Notice of hearing signed by Chairman 18
with cert, of service on Mrs. White 18
6 - Mrs. White's contract 18
7 - Supplement " 18
8 - Memo from Principal to teachers 23 36
9 - Letter to Mrs. White 41
10 - Evaluation of Mrs. White 42 45
11 - March 25 memo from Principal to Mrs. White 50 51
12 - Letter April 1 51
13 - Letter April 24 52
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
MEETING WAS CALLED TO ORDER BY THE CHAIRMAN AT THE
APPOINTED HOUR OF 10:00 O’CLOCK, A.M., AUGUST 21, 1969:
MR. GUARISCO: Are we ready to proceed?
MR. MARSHALL: Mrs. White is not here yet.
MR. GUARISCO: Let the record show that we are wait
ing for the respondent, Alberta White.
MR. McCLURE: Would it be appropriate for me to move
for a short recess?
MR. GUARISCO: Yes, sir, but as soon as she comes in
we will need to start the hearing. Let’s take a few min
utes recess here until she comes in.
MR. McCLURE: All right, sir.
MR. GUARISCO: While we’re waiting, why don’t you
gentlemen, for the benefit of the Court Reporter, intro
duce yourselves and proceed to that preliminary so that
it can be taken care of.
MR. MARSHALL: My name is Reese Marshall and I rep
resent Mrs. Alberta White in this cause.
MR. McCLURE: I am Charles McClure and I have been
retained to prefer the charges against Mrs. White and pre
sent them to the Board.
MR. GUARISCO: Mr. Marshall, would you give your
address for the record?
MR. MARSHALL: My address is 625 West Union Street,
Johnson and Marshall, Attorneys at Law, Jacksonville,
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
Florida, 32202.
MR. GUARISCO:
MR. MARSHALL:
MR. GUARISCO:
Mr. McClure, do you
MR. McCLURE:
I believe Mrs. White is here now.
May I have one further moment, please']
Yes, if you need a few minutes furthea
need a moment, also?
Yes. sir, I want them to study a dia
gram of the school.
MR. GUaRISCO: Let the record show that Mrs. Alberta
White has made her appearance here. This is a hearing
with the regard of the dismissal of Alberta White, 1112
Orange Avenue, Tallahassee, Florida. We will make part
of the record the notice of charges and I am sure counsel
will probably introduce those and also the notice of the
hearing which was mailed to the respondent. At this poin
then, with these preliminaries, Mr. McClure, are you
ready to present your case?
MR. McCLURE: Yes, sir, I am. I would like the
Board's permission for a brief opening statement and ther
the presentation of my case.
MR. GUARISCO: For the record, to make sure that we
can show that the Board members present are four, these
are Mr. Mike J. Beaudoin, Mr. Ernest Menendez, Mr. T. B.
Revell, Pete Guarisco, and the record will also show tha :
the Superintendent is also in the room representing the
the Executive Secretary, officer of the system,system as
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
Freeman Ashmore. Did you want to invoke the Rule, by the
way, before we get started?
MR. McCLURE: Yes, I would like to. I think it would
be a proper procedure at this time.
MR. GUARISCO: I think it’s fair to both sides if
you do invoke the Rule. Do you want to make the statement
now and then invoke the Rule after that?
MR. McCLURE: No, I would like to invoke the Rule
first.
MR. GUARISCO: Why don’t you get your witnesses to
gether and we will get the Reporter to swear them in and
invoke the Rule at this point and then proceed from there.
MR. McCLURE: All right, sir.
MR. GUARISCO: All witnesses that are going to appear
if you will come forward.
MR. McCLURE: Mr. Chairman, we have one witness who
will be coming in and who is at this point manning the
school, I believe, and is at another meeting. She will
be coming in later on.
MR. GUARISCO: All right, do you have any witnesses
at this time, Mr. iMarshall?
MR. .'1ARSHALL: No, but I would like to make an an
nouncement after the Rule is invoked to the Board.
MR. GUARISCO: Does anyone in the room here repre
sent anyone that you're going to use as a witness?
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
MR. MARSHALL: No, except, of course, Mrs. White.
MR. GUARISCO: The respondent is all right, but those
who are in here, once we invoke the Rule you can't use
them as witnesses.
MR. McCLURE: Mr. Chairman, Mr. Tooks is here and I
have asked .Mr. Marshall for a stipulation that he would
be able to remain here in the hearing room.
MR. GUARISCO: Do you stipulate to that?
MR. MARSHALL: Yes, sir.
MR. GUARISCO: All right, it is stipulated that
Mr. Tooks may remain in the room. All right, Mrs.
Causseaux, you may swear the witnesses and instruct them
as to the Rule.
(WITNESSES WERE SWORN AND PLACED UNDER RULE BY
REPORTER.)
.MR. GUARISCO: Sterling, you can make these people
comfortable in another room somewhere and perhaps you
can act as bailiff.
(WITNESSES WERE ESCORTED TO WITNESS ROOM.)
MR. MARSHALL: Mr. Chairman, I would like to move
for a continuance of this hearing because the witnesses
for Mrs. White, after my having contacted some twenty
persons, failed to appear because, in their mind, this
was an adversary proceeding and they were not clear as to
whether or not it would be ethical for them to appear b e
fore the School Board. All of them indicated that they
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
would like some reassurance from the Board that it is
proper and that they can appear and that they can give
testimony in this cause on behalf of Mrs. White. For tha
reason we only have one witness here today but there are
other names that we have and I can certainly furnish all
of those names to the Board and I would like for the
Board, in some form either formal or informal, to assure
them that it is proper for them to appear before this
Board and it is not an adversary proceeding in the sense
that the Board is moving against somebody as a defendant.
MR. GUARISCO: You are asking for a continuance for
the entire hearing?
MR. MARSHALL: Not for the entire hearing, no, but
for my - -
MR. GUARISCO: You mean for your side of the case?
MR. MARSHALL: Yes, for my side, yes, sir.
MR. GUARISCO: Well, that’s understandable, and I
think that request can be granted. If there is no objec
tion to that, we can proceed with the case that the Schoo
Board has and we can have a continuance for your side of
it. The motion is granted on that basis.
MR. McCLURE: Mr. Chairman, was this continuance for
another day this week or would it be for a specified timefi
MR. GUARISCO: I think we can arrive at a date here
before we get started now. We can select a date now,
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
and place, and proceed from there.
MR. McCLURE: Well, I did want to speak in oppositio
to the motion here.
MR. GUARISCO: Oh, you did, I’m sorry.
MR. McCLURE: Yes, sir, because I believe that the
notice was mailed out to Mrs. White on August the 8th and
the certificate of service shows that it was mailed on
that day to her through the United States mail and it is
the position of my client that they have had sufficient
notice to bring their witnesses before this hearing today
and that the plaintiff in this case is ready. There was
no prior notification of a motion for postponement and I
have gotten my witnesses here today. We have arranged
for them to be present and we have had no problem on get
ting witnesses and I think, without a prior motion being
filed, it would be an undue delay on the part of the
respondent here to ask for another continuance.
MR. GUARISCO: Your argument is well taken, counsel.
This hearing cannot go beyond 12:30 today due to prior
committment of members of the Board, so that we can allow
you to put on your case and if you are through, I think
Mr. Marshall can put the witness that he has heie on the
stand and then any continuance we might have would be in
respect to time running out, in which event we would have
to continue the case anyway. I agree with you that there
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
was ample notice and there is no excuse for the witnesses
not being here, but on the basis of the fact that we mighl
have to continue it for reasons other than the witnesses
not being able to be here, we can give them an opportunity
to bring them in at a later date. Now, we can get off th«
record and decide on a date and a time.
(DISCUSSION OFF THE RECORD.)
MR. GUARISCO: Let the record show that after 12:30
today the hearing will be continued to Saturday morning,
at 8:00 o'clock in the same room, the same place, and tha-:
both counsel have agreed that there will be no more con
tinuances for this case after today. You may proceed,
Mr. McClure.
MR. McCLURE: Members of the School Board, I would
like to make a few brief opening remarks to acquaint you
with what to expect will be presented today in support of
the charges for dismissal of Mrs. Alberta White, the
respondent. We are here today on a landmark decision in
Leon County. Your job, as members of the School Board,
is not a pleasant one; it's one that people would rather
not have, as a matter of fact, to prefer charges against
someone who has been in the school system for a long time
and prefer those charges in an attempt to terminate her
contract and terminate her services as a school teacher.
It's one, certainly, that the witnesses would rather be
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
someplace else than to be here to testify and certainly,
with the witnesses that we will call today as being con
temporaries of Mrs. White, fellow faculty members for one
or two years, and maybe even more. It's one that Mr. Took
the principal of Pineview Elementary School, certainly
doesn't like to bring up, but because of the responsibilit
and importance of this particular type of proceeding and
the effect not only that he has had in the past but would
be projected in the future if Mrs. White were allowed to
continue in teaching, the effect on our children is the
primary importance here today. It is not pleasant for
me to bring these charges, to draw them up, to interview
witnesses and to ask people to appear here and testify
today of the things they observed during the past two
school years, '67-'68 and '68-'69. It's not pleasant for
anybody, but the importance of this job is similar to
other jobs that juries have to maintain order in our
society and mairtain the peaceful community and to save
the taxpayers money. Today evidence will be introduced
that will attack the very competence of Mrs. White. She
has taught for nearly forty years, I'm told, in the
school system of our State but this evidence, some of it
will border on insubordination, neglect of duty, or in
competence. It's going to be embarrassing to have people
come up and testify to that. We don't like to do it but
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
we have a job to do. You will hear testimony that Mrs.
White couldn’t control her children in her classroom.
You will hear testimony that the children were even slip
ping out of her classroom while Mrs. White was there,
without any authority and without any purpose or any
place to go. You will hear testimony that Mrs. White
couldn't even stay awake in her classroom. These are not
pleasant things; the testimony will show that she went to
sleep, not on isolated instances, but on numerous occasio
throughout two school years, at least two school years,
and that she was so sound asleep in her classroom that
some of the fellow faculty members and secretaxies from
the school went to the door where Mrs. White's classroom
was, and, from the door, saw that she was asleep and call
her and walked all the way across the room to her desk
and called several times to her before she waked up.
These are not nice things to talk about but they are im
portant things to talk about. You will hear evidence tha
Mrs. White couldn't or wouldn't keep her room or her desk
straight or clean. For example, you will hear testimony
of old food wrappers and things like that on her desk
that were not just from a recent snack, but appeared to
be left there from several days. You will hear testimony
of papers on the floor. Now, everybody knows that childn
in grammar school, these children are going to have paper:
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
and things dropping on the floor and we're not saying tha
teachers should have a custodial duty here in Leon County
They have a professional duty, but to offer a proper edu
cational climate in the classroom for the students, they
have to keep some order and maintain some sort of clean
liness there, but you will hear testimony that her desk
and her room were filthy and what sort of educational
climate is derived from that type of condition? You will
hear testimony that Mrs. White couldn't, or wouldn't fol
low directions and orders from her principal, Mr. Tooks.
These are very basic things, not technical things, but
very basic things that she could not or would not do.
You will hear testimony that there was no evidence of an̂
lesson plans in her classroom. What effect does this ha\
on a school day for elementary school children? You wil]
hear testimony that she wouldn't read any messages that
came from Mr. Tooks, her own principal; that when the
messages were sent to her by one of the secretaries, tha1
she would either sign them and not read them or just say,
"They say I'm not a teacher, anyway, so there's no use oi
my reading these messages". You will hear after a con
ference with Mr. Tooks, after a continued attempt by
Mr. Tooks to have Mrs. White correct these different
discrepancies, that she directly disobeyed his order not
to return to the classrodm and you will hear the circumsf
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
whereby Mr. Tooks - - I mean Mrs. White, that she was al
most in a state of hysteria; that she was crying and
screaming end hollering, and this is the reason Mr. Tooks
told her not to return to her classroom because of the
example and the emotional impact that it would have on
her students. You will hear testimony that she did, in
fact, return in this state to her classroom. You will
hear testimony that she failed to prepare any records or
any plans for field trips and you will hear the importanc
of this. Students need to have field trips and principal
need to have some sort of plans to show that the teacher
has planned field trips. You will hear evidence that
there was no physical evidence or documentary evidence
that she had even taken her children to the library. How
important is the library to students, to youngsters try
ing to learn, and trying to get ahead in this world?
You will hear evidence that there was no grouping of
students in reading level groups or capability groups
or any group at all, but that they were all sitting as
one great big classroom. You will hear evidence that
the children's work was not displayed on the bulletin
board and each of you knows the importance of a child
getting involved in their work and having something to
be proud of, no matter how simple or how complicated it j
They need to have something to show off and say that the}
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
IS
20
21
22
23
24
25
did it. You will hear evidence that there was none of th
displayed in Mrs. White’s classroom and you will hear
evidence that the very one program, an assembly program,
that she had during the past year at Pineview on Memorial
Day was completely disorganized; that there was no point,
that there was no organization, there was no follow throe
and the results of the program itself were just tragic,
more than anything else. You will hear the testimony tha
she continually sent a stream of students down to Mr. Too
office for things that she could have controlled herself
and that a teacher normally would control herself. No,
these things aren't pleasant to talk about, but these are
all things, that, lumped together, you must take into
consideration who are the losers. The children are the
losers; they are the ones that are not able to catch up
because they weren't properly oriented and programmed in
their schooling. We are here today to present the case
and you have, as your job on the School Board, to listen
to all the testimony and to make your decision of whethei
or not Mrs. White should continue in any capacity in the
Leon school system and continue teaching our youngsters
and our children and to continue setting the example of
what she has set in the past few years and what effect
this may have on the children in the future. Thank you.
MR. MARSHALL: Mr. Chairman, I would like to reserve
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
IS
20
21
22
23
24
25
my opening statement to the time when I put on my case.
MR. GUaRISCO: All right, Mr. McClure, are you ready
for your first witness?
MR. McCLURE: Yes, Mr. Chairman, but first, Mr. Mars
and I have stipulated on the introduction of certain docu
mentary evidence dealing with the chages and notification
of charges and the response from Mrs. White, and Mrs.
White's continuing contract and her supplement to her con
tinuing contract, and we have also stipulated to the inti
duction at this point of the record book showing the date
the charges were originally brought before the School
Board, which are contained or which were decided on July
of this year. I would like at this time, without any ob
jection, to submit to the Board these documents, the firs
being, as plaintiff's exhibit No. 1, and if you will help
me keep up with the numbers here, Carol, is the notice to
Mrs. White informing her of her right to a public hearinc
and her right to counsel and cross examination of witness
and, without objection, I would like to introduce that ir
evidence.
MR. GUARISCC: Let's call these County exhibits in
stead of plaintiff's exhibits. Let's make this County
Exhibit No. 1.
MR. McCLURE: And at the end of the hearing here I
would also like, and I think Mr. Marshall has agreed, tha
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
some of the documents which belong in Mrs. White’s per
sonnel jacket, could be removed from the hearing record
and copies substituted in there, and also the record book
could be substituted. This is the notice of charges
specifying that Mrs. White has been accused of neglect
of duty, incompetence and gross insubordination, with the
specification as to times and places of these charges,
and that would be County Exhibit No. 2.
MR. GUARISCO: You don't have any objection to Ex
hibits No. 1 and 2, do you, Mr. Marshall?
MR. MARSHALL: No, in fact I have already stipulatec
to the introduction of those.
MR. GUARISCO: That they could be introduced now?
MR. .MARSHALL: Yes.
MR. McCLURE: Thirdly is notification from Mrs. Whii
of her request for a hearing. Fourthly, and this probabi
should have been numbered earlier, but this is the cover
letter from Mr. Ashmore on the charges and if we could
make that a composite exhibit.
MR. GUARISCO: All right, I*ve marked 3 and 4 as a
composite.
MR. McCLURE: Next is the notice of hearing signed
by the Chairman with a certificate of service on Mrs. Wh:
MR. GUARISCO: That's 5.
MR. McCLURE: Next would be Mrs. White’s continuing
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
contract of employment. I have previously shown all thes
to Mr. Marshall.
MR. GUARISCO: Do you have copies now that you want
to submit?
MR. McCLURE: No, I don’t have them all. I have
copies of the contract and the supplement to the contract
MR. GUARISCO: You have no objection to substituting
the copies?
MR. MARSHALL: No, I have no objection.
MR. McCLURE: The next one is a supplement to her
contract, '68-*69.
MR. GUARISCO: All right, sir, that will be Exhibit
6 for the contract and Exhibit 7 for the supplement.
MR. McCLURE: At this point, the last thing is the
record book and I would like to read into the record the
book and page number. These are the official minutes of
the Board of Public Instruction. I furnished Mr. Marshal
with a copy of the page and I would like for the Board tc
take official notice of the time and the minutes of the
meeting contained in the book, Minute Book 9, beginning
at Page 475 and continuing on Page 476, as it relates to
this particular case, showing that the origination of the
charges by Mr. Tooksand the Board'oaction, showing the
members present at the Board to be a majority of the
Board and that the vote was unanimous on preferring the
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
charges. I would like to submit this for the Board to
take official notice of it.
MR. GUARISCOi Let the record show that the Minute
Book is here and available to the Board members and take
official notice of it and if you want to look through the
minutes now or at any time later you can do that.
MR. McCLURE: I have it marked with a piece of paper
I have other documentary evidence that I will introduce
as the testimony goes along here.
MR. GUARISCO: All right, let the record show, then,
that County Exhibits 1 through 7 are admitted into eviden:
County Exhibits 1 through 7
admitted into evidence.
MR. McCLURE: Mrs. Lavania Lackey is here and she
is the custodian of the files and I have no longer need
for her to remain. Her presence was merely to have her
introduce these but we have agreed that the documentary
evidence could come from the files and records of the
School Board.
MR. GUARISCO: Mr. Marshall, have you stipulated to
that?
MR. MARSHALL: That’s fine.
MR. McCLURE: I’m sure that Mr. Ashmore needs her
back at the office if it would be all right for her to
leave at this point.
MR. ASHMORE: Mr. Chairman, if she could be excused.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
IS
20
21
22
23
24
25
we are in the midst of compiling our new schedules and
things and there are many important matters to be attende
to in the office.
MR. GUARISCO: All right, we'll excuse her.
JAMES N. TOOKS
was called as a witness and having been sworn, was examii
and testified as follows:
DIRECT EXAMINATION
BY .MR. McCLURE:
Q Give the Board your name and address, please, sir.
A James N. Tooks, Principal of Pineview Elementary School,
3303 Wheatley Road.
Q And you say you are the principal of Pineview Elementary
School?
A Yes, sir.
Q Do you know the respondent, Mrs. Alberta White?
A I do.
Q Would you point her out to the Board?
A She is sitting to my left at the end of the table here.
MR. McCLURE: We would like the record to show that
he did point to Mrs. White.
Q How long have you been principal of Pineview Elementary
School?
A Since July 1, 1967.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
Q Have you ever been a principal before?
A Yes, I was principal of Barrow Hill School prior to assum
ing the principalship at Pineview.
Q All right, sir, and how about before that, were you a
teacher?
A I was a teacher at Barrow Hill one year prior to that tim =
Q How long have you been a principal, Mr. Tooks?
A I started teaching the school term of '56-'57 at Griffin
Junior High School, teaching mentally retarded children.
Q Now, I would like to refer you to the school term of 1967-
'68 and direct your attention, so we can bring out an
orderly presentation of the evidence here, and was Mrs.
White a teacher at Pineview Elementary then?
A Yes, sir, she was.
Q Where was her room at the time?
A (No response.)
W*. McCLURE: For the purposes of identification
here, and Mr. Marshall has agreed, Mr. Tooks has preparec
a diagram of Pineview Elementary School and I would like,
at this time, to have him testify as to where his office
is and where Mrs. White’s room is located.
Q For identification purposes, will you tell the Board
where you got that diagram and what it is of?
A This is a diagram of the floor plan of Pineview Elemental
School. This is the room assignment for the past school
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
IS
20
21
22
23
24
25
term. There were one or two changes - -
Ml. GUARISCO: I believe if you would take it to the
easel that it would be able to be seen by everyone.
Q All right, could you give us first the location of Mrs.
White's room?
A This is the school's office here and Mrs. White's room
is located here, or was located here during the '67-'68
school term. During the '68-'69 school term her room
was located here.
Q For the record would you identify where you office is anc
how many rooms are in between your office and Mrs. White'
room for the '67-'68 school term and the '68-'69 school
term?
A I am putting my finger on the exact location of my offic«
now.
Q All right, and where does that appear on the chart here?
A In the southeast corner here. There are two rooms betwee
the office and Mrs. White's room during the '67-’68 schoo
term, including a boys'and a girls’restroom.
Q All right, and what about the '68-*69 term?
A The boys' and the girls' restroom were the only existing
structures betweenmy office and Mrs. White's office.
Q All right, I would like to direct your attention - - and
you may be seated now (witness seated). I would like to
direct your attention to on or around November 11, 1967,
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
18
17
18
19
20
21
22
23
24
25
and have you testify as to what event happened with rela
tion to Mrs. White and your school plan for the school
year?
A During this time all teachers at Pineview were issued a
memorandum of the things in which I would be looking for
upon visiting their classes. The memorandum had referenc
to do with schedule of principal's official classroom
visitation. Each teacher at Pineview was given this. I
indicated to all teachers at that time, after this visit,
that I would have a personal conference with each of the
classes visited. Upon visiting Mrs. White's class, she
was in receipt of this memorandum.
Q Would you identify that memorandum, does it have a letter
head on it and someone's name?
A All right, this is a typical memorandum that I sent out t
all teachers from the school's office.
Q All right, and what is the subject matter of the memoranci
A The schedule of principal's official classroom visitation
Q Was one like this sent to Mrs. White, this memorandum?
A Yes, it was.
MR. McCLURE: I would like to show that to opposing
counsel here. (Document examined by Mr. Marshall.) With
out objection I would like to have it marked for identi
fication.
MR. GUARISCO: That will be marked as Exhibit 8 for
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
identification.
County Exhibit No. 8 sub
mitted for identification.
Q And do you also have a classroom visitation check list?
A The checklist corresponded with the items that I observec
or did not observe in the classroom. This, of course, I
went through with each teacher here.
MR. GUARISCO: Is this a composite or will this be
individual exhibits?
MR. McCLURE: Well, without objection, I would like
to introduce it as a composite because they relate to th<
same thing.
Q Does this show a name of the teacher?
A Yes, it does.
Q Who does it show?
A Mrs. A. White.
Q All right, and where did you get that form from?
A This form was developed at Pineview School.
Q Is this the form that appears in Mrs. White's jacket at
your school?
A Yes, it did.
MR. McCLURE: All right, I would like to have this
marked as a composite exhibit.
MR. GUARISCO: All right, this is part of the County
Exhibit No. 8 for identification, a composite.
Q Mr. Tooks , I would like for you to tell the Board in youh
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
own words what you did insofar as Mrs* White and what you
observed in the classroom after receiving notification,
and I would like for you to explain to the Board where
this form came from, who agreed on it, and go through the
form and explain, item by item, what you expected and
what you found.
aA The form itself was/result of several years experience
as a principal observing certain things in the classroom
and listening to the teachers and the comments that they
would make and I would suggest at this point that the
entire instrument, as a composite of feelings and expres
sions of teachers and the type of things they would like
to be informed about prior to a principal's official visi
Q Was this form decided on by the teachers at Pineview
Elementary or did they assist in making it up?
A A committee of teachers did, yes.
Q All right, go ahead and explain your classroom observatio
at that time and the date of it.
A Well, the first thing that’s listed here, the first ques
tion asked is whether or not lesson plans, since the be
ginning of the school term, were present in the classroon
There was no indication of this. It’s reasonable to ex
pect that there is a tremendous amount of spontaneous
learning going on in a class but you would not expect all
of it to be spontaneous.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
Q You didn't find any lesson plans?
A None were presented to me when I walked into the classroo
and, of course, I would assume, inasmuch as all teachers
had this form, that I had specifically stated that I want
certain things in a particular area when I walked into th
classroom so that I would not have to disturb the teacher
while teaching. These are the things that were not there
the lesson plans. I did not see any samples of the
childrens' work. I did not see any evidence of grouping
other than the fact that the entire class was sitting to
gether as a body.
Q Why is it necessary to have grouping?
A Well, I think just because - - we believe that children
are different and they learn at different rates. Their
interest span is different and we can see that when the
bell rings all children are not ready for math and all
children are not ready for social studies and all childr*
are not ready to eat, so it's reasonable to expect that
the different interest levels of children would vary so,
therefore, we need to meet the needs of the children.
This is especially so in the area of reading. We need tc
think in terms of different levels that children read on
and provide the individual interest and the individual
teaching procedures and this, of course, could not be
carried on when students were sitting together as a body
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
The next four or six items on here related to things in
which were not necessarily present in the classroom. I
did not make any comment, whether they were existing yes
or no, because these records were available in the libra
or other places. For instance, with regard to the film
strip and records - -
HR. MARSHALL: Excuse me, Mr. Chairman, but I'm ha1
difficulty following this, Mr. Chairman, and is it my
understanding that this is offered in evidence or - -
MR. GUARISCO: This is for identification purposes
at this point.
MR. McCLURE: I do plan to introduce it into evidenc
after he has finished his testimony.
MR. GUARISCO: This is still introduced as an exhibi
for identification at this point. Just identify the iten
and explain what it stands for, that item.
Q All right, continue now.
A Item 4,"Records in your class, number and names of film
strips used since opening of class," and this, of course
I did not indicate on the check list that she should
direct her attention to because this information was
available in the library. Item b,"Names and places of
field trips,list of places planned for the rest of the
school term." This, of course, I did not see in the
classroom and I did not indicate it on the classroom
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
visitation check list because duplicate copies of these
are available to me in the office. Item b, "Names of
parents visited this school term." This, of course, was
not present neither was it presented to me. This infor
mation also is available to me in the office. No. 7,
"The number of times and dates the class visited the
library." This she was not checked on in the evaluation
check list, the classroom visitation check list.
Q Did you find any evidence of her class visiting your
library?
A No, I did not.
Q All right, continue.
A No. 8, "The number and name of library books read by
students in the classroom." This, of course, was not
present at that particular time and, of course, it is not
checked on the evaluation check list. Now, with regard
to the type of things I felt really reflected learning
in the classroom, I underlined evidence of children's
art work as no, that I did not see that at this time and
there had not been any indication that it had gone on as
of the 20th of November of '67.
Q All right, why is it important to have children's art wor
A I think that as a result of children working and express
ing themselves through the art media they get a chance to
relieve their inhibitions and get a chance to develop
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
their finger dexterity by using the finger paint, using
paste, being able to do things in three dimensional. This
develops a self-concept and at the same time it develops
their concept of the world around them. Then No. 10,
"Evidence of the classroom illustrating orderliness, good
taste and systematic procedure."
Q Would you explain what you would expect on that?
A Well, I don't expect chaos; I don’t expect regimentation;
I do think that children can be busy going about their
classroom and be engaged in meaningful activities and
experiences without feeling as though they are restricted
from moving.
Q And what did you find?
A I found children going about doing this - - some children
were working math problems out of work books. She was
sitting to the desk. One or two were reading comic books
and this sort of thing. The classroom, of course, was
disarrayed.
Q Would you go into detail as what you best recall about it
being in disarray?
A In my way of thinking there is a systematic way of
disorder. You can look at a person's desk and you can sej
that a person is busily engaged in something constructive.
You can look at the desk and you can also see a lack of
organization that they can't really put their hands on
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
anything because they don't know where it is.
Q What did you find on Mrs. White's desk, if anything?
A Quite a bit of paper, the desk was very dirty, food wrapp
and candy wrappers. I can't say it was hers and I don't
know whether it belonged to the kids, but it was there.
Q It was on her desk?
A Some was on her desk and some of this was on the work
tables in the classroom and this sort of thing.
Q When you say that the desks in her room were dirty, what
do you mean by that? What did you find on the desk or in
the room that would make it dirty?
as
A Such things/ broken chalk on the floor that certainly had
not been there for just that - - it had been there for a
period of time. The papers that were crumpled and paste
isand watermarks, this^/the general impression that I had.
Q Are these the type things that teachers are normally ex
pected to correct or is that a janitorial service that
the cleaners are supposed to keep up?
A Well, we don't want to have teachers doing custodial work
but we certainly want them to involve children in trying
to keep their surroundings clean. I don't mean they have
to take a broom every thirty or forty minutes during the
day or every ten or fifteen minutes during the day, and
sweep, but they certainly ought to provide them with some
housekeeping chores. I think this is a vital learning
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
experience that teachers can provide for children. In
many instances the custodians are available on the school
grounds and many times are engaged in other things, but I
don't think the students and teachers need to sit back
and wait for them to do it. If a teacher can’t get this
done, certainly the children on the fourth or fifth grade
level really get a big kick out of doing this type of
thing.
Q All right, and what grade was Mrs. White teaching in 1967-
A She was teaching fifth grade then.
Q What sort of educational climate does a room in Mrs. Whits
condition create for the children?
A Well, I didn’t think that it created much of an educations
climate at all. I was convinced that, in spite of perhaps
something she had to offer the children, I felt that
teaching wasn't it.
Q All right, go ahead and continue with your items there
and calling out the numbers, if you would.
A Well, 11 I think we have just explained, "Evidence that
your room and facilities are properly cared for." No. 11,
"Evidence that work was evaluated and returned to pupils.'
MR. MARSHALL: I'm sorry, but could you give me
No. 11; I was on 10.
A "Evidence that your room and facilities were properly
cared for." Then we go to No. 12, "Evidence that you
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
evaluated and returned all work that pupils are required
to turn in."
Q All right, and what were your results of the finding in
that?
A This, of course, I have a Mno"check which means that I did
not see any evidence of this.
Q All right, go ahead.
A 13, "Your personal appearance", and I have "no" here be
cause it was certainly, in my opinion, unsatisfactory.
Q Could you go into detail on that because this is a very
important thing here. Why should personal appearance be
an important part of a teacher's duty?
A I think a teacher represents something to kids that many
of them, perhaps, don't get from other people. I don't
think they have to come dressed as if they were going to
a White House steak dinner but certainly they need to
come attired pleasant, appealing, not, of course, sugges
tive, either, but something that children can look at and
admire. I don't think that it would be appropriate for
me to wear Bermuda shorts or a teacher to wear slacks.
Neither do I think that it is proper for a teacher to
have on dresses that have been worn for a period of time,
dirty. I know that teachers and ladies in many instances,
because they get out of cars, they have a run in their
stocking, but I don't think this should happen every day.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
I think that their shoes should be shined sometime if
they are going to have those types of shoes that need to
be shined. I think that their B.O. should be pleasant so
that children can be happy to be around them and if this
is unpleasant the children certainly don’t get any love
and affection out of a teacher that they can’t enjoy
smelling.
Q All right, go ahead and continue.
A 14, "Evidence of a warm and friendly relationship with
your pupils."
Q What were the results of your findings and would you ex
plain this to the Board, what that means in your mind?
A I guess like much of us, it is debatable. On one hand it
may be yes and on the other hand it may be no. If you
are concerned bout the type of thing that is really good
for the children, that is. I recall on one morning about
7:30 Mrs. White had a group of children in her room and
it had been reported to me that there had been modern
dancing, not modern creative dancing, of course, but
modern dancing with the up-beat tempo. That was 7:30 in
the morning. I turned on the intercom and I happened to
have got a good ear of this and I said to her over the
intercom that I was enjoying the music. So she came to
the office and said to me, "Oh, you are, I have spent a
great deal of money buying these type of records and the
children love them." I think she missed my point.
Were you, in fact, enjoying the music or were you trying
to make a point in this way?
I was trying to make a point, very hard, that I was not
enjoying the music, and apparently it was not understood
that way. But I did go back to her on another occasion.
Perhaps at that time I indicated to her that this was not
the type of thing that ought to be going on in school, not
at 7:30 in the morning.
Do other teachers play this type of music?
It was never reported to me and I never heard it over the
intercom, nor did I ever see it.
All right, let me direct your attention back to this forrr
here and ask you to go ahead with that.
Well, in this instance perhaps it would be a friendly
relationship for the kids for them to dance if they
wanted to dance, but it was not that way with me. I did
not think that this would be a warm and friendly relation
ship. I guess there are standards that you have, intan
gible standards that an individual would have to have in
dealing with children. This is a good example, I guess,
of any. Perhaps there are standards that she had that
did not dictate to her that there was nothing wrong with
this. Perhaps these feelings transferred over into other
things.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
Q Go ahead and continue.
A 15, "Indication of classroom enthusiasm." I have that
checked "no" because I did not see enthusiasm.
Q What sort of enthusiasm would you expect to see?
A Well, children excited and eager to learn; children who
want to participate in class discussions and children who
want to talk about their experiences; children who are
happy to be in school and children who are happy to be in
a particular classroom.
Q You did not observe this when you were in the classroom?
A No, I did not observe it then, I did not observe it prior
to then and I did not observe it subsequent to that time
Q All right, then this was not just an isolated instance.
This, in your opinion, was over a period of time?
A Over a period of time and this is still my opinion.
Q All right, continue, please.
A 17, "Evidence of students'progress in fundamental knowlec
skills, abilities, attitudes, and appreciation of reading."
17 I checked "no", because I did not see any evidence of
children's progress in fundamental knowledges and skills
and their understanding and concept and appreciation of
reading. If so, then we would seen an appreciable degree
of students participating in reading activities, going tc
the library, checking out books, and this we did not see
Q All right, go ahead, sir.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
A 18, "The following schedules posted on your bulletin board
in your classrooms! 1, grade level; 2, classroom; 3, musi:
4, P.E.; 5, speech schedule." This was not there and hers
again, this would indicate the fact that the absence of
the schedule - - the absence of these schedules would in
dicate that children who would be scheduled for speech
would not know when they were to go to speech. Neither
would they know when to go to music or to P.E.
Q Did you make an investigation as to trips to the library
and, if so, what were the results of those trips, or that
investigation?
A A few trips had been made to the library. There were son
times in which activities had been scheduled for her clas
to come to the library and, of course, on each occasion
that the library had her scheduled to come she carried
her class along, but there were many other instances tha1
the library had not been used, nor the children in her
classroom had not used the library.
MR. McCLURE: I would like to have this introduced
at this time into evidence.
MR. MARSHALL: May I ask a few questions?
MR. GUARISCO: Yes, sir.
BY MR. .MARSHALL:
Q Is this the original of this record, Mr. Tooks?
A Yes, sir.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
Q And these are your notes?
A Yes, sir.
MR. MARSHALL: No objection.
MR. GUARISCO: All right, this will be County Exhibi :
No. 8 in evidence.
County Exhibit No. 8
received in evidence.
BY MR. McCLURE:
Q Mr. Tooks, after you made this plassroom observation did
you go over this critique with Mrs. White at a subsequent
time?
A Yes, sir, immediately after this visitation I had Mrs. WhL
in the office and we went through this and she concurred
in everything that was there and she indicated to me at
that time that she would try to do all she could to corre:
some of these inefficiencies. The lack of things that I
did not find in the classroom, on one or two occasions,
she would come to me and point out one or two things on
here that she had been doing. This was very sporadic,
though, without any consistency at all.
Q Did you make additional observations of the things that
you pointed out to Mrs. White after the conference?
the
A Yes, sir, none of this sort, none to/scope to which this
one complied. A casual observation or a regular observa
tion by a principal should make, and anyone else would mal
a point of going into the classroom from day to day and a
1
2
3
4
5
6
7
8
9
10
11
12
13
14
IS
16
17
18
19
20
21
22
23
24
25
a result of trying to learn the children, I think after
this visitation I got a pretty good indication of the typ
of things that were going in in the classroom. I might
point out, too, that the form that we had, this was a
form that each teacher had in her hands at least two week|=
prior to the visitation, which would have given each
teacher, I think enough time to prepare herself if she
did not have it already.
Q All right, I direct your attention to on or about
December 11th. Did you have any communication, or what
communication, if any, did you have with .Mrs. White with
regard to her duties as a teacher at Pineview Elementary
School?
A I guess in the course of trying to get adjusted to a
school the first year that a principal does not have time
to talk to teachers each time something comes up that the^
need to be reminded of. I simply followed a pattern that
when teachers reported late for work, rather than having
them to come in and make excuses, or something else that
would be of relative insignificance, to come in and ask
for forgiveness or to be excused, that there is no need
to do this unless there is a consistent pattern and once
I have been able to determine that there has been a con
sistent pattern with somebody, we simply use a letter that
we send out to the teachers, reminding them that they hav»
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
been derelict in this or derelict in that and we wished
that they make note of it and do something about it. This
is the essence of it. On that particular day a letter
was sent to her with regard to not getting her absentee
forms into the office by 9:00 a.m. We had generally
stated that - -
MR. MARSHALL: Mr. Chairman, excuse me. I haven't
objected to anything thus far, but with the pleasure of
the Chairman, Mr. Tooks refers, like he just did, to
"what we do when a person is late". I don’t want to
create any undue impressions about what we are talking
about and, if we can, let him just address himself to
the particular charges made relative to Mrs. White becauss
all of these statements may not be exactly relevant or
do not apply to her.
MR. McCLURE: Mr. Chairman, I think that we will con
nect it up and show where it will apply to Mrs. White.
MR. GUARISCO: Well, I think the point is well taken
so let's stick to the charges and the individual here,
who is the respondent, in these charges- Let's do this
to keep the record straight and also, if we keep going
back and forth, we will be here for two days trying to
get this case tried.
NR. McCLURE: All right, sir, is Mr. Marshall object
ing to this letter? The intent of the letter and the
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
IS
20
21
22
23
24
25
evidence
MR. MARSHALL: No, I'm not talking about the letter,
I'm talking about the response of Mr. Tooks to somebody
being late for work and certain things that might not be
relevant here. I see no connection about somebody being
late here and Mrs. White. I have no objection to the
letter.
MR. GUARISCO: I think the objection is well taken,
so let's stay with the respondent and her activity.
MR. McCLURE: All right, sir, we will certainly do
that.
BY MR. McCLURE:
Q Mr. Tooks did you have an occasion to send Mrs. White a
letter on December 11th?
A Yes, sir, I sent her a letter reminding her that a summar
of her absences had not been coming into the office as I
had requested for it to be.
Q All right, sir, do you have a copy of that letter in your
file?
A Yes, sir.
Q Is this a carbon copy of the letter that was sent to
Mrs. White?
A Yes, sir, this is a copy of the letter that was sent to
Mrs. White.
Q And what date is on that letter?
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
A December 11, 1967.
Q All right, and where has this copy been since you sent it
out?
A In her personnel folder in the school.
Q Has it at any time left the personnel folder?
A No, other than now.
MR. McCLURE: I would like to offer this.
MR. .'MARSHALL: I would like to object to that copy
being offered in evidence because the best evidence is
the original, unless there can be some good showing why
the original is not here.
WITNESS: Well, she has the original.
MR. 'MARSHALL: Also, that this is not a proper - -
the proper foundation has not been laid to introduce the
carbon copy into evidence.
.‘MR. GUARISCO: Mr. Tooks, has this copy been in your
records all this time?
WITNESS: Yes, sir.
MR. GUARISCO: And this is what you wrote in the
normal course of your duties as principal of Pineview
Elementary School?
WITNESS: Yes, sir.
MR. GUARISCO: All right, and where is the original
copy?
WITNESS: The original was mailed to her.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
MR. GUARISCO: All right, I will accept that as
County Exhibit No. 9 in evidence.
County Exhibit No. 9
received in evidenceBY MR. McCLURE:
Q All right, sir, why was it necessary to send Mrs. White
this letter?
A Because she had not done as had been requested of her to
do, to get the summary of absentees into the office,
all right, and you had requested her to do that?
Yes, sir, I had requested all the teachers to do this in
order to do a school-wide count each morning.
Q And what reaction, if any, did (Mrs. White have to this
memorandum?
A None to me personally.
She never responded to that memorandum?
A Other than perhaps to try to see that this was not done
anymore. I never had another occasion to write her a
similar letter.
Q Now, at the end of the '67-*68 school term, did you make
an overall evaluation of Mrs. White's duties as a teacher
at Pineview Elementary School?
A Yes, sir, I did.
Q Is this it here?
A Yes, sir.
•MR. McCLURE: I would like to have this offered for
identification purposes as County Exhibit No. 10.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
Exhibit No. 10.
County Exhibit No. 10
for identification.
Q Would you explain to the Board where this form has been
and the results of your examination in this form?
MR. MARSHALL: Excuse me, but could I see this befoi
he testifies to it?
iMR. McCLURE: Excuse me, yes. (Exhibit supplied.)
MR. MARSHALL: Okay, go ahead.
A This form has been in Mrs. White’s personnel record at
Pineview School and a copy of this has been in the
Superintendent's office in the personnel records there.
Q Would you identify that as to what type form it is?
A This is a form that was developed by a group of Leon
County teachers, principals and administrators to evaluai
the instructural effect of teachers.
Q Does it have a title?
A Yes, it does. The title is “Instructural Effectiveness,
Leon County Evaluation Instrument, Tallahassee, Florida."
Q All right, now is there a name on there as to who the
form was about and who made the evaluation and what year"’
A Yes, sir, the name on here is Alberta White and the
evaluator is James N. Tooks.
Q and is that the form that you made?
A This is the form that I made.
MR. GUARISCO: It will be for identification County
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
A Yes, sir, it is.
Q Would you tell the School Board, in a general summary
way, of how you evaluated Mrs. White during the school
year 1967-68?
A The evaluation scale ranged from below average, 1 to 3;
and average, 4 to 6; superior, 7 to 9. Only in seven
instances did Mrs. White receive a higher evaluation
score than 4.
Q And 4 is what, now?
A Average, low average. The average ranged from 4 to 6.
Over all, on the entire instrument which includes a
professional person, under inter-personal relations,
professional person under organization, she had an averac
of 85% below average on all of the items listed. In man}
instances she received 1 and in some instances she recei\
2.
Q The grade 1 and 2, is that what you're indicating there?
A The grade 1 and 2, receiving the grade 1 for some items
and the grade 2 for other items.
Q And in what category does that fall in?
A Below average.
Q What percentage of below average did she rate?
A On 85% of them.
Q All right, does it show writing in this form?
MR. McCLURE: I would like at this time to introduce
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
that into evidence, if I may.
MR. MARSHALL: Mr. Chairman, I respectfully object to
this being introduced into evidence, No. 1, and No. 2, to
move that all such testimony concerning this record be
stricken. The charges against Mrs. White, specifically
No. 4, relate to competency and it outlines four items.
Certainly this is a complete surprise to her and this is
the first I have heard of it, the first I have seen it,
and it certainly should have been included in No. 4.
Since it is not, it is a complete surprise and certainly
she has not been informed of this and nothing in the recoi
reflects that she has been advised of this and I respect
fully request that it be stricken, or that all testimony
concerning this be stricken.
MR. McCLURE: Mr. Chairman, I think it is pertinent
to show her incompetency, in general, insofar as that is
concerned and this was done by her principal, Mr. Tooks,
and this was done at the direction of the Leon County
school system and I respectfully submit that this is a
proper document for introduction at this time, going to
the general incompetence of - - I believe it touches on
some of the things that were in the specific charges.
MR. GUAR1SCO: I will overrule that objection and
use this to evaluate the overall evidence that you are
going to introduce by testimony from the witness. He sho'
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
N
try to stay within his knowledge of what constitutes in
competency, as set out in charge 4, specifically his
knowledge of what happened and specify those particular
items. I will admit this in evidence as County Exhibit
No. 10.
County Exhibit No. 10
submitted in evidence.
Q Mr. Tooks, in light of the charges that we have preferred
against the respondent here, I direct your attention to
the year 1968-69. I would like for you to give a general
summary of the things that you found to be missing in
Mrs. White’s classroom insofar as her day to day work
with the students and the lesson plans and the activity
plans and the plans that the teacher should have had or
could have had for the students at Pineview Elementary
School.
MR. MARSHALL: Excuse me, but once again, not to
delay matters, but certainly Mr. McClure is being very
skillful and has suggested all sorts of answers in a
compounded question that even I couldn’t follow. Certair
it leaves the field wide open and this man can testify tc
anything he wants to. I would respectfully request of
the Chairman that he not lead- the witness, what should
have been there or what could have been there and was
not there and just let him answer specific questions.
He is the principal and we should limit this to specific
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
questions and answers as to his knowledge.
MR. McCLURE: I will be glad to rephrase that questio
MR. GUARISCO: I will sustain that objection,
Mr. McClure. Ask him specific questions and get specific
answers. Be responsive to the question that he asks and
if we move it in this direction, and a little faster if
we can, I think that we can accomplish what we are here fc
Q Mr. Tooks, I would like for you to tell us the results of
any investigation that you might have made insofar as
lesson plans that Mrs. White had for the school year 1968-
A Would you repeat that question, please?
Q MR. McCLURE: Would you read the question, please?
(QUESTION READ BY REPORTER.)
A I never saw any lesson plans that Mrs. White had for 67-’<
school term or the ,68-,69 school term.
Q All right, did you made an observation of her room and,
if so, what did you find on the atmosphere or the - -
MR. MARSHALL: Once again, just to make the same
objections, the question has been asked and it suggests
the answer and he is looking for a certain answer, and,
once again, I don’t think that is necessary, Mr. Chairman
MR. GUARISCO: I will sustain that objection.
Mr. McClure, you might ask the question as to the particu!.
and
period of time that you want it,/as to the particular tes :
mony that you are seeking.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
MR. McCLURE: All right, sir.
Q I would like to direct your attention to the cleanliness
of Mrs. White's classroom. You have testified before as
to the cleanliness. Did you make any observation as to
that particular item during the year 1968-'69 and, if so,
what were the results of that examination?
A I did not make, if I understand the question, whether or
not I made any examination with regard to the cleanliness
in the room, I observed that the room was disorganized an<
there was a lack of orderliness in the room and I tried t<
do all that I could to see that this particular thing
would not happen.
Q What conferences, if any, did you have on or about
November 12, 1968, with Mrs. White?
A I had a conference with regard to the things in which I
had been dissatisfied with and the things that were - -
the things that the two of us had talked about; that is,
the areas of weaknesses that I felt she possessed and wha';
she should and could do.
Q All right, and what are the areas of weaknesses and what
conferences did you have on those?
A I had a conference with her as a result of the evaluative
instrument and the result of the classroom observation.
In terms of classroom organization and her use of materia..
and resources within the classroom, her interpersonal
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
relationship with the faculty, and her personal appearance
Q All right, who else was there at the conference?
A At this conference a Mrs. Hollis and a Mrs. Manning were
present and I mentioned to Mrs. White at that time that
it would be good for the grade level chairman, Mrs. Hollis
to be present and for the area coordinator, Mrs. Manning,
to be present to offer any suggestions they might have to
work with her and help her in any way possible. She ap
peared to have been quite perturbed and upset over this
after it was all over with and she left the office and
she was very hysterical and upset and she walked into the
teachers' lounge and I heard the noise and I guess every
one else on the school ground heard the noise, too.
Since I represented the threat that had caused this emo
tion, I sent the area coordinator, Mrs. Manning, to tell
her not to go back to the classroom but to come back to
the office and instead she went to the classroom so that
the kids saw her in this condition.
Q All right, where did Mrs. White go, if you know, after
you told her not to go back to the classroom?
A She went back into the classroom and I sent someone down
for her a second time and the person who went returned
with her and I told her that I did not think that she was
in a condition to be with her children and that possibly
it would be best for her to take the rest of the day off
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
and she felt that she was not that bad off, but I felt
that she was.
Q All right, and what directions did you give her, if any?
A I made it very clear to her that after she refused the
first time that I was suggesting very strongly for her to
take the rest of the day off.
Q All right, now I would like to direct you to February of
1969 and ask you if you had a conference with Mrs. White
on her duties as a teacher?
A Yes, sir, this conference with her bordered on the same
area that all the rest of the conferences had bordered on,
We were trying to do the same thing in the same areas.
Q You mean, you had the objections that you had had before
on her organization of the classroom?
A Yes, sir.
Q All right, I would like to direct your attention to on or
about March 25th and ask you what communication, if any,
you sent to Mrs. White?
A Well, I didn’t send it to her, I passed to her across my
desk the statement that I had written. "I am not satisfi?
with your performance as a teacher and suggest that you
look real closely into retirement benefits," and I asked
her whether or not she had any questions.
MR. MARSHALL: May it please the Court, I object to
what was just read being competent because the best evider
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
as to what was being read is the instrument itself and it
has not been offered into evidence and I respectfully re
quest that it be stricken.
MR. McCLURE: All right, I will take that procedure,
Mr. Chairman. I would like to offer this and ask that it
be marked for identification as County Exhibit No. 11.
MR. GUAR1SCO: All right, for identification, No. 11.
County Exhibit No. 11
received for identificat i
Q All right, sir, I hand you this instrument here. Is this
the communication that you read to Mrs. White?
A Yes, sir.
Q Whose handwriting is that in?
A This is in my handwriting.
Q Where has this instrument been since that conference?
A It has been in Mrs. White’s personnel record.
Q And where are those personnel records kept?
A At Pineview School.
MR. MARSHALL: May I just ask one question?
MR. GUARISCO: Certainly.
BY .MR. MARSHALL:
Q Who is the custodian of these records, Mr. Tooks?
A I am,
Q You are the custodian of the records?
A Yes, sir.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
MR. MARSHALL: No objection.
MR. McCLURE: I would like to introduce that into
evidence at this time.
MR. GUARISCO: This will be County Exhibit No. 11
admitted in evidence.
County Exhibit No. 11
admitted in evidence.
Q What communication, if any, did you have with Mrs. White
on or about April 1, 1969?
A I wrote a letter to Mrs. White stating at that time to
her that I was not going to recommend her for - -
Q You wrote her a letter?
A That's right.
Q Is this a carbon copy of the letter that you wrote?
A Yes, sir.
Q All right, sir, and where has this been since you wrote
this to Mrs. White?
A In the personnel records at Pineview of which I am the
custodian.
MR. MARSHALL: We will stipulate as we already have.
MR. McCLURE: I will offer that into evidence.
MR. GUARISCO: Without objection, this will be
County Exhibit No. 12 in evidence.
County Exhibit No. 12
admitted in evidence.
Q What communication did you have with her, if any, on or
about April 24th?
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
A
Q
A
Q
A
Q
A
Q
A
Q
I mailed her a letter.
Is this a copy of that letter?
This is a copy of that letter, yes.
Where has this copy been?
The copy has been - -
MR. MARSHALL: Excuse me, but we have already stipu
lated to this and I have no objection.
MR. GUARISCO: With no objection, this is County
Exhibit No. 13 in evidence.
County Exhibit No. 13
admitted in evidence.
Mr. Tooks, explain this letter and why you wrote it.
Those were the reasons that I felt that I could not reco
mmend her for another year’s employment.
At Pineview?
At Pineview.
All right, I would like to ask you, with regard to studen|t
being sent to your office by Mrs. White, would you tell
the Board what you can recall during the 1968-'69 school
year of any students coming from Mrs. White’s classroom
to your office?
Yes, sir, I could be in my office and the secretary would
come into my office telling me that there were some studeh
out and we had a standing joke that I knew where they werp
coming from before I saw the child.
MR. MARSHALL: Mr. Chairman, I object to that.
53
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
A
Q
A
Q
Q
MR. GUARISCO: Objection sustained. Give us the
actual events and how they happened and when they happened
without editorializing the testimony.
Just tell on how many occasions you recall the students
coming.
Oh, about two or three occassions a week students were
reported to the office for disciplinary reasons.
What type disciplincary reasons were these, Mr. Tooks?
Well, I thought they were petty. It was a matter of
children pushing or shoving in line coming from the rest
room, making noise in the restroom, boys going into girl* ’
restroom and girls going into boys’ restroom.
Is that the type thing that teachers, in your professional
opinion, normally send students down to the principal’s
office for?
No, sir, this was the only teacher that I had this happen
ing with.
One last question, Mr. Tooks. In your professional opinion,
what would you say about Mrs. White's appearance as a
teacher during school hours at Pineview Elementary School
I would say that it was below average.
MR. McCLURE: I have no further questions of Mr. Tooks.
MR. GUARISCO: Mr. Marshall?
CROSS EXAMINATION
BY MR. MARSHALL;
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
Q Mr. Tooks, you say that a teacher who would discipline a
boy for going into the girls’ bathroom, or vice versa, a
girl going to the boys’ bathroom, that this is a petty
disciplinary action on the part of that teacher?
A No, sir, this is not what I said. I did not say that.
Q Then what did you mean by saying that students would come
in for petty reasons and this was one of the reasons why
they came in.
A They were sent in to be disciplined in the office because
they were not disciplined in the classroom for these type
things.
Q And you would say that a person who would send a boy or
a girl in for this reason would also, on the other extrem
play rock and roll music in her classroom, is that right?
A I don't understand your question.
Q The question is that earlier you testified to music over
an intercom?
A I testified to hearing music, yes.
Q Would you say that the same teacher would do both acts;
on the one hand she would send a student in to be disci
plined for this reason and on the other extreme she would
play unacceptable music in her classroom, is that what
you said?
A No, sir, that's not what I said. I didn’t try to relate
one with the other. These happened in isolation and not
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
necessarily this type teacher would do this type thing.
MR. MARSHALL: Mr. Chairman, may I have that first
evaluation report?
MR. GUARISCO: Certainly. (Supplied.) This is Exhib
Q Mr. Tooks, to the best of your recollection, when was thi
sent out to the teachers, and I am speaking now about the
did I understand you to say that this was sent out to the
teachers at Pineview Elementary School?
A Yes, sir.
Q I am asking you now when was that sent out?
A At least two weeks prior to my first visit.
Q Two weeks prior to your first visit to the classroom?
A Yes, sir.
Q How did it go out to the teachers, can you recall?
A In the regular school distribution or memorandums.
Q And that would be what?
A I don't think I understand your question. You mean how
did this particular teacher get the form, is that what
you're asking?
Q That's right.
A Specifically I don't recall how she got it in her hand.
Q So you don’t know whether she had it two weeks prior to
your visiting the classroom or not, do you?
A Well, in most cases more than likely the teacher on the
fifth grade level, the teacher on grade level, talk abou",
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
these type of things, the fifth grade teacher with the
grade level chairman. I'm certain that she had her’s at
least three weeks prior to this because I did not visit
her the first week of visitation. This was done during
the following week.
Q Can you recall when you got together with various teacher
there to plan this schedule?
A We had a steering committee. Each grade level chairman
had a steering committee at that time. The librarian,
the music teacher and the librarian were members of the
steering committee and from the suggestions that they ad
vanced to me these were the things that I compiled here
and I also set some basic individual comments on the
things that they wanted principals to look for when they
walked into the classroom.
Q Now, did I understand you correctly that after the 20th
of November, 1967, you didn’t make another evaluation lik
this one, is that right?
A That's right, like that.
Q And according to this record you found only one item
present in the classroom that you expected to find, is
that right?
A Yes, sir.
Q Now, in the column marked "Unsatisfactory" can you expla:.
why you made no comments if you found this to be such as
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
you say and nothing having been present in the room that
you expected to find, do you know why you made no comments
about it being unsatisfactory on this form?
A No particular reason.
Q Well, a situation this grave you did not feel as though
it was necessary to make a comment, is that right?
A That’s right.
Q Now, you mentioned about the general appearance of Mrs.
White's desk and also the classroom itself. Isn’t it tru
that it is the duty of the custodian to keep the room
clean in terms of the desk and if there is old chalk on
the floor? That's really custodial duties, is it not?
A Yes, sir, to a reasonable and certain extent, yes.
Q And even old candy wrappers on a desk, that, too, is a
custodial duty, is that right?
A Yes, sir, to a certain extent it is.
Q Even glue and water coloring on a desk, that also is a
custodial duty, is that right?
A Yes, sir, to an extent it is.
Q And certainly to the extent that if it had just been
placed there it would be the next morning before it woulc
be cleaned up, is that right?
A I don’t understand your question.
Q I mean if water colors, glue and candy wrappers were plac<
on a desk it would be the following morning or that eveni;
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
IS
20
21
22
23
24
25
sometime before the custodial services could come in and
clean the room properly, is that right?
A Yes, sir.
Q Can you recall the time of day it was back in ’67 when
you visited the classroom?I A I recall this as being in the morning.
Q Just for the purpose of the record, what time does school
begin or did it begin back in November of '67, do you rec
A What time did school begin in ’67?
Q Yes, sir, in the morning, the morning classes.
A Would you restate the question?
Q What time in the morning would classroom hours begin, orI what time would school classes resume?
A 8:30.IQ So then when you mentioned a class being in session at
7:30 in the morning, how was that possible?
A Well, I didn’t say the class was in session at 7:30. I
said children were in the classroom at 7:30 and there was
a modern dance group with the up-beat tempo going on at
that particular time at approximately 7:30 in the mornintI with Mrs. White present at that time.
Q Did you go down into her classroom or did you listen to
this on the intercom?
A I listened to this on the intercom. I had tried to go
down on several occasions and I was detected walking down
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
the hall and it had stopped by the time I got there, so I
turned on the intercom this time.
Q So did you actually see the children in the classroom at
7:30 in the morning or did you hear them?
A I heard them over the intercom dancing and laughing.
Q But you don't really know who it was there, though, do yo.
A I don't believe I understand your question.
Q You didn't see anybody but you're saying now what you heat
A Yes, sir.
Q And tell me, is it the custom of the children to be preser
in the classrooms at 7:30 in the morning?
A At Pineview they are present before 7:00.
Q Before 7:00?
A Yes, sir.
Q I see, but you actually saw no one in that classroom
dancing, is that right?
A No, sir.
Q So can you tell the School Board where you got the impres
sion that modern dancing was being held?
A Impression?
Q Yes, sir.
A It was reported to me from several sources that children
had been dancing in the room. It was reported that mornir
that the children were dancing and I turned on the intercc
and I heard their feet moving about and I heard the music.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
q so what you’re telling us at this point is what somebody
told you, is that right, and not what you observed?
A Which is which, what are you asking me?
Q Well, did you observe anything at all out of the ordinary
on this particular morning at 7:30, did you personally
observe anything?
A No, sir.
Q Now, let's go down your list, if you will, Item No. 15,
which is classroom enthusiasm.
A Yes, sir.
Q Once again tell us just how you made your evaluation.
What went through your mind as to enthusiasm of a child
in the fifth grade?
A You’ll have to repeat your question.
Q Well, tell us the evaluation -- your evaluation was
based on indications of classroom enthusiasm?
A Yes, sir.
Q Of the child?
A Yes, sir.
Q What I want to know is how your base your a/aluation of
enthusiasm of a child in the fifth grade.
A How do I base it?
Q Yes, sir.
A I think that you can base it on the experience factor;
you can observe children over a period of time and you c<
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
see the reaction they have to the types of things that
are going on in the classroom, and it's very obvious when
you walk into a classroom whether or not children are ex
cited or whether or not they are bored to death.
Q Now, did you talk to any of the children to see whether
or not they were enthusiastic, or did you just observe it
A I observed it.
Q But you didn’t ask any questions, is that correct?
A I did ask questions of the children.
Q Can you tell us how long a period of time - - how many
classrooms did you observe during the course of one day
while this was going on?
A On this particular day I believe I spent most of the day.
Some of the other classes I spent the entire day, from
the beginning of classes until the end of the school day
with the children, including going to the lunchroom with
them. I decided that I would take an entire week for a
particular grade and there were three grade levels, or
three classes on each grade level.
Q How long did you remain in Mrs. White’s classroom, if you
can recall?
A About half of the school day.
Q Half of the school day?
A Yes, sir.
Q All right, tell me this: do you take into account the
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
background of the child involved to make your determinate
as to whether or not this child would be responsive to
what we call an educational atmosphere?
A Do I take it into consideration to what?
Q In arriving at your judgment on the ability of a teacher
to even communicate with the student?
A Well, there's no question about it that the two are in
separable .
Q All right, and were you aware of the student's general
background, not every individual student but the general
background of the students in Mrs. White's classroom?
A I think I was as well as I was with any other class, in
terms of the background.
Q That would have been only two months' worth of knowledge,
though, because you had just gotten there?
A No, I started July 1st.
Q So that would be five months?
A Yes, sir.
Q And how many students would you say were in your school
at that time, approximately?
A About 482 children.
Q Can you recall how large a class Mrs. White had at that
point, just in general numbers, if you can recall?
A Yes, sir, it was less than twenty-five.
Q Less than twenty-five?
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
A Yes, sir, and I'm certain less than thirty because classe*
were very, very small.
Q Now, let’s go to several more. Item No. 14, I believe,
which concerns a warm and friendly relationship with the
pupil.
A Yes, sir.
Q Did you talk with any of the students there to determine
this kind of pupil-teacher relationship?
A Well, I had indicated on the evaluation form yes to that
because I felt this was a very debatable sort of thing,
as perhaps some of the others are, but I tried to equate
it as a matter of judgment, as to what’s warm and what's
friendly, in terms of the teacher.
Q Put you did talk to the students about that?
A About what, sir?
Q About the pupil-teacher relationship. Did you inquire,
you know, in general conversation with the pupils whether
or not - -
A You mean when I walked in there at that particular time?
Q During the half day that you were there.
A No, I’m not answering your question, I'm just trying to
understand your question.
Q During the half-day that you were there, did you just
talk to the students to see whether or not there was, in
their minds, a warm and friendly - - you were talking abo
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
variables - - in relationship between the pupil and teach*
A The question was not asked of the students, no.
Q Now, just to clear up the library hours. You did say tha‘
Mrs. White visited the library on each and every occasion
that she was scheduled to visit by the librarian, is that
right?
A I said when certain activities were scheduled, she had
the chance to go. We did not usually schedule library
periods, but when activities had been scheduled, she woul
go.
Q She would go at that time?
A Yes, plus some other occasions, too.
MR. -MARSHALL: Now, may I see County Exhibit No. 107
(Supplied.)
Q Mr. Tooks, this evaluation was made in the school year
1967-'68, is that right?
A Yes, sir.
Q And, likewise, this first evaluation or the visitation
check list that I have here was made in ’67, right?
A Yes, sir.
Q And Mrs. White did teach last year, for the purpose of
the record, is that right?
A Yes, sir.
Q Now, did you go back to make observation of the teacher
when you made this evaluation, Mr. Tooks?
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
A Which one, that one there?
Q Yes, Exhibit 10.
A Yes, sir.
Q You did go back?
A Yes, sir.
Q Also, on the very back of this report there is a section
for remarks, right?
A Yes, sir.
Q And I believe you said that Mrs. White was in the lower -
that 85% of the people were in a higher range or a higher
category than Mrs. White on this, is that right?
A No, sir, I did not say that.
Q What did you say?
A I said she scored below average on 85% of the items
listed on the form.
Q I see, and despite the fact that she made such a low
score, you made no remarks on this form at all?
A Well, I didn’t think it was necessary. It’s obvious,
based on a casual observation of the categories on the
v form itself.
Q Tell me, did you confront Mrs. White with this prior to
today? Did she know about this?
A Yes, sir, every teacher does.
Q She did?
A Yes, sir.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
Q When was she told about the rating that she got on this
form?
A Each teacher was given this in a general meeting and I
went through this with any teacher who had any questions
about it.
Q When was that?
A This was at the end of last school term, the '67-’68 scho
term.
Q And she did teach the following school term?
A Yes, sir.
Q Now, let’s go to November 12, 1968. I believe there was
a conference on that day between yourself and Mrs. Hollis
and Mrs. Manning and Mrs. White, is that right?
A Yes, sir.
Q Can you tell us - - you say that Mrs. White went away,
that when she went away she was upset?
A No, sir, I said that she was hysterical.
Q Hysterical?
A Yes, sir.
Q Can you tell us whether or not anything was said on your
part to cause her to react in this way? Was anything out
of the ordinary or usual said to her?
A Well, possibly so. I’m sure she must have taken it out
of the ordinary in order for her to act out of the ordina
It was not my intent because I specifically stated to her
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
when I asked her to come back to the office, it was not
my intent to evoke those type of emotions.
Q Well, do you know what you said to her to evoke these
emotions?
A No, sir, not to evoke those type of emotions, I don't
know what I said to her, no.
Q Well, can you tell us in general what you said, as best
you can remember? You said there was a conference, right
A Yes, sir.
Q What did you say to her?
A I said to her that I had Mrs. Manning, the area co
ordinator, and Mrs. Hollis, the grade level chairman, in
to her
to talk/about some of the things that I felt I was dis
satisfied with as to her effectiveness instructorily. We
had two evaluation instruments that we had used at that
time. We had this one, which she had seen, and we had
this form which she had seen, and I asked for her, at the
end of the first year, to consider resigning.
Q Do you have that letter or memorandum form when you asked
her to consider resigning then?
A Then?
Q Yes.
A You asked me what I said to her at that time and I'm tell
you what I said.
Q Well, now I’m asking you if you had that in writing? Was
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
it in a memorandum?
A No, this was a conference that I was having with Mrs. Whi
Mrs. Manning and Mrs. Hollis.
Q I realize that we are all human and can’t remember every
single thing that is said but were there any harsh words
on your part that would upset any person in particular?
A No, sir I don’t think so.
Q What happened after she left this conference in this
hysterical mood?
A She walked into the lounge, the teachers' lounge, and I
asked for her to come back to the office.
Q That’s what I want to get to. When she walked into the
lounge, did you go into the lounge yourself?
A No, sir, I said I asked someone to bring her back to the
office.
Q You mentioned noisy, did you actually see Mrs. White, or
this could have been anybody in there in the lounge,
couldn't it?
A I opened my office door and I looked out into the corrido:
and it was Mrs. White screaming real loudly with her arms
protruding out in that manner (demonstrating).
Q Could you look into the lounge from your office?
A She was on her way to the lounge.
Q But in the lounge yourself, you really couldn't see,
could you?
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
A No, but I saw her going to the lounge crying.
Q But not in the lounge itself?
A No, going to the lounge.
Q Did you see - - I suppose it was your aide who went down
to ask Mrs. White to come back. Did you see her actually
go down and see her ask Mrs. White to come back?
A No, sir.
Q So you don't know whether Mrs. White refused to come back
because you don't know whether or not she was even told*
to your own personal knowledge?
A I expect that she was.
Q Tell me, in your experience as a principal, do you some
time confiscate from students or even from teachers any
material that you may not think to be in the best interes
of the school or the teacher or the student?
MR. McCLURE: Your Honor, I would like to object to
the word "confiscate".
MR. GUARISCO: Sustained. I will sustain the objec
tion, but is this responsive to anything in direct? I
don’t recall any testimony like this.
MR. McCLURE: I don't know what he's getting at.
Q Is it your practice to remove articles from either teacheh
or students that you feel are npt in the best interests oJ
the image of the school or the education of the child or
your general school atmosphere? Do you ever do that?
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
Q Right, a knife or such.
A Would I remove it, would I take it off of him physically?
Q Right.
A I would ask him to hand it to me.
Q Right, you would ask him to hand it to you.
A Yes.
Q How about records that you felt were not in the best in
terest, like an out-of-place record in the school atmosph'
would you ask that that be given to you by the teacher or
the student, or anybody?
A An out-of-place record?
Q Yes, a record.
A (No response.)
1R. GUaRISCO: By a record, do you mean a musical
record?
MR. MARSHALL: Yes, sir.
A Would I ask the teacher to give it to me?
Q Yes.
A Well, I haven't. I can't think of any circumstances wher
I would.
Q Even if it were out of place or out of tune with school
atmosphere, you would not ask that it be brought to your
office?
A I have not done so.
A Are you talking about a student with a knife?
1
2
3
4
S
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
records playing, the recordings that were playing in the
classroom?
MR. MARSHALL: Yes, sir, that's exactly right.
MR. GUARISCO: Do you understand the question now?
WITNESS: I understand it now. The question is did
I ask for this to be turned in to the office.
Q Yes, sir.
A No, sir, I didn't, because it was not school property and
in this particular instance she indicated to me that she
had used her personal money to buy it.
Q But other items, and I suppose I must be very broad when
I say, would you consider this record to be not in keepin
with general school practices and general sclool require
ments; did you consider that?
A I thought this particular incident at that particular
time was very unwholesome at 7:30 in the morning.
Q And despite your feelings along those lines you still die
not simply ask her to bring the records into your office1*
A I thought possibly that I could communicate to her so tha
she would understand that I did not think this was appro
priate.
Q Have you heard any such recordings since that date?
A No.
Q So she did respond, didn't she?
MR. GUARISCO: Are you referring specifically to the
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
A Yes.
Q Just like - -
A Well, I don't know whether she responded, really, I just
said I didn't hear any.
Q Right, and sometime silence is a response. Just like the
response she gave to your memorandun about the absentees.
You no longer had any other complaints since that time
you sent the memorandum which is in evidence?
A No, sir, I didn’t say that.
Q What did you say?
A I said that these type memorandums are sent out when ther
is a prolonged consistency of these type of things not
happening. There has not been another instance where
there has been an> inconsistency in her turning in her
absentees. There could have been many occasions where
there might have been one or two or three days, or even
four days, that theyvere not there or that this had oc
curred .
Q But my question is, once you sent out your memorandum - -
A I never had to send another memorandum out, no.
Q So that, too, was a response just like the records, is
that correct?
A Yes.
Q Now, how about when you compared Mrs. White, were you
pairing her against all the other teachers in the Pinevie
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
Elementary School?
A When I compared her?
Q That's right, to make up your evaluation. Did you evalua
her as against everybody else in the school or what was
the general feeling as to what ought to be done in the
school as regards to making this evaluation.
A I looked at Mrs. Y/hite on an individual basis, if this is
your question.
Q Right, but did you compare her to make your evaluation, -
vas she compared with the teachers at Pineview Elementary
School or with teachers throughout the Leon County school
system?
A Neither.
Q Neither?
A No, sir, because I did not compare her.
Q Well, what I'm after is, for example, when you make an
evaluation you just take any number, any random number
here. You say shows independence but not over aggressive
and you rated her below average. That is below average
to whom, nobody in the Leon County school system?
A The score that she received was a below average score bu1
the reason she got a below average score was not on a
comparative basis. It was based on the fact that this i;
the degree to which I felt she had performed in that par
ticular item.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
Q How would she have compared to other teachers in the Pine ■
view Elementary School?
h I never thought about comparing Mrs. White to any other
teacher, or any other teacher with any other teacher.
Q Now, I just have several more questions. I must agree tha
this is a bad report if it's an accurate report of Mrs. Wi
Is it correct that this is an accurate report, we can
generally say that?
A Yes.
Q What is it your practice to do when you have a teacher who
shows up as bad on these evaluation reports as Mrs. White
had? What do you do ordinarily?
A As I did in this particular case and as I have on any
number of other cases, had conferences with her and talked
with her and offered her any help that I can. Also, in
this particular instance I suggested that possibly if she
could look into the benefits of the retirement system.
Q Now, then, it is your practice and habit that when you
find a person scores this low on evaluation reports, to
require her to be dismissed from the school system, is
that right?
A No, sir.
Q Or ask that she would be dismissed - - excuse me, retire.
A She told me she was not ready to retire, when I asked her
this and I told her fine, that I would give her one addit. u
7 b
year to improve in her efficiency as a teacher and that,
at the end of another year, she had not improved that I
would certainly be put in a position where I could not
recommend her and, in the iterim, I tried to do all that
I could to help her.
Then is it your opinion that she is not a fit person to
teach in the Leon County school system?
Yes, sir, it is my opinion that children will suffer as a
result of her being a teacher.
If that record is true, then, why did you then say in the
record book, Minute Book Page 475-476, why did you say th&t
she was also informed during the month of March that if
she could secure placement in another school that you
would gladly agree to the transfer.
Why did I say that?
Yes.
She again told me - - well, I think prior to that time sh
was called into the office and I made a call in her presehce
to the State Retirement Office to send her a financial
analysis of her account and she indicated that, upon re
ceiving this, she would bring it 5n and talk to me about
it and I never heard anything from her with regard to thaft
conference. So I called her in the office one day prilor
to teacher recommendation and I asked her had she been in
receipt cf this information and she said no, she had not,
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
but that she had given some more thought to it and she wa
in no condition to retire. So I explained to her that I
just could not, in any clear conscience, recommend her
for another year at Pineview School.
Q Despite the fact that you thought that she was not a fit
person to teach in the Leon County school system?
A Yes, sir.
Q And despite the fact that she received a very, very low
rating on the evaluation report?
A Yes, sir.
Q In spite of all that, you were still willing that if she
would request transfer you would gladly agree to one?
A Yes, sir. If she could have found a place to work as a
teacher I would not have had any objection to that. My
responsibility is at Pineview.
Q But you wouldn’t mind a bad teacher to go into some
other school.
A That’s why I did what I did in the final analysis.
MR. MARSHALL: I have no further questions.
MR. GUARISCO: Anything further, Mr. McClure?
MR. MeCLURE: Yes, sir, just a few.
REDIRECT EXAMINATION
BY MR. McCLURE:
Q When Mr. Marshall was asking you about did you go down
and take the records or require Mrs. White to bring the
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
records to your office, would it be a normal thing for a
principal to go down and take things from a teacher?
A No, sir.
Q Why would you not take things away from a teacher where
you might take things away from a student?
A I think a teacher, if she is a teacher, has a different
perspective that she is looked upon by people and certain
by students and I don’t think they should be embarrassed.
Q And you feel that a teacher should have more responsibili'
about her personal things than a student?
A Yes, sir, I do.
Q I would like to ask you if you made an evaluation report
of the ’68-'69 school term.
A Yes, sir, I did.
Q Do you have that report with you?
A Yes, sir.
MR. MARSHALL: I object to this because it was
certainly not brought out on anything in my case. He ha<
an opportunity in his case in chief to bring that out and
I don’t know what he's talking about and this is a com
plete surprise.
GUARISCO: All right, I will sustain that objec
tion.
Q Now I believe you testified that you observed that there
were no children’s work in the classroom, Mrs. White’s
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
"16
17
18
19
20
21
22
23
24
25
classroom, when you went to observe there?
A Yes, sir.
Q And I believe you testified, also, that your instructions
were to have the children get involved in the classroom
work?
A Yes, sir.
Q Is this a normal thing for children to get involved in
classroom work around the holiday season?
A Yes, sir, very definitely, because we try to make it
meaningful to children.
MR. MARSHALL: Excuse me, I am going to object to
this because I don’t recall going into anything about any
child's work during a holiday season. This was certainly
not brought out in my case and it is repetitious.
MR. McCLURE: Mr. Chairman, it's not repetitious but
it connects up with his observation of no children’s work
being given at any time that he observed and I believe
that this will pinpoint primary areas and primary times
during the two years where the children's work should be
exhibited.
MR. GUARISCO: I will overrule that objection.
MR. McCLURE: Would you repeat the question, please
Ma’am?
(question and answer read by the rep o r t e r.)
Q Did you observe any children’s classroom work up in the
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
room, Mrs. White's room, during the holiday season?
A No, sir.
Q What did you observe, what type of work?
A I observed a tremendous amount of commercial work, store-
bought material, where if the children had participated
in this they had only participated in possibly putting it
on the board and not actually participating in the drawin
and the writing and the talking about it and discussing
it and the research about the various characters and
various meanings for various holidays; Easter, for instan
or Christmas or Thanksgiving.
Q What about the other holidays during the school year?
A These are really the major holidays, Easter and Christmas
and Thanksgiving. Then you have maybe the Memorial day,
all national holidays which are recognized in one fashion
or the other.
Q Then you didn't observe any children's work during the
school year on the holidays?
A There were more occasions when I observed none than when
I observed some.
Q Mr. Marshall has asked you about what you heard over the
intercom system and the fact that you did not go down to
Mrs. White's room when the records were playing.
A Yes, sir.
Q When you turned on the intercom system, did Mrs. White
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
respond to you and did you recognize her voice?
A Yes, sir.
Q What other voices, if any, did you hear?
A I heard children’s voices laughing and I heard the shuffli
of feet and I said over the intercom, I called out to
Mrs. White and said I was enjoying the music and she said,
"Oh, you are?" and I said, "Yes, I am," and she came down
to the office and she inquired further as to the extent ot
my enjoyment.
Q All right, then Mrs. White was in the room at the time?
A
Q
A
Q
A
Yes, sir.
And you did hear children’s voices in there?
Yes, sir.
Now, one last question about Mr. Marshall’s cross examina
tion on the teachers’ duties as compared to janitorial
duties that might have taken place at the school and may
be required of other people other than teachers. What
would you expect a teacher to do to maintain a clean
classroom during the day?
Well, I would think that a class ought to be free from
distraction so children can at least carry on a simulatio'
of learning experience. This is increasingly difficult
if the room is dirty and there is paper all over the floor
MR. GUARISCO: Mr. McClure, are you about through?
MR. McCLURE: That was my last question, Mr. Chariam
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
MR. GUARISCO: All right, does any of the Board
Members have any questions they would like to ask? If so ,
go ahead, and I have two or three that I would like to
ask to clarify something on the record. In going to the
chart earlier, you indicated where the classroom was lo
cated in the year 1967-’68 and you said that there were
the children's restrooms and two classrooms between her
classroom and your office, is that right?
WITNESS: Yes, sir.
BY MR. GUARISCO:
Q In the year 1968-'69, you had moved Mrs. White closer to
your office so that there were only the restrooms between
her and your office?
A Yes, sir.
Q What was the reason for the move?
A The difference of grades. She was teaching fifth grade
and the next year she was teaching fourth.
Q That was my next question, she was teaching fifth grade
in '67-'68?
A Yes, sir.
Q And was teaching the fourth grade in the '68-'69 year?
A Fourth, yes.
Q Now, on the day that you asked her to take the day off
and you say that she exhibited an unusual behavior when
you asked her to take the day off, did she take the day of
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
A Yes, sir.
Q Who replaced her and what happened to that class?
A We had a floating teacher at Pineview School and this
person was sent to the room on that date, a Mrs. Fannie
Marshall, to take her place.
Q Now, in the school year 1968-'69 she worked after you had
all these conferences with her. Was she, in your opinion
given a second opportunity on a trial basis this particul
year?
A The second year?
Q The 1968-'69 year, her opportunity to come back to work
in that particular year - -
A Yes, sir.
Q - - was that on a trial basis?
A Yes, sir.
Q Did she understand that?
A I told her that.
MR. GUARISCO: Anybody else have any questions?
BY MR. BEhUDOIN:
Q Mr. Tooks, why are there children at Pineview School as
early as 7:00 o’clock in the morning?
A I don’t know, we just have parents who work and they have
to be at work at 8:00 o’clock and we try to have the
building open by 7:00 and some of them are standing on
the outside at 7:00 o'clock in the morning.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
Are provisions made for somebody to supervise these childx
that early in the morning?
I'm usually there at 7:30,and the custodians, but I have
not pulled myself to require my teachers to be there to
supervise that early.
MR. GUARISCO: Any other questions? (No response.)
All right, we will stand adjourned until Saturday morning
at 8:00 o'clock. We're through with Mr. Tooks up to now?
MR. McCLURE: Yes, I have no further questions.
MR. GUARISCO: All right, and you’re going to have
your witnesses here, Mr. Marshall?
MR. MARSHALL: Yes, sir, Mr. Chairman, if I may have
the authority to say to them that this is not an adversar
proceeding ?
MR. GUARISCO: Yes, this is merely - - well, you
might say that it would be for Mrs. White, it would be
doing her a favor, and the School Board won't look on
this thing with any disfavor. She has an opportunity to
bring people in and make her case and she is entitled to
bring anybody in or out of the school system and we cer
tainly won't hold it against anybody.
MR. MARSHALL: Thank you very much.
(THEREUPON HEARING WAS ADJOURNED, TO RECONVENE AT
THE APPOINTED HOUR.)
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
F L O R I D A )
COUNTY OF LEON )
I, CAROL C. CAUSSEAUX, C.S.R., Official Court Reporter
for the Second Judicial Circuit of Florida, and Notary Public,
State of Florida At Large, do hereby certify that I reported
the foregoing hearing in shorthand and by Audograph record
ing at the time and place and in the cause indicated in the
caption; that the same has later been reduced to typewriting
under my direct supervision and that the preceding pages 1
through 83, inclusive, constitute a true and accurate trans
cription of my notes and records of said proceeding had.
WITNESS my hand and official seal at Tallahassee, Leon
County, Florida, this 1969.
CAROL C. CAUSSEAUX
“ otary Public Stile of Florida at la r
•;./ Gwe&y.ion Expires Dec 3, W