Brief Amicus Curiae US Dept of Health and Human Services
Public Court Documents
August 1, 1991
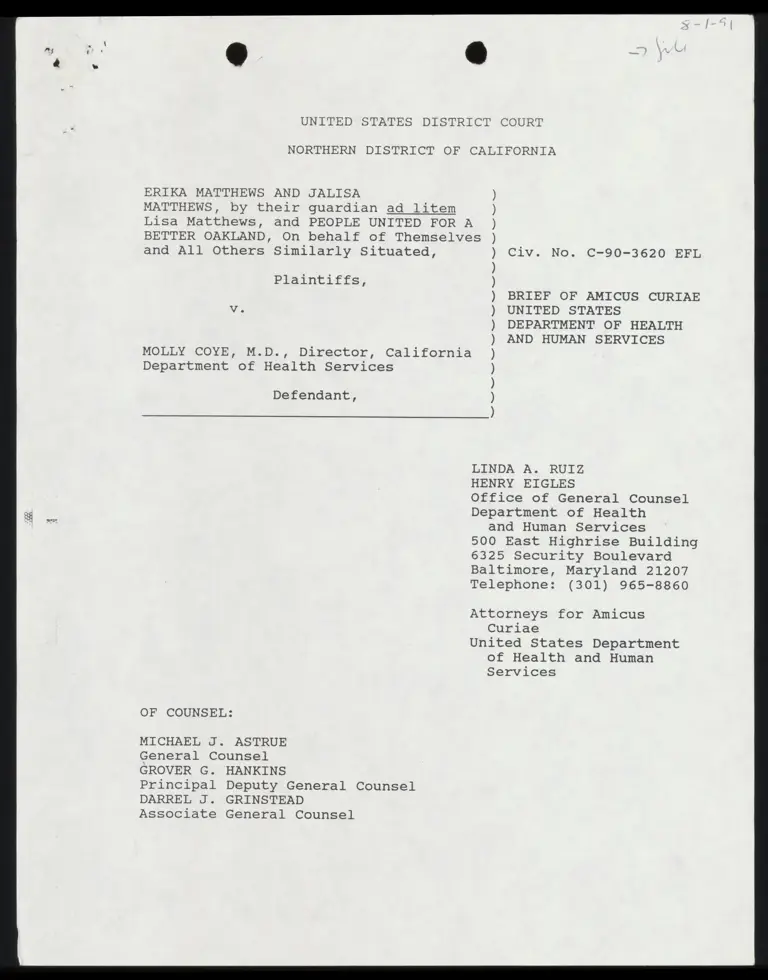
70 pages
Cite this item
-
Case Files, Matthews v. Kizer Hardbacks. Brief Amicus Curiae US Dept of Health and Human Services, 1991. 3abf6683-5c40-f011-b4cb-7c1e5267c7b6. LDF Archives, Thurgood Marshall Institute. https://ldfrecollection.org/archives/archives-search/archives-item/c522eac7-eb73-48b1-9548-ea719fde27c2/brief-amicus-curiae-us-dept-of-health-and-human-services. Accessed February 21, 2026.
Copied!
UNITED STATES DISTRI CT “COURT
NORTHERN DISTRICT OF CALIFORNIA
ERIKA MATTHEWS AND JALISA
MATTHEWS, by their guardian ad litem
Lisa Matthews, and PEOPLE UNITED FOR A
BETTER OAKLAND, On behalf of Themselve
and All Others Similarly Situated,
Plaintiffs,
MOLLY COYE, M.D., Director, California
Department of Health Services
Defendant,
S
Civ. No. C-90-3620 EFL
BRIEF OF AMICUS CURIAE
UNITED STATES
DEPARTMENT OF HEALTH
AND HUMAN SERVICES
N
t
?
N
a
?
Na
st
?
N
a
a
?
e
n
?
a
?
a
?
N
a
s
?
S
t
?
S
t
?
S
u
l
a
?
s
t
?
u
n
?
S
u
s
”
“
a
n
e
”
OF COUNSEL:
MICHAEL J. ASTRUE
General Counsel
GROVER G. HANKINS
Principal Deputy General Counsel
DARREL J. GRINSTEAD
Associate General Counsel
LINDA A. RUIZ
HENRY EIGLES
Office of General Counsel
Department of Health
and Human Services
500 East Highrise Building
6325 Security Boulevard
Baltimore, Maryland 21207
Telephone: (301) 965-8860
Attorneys for Amicus
Curiae
United States Department
of Health and Human
Services
MICHAEL J. ASTRUE
General Counsel
GROVER M. HANKIN
Principal Deputy General Counsel
DARREL J. GRINSTEAD
Associate General Counsel
LINDA A. RUIZ
HENRY EIGLES
Attorneys
Office of General Counsel
Department of Health and Human Services
500 East Highrise Building
6325 Security Boulevard
Baltimore, Maryland 21207
Telephone: (301) 965-8860
Attorneys for Amicus Curiae
United States Department of Health and Human Services
Health Care Financing Administration
UNITED STATES DISTRICT COURT
NORTHERN DISTRICT OF CALIFORNIA
ERIKA MATTHEWS AND JALISA
MATTHEWS, by their guardian ad litem
Lisa Matthews, and PEOPLE UNITED FOR A
BETTER OAKLAND, On behalf of Themselves
and All Others Similarly Situated,
Civ. No. C-90-3620 EFL
Plaintiffs,
BRIEF OF AMICUS CURIAE
UNITED STATES
DEPARTMENT OF HEALTH
AND HUMAN SERVICES
MOLLY COYE, M.D., Director, California
Department of Health Services
Defendant,
N
o
N
t
?
N
e
t
?
N
a
e
?
N
a
f
e
f
N
e
N
f
e
f
a
?
e
l
N
e
N
t
a
’
e
r
INTRODUCTION
This action arises under the Medicaid statute, Title XIX of
the Social Security Act (the Act), and challenges the California
Department of Health Services’ compliance with federal law and
requirements concerning screening and treatment of young
children for lead toxicity under a mandatory part of the
Medicaid program, Early and Periodic Screening, Diagnosis and
A
Treatment (EPSDT). Plaintiffs in this case contend that
federal law requires the California Department of Health
Services to conduct blood lead testing of all Medicaid eligible
children ages 1-5, as part of its EPSDT procedures. The State
maintains that blood lead testing of children ages 1-5 is within
the discretion of the physician. The parties each look to the
State Medicaid Manual, §5123.2D, of the Health Care Financing
Administration (HCFA)' in support of their positions.
The Court issued an order on June 20, 1991 requesting that
HCFA submit an amicus curiae brief addressing the following
questions:
1. On the facts of this case, does the Medicaid Act
require blood lead level testing by the California Department of
Health Services of all children ages one to five eligible under
the Act?
2. On the facts of this case, does the State Medicaid
Manual, §5123.2D indicate that blood lead level testing by the
California Department of Health Services of eligible children
ages one to five is mandatory or discretionary?
This brief is in response to the Court's request.
BACKGROUND
A. The Medicaid Proqran
Title XIX of the Act, commonly known as Medicaid, 42 U.S.C.
§§ 1396 et seq., establishes a jointly funded, cooperative
1
The Secretary of Health and Human Services has delegated
the responsibility of administering the federal aspects of the
Medicaid program to the Administrator of the Health Care
Financing Administration.
g
4 §
27
28
federal-state program designed to "enabl[e] each State, as far
as practicable under the conditions in such State," to furnish
medical assistance to eligible individuals. 42 U.S.C. §1396.
See Atkins v. Rivera, 477 U.S. 154, 165, 106 S. Ct. 2456, 2458
(1986) ; Schweiker v. Hogan, 457 U.S. 569, 571 (1982); Harris v.
McRae, 448 U.S. 297, 301 (1980). While the Medicaid program is
voluntary, states which choose to participate must submit a
state plan that fulfills all requirements imposed by the
Medicaid statute and its implementing regulations. 42 U.S.C.
§1396a. See Schweiker v. Gray Panthers, 453 U.S. 34, 36 =-37
(1981); Harris v. McRae, 448 U.S. at 301. The Secretary is
obligated to approve a state plan that meets all federal >
requirements. 42 U.S.C. §1396a(b).
Upon approval of the state plan, the state becomes entitled
to reimbursement by the federal government, termed "federal
financial participation" (FFP), for a portion of its payments to
hospitals, nursing homes, and other providers furnishing medical
assistance to eligible recipients. 42 U.S.C. §1396b(a). Both
the state plans and the states’ implementation of the plans are
subject to oversight by the Secretary to ensure continued
compliance with the Federal requirements. 42 U.S.C. § 1396c.
State Medicaid programs are administered by the states, not
by the federal government. Within the broad framework of
federal requirements and oversight, the states operate their
individual programs in accordance with state rules and criteria
that vary widely. "As long as a State complies with the
requirements of the Act, it has wide discretion in administering
3
re
its local program." Lewis v. Hegstrom, 767 F.2d 1371, 1373 (Sth
cir 1985).
The Medicaid statute, however, does mandate that, at a
minimum, states provide certain eligible groups with some
specific services. In addition to those services and eligible
groups mandated by the statute, each ‘state decides for its
program, within the constraints imposed by the statute, the
types and range of services it offers, the payment levels for
services, and the groups eligible in addition to those mandated
by the Act. The states also have considerable discretion
concerning the administrative and operating procedures they will
use to implement Federal requirements, although the Secretary
has imposed some requirements on the $iatas through regulations.
HCFA provides instructional and interpretive guidance to
the states through transmittals, issued as part of the State
Medicaid Manual, about how to comply with federal law.
B. The Early and Periodic Screening,
Diagnostic and Treatment Program
The Medicaid statute mandates that Medicaid recipients
under the age of 21 receive EPSDT services. 42 U.S.C. §§
1396a(a) (43) (A) and 1396d(a) (4) (B). Congress amended the
statute to define EPSDT services when it enacted the Omnibus
Reconciliation Act of 1989 (OBRA 89), Pub. L. 101-239, 103 stat.
2106 (December 19, 1989). Section 6403 of OBRA '89 provided the
28 |
definition of EPSDT services by adding §1396d(r) to the statute,
effective April 1, 1990.°
In particular, §1396d(r) defines screening services to
include, at a minimum,
(1) a comprehensive health and developmental
history (including assessment of both physical
mental health development),
(1i) a comprehensive unclothed physical exam,
(iii) appropriate immunizations according to age
and health history,
(iv) laboratory tests (including lead blood level
assessment appropriate for age and risk factors), and
(v) health education (including anticipatory
guidance).
The Secretary's regulation, promulgated before the 1989
amendment and found at 42 C.F.R. §440.40(b), generally defines
EPSDT services, but does not define the services in detail. The
statutory provision and the regulation are interpreted by the
Secretary in the State Medicaid Manual.
° OBRA 89, §6403, now subsection §1396d(r), was derived
from House Bill H.R. 3299, §4213. Conference Report, H.R. 101~-
386, 101 Cong. 1st Sess., p. 453. The Conference Report stated
that the legislation "codifies the current regulations on
minimum components of EPSDT screening and treatment, with minor
changes," and provides that "screenings must include blood
testing when appropriate, as well as health education."
(Emphasis supplied.) The legislative history furnishes no
additional guidance regarding tests or methods for screening.
5
27
28
C. State Medicaid Manual
In April 1990, following enactment of 42 U.S.C. §1396d(r),
HCFA issued Part 5 of the State Medicaid Manual: Early and
Periodic Screening, Diagnosis and Treatment (EPSDT). (Attachment
A hereto.)
At §5110, states are advised, consistent with the statute,
that they must provide for screening, vision, hearing and dental
services at intervals which meet reasonable standards of medical.
and dental practice established after consultation with
recognized medical and dental organizations involved in child
health care. States must also provide for medically necessary
screening, vision, hearing, and dental services regardless of
whether such services coincide with their established
periodicity schedules for these services.
Section 5122 sets out the service requirements for an EPSDT
screening process. The screening process is a medical procedure
to be performed by health professionals (listed with specificity
at §5123.1C), and includes a history of physical and mental
health development, unclothed physical examination,
immunizations, [l]aboratory tests (including lead blood level
assessment appropriate to age and risk), and health education.
Vision, dental, hearing, and other necessary health care
services are included.
Section 5123 discusses screening service delivery and
content and instructs states, at §5123.1, to set standards and
protocols which, at a minimum, meet the standards of 42 U.S.C.
1} §1396d(r) for each component of EPSDT services. The services
“ 2] listed in §5122 are to be part of the screening process.
3 Section 5123.2 sets out the content of screening services
4] to be provided by the states. In particular, at §5123.2D, the
5 Manual addresses laboratory tests that, in the Secretary's view,
6| are appropriate as part of EPSDT screening.
7 D. Appropriate laboratory tests
8 Identify as statewide screening requirements, the
minimum laboratory tests or analyses to be performed
9 by medical providers for particular age or populations
groups. Physicians providing screening/assessment
10 services under the EPSDT program use their medical
Judgment in determining the applicability of the
1 laboratory tests or analyses to be performed. If any
laboratory tests or analyses are medically contra-
12 indicated at the time of the screening/assessment, :
provide them when no longer medically contraindicated.
13 As appropriate, conduct the following laboratory tests.
fi 14 1. Lead toxicity screening
15 Where age and risk factors indicate it is medically
appropriate to perform a blood level assessment, a
16 blood level assessment is mandatory.
17 Screen all Medicaid eligible children ages 1-5 for lead
poisoning. Lead poisoning is defined as an elevated
18 venous blood lead level (i.e., greater than or equal to
25 micrograms per deciliter (ug/dl) with an elevated
19 erythrocyte protoporphyrin (EP) level (greater than or
equal to 35 ug/dl of whole blood). In general use the
20 EP test as the primary screening test. Perform venous
blood lead measurements on children with elevated EP
21 ) levels.
22 Children with lead poisoning require diagnosis and
treatment which includes periodic reevaluation and
23 environmental evaluation to identify the sources of
lead.
24
* * *
25
26
27
28 7
DISCUSSION
The provisions of the State Medicaid Manual restate and
interpret the provisions of §1396d(r). States must set
standards and protocols that, at a minimum, meet statutory
requirements. Among other things, states must provide for EPSDT
screening services. The screening process at the outset
includes taking a history of physical and mental health
development, unclothed physical examination, immunizations,
laboratory tests (including lead blood level assessment
appropriate to age and risk), and health education.
As set out above, § 5123.2D recognizes that, under the
EPSDT program, physicians performing screening services are to -
use their medical judgment in determining the applicability of
the laboratory tests or analysis to be performed. A blood lead
level assessment is mandatory where age and risk factors make it
medically appropriate.
The Manual interprets this statutory requirement by
identifying some specific instances where blood lead assessments
are appropriate. With respect to children ages 1-5, the Manual
provides for certain specific screening measures, including lead
toxicity screening.’ The Manual instructs that, in general, the
> As included in the Manual, the Center for Disease
Control (CDC) has defined lead poisoning as an elevated blood
lead level, which is a level greater than or equal to 25
micrograms per deciliter (ug/dl), accompanied by an elevated
erythrocyte protoporphyrin (EP) level that is greater than or
equal to 35 ug/dl of whole blood.
8
primary screening test is a test to determine elevated
erythrocyte protoporphyrin (EP), which is usually associated
with an elevated blood lead level, referred to as an "EP" test.’
The Manual instructions further provide for venous blood lead
level measurements when elevated EP levels are present.
Thus, the Manual instructs that as part of the medical
screening procedure for children ages 1-5, lead toxicity
screening should be routinely performed via the EP test,
although it may be appropriate not to perform such a test where,
in the physician's "medical judgment," the test is "medically
contraindicated.” That situation should be the exception,
however, rather than the rule, under the Manual's instructions...
The Manual does not provide for venous blood lead level testing
for all children as a screening method, but does instruct that
such testing be done where EP levels are determined to be
elevated.
This Manual instruction is consistent with the Center for
Disease Control's (CDC) Statement on Preventing Lead Poisoning
in Young Children (January, 1985). (Attachment B)> In that
Statement, CDC indicates that "the blood lead levels of U.S.
* The EP test is distinguished from a test for a venous
blood level assessment because an EP test is a test for an
enzyme level that is associated with high blood lead levels. A
venous blood lead level assessment commonly furnishes accurate
results of lead toxicity. (Attachment B, infra, p. 9)
5
CDC personnel have informally advised HCFA that CDC
expects to issue a new Statement in the near future. When CDC
issues its new Statement, HCFA will review its policies
regarding screening procedures by which physicians are to
undertake a blood lead level assessment of Medicaid eligible
children ages 1-5.
children reflect a high degree of environmental contamination by
lead," (Attachment B, p. 9), that lead is most harmful to
children between the ages of 9 months and 6 years, and that,
"ideally, all children in this age group should be screened."
(Attachment B, p. 8) CDC's Statement also recommends that the
"most useful screening tests are those for erythrocyte
protoporphyrin (EP) and blood lead." (Attachment B, P:9). CDC
explained in that Statement that these two tests measure
different aspects of lead toxicity. EP tests measure the level
of EP in the blood, and an elevated level (35 ug/dl or more) may
indicate lead toxicity. Blood lead tests measure lead
absorption, and a confirmed concentration of 25 ug/dl or more
reflects an excessive absorption of lead. (Id.)
CDC further recommended three "feasible" screening
strategies --
1. Screening with EP tests, followed by blood lead
measurements if indicated.
2. Screening with both EP and blood lead tests.
3. Screening with blood lead tests, followed by EP
measurements if indicated.
In particular, CDC recommended EP tests, followed by blood lead
measurements for children with an elevated EP level.
(Attachment B, p. 12)
The State Medicaid Manual instructs states to use, at a
minimum, method 1.
In summary, then, the Manual interprets the statutory
language "appropriate for age and risk factors" to mean that,
with respect to children between the ages of 1-5, the EP test
10
should generally be used as the primary screening device,
followed by venous blood lead assessments where the EP tests
indicate, but acknowledges the physician's discretion not to
perform such tests where medically contraindicated.
OF COUNSEL:
MICHAEL J. ASTRUE
General Counsel
GROVER G. HANKINS
Principal Deputy General Counsel
DARREL J. GRINSTEAD
Associate General Counsel
Respectfully submitted,
2 A
TINTS = RU
HENRY EIGLE
Office of General Counsel
Department of Health
and Human Services
500 East Highrise Building
6325 Security Boulevard
Baltimore, Maryland 21207
Telephone: (301) 965-8860
Attorneys for Amicus
Curiae
United States Department
of Health and Human
Services
1 CERTIFICATE OF SERVICE
2
I HEREBY CERTIFY that on August 1, 1991, a copy of the
3| Brief of Amicus Curiae, United States Department of Health and
Human Services, in Matthews v. Coye (N.D. Cal., Civ. No. C-90-
4| 3620 EFL), was served by United States mail, postage prepaid, to
the following counsel:
5
JOEL R. REYNOLDS, ESQ.
6 JACQUELINE WARREN, ESQ.
NATURAL RESOURCES DEFENSE COUNCIL
7 617 S. Olive Street, Suite 1210
Los Angeles, California 90014
8
JANE PERKINS, ESQ.
9 NATIONAL HEALTH LAW PROGRAM
: 2639 S. La Cienega Boulevard
10 Los Angeles, California 90034
11 SUSAN SPELLETICH, ESQ.
KIM CARD. ESQ.
12 LEGAL AID SOCIETY SOCIETY OF ALAMEDA COUNTY
1440 Broadway, Suite 700
13 Oakland, California 94612
rn
i 14 BILL LANN LEE, ESQ.
KEVIN S. REED, ESQ.
15 NAACP LEGAL DEFENSE AND EDUCATIONAL FUND, INC.
315 W. 9th Street, Suite 208
16 Los Angeles, California 90015
17 MARK D. ROSENBAUM, ESQ.
ACLU FOUNDATION OF SOUTHERN CALIFORNIA
18 633 South Shatto Place
: Los Angeles, California 90005
: 19
hs EDWARD M. CHEN, ESQ.
20 ACLU FOUNDATION OF NORTHERN CALIFORNIA
1663 Mission Street, Suite 460
§ 21 San Francisco, California 94103
22 HARLAN E. VAN WYE, ESQ.
DEPUTY ATTORNEY GENERAL, CALIFORNIA
23 2101 Webster Street, 12th Floor
Oakland, California 94612-3049
24
25
26 :
27
28 32
ATTACHMENT A
. EL TE - . . © sami > =
state medicaid manual o2rimenT ol Heaiin NG Human Services Part § — Early and Periodic Screening, nce rnneng Diagnosis, and Treatment
(EPSDT)
Tranamittat No. 3
Date APRIL 1990
REVISED MATERIAL REVISED PAGES REPLACED PAGES
Table of Contents $-1(1p.) S-1(1p.) Sec. 5010 - 5350 5-3 - 3-55(38 pp.) 5-3 - 5-39(37 pp.)
NEW IMPLEMENTING INSTRUCTIONS—EFFECTIVE DATE: APRIL 1, 1990
This transmittal provides guidance on §56403(a), (d) and (e) of OBRA'8S relating to early and periodic screening, diagnostic and treatment services under Medicaid. The cited subsections amended $§1902(a)(43), 1905(aX4XB) and added 2 new §1905(r) to the Act.
The primary purpose of the amendments is to incorporate into the statute existing regulatory requirements found at 42 CFR 440.40(b) and Part 441, Subpart B. However, §6403 does make certain changes as follows:
° modifies the definition of screening services by including appropriate blood lead level testing and health education;
(] requires distinct periodicity schedules for screening, dental, vision and hearing services and requires medically necessary interperiodic screening services;
° adds a new required service component of "other necessary health care, diagnostic, treatment and other measures described in section 1905(a) to correct or ameliorate defects and physical and mental {llnesses and conditions discovered by the screening services, whether or not such services are covered under the State Medicaid plan.”; and
[] clarifies that nothing In the Medicaid law permits limiting EPSDT providers to those which can furnish all required EPSDT diagnostic or treatment services or as preventing qualified providers which ean provide only one such service from program participation.
Changes have been made throughout the manual to accommodate the modifications discussed above,
In addition, §56403(b) and (C) included requirements relating to annual reporting requirements and development of EPSDT participation goals, respectively. This material will be included in a future manual {ssuance.
HCFA-Pub. 45-8
‘
Attachment A
sd ®
»
\
.
CEAPTER V
EARLY AND PERIODIC SCREENING, DIAGNOSTIC AND TREATMENT
(EPSDT) SERVICES
Introduction
ONE Ws tesa resnsncrisnrnsrennrnsnsnrensos ries osinss Los $5010 $3
Program Requirements and Methods
Basie i TOE SS a $110 §S=8
Inforaing Panilies of EPSDT 5429008 srenansssersrsnecne. $121 $=7 EPSDT Service i bbl LT TRIS aaa G dag $122 $9 Screening Service Delivery and CONLONtLsennesretsessnrene $123 $-10 Minimum Standards and RAV PBN S. ss snes tsrnrscensns $123.1 $=10 Screening Service CODLONLInsnsrsnesesnncersarascessiay $123.2 S-11
: Diagnosis and DEGALRANL. cuuansnrsvcertrincescvronronnrn ss $124 €=17 Periodicity i rated 1 Tre aatheia hah hid $140 S-20 Transportation and Scheduling AIBIILANCR cs set rentecccerss $150 $=-23
Utilization of Providers and Coordination with Related Prograzs
Referral for Services Not Covered Under Medicaid.iceeceee. $210 S-25% Utilization of A Lita at PE SE COS $220 $26 Coordination with Related Agencies and PIOR IANS veccereen $230 S-27 Relations With State Maternal and Child Bealth i
PLOGEARS. torerasansrervacevetrvons vovesnererssnss $230.1 S-28 Other Agencies and PIOGIaNS.cetsnersneenesrscecsorvons $230.2 $=-30
F Continuing CAIBessscerrriessrerssntecroneenrnsoncosree ons $240 $=313 {
R pis
Administration
Program Yonitoring, Planning, and BVA luAL iO Mescrnnseceens $310 5-38 Inforaation Needs and ud aah ts TEE Dy VRURLI NE SR Behe $320 S-38 Mainistrative Information Requirements. ceeeececceccns $320.1 5-38 Records or Information on Services and Recipients..... $320.2 S-38 { 180 11m0800000r0u0nsaencnsesncerrvrnersens rion anetynn $330 $=-45 | Re 1EDUPIRMONTcseaannsessetasstsnsrinnscersormrmsnn rss $340 S-51 ro CONIA EAdILY ss suenrssncnssssectenoncnces rene ersnins $350 $=55
Rev. 3
5-1
EARLY AND PERIODIC SCREENING, 04-50 DIAGNOSTIC AND TREATMENT SERVICES $010
4 : Introduction
$010. OVERVIEW
A. Ear]
and Treatment Benefit. —Early ang
periodic screen agnostic and treatment services (EPSDT) is a required service under
the Medicaid program for categorically needy individuals under ge 21. The EPSDT
benefit is optional for the medically needy population. However, if the EPSDT benefit is
elected for the medically needy population, the EPSDT benefit must be made available to
B. A Comprehensive Child Health Program.--The EPSDT program consists of two,
mutually supportive, operational components; : % : :
© assuring the availability and accessibility of required health care resources
\
and
© helping Medicaid reciplents and thelr parents or guardians effectively use
them,
These components enable Medicaid agencies to manage a comprehensive child health
program of prevention and treatm ent, to systematically:
. © Seek out eligibles and inform ‘them of the benefits of prevention and the
health services and assistance available,
© Help them and their familles use health resources, Including thelr own
talents and knowledge, effectively and efficiently,
© Assess the child's health needs through initial and periodic examinations and
evaluation, and
© Asswe that health problems found are diagnosed and treated early, before
they become more complex and their treatment more costly, Although "case
management” does not appear in the statutory provisions pertaining to the EPSDT benefit,
the concept has been recognized as a means of increasing program efficiency and
effectiveness by assuring that needed services are provided timely and efficiently, and
that duplicated and unnecessary services are avoided,
re C. Administration.--You have the flexibility within the Federal statute and
regulations to design an EPSDT Program that meets the health needs of recipients within
your jurisdiction. Title XIX establishes the framework, containing standards and
|_fequirements you must meet,
Rev. 3 : : 5-3
*® EARLY AND PERIODIC SCK.eNING, 0490 DIAGNOSTIC AND TREATMENT SERVICES
Program Requirements and Methods
$110. BASIC REQUIREMENTS
[oBRa 89 amended §51902(aX43) and 1305(aX4XB) and created §$1905(r) of the Social
Security Act (the Act) which set forth the basic requirements for the Program. Under the
EPSDT benefit, you must provide for screening, vision, hearing and dental services at
intervals which meet Feasonable standards of medical and denta) practice established
after consultation with tecognized medical and dents) organizations involved in child
health care. You must also provide for medically Necessary screening, vision, hearing and
dental services regardless of whether such services coincide with Jour established
periodicity schedules for these services, Additionally, the Act requires that any service
which you are permitted to cover under Medicaid that Is necessary to treat or ameliorate
a defect, physical and mental illness, or a condit] n Identified by a screen, must be
provided to EPSDT participants regardless of whether the service or item fis Sitarvis
The statute provides an exception to comparability for EPSDT services, Under this .
exception, the amount, duration and scope of the services provided under the EPSDT
Program are not required to be provided to other program eligibles or outside of the
EPSDT benefit. Services under EPSDT must be sufficient in amount, duration, or scope to
reasonably achieve their purpose. The amount, duration, or scope of EPSDT services to
recipients may not be denied arbitrarily or reduced solely because of the diagnosis, type
of illness, or condition, Appropriate limits may be placed on EPSDT services based on
medical necessity,
. Rev. 3
3-3
EARLY AND PERIODIC SCR_.NING,
0490
DIAGNOSTIC AND TREATMENT SERVICES $121 $121. INFORMING FAMILIES OF Epspr SERVICES
A. Cenera) Information.—Section 1902(a)43) of the Act requires that the State plan
provide for infor ming all eligible Medicaid recipients under 23 about EPSDT, The intent
of the statute is to allow flexibility of Process as long as the Outcome is effective and is
achieved in o timely manner, generally within 60 days,
: The informing process, which may begin at the intake Interview, extends to no later than
60 days following the date of a family's op individual's initia] eligibility determination, op
of a determination efter a period of ineligibility, A combination of face-to-face, oral,
and written informing activities {s most productive, al
The regulation requires you to assure that your combination of written and oral Inform
methods are effective. Use methods of communication that recipients ean clearly and
easily understand to ensure that they have the information they need to utilize services to
which. they are entitled, HCFA considers "oral" methods to inciude face-to-face
informing by eligibility case workers, health aides and providers as well os public service -
i : It is effective and efficlent to target specific Informing activities to particular "at risk®
groups. For example, mothers with babies to be added to assistance units, familes with
infants, or adolescents, first time eligibles, and those not using the program for- over
2 years might benefit most from oral methods, We nag : B. Individuals to Be Informed.= - - Tare EE
ne ALLA 2°
3
; : Fi
© Inform all Medicald-eligible families about the EPSDT program.
© Inform newly eligible families, either determined eligible tor the first time, for at least 1 year. Use a combination of written and oral methods, generally within
80 days following the date of the eligibility determination, .
Families that go on and off the rolls do not have to be Informed more than once in %
12-month period.
;
© There Is no distinction between title IV-E foster care families and others,
For title IV-E foster care individuals, informing must be with the unit receiving the cash
assistance (e.g., foster parent, administrator of institution), Many title IV-E foster care
individuals are rotated frequently through foster care homes or institutions, and, in some
cases, there are changes in foster parents, institution administrators, or responsible
social workers, It is to the individual's benefit that informing de done initially, not only
with the unit receiving the cash assistance, but with parties who have legal authority over
or custody of the individual
Rev, 3
3
*
$-7
® EARLY AND PERIODIC SCREEN] ’ $121 (Cont.) DIAGNOSTIC AND TREATMENT SERVICES 04.90
tosm——
Informing about EPSDT encourages appropriate planning for the health ne i When informing foster parents or administrators of 5 Sind i bintadiucg vn foster care individuals in thelr care. Inform institutions or homes having a number of ( individuals annually or more often when the need arises, such as when changes in : administrators, social workers or foster parents ocowr. If an individual is rotated through foster care homes, inform the responsible parties at the homes, unless previously done within the year for other foster care individuals. Annual contact establishes a relationship with the facilities to resolve any problems arising.
o Inform a Medicaid eligible pregnant woman about the availability of EPSDT services for children under age 21 (including children eligible as newborns). A Medicaid eligible woman's positive response to an offer of EPSDT services during her pregnancy, which is medically confirmed, constitutes a request for EPSDT services for the child at birth. For a child eligible at birth (i.e., as a newborn of a woman who is eligible for and receiving Medicaid), the request for EPSDT services is effective with the birth of the child. The parent or guardian of an infant who is not deemed eligible at birth as a [_newborn must be informed at the time the infant's eligibility is determined.
C. Content and Methods.—
© Use clear and nontechnical language, provide a combination of oral and written methods designed to inform all eligible individuals (or their familles) effectively describing what services are available under the EPSDT program; the benefits of preventive health care, where the services are available, how to obtain them; and that necessary transportation and scheduling assistance is available.
Fn Mntorm eligible individuals whether services are provided without cost. States may im y impose premiums for Medicaid on individuals (i.e., pregnant women and infants) whose family income exceeds 150 percent of Federal poverty levels as described In §3571 and, for medically needy participants, may impose enrollment fees, premiums or similar charges [_for participation in the medically needy program.
O
n
© Provide assurance that processes are in place to effectively inform individuals, generally within 60 days of the individual's Medicaid eligibility deter mination and, if no one eligible in the family has utilized EPSDT services, annually thereafter,
o Utilize accepted methods for informing persons who are literate, blind, deaf, or cannot understand the English language. Por assistance in developing appropriate bos procedures, contact agencies with established procedures for working with such individuals, e.g., State or local education departments, employment secwrity offices,
handicapped programs. :
© You have the flexibility to determine how infec mation may be given most
appropriately while assuring that every EPSDT eligible receives the basic information
necessary to gain access to EPSDT services.
$-8 Rev. 3
UNITED STATES DISTRI CT COURT
NORTHERN DISTRICT OF CALIFORNIA
ERIKA MATTHEWS AND JALISA
MATTHEWS, by their guardian ad litem
Lisa Matthews, and PEOPLE UNITED FOR A
BETTER OAKLAND, On behalf of Themselve
and All Others Similarly Situated,
Plaintiffs,
MOLLY COYE, M.D., Director, California
Department of Health Services
Defendant,
S
Civ. No. C-90-3620 EFL
BRIEF OF AMICUS CURIAE
UNITED STATES
DEPARTMENT OF HEALTH
AND HUMAN SERVICES
N
t
?
N
a
l
N
a
s
t
?
N
a
s
i
?
a
i
N
a
a
e
?
S
i
t
?
a
n
?
a
n
?
S
l
i
?
a
?
a
a
t
’
“
u
n
?
OF COUNSEL:
MICHAEL J. ASTRUE
General Counsel
GROVER G. HANKINS
Principal Deputy General Counsel
DARREL J. GRINSTEAD
Associate General Counsel
LINDA A. RUIZ
HENRY EIGLES
Office of General Counsel
Department of Health
and Human Services
500 East Highrise Building
6325 Security Boulevard
Baltimore, Maryland 21207
Telephone: (301) 965-8860
Attorneys for Amicus
Curiae
United States Department
of Health and Human
Services
EARLY AND PERIODIC SCREENING, 0490 DIAGNOSTIC AND TREATMENT SERVICES 3122
JPA
The EPSDT benefit, in accordance with 51905(r) of the Act, must include the forth below. The frequency with which the services must be provided fs §5140.
EPSDT SERVICE REQUIREMENTS
services set
discussed in
A. Screening Services.—Screening services include all of the following services:
0 A comprehensive health and developmental history (including assessment of both physical and mental health development); ;
© A comprehensive unclothed physical exam;
© Appropriate Im munizations according to age and health history; .
© Laboratory tests (including lead blood jevel ‘assessment appropriate Shes and risk); and ; Ean idly hi |
© Health education (Including anticipatory guidance).
Immunizations which may be appropriate based on age and health history but which are medically contraindicated at the time of the screening may be rescheduled at an
appropriate time.
~ B. Vision Services.—At a minimum, inelude diagnosis and treatment for defects in vision, Including eyeglasses. . 3 CRM
£ C. Dental Services.—At a minimum, fnelude relief of pain and infections, - restoration of teeth and maintenance of dental health, Dental Services may not be limited to emergency services.
° '.
D. Bearing Services.—At a minimum, include diagnosis and treatment for defects in hearing, including hearing aids.
E. Other Necessary Health Care.~Other necessary health care, diagnostic services, treatment and other measwres described in 51905(a) of the Act to correct or ameliorate be defects, and physical and mental [llnesses and conditions discovered by the screening services,
; i PF. Limitation of Services. ~The services available in subsection E are not limited to i those included in your State plan.
© Under subsection E, the services must be "necessary . . . to correct or | ascents defects and physical or mental Qlnesses of conditions . ..." and the defects,
Rev. 3
8-9
yr
® EARLY AND PERIODIC a, : $123 DIAGNOSTIC AND TREATMENT SEh vICES 01-90
—
Lllnesses and conditions must have been discovered or shown to have increased in severity Dy the screening services. You make the determination as to whether the service is Necessary. You are not required to provide any items or services which you determine are not safe and effective or which are considered experimental.
[= © 42 CFR 440.230 allows you to establish the amount, duration and scope of services provided under the EPSDT benefit, Any limitations imposed must be reasonable and services must be sufficient to achieve their purpose (within the context of serving the needs of individuals under age 21). You may define the service as long as the definition comports with the requirements of the statute in that all services included in §1905(a) of the Act that are medically necessary to ameliorate or correct defects and physical or mental illnesses and conditions discovered by the screening services are provided.
© All services must be provided in accordance with both §1905(a) of the Act - and any State laws of general applicability that govern the provision of health services. Home and community based services which are authorized by §1915(¢c) of the Act are not included among the other health care under subsection E because these services are not included under §1905(a) of the Act.
5123. SCREENING SERVICE DELIVERY AND CONTENT
$123.1 Minimum Standards and Requirements. —
A. State Standards.--Set standards and protocols which, at a minimum, meet the standards of $§1905(r) of the Act for each component of the EPSDT services, and maintain written evidence of them. The standards must provide for services at intervals which meet reasonable standards of medical and dental practice and be established after consultation with recognized medical and dental organizations involved in ehild health care, The standards must also provide for EPSDT services at other intervals, indicated as medically necessary, to determine the existence of certain physical or mental illnesses or conditions. The intervals at which services must be made available are discussed in §5140.
B. Services,—
© Provide an eligidle individual requesting EPSDT services required screening services listed in §5122. This initial examination(s) may be requested at any time, and must be provided without regard to whether the individual's age coincides with the established periodicity schedule. Sound medical practice requires that when children first enter the EPSDT program you encourage and promote that they receive the full panoply 1. screening services available under EPSDT.
© It is desirable that a parent or other responsible adult accompany the child to the examination. When this is not possible or practical, arrange for a followup worker, social worker, health aide, or neighborhood worker to discuss the results in a visit to the home or in contacts with the family elsewhere.
$-10
EARLY AND PERIODIC SCREL SG, . DIAGNOSTIC AND TREATMENT SERVICES $123.2
———
C. Who Screens/Assesses?—
© Examinations are performed by, or under the supervision of, a certified Medicaid physician, dentist, or other provider qualified under State law to furnish primary medical and health services. These services may be provided within State and local health departments, school health programs, programs for children with special health needs Maternity and Infant Care projects, Children and Youth programs, Head Start programs, community health centers, medical/dental schools, prepaid health care plans, a private practitioner and any other licensed practitioners in a variety of arrangements,
© The use of all types of providers Is encouraged. Recipients should have the greatest possible range and freedom of choice. It is required, in the case of title Y, and encouraged, in the case of the primary care projects (I.e., community health centers), that maximum use be made of these providers. Day care centers may provide sites for examination activities. Encourage cooperation when and where other broad-based assessment programs are unavailable, ™ i+. =. ie vz
Fo © Providers may not be limited to those which have an exclusive contract to perform all EPSDT services. Service providers may not be limited to either the private or puble sector or because the provider may not offer all EPSDT services or because it Lofters only one service. Assure maximum utilization of existing resources to more e{fectively administer and deliver services, -
Medicaid providers who offer EPSDT examination services must assure that the services they provide meet the agency's minimum standards for those services In order to be reimbursed at the level established for EPSDT services. - :
To
5123.3 Screening Service Content,— ~~. ‘ton a a
A. Com rehensive Health and Developmental History ‘Information from the parent or other responsible adult who is familiar with the child's history and include an assessment of both physical and mental health development, , Coupled with the | physical examination, this Includes: - hi.” at RT ere a i 2 .
1. Developmental Assessment.—This includes 8 range of activities to determine whether an individual's developmental processes fall within a normal range of achievement according to age group and cultural background, Screening foe developmental assessment is a part of every routine initial and periodic examination,
J
* EARLY AND PERIODIC SCREENI.
$123.2(Cont.) DIAGNOSTIC AND TREATMENT SERVICES 04 4p
Developmental assessment is also carried out by professionals to whom children are referred for structured tests and instruments after potentia] problems have been identified by the screening process. You may build the two aspects into the program so that fewer referrals are made for additional developmental assessment,
a. Approach.—There is no universal list of the dimensions of development for the different age ranges of childhood and adolescence. In younger children, assess at least the following elements: :
© Gross motor development, focusing on strength, balance, locomotion;
© Fine motor development, focusing on eye-hand coordination;
© Communication skills or language development, focusing on expression, comprehension, and speech articulation;
© Self-help and self-care skills;
© Social-emotional development, focusing on the ability to engage in social interaction with other children, adolescents, parents, and other adults; and
© Cognitive skills, focusing on problem solving or reasoning,
As the child grows through school age, focus the program on visual-motor integration, visua)-spacial organization, visual sequential“ memory, attention skills auditory processing skills, and auditory sequential memory. Most school systems provide routines and resources for developmental screening,
For adolescents, the orientation should encompass such areas of special concern as potential presence of learning disabilities, peer relations, psychological/psychiatrie problems, and vocational skills,
b. Procedures.—No list of specified tests and instruments is prescribed for identifying developmental problems because of the large number of such instruments, development of new approaches, the number of children and the complexity of developmental problems which occur, and to avoid any connotation that only certain tests or instruments satisfy Federal requirements. However, the following principles must be consider od:
© Acquire information on the child's usual functioning, as reported by the child, parent, teacher, health professional, or other familiar person.
$-12 : : Rev, 3
o
n
i EARLY AND vesioti Wes ING,
0490 DIAGNOSTIC AND TREATMENT LcRVICES
5123.2(Cont.)
© In- screening .for developmental assessment, the examiner incorporates and reviews this information in conjunction with other information gathered during the physical examination and makes an objective professional judgement whether the child is within the expected ranges. Review. developmental progress, not in isolation,
but as 8 component of overall health and well-being, given the child's age and culture,
© Developmental assessment should de culturally sensitive and valid. Potential problems should not be dismissed or excused improperly on grounds of culturally
appropriate behavior, Do not initiate referrals improperly for factors associated with
cultural heritage.
© Programs should not result in a label or premature diagnosis of a
child. Providers should report only that a condition was referred or that a type of diagnostic or treatment service Is needed. Results of {nitial screening should not be
accepted as conclusions and do not represent a diagnosis,
© Refer to appropriate child development resources for additional
assessment, diagnosis, treatment or follow-up when concerns or Questions remain after
the screening process.
2. Assessment of Nutritional Status.—This is accomplished in the base
examination throughs ;
© Questions about dietary practices to identify unusual eating habits (such
as pica or extended use of bottle feedings) or diets which are deficient or excessive in one
or more nutrients.
© A complete physical examination including an oral dental examination.
Pay special attention to such general features as pallor, apathy and Irritability.
© Accurate measurements of height and weight are among the most
important indices of nutritional status,
© A laboratory test to screen for iron deficiency. HCFA and PHS
recommend that the erythrocyte protoporphyrin (EP) test be utilized ‘when possible for
children ages 1-5. It is a simple, cost-effective tool for screening for iron deficiency
Where the EP test is not available, use hemoglobin concentration or hematoerit.
oc I feasible, screen children over 1 year of age for serum cholesterol
determination, especially those with a family history of heart disease and/or hypertension
and stroke.
<
Rev, 3 . $-13
3 @® ciriv ano rrrionic scl © 3123.2(Cont.) WIAGNOSTIC AND TREATMENT SER ._ES 05-90
If information suggests dietary inadequacy, obesity or other nutritional problems,
assessment is indicated, including: further
© Family, sociceconomic Of any community factors,
© Determining Quality and Quantity of individual diets (e.g., dietary
intake, food acceptance, meal patterns, methods of food preparation and preservation,
and utilization of food assistance programs), :
© Further physical and laboratory examinations, and
© Preventive, Treatment and follow-up services, including dietary
counseling and nutrition education.
B. Comprehensive Unclothed Physical Examination:~Includes the following:
1. Physical Growth.—Record and compare the child's height and weight with those considered normal Jor that age. (In the first year of life head circumference measurements are important), Use a BTaphic recording sheet to chart height and weight over time.
2. Unclothed Physical Ins ction.—~Check the general appearance of the child to determine overall health status, This process can pick up obvious physical defects, including otthopedie disorders, hernia, skin disease, and genital abnormalities. Physical inspection includes an examination of all organ systems such as pulmonary, cardiae, and gastrointestinal, :
4 Cc, Appropriate Immunizations. —Assess whether the child has been immunized (
against diphtheria, pertussis, tetanus, polio, measles, Fubella, and mumps, and whether k
booster shots are needed. The child's immunization record should be available to the provider. When an immunization or an updating is medically Recessary and appropriate, provide it and so inform the child's health supervision provider.
Provide immunizations as recommended by the American Academy of Pediatrics (AAP) and/or local health departments.
D. A iate Laborator Tests.—Identify as statewide screening requirements, the minimum laboratory tests or analyses to be performed by medical providers foe particular age or population goups. Physicians providing screening/assessment services under the EPSDT program use their medical judgement in determining the applicability of the laboratory tests or analyses to be performed. If any laboratory tests or analyses are
fo 1. Lead Toxdeity Screening —Where age and risk factors indicate it is medically appropriate fo perioem a blood level assessment, a blood level assessment is |_mandatory.
$-14
Rev. 3
EARLY AND PERIODIC SCREENING, 07-90 DIAGNOSTIC AND TREATMENT SERVICES '5123.2(Cont.)
I Sergen all Medicaid eligible children ages 1-5 for lead poisoning, Lead poisoning is defined as an elevated venous blood lead level (i.e., greater than or equal to 25 micrograms per deciliter (ug/dl) with an elevated erythrocyte protoporphyrin (CP) level (greater than or equal to 35 ug/dl of whole blood). In general, use the EP test as the primary screening test. Perform venous blood lead measurements on children with elevated EP levels.
Children with lead poisoning require diagnosis and treatment which includes periodic re- evaluation and environmental evaluation to identify the sources of lead. . Co MN Wc ph
8
2. Anemia Test.—~The most easily administered test for anemls” hy: a microhematocrit determination from venous blood or a fingerstick., ii et bo CaS o
N
3. Sickle Cell Test.—Diagnosis for sickle cell trait may be done with sickle cell preparation or 8 hemoglobin solubility test, If a child has been properly tested once for sickle cell disease, the test need not be repeated.
he 4. Tuberculin Test.—Cive a tuberculin test to every child who has not received one within a year,
io
-
x S. Others.—In addition to the tests above, there are several other tests to consider. eir appropriateness are determined by an individuals age, sex, health history, clinical symptoms and exposure to disease, These include a urine screening, pinworm slide, urine culture (for girls), serological test, drug dependency screening, - stool specimen for parasites, ova, blood, and HIV screening. ee
development and to provide information about the benefits of healthy lifestyles and practices as well as accident and disease prevention,
F. Vision and Hearing Screens.—Vision and hearing services are subject to their own periodicity schedules (as described in §5140). However, where the periodicity schedules coincide with the schedule for screening services (defined in §5122 A), you may include vision and hearing screens as a part of the required minimum screening services,
2. Appropriate Hearing Screen.—Administer an age-appropriate hearing assessment. Obtain consultation and suitable procedures for screening and methods of administering them from audiologists, or from State health or education departments.
Rev, 4&
35-15%
i
L
- EARLY AND PERIODIC SCREENING, :
$123.2(Cont.) DIAGNOSTIC AND TREATMENT SERVICES i 07-90
. are needed at an earlier age, provide the needed dental services,
G. Dental Screening Services.——Although an oral screening may be part of a physical examination, it does not substitute for examination through direct referral to a dentist. A direct dental referral is required for every child in accordance with your periodicity schedule and at other intervals as medically necessary, Prior to enactment of OBRA 89, HCFA in consultation with the American Dental Association, the American Academy of Pediatrics and the American Academy of Family Practice, among other organizations, required direct referral to a dentist beginning at age 3 or an earlier age If determined medically necessary. The law as amended by OBRA 89 requires that dental services (Including initial direct referral to a dentist) conform to your periodicity schedule which must be established after consultation with recognized dental organizations involved In child health care.
~\
© Especially in older children, the periodi~!ty schedule for dental examinations is not governed by the schedule for medical examinations. Dental examinations of older children should occur with greater frequency than is the case with physical examinations, The referral must be for an encounter with a dentist, or a professional dental hygienist under the supervision of a dentist, for diagnosis and treatment. However, where any screening, even as early as the neonatal examination, indicates that dental services
ov"
© The requirement of a direct referral to a dentist can be met in settings other than a dentist's office. The necessary el ment is that the child be examined by a dentist or other dental professional under the supervision of a dentist. In an ares where dentists are scarce or not easy to reach, dental examinations in a clinie or group setting may make the service more appealing to recipients while meeting the dental periodicity schedule. If continuing care providers have dentists on their staff, the direct referral to a dentist requirement is met. Dental paraprofessionals under direct supervision of a dentist may perform routine services when in compliance with State practice acts,
.
© Determine whether the screening provider or the agency does the direct referral to a dentist. You are ultimately responsible for assuring that the direct referral is made and that the child gets to the dentist's office in a timely manner.
5-18
Rev. &
ATTACHMENT B
99-2230
A STATEMENT BY THE
CENTERS FOR DISEASE CONTROL
JANUARY 1985
Reprinted July 1985
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
PUBLIC HEALTH SERVICE
CENTERS FOR DISEASE CONTROL
CENTER FOR ENVIRONMENTAL HEALTH
CHRONIC DISEASES DIVISION
ATLANTA, GEORGIA 30333
Attachment B
Use of trade names is for identification only and does not constitute endorsement by the Public
Health Service or by the U.S. Department of Health and Human Services.
Preface
This second revision of the Centers for Disease Control's (CDC's) statement, Preventing Lead
Poisoning in Young Children, is more comprehensive than the two previous versions. With help
from members of CDC's Ad Hoc Advisory Committee on Childhood Lead Poisoning Prevention
and other expert consultants, we have considered new research findings on lead toxicity, redefined
lead poisoning at a lower blood lead level, and updated our recommendations on lead-based paint
abatement. In addition, a recent article on a new treatment scheme for lead poisoning (symptomal-
ic and asymptomatic) is included.
The precise threshold for the harmful effects of lead on the central nervous system is nol
known. In the meantime, we have used our best judgment as to what levels of lead are toxic and
whal practical interventions will lower blood lead levels. As public health officials. our duty is to
protect children as best we can—given the limitations of science and the need to make decisions
without perfect data. This is the Department of Health and Human Services’ major policy statement
on the issue.
The progressive removal of lead from leaded gasoline is lowering average blood lead levels in
the United States, but the problem of the major source of high blood lead levels in our.
country—millions of old housing units painted with lead-based paint—is largely unsolved. Until
betler approaches and more resources are available for removing lead paint hazards in older dwell-
ings where children live, lead poisoning will continue to be a public health problem.
The Committee considered a number of controversial issues, and members vigorously debated
until a majority indicated that they could support the point under consideration. Readers should
carefully weigh the recommendations in this document, and they should pay particular attention to
references to work done since the 1978 CDC statement on lead. This 1985 statement represents
agreement of 11 of the 12 Advisory Commitiee members. One member, Dr. Jerome F. Cole of the
International Lead Zinc Research Organization, did not support the recommendations. Minutes of
the Advisory Committee meeting on May 17-18, 1984, and Dr. Cole's statement of dissent are
available upon request.
ACKNOWLEDGMENTS
The time, effort, and meticulous care the Committee devoted 10 this statement are gratefully ac-
knowledged. This group of dedicated health professionals, along with notable expert consultants,
labored through the results of several years of research in order to gain consensus on extremely
complex issues. The various drafts of this document had the benefit of thoughtful suggestions from
Committee members and consultants alike. Their work will help protect the children of this nation
from this preventable disease for many years {0 come.
Vernon N. Hoult, M.D.
Director
Center for Environmental Health
iii
Contents
INTRODUCTION or UT Rn I EES CR Be SN CE ER NG Sed Rt Oe IE SN (ER |
pnt Dale DRE See TR ee IRL NRE LE OF Ea CDN ER a SRE ie 1
Il. BAC KG ROUND se oi ss cs sions snr sis tne ats Phin ainnia eines said ide 3
111. SOURCESOF LEAD EXPOSURE a. i. iidbt sdb dd de rei ilg a 5
Lead Based Pali... co, cy ies ss etiens is nas Pe aie aise ae a dG a 5
Xen nh SIE GE Ra eR SN EE ae CC RA IN IY Se Si eC PCC 5
SE SIRE ME PT SS Ra ECORI le i IE Cl IN I NH RR BR 7
DCU DA ON SONI BE. ve tn iri, chaise tines nan ras a eA bad de AE eas a 7
tenn nn 0D UD RE I Te SUTTER JE i ae DOR We i fey hs mg VE a emi
Lead- at PO eRY ro ates sv mirv ne ov vs ales vs ames nd ane te A a a Re 7
OUNCES OUICES oy aes eo aise sioisidis nin ins von Luni rin avin nie sini = sions Hoalnnds aa ia inis sadn Sa LEO 7
IV. SO RE ENING ne et vee sais sd in anni ane natn han ay ay a eae A a 8
GOA Of ChHAhoOD Lead POISORINIE vs. oo Fal sianins ivan sini tn siviain’s aos a Sai ae ve Sl aa 8
Fare POPU ON ey se i al ss ers ie ss st sania cn En susie sins se a nn 8
Screen NE SC NBAUIE I... i ar DU re A ee a i en a i SAE 8
Ue ed MR EE SC ON TW SC IRE RC I I Sr A CNG 9
Tn rn BC BE ERI a RC DA i He RE 1 CR Teg I Be RN al Ce SES Se 9
Measurements Of ErytNIOCYIe ProlOPOTPRYIIY c. lee esis iin stsntns tur ehrsd ene sisnsonssress sete 10
Measurement of Blo Lead. . re. ey cd ee Ci er ne a ie ays ae sea 12
Shona bn TT OEE CR ER Se CIN CI Tl i SE Pa CET AT 12
Interpol aliONIORSCIEBRITIE . otic se viens sinh ioe vs Mis sie vines iv iain nie ns vay vans es Aa en rie anita sin 12
V. DIAGNOSTIC EVALUATION i es ts Cah a iofalie ns ES eieiiton + ante wwe vie sine Woabn elaiabe 14
20 en T ETT S TRO) SERNAESICT ra S RE U AON E 14
VI. CLINIC AL MANAGEMENT oo... cn aii ssn can aig vis ane yd sine vie tales ik conde ass ain» wel 16
Hot TL Re IRR TT GE a St SR a SE SEE CITE CE a. 16
LR Em IE Ta EN RR Rg SEY Js SRN BL EE EN AR Co 17
by TL I RT I RE ag RR SS a Pl 0 17
LOW RISK (i. oh ciate sh vinis sine ie sm vols Sin dein hr a ait Be sve te Be is a i a i a ae 17
VII. ENVIRONMENTAL EVALUATION AND LEAD HAZARD ABATEMENT ...................... 18
Ro Ly EEG ean AT IE CR DE ASE ERE or ENN SI SO 18
Fog on Un ER GR EER UNE VL [A CR SE SS PE ThE NE et 20
IE DL SR LE MR I Ie SL I CR pS CO (ha. I i ae 20
Log SERED ie ar TE NAT RIE Ri NE Sri ENE CVE SE ls Cet NE INE EG a 20
OCCUPA OB os i eis hein wtih Pe aids + is vins larnls 5 wn inain Mies as Ss a hes a aie a a a 20
EDLC Lo Te ee Ne AE EN AT G0 SR IN En EEE Sie Mee CL 21
VI HE AL TH ED IC AT ON ie ns te ssa sn nse mines o Bn viv vin + eu ih vim v ale av ar 22
IX. REPORTING LEAD TOXICITY ANDELEVATED BLOOD LEADLEVELS .....vvovv vin oife ius 22
X. REE RE RENCE i cr ce ere vis Vm ii ssi chat ainiasn ware ain se Sn 4s ala a mien enincainte waa asa nS ay aia 23
APPENDIX — Management of Childhood Lead Poisoning: Special Article ............. 0 iiiiiienninn.. 26
Contents - continued
Figure 1. Sources of Lead in a Child’s Environment ESSN Treen si SB asi tt ss vais enniateieinnints bie wione ee eit ee i
Table 1. Suggested Priority Groups for Lead no Se EEN Pale Cea Le a
Table 2.A Zinc Protoporphyrin (ZnPP) by Hematofluorometer: Risk Classification of
Asymplomatic Children for Priority Medical Evaluation ..................................
Table 2.B Erythrocyte Protoporphyrin (EP) by Extraction: Risk Classification of
Asymptomatic Children for Priority Medical Evaluation SBS eI We v8 9 0 8 ale Sale 00 A008 Sinn we ee eae
Lead is ubiquitous in the human environment as a
result of industrialization. It has no known physiologic
value. Excessive absorption of lead is one of the most
prevalent and preventable childhood health problems in
the United States today. Children are particularly sus-
ceptible to its toxic effect.
Since 1970, the detection and management of children
exposed to lead has changed substantially. Before the
mid-1960’s, a level below 60 micrograms of lead per
deciliter (ug/dl) of whole blood was not considered
dangerous enough to require intervention (Chisolm,
1967). By 1975, the intervention level had declined
50% —t0 30 ug/dl (CDC, 1975). In that year, the Center
{now Centers) for Disease Control (CDC) published /n-
creased Lead Absorption and Lead Poisoning in Young
Children: A Statement by the Center for Disease Conirol.
Since then, new epidemiologic, clinical, and experimental
evidence has indicated that lead is toxic at levels pre-
viously thought to be nontoxic. Furthermore, it is now
generally recognized that lead toxicity is a widespread
problem —one that is neither unique to inner city children
nor limited to one area of the country.
Progress has been made. The Second National Health
and Nutrition Examination Survey (NHANES II) has es-
tablished average blood Jead levels for the U.S. popula-
tion; lead-contaminaled soil and dust have emerged as
important contributors to blood lead levels, as has leaded
gasoline, through its contribution to soil and dust lead
levels. An increasing body of data supports the view that
lead, even at levels previously thought to be “safe,” is
loxic to the developing central nervous system; and
screening programs have shown the extent of lead poison-
ing in target populations.
A major advance in primary prevention is the phased
reduction of lead in gasoline. It is probably responsible
for the findings of reduced average blood lead levels in
children nationwide (Annest et al., 1983) and in (wo
major cities (Rabinowiiz and Needieman, 1982; Billick ei
al., 1980; Kaul et al., 1983). Lead is no longer allowed in
paint to be applied \o residential dwellings, furniture, and
toys. '
The sources of lead are many. They include air, walter,
and food. Despite the 1977 ruling by the Consumer Pro-
duct Safety Commission (CPSC) that limits the lead con-
I. Introduction
tent of newly applied residential paints, millions of hous-
ing units still contain previously applied leaded paints.
Older houses that are dilapidated or that are being
renovated are a particular danger to children. In many
urban areas, lead is found in soil (Mielke ei al., 1983) and
house dust (Charney et al., 1983). Consequently, screen-
ing programs—a form of secondary prevention —are still
needed to minimize the chance of lead poisoning devel-
oping among susceptible young children.
Lead poisoning challenges clinicians, public health au-
thorities, and regulatory agencies to pul into action the
findings from laboratory and field studies that define the
risk for this preventable disease. Although screening pro-
grams have been limited, they have reduced the number
of children with severe lead-related encephalopathy and
other forms of lead poisoning.
The revised recommendations in this 1985 Statement
reflect current knowledge concerning screening, diagno-
sis, treatment, followup, and environmental intervention
for children with elevated blood lead levels. Clearly, the
goal is to remove lead from the environment of children
before it enters their bodies. Until this goal is reached,
screening, diagnosis, treatment, followup, and secondary
environmental management will continue to be essential
public health activities.
DEFINITIONS
The two terms defined below—elevated blood lead
level and lead toxicity —are for use in classifying children
(whose blood has been tested in screening programs) for
followup and treatment. The terms should not be inter-
preted as implying that a safe level of blood lead has been
established. Furthermore, they are 10 be used as guide-
lines. They may not be precisely applicable in every case.
Each child needs to be evaluated on an individual basis.
The CDC is lowering its definition of an elevated
blood lead level from 30 10 25 ug/dl. The definitions
below are simplified versions of those in Preventing Lead
Poisoning in Young Children: A Siatemeni by ihe Center Jor
Disease Control: April 1978 (CDC, 1978).
® elevated blood lead level, which reflects excessive
absorption of lead, is a confirmed concentration of
lead in whole blood of 25 ug/dl or greater:
® lead toxicity is an elevated blood lead level with an
erythrocyle protoporphyrin (EP)”_level in whole
blood of 35 ug/dl or greater.
As defined by blood lead and EP levels, the terms lead
raxicity and lead poisoning are used synonymously in this
document. “Poisoning” is generally used to describe epi-
sodes of acute, obviously symptomatic iliness. The term
“toxicity” is used more commonly in this document,
since screening programs usually involve asymplomatic
children.
EP results are expressed in equivalents of free erythrocyte protoporphyrin (FEP) extracted b
ed in micrograms per deciliter of whole blood. |
= 9 _ ott oe. dd ene. be SL. x
According to this Statement, the severity of lead toxici-
ty is graded by two distinct scales—one for use in screen-
ing, the other for use in clinical management. In the scale
used in screening, children with lead toxicity are divided
into classes 1, II, 111, and IV (section IV). These classes
indicate the urgency of further diagnostic evaluation (sec-
tion V). After the diagnostic evaluation, they are placed
in one of four risk groups: urgent, high, moderate, and
low (section VI). .
y the ethyl acetate-acetic acid-HCl method and report-
n this Statement, 2in¢ protoporphyrin (ZnPP) and FEP are referred to as EP.
U
F
A nationwide survey, conducted from 1976-1980,
showed that children from all geographic areas and socio-
economic groups are at risk of lead poisoning (Mahaffey,
Annest et al., 1982). Data from that survey indicate that
3.9% of all U.S. children under the age of § years had
blood lead levels of 30 ug/dl or more. Extrapolating this
to the entire population of children in the United States
indicates that an estimated 675,000 children 6 months to
5 years of age had blood lead levels of 30 ug/d! or more.
There was, in addition, a marked racial difference in
those data. Two percent of white children had elevated
blood lead levels, but 12.2% of black children had elevat-
ed levels. Further, among black children living in the
cores of large cities and in families with annual incomes
of less than $6,000, the prevalence of levels of 30 ug/dl
or more was 18.6%. Among white children in lower
income families, the prevalence of elevated lead levels
was eight times that of families with higher incomes.
In the past decade, our knowledge of lead toxicity has
greatly increased. Previously, medical attention focused
on the effects of severe exposure and resultant high body
burdens associated with clinically recognizable signs and
symptoms of toxicity (Perlstein and Attala, 1966; Chi-
solm, 1968; Byers and Lord, 1943). It is now apparent
that lower levels of exposure may cause serious behavior-
al and biochemical changes (De la Burde and Choate,
1972, 1975, NAS, 1976; WHO, 1977). Recent studies
have documented lead-associated reductions in the bio-
synthesis of heme (Piomelli et al., 1982), in concentra-
tions of 1,25-dihydroxy vitamin D (Rosen et al., 1980;
Mahaffey, Rosen et al., 1982), and in the metabolism of
erythrocyte . pyrimidine (Angle and Mclintire, 1978;
Paglia et al., 1977). Results of a growing number of stud-
ies indicate that chronic exposure to low levels of lead is
associated with altered neurophysiological performance
and that the young child is particularly vulnerable to this
effect (Needleman et al., 1979; Winneke, 1982; Yule et
al, 1981). Investigations have also shown alterations in
electroencephalograms (EEG’s) (Burchfiel et al., 1980;
Benignus et al., 1981; Otto et al., 1982) and decreased
velocity in nerve conduction (Seppalainen and Hernberg,
1982; Feldman et al., 1977).
Many factors can affect the absorption, distribution,
and toxicity of lead. Children are more exposed to lead
than older groups because their normal hand-to-mouth
II. Background
activities introduce many nonfood items into their bodies
(Lin-Fu, 1973). Once absorbed, lead is distributed
throughout soft tissue and bone. Blood levels reflect the
dynamic equilibration between absorption, excretion,
and deposition in soft- and hard-tissue compartments
(Rabinowitz et al., 1976). Young children absorb and
retain more lead on a unit-mass basis than adults. Their
bodies also handle lead differently. Higher mineral turn-
over in bone means that more lead is available to sensitive
systems. The child's nutritional status is also significant
in determining risks. Deficiencies in iron, calcium, and
phosphorus are directly correlated with increased blood
lead levels in humans and experimental animals (Mahaf-
fey, 1981; Mahaffey and Michaelson, 1980). Increased
dietary fat and decreased dietary intake of calcium
(Barltrop and Khoo, 1975; Rosen et al., 1980), iron
(MahafTey-Six and Goyer, 1972), and possibly other nu-
trients enhance the absorption of lead from the intestine
(NAS, 1976; Barltrop and Khoo, 1975).
Since lead accumulates in the body and is only slowly
removed, repeated exposures to small amounts over
many months may produce elevated blood lead levels.
Lead toxicity is mainly evident in the red blood cells
and their precursors, the central and peripheral nervous
systems, and the kidneys. Lead also has adverse effects
on reproduction in both males and females (Lane, 1949).
New data (Needleman et al., 1984) suggest that prenatal
exposure to low levels of lead may be related to minor
congenital abnormalities. In animals, lead has caused
tumors of the kidney. The margin of safety for lead is
very small compared with other chemical agents (Royal
Commission on Environmental Pollution, 1983).
The heme biosynthetic pathway is one of the biochemi-
cal systems most sensitive to lead. An elevated EP level
is one of the earliest and most reliable signs of impaired
function due to lead. A problem in determining lead
levels in blood specimens is that the specimen may be
contaminated with lead, and thus the levels obtained may
be falsely high. Therefore, in the initial screening of
asymptomatic children, the EP level (instead of the lead
level) is determined.
The effects of lead toxicity are nonspecific and not
readily identifiable. Parents, teachers, and clinicians may
identify the altered behaviors as attention disorders,
learning disabilities, or emotional disturbances. Because
i.
1
| 1]
of the large number of children susceptible to lead poison-
ing, these adverse effects are a major cause for concern.
Symptoms and signs of lead toxicity are fatigue, pallor,
malaise, loss of appetite, irritability, sleep disturbance,
‘sudden behavioral change, and developmental regres-
sion. More serious symptoms are clumsiness, muscular
irregularities (ataxia), weakness, abdominal pain, persist-
ent vomiting, constipation, and changes in consciousness
due to early encephalopathy. Children who display these
symptoms urgently need thorough diagnostic evaluations
and, should the disease be confirmed, prompt treatment.
In this Statement, screening is distinct from diagnosis.
“Screening” means applying detection techniques to
large numbers of presumably asymptomatic children
to determine if they have been exposed to lead and, if
so, what the risks of continued exposure are. Diagno-
sis, on the other hand, means the categorization of a
child appearing to have excess exposure to lead accord-
ing to the severity of burden and toxicity so that ap-
propriate management can be started. No child with
symptoms suggesting lead toxicity should be put
through the screening process. He or she should be
brought directly to medical attention.
111. Sources of Lead Exposure
Children may be exposed to lead from a wide variety
of man-made sources. All U.S. children are exposed to
lead in the air, in dust, and in the normal diet (Figure 1).
Airborne lead comes from both mobile and stationary
sources. Lead in walter can come from piping and distribu-
tion systems. Lead in food can come from airborne lead
deposited on crops, from contact with “leaded” dust
during processing and packaging, and from lead leaching
from the seams of Jead-soldered cans. In addition to expo-
sure from these sources, some children, as a result of
their typical, normal behavior, can receive high doses of
lead through accidental or deliberate mouthing or swal-
lowing of nonfood items. Examples include paint chips,
contaminated soil and dust, and, less commonly, solder,
curtain weights, bullets, and other items.
LEAD-BASED PAINT
Lead-based paint continues to be the major source of
high-dose lead exposure and symptomatic lead poisoning
for children in the United States (Chisolm, 1971). Since
1977, household paint must, by regulation, contain no
more than 0.06% (600 parts per million (ppm)) lead by
dry weight. In the past, some interior paints contained
more than 50% (500,000 ppm) lead. The interior surfaces
of about 27 million households in this country are con-
taminated by lead paint produced before the amount of
lead in residential paint was controlled. Painted exterior
surfaces are also a source of lead. Unfortunately, lead-
based paint that is still available for industrial, military,
and marine usage occasionally ends up being used in
homes.
Usually, overt lead poisoning occurs in children under
6 years of age who live in deleriorated housing built
before World War 11. Pica, the repeated ingestion of non-
food substances, has frequently been implicated in the
etiology of lead toxicity in young children. In many cases,
however, lead-paint ingestion is simply the result of the
normal mouthing behavior of small children who live in
lead-contaminated homes. Cases of children poisoned by
lead paint have been reported ffom all regions of the
United States and from both urban and rural settings. In-
creasingly, this poisoning has been reported when fami-
lies move into a city as “urban homesteaders.,” and the
children are inadvertently exposed to chips, fumes, or
dust from lead-based paint as houses are rehabilitated.
Clusters of lead-based paint poisonings have also resulted
from demographic shifts within cities, when families with
young children have moved into neighborhoods with
deteriorating older housing. Increased lead absorption
has been reported in children exposed to chips or dust
from lead-based paint produced during the deleading of
exterior painted steel structures, such as bridges and ex-
pressways (Landrigan et al., 1982).
AIRBORNE LEAD
Generally, inhalation of airborne lead is a minor expo-
sure pathway for individual children, but lead-containing
particles—airborne and then deposited —can be responsi-
ble for high concentrations of lead in dust that children
ingest. Studies in New Jersey (Caprio et al., 1974).and
California (Johnson et al., 1975) have shown that chil-
dren living within 100 feet of major roadways have higher
blood lead levels than those living farther away. These
levels also correlate positively with the average daily traf-
fic volume on roads near homes (Caprio et al., 1974).
Previous estimates of the quantitative relationship be-
tween ambient air lead levels and blood lead levels may
need lo be revised because of new experimental and
survey dala. Preliminary results from an isotopic lead ex-
periment (Facchetti and Geiss, 1982) suggest that lead
from leaded gasoline is a much more important contami-
nant than it was previously thought to be. The preliminary
estimates from that study indicate that at least 25% of the
blood lead of residents of Turin, lialy, is derived from
lead in gasoline. In Turin, the average blood lead level in
adult males is 25 ug/dl; this corresponds to about 6 ug/dl
attributable to gasoline.
Data from NHANES II also indicate that leaded gaso-
line is a more significant source of lead than previously
thought. Annest et al. (1983) correlated major reductions
in the amounts of lead added to gasoline sold in the
United States with significant reductions in children’s
blood lead levels. They found that between 1976 and
1980, the overall mean blood lead levels in the U.S. popu-
lation dropped from 14.6 ug/dl 10 9.2 ug/dl. A similar
relationship between leaded gasoline sales and umbilical
cord blood lead levels has been shown by Rabinowitz and
Needleman (1983).
Stationary sources can produce concentrated zones of
exposure, especially where climatic conditions such as
pT SC dr. a
; oc, byl iy Foam
's a 87
- : Figure 1
SOURCES OF LEAD IN A CHILD'S ENVIRONMENT
Industrial
Sources
Mobile Airborne
Sources
-
(cars, etc.)
; pW J
inhalation
Household
Sources*
Deposition
Household
U5 Sel) pl A .
TRIN LET . -
Processing
& Canning
J
Other
Nonfood
Items**
’
*production of bullets or fishing sinkers
Soldering and stained-glass work
Gasoline sniffing
Pottery glazing
Burning of batteries, colored newsprint, lead-painted objects, snd waste oil
**Toys and figures containing lsd
Folk remedies
Cosmetics (especially Oriental cosmetics, 8.g., Surma, 8 bisck eyeliner)
Jewelry (painted with lead to simulate peerl)
Leed-contsining dust transmitted on clothing from workplace
aridity, low wind velocity, and frequent thermal inver-
sions minimize dispersal of airborne lead. The worst situ-
ations of this kind in the United States have existed in the
vicinity of primary lead smelters (Baker, Hayes el al.,
1977). - :
SOIL AND DUST
Soil and dust that contain lead are often an important
source of lead exposure for children. The particles of air-
borne lead deposited in soil and dust usually come from
automotive, industrial, and similar sources. Flaking lead
paint adds to this contamination, particularly in and
around houses. In soil, lead tends to remain in the top
centimeter, but most soils are contaminated 10 a much
greater depth when the topsoil is disturbed and turned
under.
Children appear to obtain lead from dust and soil as a
result of their normal exploratory behavior (Barltrop,
1966, Sayre et al., 1974; Roels et al., 1976), coupled in
some instances with pica. Because of those mouthing
tendencies, young children who live near major sources
of airborne lead pollution must be considered at risk of
exposure both by inhalation of airborne lead and by inges-
tion of deposited lead from soil and dust.
In general, lead in soil and dust appears to be responsi-
ble for blood lead levels in children increasing above
background levels when the concentration in the soil or
dust exceeds 500-1,000 ppm.
OCCUPATIONAL SOURCES
Lead dust can cling to the skin, hair, shoes, clothing,
and vehicles of workers, and lead can be carried from
workplace 10 home in this way. In a study in Memphis,
Tennessee, when a parent worked with lead, the amount
of lead in the children’s blood correlated with the concen-
tration of lead in dust in their homes (Baker, Folland et
al., 1977). Of 91 children tested, 38 (41.8%) had blood
lead levels of 30 ug/dl or more, and 10 either had blood
lead levels of 80 ug/dl or more or EP levels above 190
ug/dl.
Strict compliance with Occupational Safety and Health
Administration (OSHA) standards is quite effective in
decreasing this type of exposure. However, many occupa-
lional exposures to lead are not covered by the OSHA
standards. Companies with fewer than 10 employees (cot-
lage industries, “hobby” production of potiery and
stained glasswork, and home manufacturing of bullets
and fishing sinkers) are excluded from OSH A siandards.
The OSHA standard for lead workers is a blood lead
level of 40 ug/di. In a pregnant woman, lead crosses the
placenta, and lead concentrations in umbilical cord blood
are nearly equal to those in maternal blood (Barltrop,
1966). Since the growing brain of the fetus is likely to be
al leas! as sensitive 10 the neurologic effects of lead as the
brain of a young child, umbilical cord blood levels should
be at least below 25 ug/dl. Therefore, the OSHA standard
is probably not sufficiently strict to protect the fetus. Fur-
ther study is needed to define acceptable lead levels
among women of childbearing age.
FOOD AND DRINKING WATER
Lead in food, although rarely responsible for lead
poisoning in the United States, is a ubiquitous source of
background low-dose exposure for children (Beloian,
1982). Agricultural crops grown near heavily traveled
roads or near stationary sources of lead can have signifi-
canl concentrations because of airborne lead deposited
on them. Lead may also be inadvertently added to foods
during processing and handling. Canned foods may have
particularly high lead contents, because acidic foods can
leach lead from the solder in the seams of the cans
(Lammet al., 1973).
Generally, lead in drinking water has been leached
from pipes and soldered joints by soft water having an
acidic pH. Severe lead exposure has been reported among
children in Glasgow. Scotland, where pure, acidic water
was allowed to stand overnight in attic cisterns lined with
lead (Beattie et al., 1972). The problem was alleviated by
changing the pH of the water in the walter treatment
plant. In the United States, lead water pipes are mosl
commonly found in older sections of northeastern cities
and, occasionally, in rural areas of the northeast (Morse
etal., 1979).
LEAD-GLAZED POTTERY
Although not a widespread source of lead, lead-glazed
potlery can release large amounts of lead into food and
drink. It has been responsible for outbreaks of serious
poisoning (Klein et al., 1970). In several episodes report-
ed to CDC, the pottery had been imporied. Homemade
or craft potlery and porcelain-glazed vessels have been
found lo release large quantities of lead, particularly if the
glaze is chipped, cracked, or improperly applied (Osterud
et al, 1973). If the vessels are repeatedly washed, the
glaze may deteriorate and potlery previously tested as
safe can become unsafe (D. M. Wallace, personal
communication).
OTHER SOURCES
Lead is found in a variety of items, some of which
endanger specific populations or ethnic groups. A variety
of folk remedies contain lead, including azarcon and greta
used by Mexican groups and pay-loo-ah used by Hmong
refugees from Laos. Serious poisoning can also result
from gasoline sniffing; the burning of waste oil, colored
newsprini, battery casings, or lead-painted wood; and
target practice in poorly ventilated, indoor firing ranges.
IV. Screening
GOAL OF A CHILDHOOD LEAD POISONING
PREVENTION PROGRAM
The goal of a childhood lead poisoning screening pro-
gram is to identify children with significant exposure to
lead early enough to prevent serious toxicity. Elevated
blood lead levels must be detected in asymptomatic chil-
dren, and appropriate medical and environmental inter-
ventions must follow. The goal can be reached only
through —
1. A screening program that enrolls the maximum
number of children in high-risk populations.
2. A referral system that ensures a comprehensive di-
agnostic evaluation of every child with a positive
screening test.
3. A program that assures identification and elimina-
tion of the source(s) of the child's lead exposure.
4. A system that monitors the adequacy of the treat-
ment and the followup of each child with a diagnosis
of lead toxicity.
Screening is of no value without prompt, thorough,
and continuing medical and environmental followup for
those children found to have lead toxicity—that is, as
stated earlier, an elevated blood lead level (a confirmed
concentration in whole blood of 25 ug/dl or greater) and
an EP level in whole blood of 35 ug/dl or greater. Also as
stated earlier, screening must be distinguished from
diagnosis:
Screening refers to the testing of large numbers of
children considered to be ASYMPTOMATIC in order
to identify those who need further evaluation.
Diagnosis, on the other hand, refers to categorizing a
child’s condition according to severity of lead burden
and toxicity. Then, on the basis of the category,
management is selected.
Children whose elevated blood lead levels are detected
by screening should be brought directly to medical atten-
tion, and the diagnostic process should be started without
delay. Children with symptoms suggestive of lead poison-
ing require urgent and thorough diagnostic evaluation
and, if the diagnosis is confirmed, immediate treatment.
The symptoms of lead poisoning are nonspecific: they are
described in section V.
TARGET POPULATION
Lead is most harmful to children between the ages of 9
months and 6 years. Ideally, all children in this age group
should be screened. As more children are screened for
iron deficiency with EP testing, simultaneous lead screen-
ing of these same groups becomes feasible. The list of pri-
ority groups in Table 1 highlights groups for which
screening is strongly indicated. Testing children in low-
risk groups for lead toxicity may not be practical unless it
is done simultaneously with EP tests for iron deficiency.
Children in the 12- to 36-month-old age group who
live in or are frequent visitors in deteriorating older build-
ings (including day-care centers) make up the highest pri-
ority group.
Siblings, housemates, and playmates of children with
identified lead toxicity probably have similar exposures
to lead, and they should be promptly screened. Suggested
rankings for these and other priority groups are in Table 2.
Table 1
Suggested Priority Groups for Lead Screening
Priority
1. HIGHEST—Children, age 1210 36 months, who live in or are fre-
quent visitors in older, dilapidated housing
2. Children, age 9 months to 6 years, who are siblings, housemates,
visitors, and playmates of children with known lead toxicity
3. Children, age 9 months to 6 years, living in older, dilapidated
housing
4. Children, age 9 months to 6 years, who live near lead smelters and
processing plants or whose parents or other household members
participate in a lead-related occupation or hobby
S. Children, age 9 months to 6 years, who live near highways with
heavy traffic or near hazardous waste sites where lead is 8 major
pollutant
6. Alichildren 12to 36 months of age
7. Alichildren 9 months to 6 years of age
SCREENING SCHEDULE
Screening for lead poisoning should be incorporated
into a general pediatric health care program, and children
in the target population should be screened at least once a
year. The first screening should be done when the child is
between 9 and 12 months old. Children generally have
higher blood lead levels between May and October
(NAS, 1976), so screening efforts should be concentrated
in those months. Since negative screening tests in chil-
dren living in a hazardous environment do not rule out
subsequent exposure, children 12 to 36 months old who
are at high risk of exposure should be screened every 2 to
3 months, especially during the summer. Children who
move into a high-risk area after age 3 years may also need
to be screened more than once a year.
SCREENING METHODS
Currently, the most useful screening tests are those
for erythrocyte protoporphyrin (EP) and blood lead.
Venous or capillary blood can be used for both tests, but
capillary specimens are easier to collect and are, there-
fore, more widely used. Capillary blood may be transport-
ed in a capillary tube with an anticoagulant or dried on
filter paper. Sampling methods used in the field must be
compatible with laboratory capabilities.
EP and blood lead tests measure different aspects of
lead toxicity. As stated earlier, EP tests measure the level
of EP in whole blood, and a level of 35 g/dl or more indi-
cates impaired heme synthesis, which may be due to the
toxic effects of lead; blood lead tests measure lead absorp-
tion, and a confirmed concentration of 25 ug/dl or more,
referred to as an elevaied blood lead level, reflects an ex-
cessive absorption of lead. Usually, there is a close corre-
lation between results of the two tests for specimens from
the same child, but, occasionally, the result of one test
may be elevated and the result of the other, not elevated.
The EP test has three advantages over the blood lead test:
(1) when blood lead levels are moderately elevated, the
EP test better identifies children with rising blood lead
levels (Reigart and Whitlock, 1976); (2) if the specimen
is contaminated with lead, the contamination does not
affect the EP test; and (3) the EP test is an accepted
screening test for iron deficiency.
INTERVENTION LEVELS
Children screened for lead poisoning can be grouped
into two categories: those who require further evaluation
and those who do not. Choosing the intervention level
that divides these two groups is based on a compromise
among the following:
(1) the desire to identify all children with any degree
of lead toxicity
(2) a judgment about the urgency of preventing vari-
ous detectable effects
(3) the sensitivity and specificity of a practical screen-
ing test
(4) society's ability to remove the sources of lead
exposure
A. Pathophysiological Considerations
In recent years, levels of exposure previously consid-
ered “safe” have been shown to produce adverse effects.
In addition, contemporary people (including children)
living in remote areas with negligible exposure to lead
have blood lead levels much lower than people living in
the United States (Piomelli, 1980). Thus, the blood lead
levels of U.S. children reflect a high degree of environ-
mental contamination by lead. Today, the average blood
lead level in the U.S. population is about 10
ug/dl—approximately three times the average level
found in some remote populations. These observations
suggest that the average level in the U.S.A. should be re-
duced. At present, however, because of practical consid-
erations, the goal of reducing U.S. levels 10 those of
remote populations is unattainable. Therefore, the blood
lead level at which intervening action should be taken
should be based on (1) criteria that indicate significant
risk to the individual child and (2) the best combination
of tests: a test for the blood lead level as an indicator of ab-
sorption and a test for EP as an indicator of biochemical
derangement.
Since the CDC's 1978 statement on lead poisoning,
several investigators have demonstrated effects of low-
level lead exposures in these areas:
1. children’s behavior and intelligence (Needleman et
al., 1979; Winneke, 1982; Yule et al., 1981)
2. the central and peripheral nervous systems of adult
workers (Mantere et al., 1982; Seppalainen and
Hernberg, 1982) :
3. heme biosynthesis in children (Piomelli et al., 1982)
4. nucleotide metabolism (Angle and McIntire, 1978)
5. vitamin D metabolism in children (Rosen et al.,
1980; Mahaffey, Rosen et al., 1982).
The precise level at which lead exposure begins 10"
cause developmental or neurobehavioral problems in
children may be impossible to define in the near future.
In the meantime, decisions on public health measures
have to be made on the basis of (1) other, more objective- '
ly measurable effects and (2) an adequate margin of
safety. X
The elevation of EP, a toxic effect of lead in humans,
has been well studied and it can be measured objectively.
Among the biologic markers of lead toxicity, EP measure-
ments have been the most useful in screening programs
for lead poisoning. Recent studies have shed new light on
the effects of lead and of iron deficiency on EP levels.
Several years ago, Roels et al. (1976), basing their
argument on EP measurements, stated that a blood lead
level of 25 ug/dl should be the maximum permissible
concentration. Cavalleri et al. (1981), who made a study
around a lead smelter, indicated that even this level may
be too high. This group found an EP response at blood
lead levels ranging between 10 and 20 ug/dl, suggesting
that the EP no-response level is lower than 10 ug/dl. In a
more recent and comprehensive examination of the
issue, Piomelli et al. (1982) studied data from over 2,000
children. Blood lead and EP tests were done on venous
specimens collected from children throughout New York
City. Piomelli and his colleagues were trying to find the
biood lead level at which the EP level began 10 increase.
A variety of statistical techniques were used, and the find-
ings were consistent; when blood lead levels increased
linearly above the area of 15-18 ug/dl, the EP level in-
creased exponentially.
Recent studies of EDTA (calcium disodium ethylene
diamine tetraacetic acid) mobilization testing indicate
that the amount of lead excreted by children with blood
lead levels of 30-40 ug/dl may often be comparable to
that excreted by children with levels of 50-70 ug/dl (Mar-
kowitz and Rosen, 1984). This finding suggests that the
“blood lead level may underestimate the body burden of
lead.
In summary, the EP data, with data from the other
‘studies referred to, indicate that the 1978 blood lead
guideline of 30 ug/dl has little or no margin of safety and
should be lowered.
B. Practical Considerations
Although the biologic threshold for lead toxicity, as
manifested by increasing EP levels, is less than 20 ug/dl,
the criteria for a screening program have to take into ac-
count additional factors: (1) acceptability, sensitivity, and
specificity of the screening procedure; (2) cost-
effectiveness; and (3) the feasibility of effective interven-
tion and followup.
The identification of children with blood leads below
25 ug/dl would require screening with a blood lead assay
rather than an EP test, since the latter screening test has a
very poor sensitivity and specificity below a blood lead
level of 25 ug/dl. Such a recommendation would require
most programs to use venous blood samples or to adopt
impractically rigorous training and quality control proce-
dures. Capillary blood samples are prone to environmen-
tal contamination with lead. In most programs, particular-
ly those in high-risk areas, the use of “routine” capillary
blood-drawing techniques results in an unacceptably high
frequency of falsely elevated blood lead levels. On the
other hand, taking blood samples from the veins of small
children is less acceptable to parents and technically
much more difficult. In addition, the cost of the screening
program would increase severalfold. For all these reasons,
an intervention level set at blood lead values below 25
ug/dl might ultimately substantially decrease the number
of children being screened.
If local screening programs evaluate the distribution of
moderately and highly elevated blood lead levels within a
community, the findings may identify sources of lead that
might go unnoticed if the program focused solely on
children with high lead levels.
Even when slightly elevaied blood lead levels are
found, some interventions are possible and effective.
House dust is an insidious but apparently effective carrier
of lead to children in contaminated environments. In
urban areas dust frequently contains large amounts of
lead, thought to come primarily from airborne sources or
leaded paint. Charney et al. (1983) have documented the
effectiveness of controlling house dust; thus, in some sit-
uations, low and moderately elevated blood lead levels
can be reduced simply by controlling house dust.
Considering these factors, CDC recommends as the in-
tervention level a blood lead level of 25 ug/dl associated
with an EP level of 35 ug/dl. When the blood lead level is
25 mg/dl or greater associated with an EP value of 35
mg/dl or greater, lead toxicity is presenti; identification of
such children is the focus of CDC's new recommendations.
Children may have mildly elevated blood lead levels with-
oul concurrent increases in EP concentrations, and it is
10
desirable to identify these children, but, at present, this is
impractical and beyond the criteria set for screening pro-
grams. Nonetheless, when resources and capabilities
permit both blood lead and EP to be measured in the pri-
mary screening program, additional children with elevat-
ed blood lead levels will be identified. A more practical
method for identifying such children needs to be
developed.
The CDC recommends the following cutoff levels for
determining a high risk for lead toxicity: for EP screening,
a level of 35 ug/dl (whole blood should be tested); for fol-
lowup testing, all children with a blood lead of 25 ug/dl or
more should be considered at risk for the toxic effects of
lead. Since the EP level is also elevated in iron deficiency,
an elevated EP test alone should not be considered to be
diagnostic of lead toxicity.
MEASUREMENT OF
ERYTHROCYTE PROTOPORPHYRIN
Erythrocyte protoporphyrin (EP) may be measured by
fluorometry after it has been .extracted from the red
blood cells or by direct fluorescence in intact cells
(Lamola et al., 1975; Blumberg et al., 1977). In lead
toxicity and iron deficiency, this metabolite is presént in
the red cells mainly as zinc protoporphyrin (ZnPP), but
the ethyl acetate-acetic acid extraction procedure converts
zinc protoporphyrin to erythrocyte protoporphyrin.
Measuring ZnPP by hematofluorometer and EP after it
has been extracted from the cells reflects essentially the
same compound. In erythropoietic protoporphyria, an ex-
tremely rare disease, EP is markedly elevaled — usually
above 300 ug/dl. This is the free EP base, but it is detect-
ed by the EP extraction method and, to a lesser extent, by
the hematofluorometer.
EP is also elevated in sickle cell anemia and other
hemolytic anemias (Langer et al., 1972). Hyperbiliru-
binemia (jaundice) will cause falsely elevated EP readings
with the hematofluorometer, but not with the extraction
method (Buhrmann et al., 1978). Recent colds, ear infec-
tions, and other minor illnesses may also cause slight ele-
vations of EP (Reeves et al., 1984). Nevertheless, lead
toxicity should always be ruled out as the cause of elevat-
ed EP levels.
A. Use of Hematofluorometers
Hematofluorometers measure ZnPP and report values
in EP equivalents. They are calibrated against the extrac-
tion method and theoretically should yield corresponding
values. In practice, the values obtained with these instru-
ments are usually not 100% of the EP present and may be
considerably less. At least two studies (Kaul et al., 1983;
Hammond et al., 1984) indicate that, at high levels,
values obtained with hematofluorometers are lower than
those obtained with the extraction method, but that up to
35 ug/dl the results are similar. Because hematofluo-
rometers give immediate results and are economical,
they are eminently suitable for field screening.
For both the hematofluorometer and the extraction
method, the distinction between a positive and negative
screening test should be based on a cutoff level of 35
ug/dl. However, for risk classification, the cutoff points
for ZnPP measured by hematofluorometer (Table 2.A)
differ from those for EP measured by the extraction
method (Table 2.B). If possible, centralized laboratories
should use extraction methods, and, if the followup
laboratory has extraction capability, all confirmatory tests
for EP should be done by extraction, not hematofluo-
rometer. Hematofluorometers are most likely to give
accurate results when used to analyze freshly collected
blood specimens. The differences between methods need
further study.
B. Erythrocyte Protoporphyrin and Iron Deficiency
A benefit of EP screening is that when an elevated EP
level proves not to be due to lead, it usually reflects iron
deficiency (Piomelli, 1977). The first signs of iron defi-
ciency are biochemical abnormalities (low serum ferritin,
low transferrin saturation, and high EP) followed by cel-
lular abnormalities (microcytosis and hypochromia).
Iron deficiency anemia follows these changes as the
hemoglobin and hematocrit values fall.
The EP test proved to be practical in screening for iron
deficiency in a population of 4,160 children (Yip et al.,
1983). The upper limit of normal for EP in this study was
35 ug/dl. The predictive value appeared to be satisfactory.
Iron deficiency is common in many of the groups at
risk for lead poisoning—especially among inner-city
children of low socioeconomic status living in old, dilap-
idated housing. Iron deficiency is common among infants
ages 9 to 24 months; the highest frequency of lead poison-
ing extends through 36 months. Iron deficiency and lead
toxicity may occur in the same child. Furthermore, ex-
perimental evidence indicates that iron deficiency in-
creases the proportion of lead absorbed from the intestine
and aggravates the toxic effects of lead.
Analysis of the NHANES 11 data has clarified the rela-
tionship between elevated EP values, blood lead levels,
and iron deficiency in a representative sample of the U.S.
population. Among children in the NHANES II survey
with elevated EP values, 31% have elevated blood lead
levels, 18% have iron deficiency (as evidenced by a trans-
ferrin saturation of less than or equal to 12%), and 11%
have evidence of both conditions (R. Yip, personal com-
munication). On the other hand, among children with
elevated blood lead levels, only about 26% have lead
toxicity—that is, an elevated EP level (NCHS, 1984). In
high priority populations (Table 1), in which iron defi-
ciency is more common and lead levels are higher, a
greater proportion of children with elevated blood lead
levels would have elevated EP levels. Analyses by both
Yip and NCHS confirm that a synergistic effect exists be-
tween lead toxicity and iron deficiency in children, as ex-
perimental studies in animals have suggested.
11
Table 2.A
Zinc Protopor} hy o (ZnPP) by Hematofluorometer
Risk Classificstion of Asymptomatic Children
fu Priuity Medical Evaluation
Erythrocyte Protoporphyrin (EP) #
Bleed Lead #
<3 35.74 75-174 >178
Not done | of . .
<24 | ba la EPP+
25-49 Ib Il mn mn
$0-69 .e mn 1] Iv
> 70 stat .s Iv Iv
# = Units are in ug/d! of whole blood.
» = Blood lead test needed to estimate risk.
EPP+ = Erythropoietic protoporphyria. Iron deficiency may cause
elevated EP levels up to 300 ug/dl, but this is rare.
= [n practice, this combination of results is not generally ob-
served. if it is observed, immediately retest with whole blood.
NOTE: Diagnostic evaluation is more urgent than the classification indi-
cates for—
1. Children with any symptoms compatible with lead toxicity.
2. Children under 36 months of age.
3. Children whose blood lead and EP levels place them in the
upper part of a particular class.
4. Children whose siblings are in a higher class.
These guidelines refer to the interpretation of screening results, but the
final diagnosis and disposition rest on a more complete medical and
laboratory examination of the child. .
Table 2.B
Erythrocyte Protoporphyrin (EP) by Extraction
Risk Classification of Asymptomatic Children
for Priority Medical Evaluation
Erythrocyte Protoporphyrin (EP) #
Blood Lead #
<38 35-109 110-249 > 250
Not done | . s og
<24 I la la EPP+
25-49 Ib 1 [1] [1]
50-69 ’e Hl in 1v
> 70 we oe Iv Iv
J = Units are in ug/dl of whole blood.
a = Blood lead test needed to estimate risk.
EPP + = Erythropoietic protoporphyria. Iron deficiency may cause
elevated EP levels up to 300 ug/dl, but this is rare.
aii = [n practice, this combination of results is not generally ob-
served, if it is observed, immediately retest with venous
blood.
NOTE: Diagnostic evaluation is more urgent than the classification indi-
cales for—
1. Children with any symptoms compatible with lead toxicity.
2. Children under 36 months of age.
3. Children whose blood lead and EP levels place them in the
upper part of a particular class.
4. Children whose siblings are in a higher class.
These guidelines refer to the interpretation of screening results, but the
final diagnosis and disposition rest on a more complete medical and
laboratory examination of the child.
MEASUREMENT OR ELOSDL nD
Unlike elevated EP levels (whi
"iron deficiency or other illnesses),
levels are specific for lead absorption. Fluctuations in
blood lead values over a short period can be due to physi-
" ologic variations or sporadic acute lead exposure.
Capillary samples are highly sensitive to contamination
with environmental lead. If such samples are to be taken
for blood lead assays, the personnel must be rigorously
trained before any screening program is begun, and dupli-
cate capillary blood specimens should be drawn. A single
tube of capillary blood should never be used for the diag-
nosis of elevated blood lead, because an elevated value
may be caused by contamination. If results of tests for
blood lead from two tubes differ substantially, the higher
value can be considered spurious. Even when the results
are equally elevated, contamination cannot be excluded.
Therefore, only venous blood samples should be used to
confirm a diagnosis or to determine or assess treatment.
There is less likelihood of contamination in a venipunc-
ture, but venous blood may be difficult to collect from
very young children. Neither the blood lead nor the ex-
traction EP test should be considered a routine procedure
in_the clinical laboratory. To help insure credible test re-
sults, laboratories performing these tests should partici-
pate in the CDC proficiency testing program or the
equivalent. ’
njay be caused by
SCREENING SCHEMES
Three feasible screening strategies are —
1. Screening with EP tests, followed by blood lead
measurements if indicated. This is the most
common procedure.
2. Screening with both EP and blood lead tests.
3. Screening with blood lead tests, followed by EP
measurements if indicated.
— The CDC recommends EP tests, followed by blood
lead measurements for all children with an elevated EP
level. The EP test has these advantages:
1. Ease of measurement by hematofluorometer or the
extraction method.
2. Results that are not affected if specimens are con-
taminated with environmental lead.
3. More cost effective than screening with the blood
lead test.
. Ability to detect a child's metabolic response to the
toxicity of lead.
. Possibility of differentiating between children with
stable blood lead levels and those with declining
levels.
6. Possibility of identifying children who have iron
deficiency. ’
In some areas, where the environment is grossly con-
taminated with lead, a strategy of simultaneous testing
for EP and blood lead levels is recommended. In these
cases, venous samples should be used for measuring lead.
When EP [ primary screening tool, two approaches
are possible:
1. EP measured on site. A capillary blood specimen is
collected, and while the child waits at the screening
site, EP is determined by hematofluorometer.
Children found to have EP values of 34 ug/dl or
less are discharged until the next routine screening.
For those with EP values of 35 g/dl or more, addi-
tional blood samples are taken (preferably by veni-
puncture) for laboratory analysis of blood lead and
of EP—Dby extraction, if the method is available.
. EP measured off site. A venous blood sample or
duplicate capillary samples are collected at the
screening site and sent to the laboratory for mea-
surement of EP, preferably by the extraction
method. The amount of blood collected should be
sufficient for confirmatory tests. Unused specimens
of blood from children whose EP levels are 34 ug/dl
or less may be discarded. For those children with
EP levels of 35 ug/dl or more, the blood lead levels
and hematocrits or hemoglobin concentrations
should be determined.
On site, EP is nearly always measured by hematofluo-
rometer; off site— preferably —it is measured by the ex-
traction method. If the blood specimen is protected from
temperature extremes and light, it may be stored for a
week to 10 days before being analyzed by the extraction
method. Blood collected on filter paper may be stored for
several weeks before it is analyzed.
INTERPRETATION OF SCREENING RESULTS
A single screening test, either for EP or blood lead,
cannot be used to categorize children for priority in fol-
lowup. Both EP and blood lead levels must be used to
determine the potential risk of lead toxicity in the chil-
dren screened.
Children can be arbitrarily divided into four classes on
the basis of EP and blood lead screening results. In view
of the observed discrepancy between results from the
hematofluorometer and extraction methods, two tables
are given: Tables 2.A and 2.B (derived from Kaul et al.,
1983). This classification merely suggests the relative
risk and the priority for medical evaluation and environ-
mental intervention, and the tables should be used only
as general guidelines. Children 12 to 36 months old
should be given priority over older ones, and children
whose EP and blood lead levels fall into the upper range
of a class should be given priority over those whose levels
fall into the lower range. For example, the urgency for fol-
lowup is greater for a 1-year-old whose EP level by extrac-
tion is 109 ug/dl and whose blood lead level is 49 ug/dl
than for a § 1/2-year-old whose EP level, by the extrac-
tion method, is 36 ug/dl and whose blood lead level is 26
ug/dl. Yet both children fall into class 11.
Children in class IV-—at urgent risk of lead
toxicity—should be medically evaluated within 24 hours,
A
and in no case later than ®.. 48 hours. Children in
class 111 are at high risk. Those in class 1I are at moderate
risk, and those in class I, at low risk.
Class I can be subdivided into two additional catego-
ries. Class la (blood lead, 25 ug/dl or less, and EP, 35
ug/dl or more) includes children with iron deficiency.
These children should be retested, with additional assess-
ment of iron status. Class Ib (blood lead, 25-40 ug/dl,
_,and EP, less than 35 ug/dl) covers children who appear
to have transient, stable, declining, or increasing blood
13
lead ve sie should be confirmed by retesting, and
the children should be carefully followed. In some cases,
the blood lead and EP results will differ. When the EP
value is significantly higher than the value suggested by
the blood lead level, the child probably has both iron defi-
ciency and excessive lead absorption.
Screening should focus on asymptomatic children.
Children with symptoms should be referred for immedi-
ate evaluation, regardless of their risk classification.
V. Diagnostic Evaluation
Screening tests are not diagnostic. Therefore, every
child with a positive screening test should be referred to a
physician for evaluation, with the degree of urgency in-
dicated by the risk classification. At the first diagnostic
evaluation, if the screening test was done on capillary
blood, a venous blood lead level should be determined in
a laboratory that participates in CDC's blood lead profi-
ciency testing program. Even when test: are done by ex-
perienced personnel, blood lead levels may vary 10% to
15%, depending on the level being tested. Tests for the
same child may vary as much as = 5 ug/dl in a 24-hour
period. Thus, differences of 1 to 5 ug/dl between screen-
ing and diagnostic levels in either direction should not
necessarily be interpreted as indicative of actual changes
in the child's lead absorption or excretion.
Additional blood samples may be needed for tests such
as complete blood counts, serum iron, total iron binding
capacity, and serum ferritin. The amounts necessary for
these tests, which usually exceed the amount obtainable
by capillary sample, can be Dbtained with a single
venipuncture. :
Symptoms, if present, constitute an urgent risk, war-
ranting prompt hospitalization (section VI). Symptoms
must be looked for, and they can be missed (Piomelli et
al., 1984):
Acute lead encephalopathy is characterized clinically
by some or all of these symptoms: coma, seizures,
bizarre behavior, ataxia, apathy, incoordination,
vomiting, alteration in the state of consciousness, and
subtle loss of recently acquired skills. Any one or a
mixture of these symptoms, associated with an eleval-
ed blood lead level, constitutes an acute medical
emergency. Lead encephalopathy is almost always as-
sociated with a blood lead level exceeding 100 ug/dl,
although, occasionally, it has been reported at blood
lead levels as low as 70 ug/dl.
Symptomatic lead poisoning without encephalopathy
is characterized by one or several symptoms: decrease
in play activity, lethargy, anorexia, sporadic vomiting,
intermittent abdominal pain, and constipation. It is
usually associated with a blood lead level above 70
ug/dl, although, occasionally, cases are associated
with a level as low as 50 ug/dl. [f the blood lead level is
below 50 pu g/dl, other causes should be vigorously sought.
Since any symptomatic child may develop acute lead
14
encephalopathy, treatment and supportive measures
must be started immediately on an emergency basis.
Whether or not symptomatic lead poisoning is present,
the child should have a complete pediatric evaluation.
Special attention should be given to—
1. A detailed history, including the presence or ab-
sence of clinical symptoms, child’s mouthing activi-
ties, existence of pica, nutritional status, family his-
tory of lead poisoning, possible source of exposure,
and previous blood lead or EP determinations.
. The physical examination, especially the neuralogic
examination.
. Nutritional status and hematologic evaluation for
iron deficiency. Iron deficiency contributes to an
elevated EP and can enhance lead absorption and
toxicity.
4. Confirmatory diagnostic tests.
S. Trends in EP and blood lead levels.
Since trends are important in diagnosis and manage-
ment, serial measurements of blood lead and EP (and
other measurements as indicated) are far more valuable
than data obtained at one time. To be comparable and in-
terpretable, serial EP levels should be analyzed by the
same method.
Probably the most reliable method for determining the
source of exposure is obtaining a careful, complete envi-
ronmental history (section 111), inspecting the home for
lead hazards, and learning about the child's hand-
to-mouth behavior through careful questioning. Pica, the
Latin word for “magpie,” describes the habitual ingestion
of nonfood substances. This should not be regarded as
synonymous with the normal oral behaviors of small chil-
dren. such as finger and thumb sucking and nail biting.
An initial plan for management requires that all inter-
acting factors be taken into account. The plan should be
modified as indicated by long-term trends in lead absorp-
tion, exposure, and clinical status.
TESTS
In addition to confirmatory and serial EP and blood
lead determinations, the following tests can be useful (if
available) in assessing the patient’s lead absorption status.
1. Tests for Iron Deficien
Because the EP can reflect iron deficiency as well as
-" lead exposure, the presence of iron deficiency must be es-
tablished or ruled out if EP levels are to be properly
interpreted.
A common misconception is that a child with a
“normal” hematocrit (33% or more) or hemoglobin con-
centration (11 g/dl or more) could nor be iron deficient.
This is not true, particularly with respect to iron deficien-
cy sufficient to affect EP and, worse, to enhance lead ab-
sorption and retention. Thus, although a complete blood
count (CBC) and a reticulocyte count are indicated in the
evaluation of lead toxicity, they are not sensitive enough
to rule out iron deficiency.
Of the red blood cell (RBC) indices, a decreased mean
corpuscular volume (MCV) is a useful indicator of iron
deficiency. Normal values depend on age (Dallman,
1982).
Serum iron and iron binding capacity are more sensi-
tive than the MCV. In general, an elevated iron binding
capacity of more than 350 ug/dl is more likely to accurate-
ly indicate iron deficiency than a normal or low serum
iron, since the serum iron is quite sensitive to both di-
etary iron and diurnal variation. Thus, if a child has eaten
an iron-rich food within 2-4 hours before the blood for
the test is drawn, the result may be closer to the normal
level than is actually the case. Under standardized condi-
tions, an abnormally low ratio of serum iron to iron bind-
ing capacity (transferrin saturation) is consistent with
iron deficiency. In addition to the level of EP itself, the
serum ferritin level is an accurate indication of overall
iron status.
2. Flat Plate of the Abdomen
Radiologic examination (flat plate) of the abdomen
may reveal radiopaque foreign material, but only if the
material has been ingested during the preceding 24 to 36
hours. Since lead ingestion is sporadic, this examination
is significant only if the results are positive; negative re-
sults do nor rule out lead poisoning. Positive results indi-
cate recent ingestion of large amounts of lead.
3. X-ray of Long Bones
X-rays of the long bones, usually the knees, may help
estimate the duration of exposure. Lines of increased
density in the metaphyseal plate of the distal femur and
proximal tibia and fibula are “growth arrest lines.” They
are caused by lead, which disrupts the metabolism of the
bone matrix. As a result, areas of increased mineraliza-
tion or calcification may be present at the metaphyses of
the long bones. Though sometimes called “lead lines,”
they are not an x-ray shadow of deposited lead.
Although definitive data are not available, these lines
are thought to become visible after at least 4 to 8 weeks
from the time exposure began; the length of time
depends on the age of the child and the degree of lead
exposure. The width and intensity of the lines reflect pro-
15
longed orcs lead absorption but do not indicate cur-
rent ingestion. They are seldom seen in children under
24 months of age. Negative x-rays do not rule out lead
poisoning.
4. Calcium Disodium EDTA Mobilization (or Provoca-
tive Test)
This test is used to identify children who will respond
to chelation therapy with a brisk lead diuresis. Children
whose blood lead level exceeds 55 ug/dl should not re-
ceive a provocative chelation test. Instead, appropriate
chelation therapy should be started. The mobilization test
is particularly useful when the screening test indicates
that the child has lead toxicity and there is some question
as to whether chelation therapy is indicated. This test pro-
vides an index of the mobile or potentially toxic fraction
of the total body lead burden (Saenger et al., 1982).
Since CDC’s 1978 statement, an 8-hour mobilization
test has been shown 10 be as reliable as a 24-hour mobili-
zation test (Markowitz and Rosen, 1984). Although an
8-hour test may be done on an outpatient basis, the pa-
tient should not leave the clinic. The careful use of “lead-
free” apparatus is mandatory.*
S. Lumbar Puncture
CAUTION:
If a lumbar puncture is needed to rule out meningitis
or other serious disease, it should be performed cau-
tiously and only after a careful search for signs and
symptoms of increased intracranial pressure. The fluid
should be obtained drop by drop, and no more than 1
milliliter (ml) should be removed.
3
The following tests are not useful in diagnosing lead
toxicity.
1. Microscopic Examination of Red Cells for Basophilic
Stippling
Since basophilic stippling is not universally found in
chronic clinical lead poisoning and is relatively insensitive
to lesser degrees of lead toxicity, it is nor considered
useful in diagnosis.
2. Tests of Hair and Fingernails for Lead Levels
The levels of lead in hair or fingernails are not well cor-
related with blood lead levels; therefore, tests for these
levels are nor considered useful in diagnosis.
*Special lead-free collection apparatus must be used if valid test results
are 10 be obtained. The laboratory performing the analysis may supply
the proper collection apparatus. Preferably, urine should be voided
directly into polyethylene or polypropylene bottles that have been
cleaned by the usual procedures, then washed in 1% nitric acid, and
thoroughly rinsed with deionized, distilled water. For children who are
not toilet trained, plastic pediatric urine collectors, with double com-
partments, may be used. Urine collected in this manner should be
transferred directly jo the urine collection bottles. Preserving the col-
lected urine with hydrochloric acid will stabilize not only lead but also §-
aminolevulinic acid (ALA).
VI. Clinical Management
The system described in section IV is for an initial
classification, to be modified by results of the diagnostic
evaluation. Thus, after all information is available to the
clinician, the child's true risk classification is established.
Clinical management includes eliminating the source of
the child’s lead exposure; providing general pediatric
care, family education, and, when appropriate, chelation
therapy; and correcting any nutritional deficiencies. In ad-
dition, followup examinations must be performed until
the risk of further damage is minimal. The single most im-
portant factor in pediatric management is to reduce the
amount of lead ingested. The family must be fully informed
of the child's condition and of the clinical and environ-
mental actions to follow.
One recommended approach to the treatment of chil-
dren with symptomatic and asymptomatic lead poisoning
is described in detail in the Appendix. The major new fea-
ture of this approach is an increased reliance on calcium
disodium EDTA mobilization testing among children
with moderate blood lead levels. The test results are used
to decide whether chelation is indicated. A full course of
chelation therapy should not be given without either a
confirmed blood lead level equal to or greater than 56
ug/dl or a positive mobilization test in children with
blood lead levels of 25-55 ug/dl. This approach is recom-
mended by four major medical centers in which the staffs
have had extensive experience in the diagnosis and treat-
ment of children with lead poisoning.
The cornerstones of clinical management are careful
clinical and laboratory surveillance of the child and a re-
duction in lead exposure to prevent further accumulation
of lead. This approach allows previously absorbed lead to
be slowly excreted. Most children with lead toxicity do
not require chelation therapy, but those who do may
need more than one course of treatment.
The followup program for asympiomalic children
depends upon the degree of risk determined during Lhe
diagnostic evaluation.
For the purposes of clinical management and followup,
the risk categories are ranked from urgent to low.
Urgent — Blood lead levels of 70 ug/dl or more with
or without symptoms.
High — Children whose repeat EP and confirmatory
venous blood lead levels fall in the class II and 11]
ranges of the screening test, but who also have a posi-
16
tive calcium disodium EDTA mobilization test or
other confirmatory diagnostic tests or risk factors.
Children in class 11 who have not had confirmatory di-
agnostic tests should be considered high risk until evi-
dence places them in another risk category.
Moderate — Children whose repeat EP and venous
blood lead levels fall into the class Il range of the
screening test but whose other confirmatory diagnostic
tests sre negative.
Low — Children whose repeat EP and venous blood
lead levels fall into the class | range of the screening
tests. These children are usually not given other diag-
nostic tests. .
This calegorization is arbitrary and can be adapted to a
particular child. For example, a 20-month old with per-
sistent pica whose environmental lead hazard cannot be
controlled satisfactorily may be considered high risk,
even if his or her repeat EP and venous blood lead levels
fall in the range of class Il and other diagnostic tests are
negative.
URGENT RISK
Children with blood lead levels of 70 ug/dl or more,
regardless of the presence or absence of clinical symp-
toms, should be treated with the same intensity as chil-
dren with frank neurologic manifestations. The higher
the confirmed venous blood lead, the greater the need for
chelation therapy. Severe and permanent brain damage
may occur in as many as 80% of children who have acute
encephalopathy (Perlstein and Attala, 1966). Treatment
before onset of encephalopathy will improve this grim
Prognosis.
Lead toxicity is a chronic medical problem. Children
who require chelation therapy will need long-term medi-
cal surveillance and care. The EP levels can fluctuate
during and immediately after chelation therapy. After an
apparently successful course of therapy with calcium diso-
dium EDTA (incorporating BAL, British Anti-Lewisite,
as necessary), the “rebound” phenomenon may be
observed.
First, the blood lead level drops during treatment.
This is not a reason to interrupt therapy. Then, after treat-
ment is stopped, the blood lead level almost invariably
rises again. This phenomenon reflects a reequilibration of
stored lead. The decision to repeat chelation therapy is
based on the blood lead level after the “rebound.”
Reduction of lead intake is urgent for all children in
this category, both as part of immediate therapy and as
part of the followup preventive procedure. Children re-
ceiving chelation therapy should not be released from the
hospital until lead hazards in their homes and environ-
ment are controlled. Otherwise, suitable alternative hous-
ing must be arranged. Thus, the appropriate public
agency in the community must be notified immediately
so that environmental investigation and intervention can
begin.
After their hospitalization and after lead has been re-
moved from their environments, these children are still
at high risk. Close followup, with blood lead and EP mea-
surements, is required. At first, these tests should be
done every 1 to 2 weeks. If the blood lead level rebounds
to its pretreatment level, a repeat of the chelation therapy
should be considered. If the blood lead level remains
stable or shows a continual decline after the first few
weeks, the interval between testing may be incrementally
increased from 1 to 6 months until the blood lead and EP
levels return to normal or the child reaches 6 years of age.
HIGH RISK
Many children in the high-risk category will have been
given a calcium disodium EDTA mobilization test to
determine whether chelation therapy is needed. If it is
needed, inpatient chelation should be performed. Under
some conditions, however, children without urgent risk
factors may be treated as outpatients. Outpatient treat-
ment should be reserved, however, for those centers
capable of providing closely monitored outpatient care
and followup supervision, and in those centers it should
be provided only if the child's source of lead exposure
has been eliminated (Piomelli et al., 1984). In addition,
the parents should be cooperative and should demon-
strate that they can follow instructions.
Followup of high-risk children should consist of blood
lead or EP tests, or both, at least monthly (especially in
the summer), until the sources of lead in their environ-
ments have been removed. If their blood lead or EP
levels have declined or stabilized, the interval between
testing may be incrementally increased, except in
summer, from } to 6 months, until the blood lead and EP
levels return to normal or the child reaches 6 years of age.
Careful neurological and psychological assessment is ad-
vised so that any behavioral or neurological deviation can
}7
be 9 early and proper therapy and school place-
ment begun.
MODERATE RISK
Generally, children in this category do not require che-
lation therapy. Reducing lead intake from all sources and
careful monitoring of the child usually suffices.
Until the lead hazards are eliminated from their envi-
ronment, these children should be tested monthly in the
summer and every 2 months in other seasons. If the
blood lead and EP levels remain stable or show a continu-
al decline after the first few months, the interval between
testing -may be incrementally increased from 2 to 6
months until the blood lead and EP levels return to
normal or the child reaches 6 years of age.
NOTE: All children in the urgent-, high-, and
moderate-risk categories may have concomitant nutri-
tional deficiencies. These deficiencies may increase the
child’s risk from lead by increasing absorption, retention,
and toxicity. All children in these categories should re-
ceive a careful nutritional evaluation, including appropri-
ate laboratory tests. In addition to the care given for lead
toxicity, nutritional therapy should be provided. When in-
creased lead absorption is found, it may be particularly
important to correct iron deficiency and maindain an ade-
quate calcium intake.
LOW RISK
When tested, children in this category do not have sig-
nificant evidence of lead toxicity. However, they require
periodic screening until they reach their sixth birthday.
Children whose elevated EP levels are not caused by lead
absorption should receive medical attention and care for
the medical condition responsible for the elevation.
Children with elevated blood lead levels but no evidence
of toxicity should be evaluated monthly until lead toxicity
can be ruled out. This can usually be done within 3
months.
In conclusion, the clinical management of children
with lead poisoning must include appropriate treatment,
adequate followup, environmental intervention, and
family education. Chelation therapy is indicated for some
children with lead toxicity. Using it indiscriminantly is
unwise, but so is withholding or delaying it when it is in-
dicated. The physician providing clinical management
must know the current status of the child's environment.
The optimal frequency of followup depends on many fac-
tors, including the child's age and environment and the
trend in results of the child’s tests.
VIL. Environmental Evaluation and
Lead Hazard Abatement
Environmental investigation and intervention should
segin as soon as lead toxicity is confirmed. Lead hazards
must be identified and removed from the environments
5f these children. Priorities for action should be deter-
. mined by the child’s risk classification. The higher the
blood lead level and the lower the child's age, the higher
the priority for removing the lead hazards. Children who
require hospitalization and chelation therapy are at the
highest risk of permanent neurologic damage from con-
tinued high-level exposure and another episode of lead
toxicity. Therefore, children in the urgent- and high-risk
categories should receive first priority for environmental
investigation and intervention. It is strongly recommend-
~ed that abatement of lead hazards in a hospitalized child’s
home be completed during the first few days of the
"child's hospitalization.
Children in the moderate-risk category are next in pri-
ority. For them, identifying lead hazards and reducing
lead intake are as much a medical necessity as clinical
management. The effectiveness of environmental inter-
vention is judged by the child’s response and not by the
services performed. Environmental management is not
successful or complete until the child's EP and blood lead
levels have declined and stabilized for at least 12 months.
The identification and removal of one source of lead
exposure does not necessarily mean that the child’s expo-
sure to lead has ended.
Because lead is a ubiquitous and powerful toxin, with
.. no known beneficial function in the human body, the
goal of prevention is to reduce children’s exposure to
lead to the maximum extent. Lead-based paint is the
most common, remediable source of lead that causes
symptomatic lead poisoning. Detailed procedures for
removing lead paint from the home environment are de-
scribed, but only general guidelines are given for control-
ling other sources of lead discussed in section III. Ideal
prevention goals are given first, when these goals cannot
be reached immediately, short-term, substitute goals are
offered.
LEAD-BASED PAINT
The ultimate goal is to remove all leaded paint from
housing in the United States. Reaching that goal will be
expensive. Short-term goals of partial removal help, but
they tend to postpone efforts for com plete removal.
All painted interior and exterior surfaces should be tested
for lead. Portable x-ray fluorescence (XRF) analyzers are
most convenient for identifying lead-based paint hazards.
These instruments can measure lead content in paint sur-
faces within £0.2 mg/cm? of exposed surface. Readings
of 0.7 mg/cm? are considered positive. The XRF analyzer
is a probability sampling device, and reliability depends
on repeated readings. If an XRF analyzer is not available,
wet chemical methods of analysis must be used. .
A lead-based paint hazard exists when (a) the XRF
reading is positive and (b) the surfaces being tested are
chewable or contain damaged (cracked, chipped,
loosened, chewed) paint. Lead-based paint on inact
walls, ceilings, or other surfaces that are not chewable
does not constitute an immediate hazard. Inspectors
should obtain measurements on any interior or exterior
surface that may constitute a lead hazard. This includes
walls, doors, window frames, baseboards, guardrails,
fences, and sidings. Outside inspection should encompass
garages and other adjacent structures as well as the main
building.
Next, the inspector should classify each interior and
exterior part of the building where lead is found according
io the degree of hazard. If nonchewable surfaces with
lead paint are smooth and intact and the supporting struc-
ture is sound, they do not present an immediate hazard
and may be left alone. Property owners and residents,
however, should be warned that smooth surfaces contain-
ing lead can become hazardous if they are not properly
maintained and are allowed to fall into disrepair. All lead-
painted surfaces that are identified as positive by XRF (or
wet chemical analysis) and that are in unsound condition
are classified as immediate hazards requiring prompt
abatement. This includes all wood trim —both interior
and exterior— with blistering, scaling, peeling, or powder-
ing paint and walls with unsound paint, painted plaster,
or painted, peeling wallpaper. Floors and ceilings, if paint-
ed with lead-based paint and if in an unsound condition,
are also included.
New information has revealed the importance of lead-
bearing dust as another major hazard for young children.
* In the past, blistering, scaling, peeling, or powdering
paint was frequently removed only to a level of 4 or S feet
above the floor, because, usually, a small child can reach
no higher. However, dust or paint chips from unsound
lead paint above this level could fall into the child's play
area. CDC now recommends that all unsound leaded
paint be removed from the interiors of dwellings, includ-
ing areas beyond the reach of children. Likewise, exterior
leaded paint (on porches, woodwork, and walls) that
either is in or can fall into the child's piay area should be
removed immediately. Places in and about the home
where young children spend much of their
time—namely, near windows, doors, and porches—are
particularly hazardous. :
In summary, paint in unsound condition or on chewa-
ble surfaces is classified as an immediate hazard requiring
prompt abatement: other lead paint in sound condition
may not require immediate attention, but it must be
identified as a potential hazard.
Next, some common methods for reducing lead-based
paint hazards are outlined.
Phase I — Emergency Intervention
As soon as an elevated blood lead level is confirmed,
residents should be advised to remove all scaling paint
from places such as window sills, door frames, doors, and
porch railings that are within easy reach of the child. A
stuff brush should be used for this. Residents should also
be advised (0 avoid inhaling the dust or contaminating
other areas. The debris should be vacuumed and bagged
for safe disposal. Then the area should be thoroughly
scrubbed, preferably with high-phosphate detergents
such as Spic and Span (Milar and Mushak, 1982). If a crib
is next to a surface with scaling paint, the crib should be
moved away. Similarly, a piece of furniture should be
moved to prevent the child from reaching areas of scaling
paint. In the past, it was advised that window sills and
other wood trim with peeling paint be covered with mask-
ing tape or some other adhesive-backed paper. This is no
longer recommended. Inquisitive young children often
remove this tape, thereby rendering the technique inef-
fective. Families should be instructed on ways to keep
these areas free from loose or flaking paint until more
definitive steps can be taken to reduce the hazard. House-
keeping techniques such as frequent wet mopping and
damp dusting are essential in maintaining a reduced level
of hazard.
Phase Il — Long-Term Hazard Reduction
Only when an ofd dwelling with lead-based paint is
gutted and completely restored can the lead hazards be
considered “permanently abated.” Less extensive, com-
monly used procedures may be called “long term”: how-
ever, how long the hazard will remain under control
depends on such factors as the thoroughness of the proce-
dure, the soundness of the underlying structure, and the
condition of the plumbing. Increased moisture from
leaky pipes behind walls can quickly cause paint that was
smooth and intact to blister and scale.
Ee A i le Bs At di — i in
Abatement entails four steps:
1. Removing lead paint from wood trim or walls.
2. Thorough vacuuming to clean up the debris.
3. Wet scrubbing for maximum elimination of fine
lead-bearing particles.
4. Repainting the area with lead-free paint (that is,
paint containing less than 0.06% of {ead in the final
dried solid).
The property owner’s responsibility is not met until all
four steps have been completed.
Just prior to and during abatement, certain precautions
are essential. Carpets, rugs, upholstered furniture, bed-
ding, clothing, and eating and cooking utensils must be
sealed as tightly as possible in plastic to protect them
from the enormous increase in lead-bearing dust created
by the removal procedures. Once items such as rugs are
impregnated with fine, lead-bearing particles, it is almost
impossible to remove the lead (Milar and Mushak,
1982). When feasible, this work should be carried out in
one room at a time, with the room closed off and all fur-
nishings removed. Until steps 1, 2, and 3 of the cleanup
process are completed, all young children and pregnant
women should live elsewhere both day and night. If this
is not possible, they, as well as the child with the index
case, should have serial blood lead tests before, during,
and after the abatement work. Those doing the work
should comply with OSHA standards: they should use re-
spirators and wear coveralls, which must not be taken to
the workers” homes for laundering.
Walls
Removing lead paint from walls, particularly lead paint
applied to plaster, is usually difficult. In most cases, a bar-
rier, such as wallboard, hardboard, fiberglass, plywood
paneling or a similar durable, fire-resistant material, can
be placed over the lead paint on the walls. These materials
must be firmly nailed, cemented, or glued in place to pre-
vent the child from removing them. The barriers should
be verminproof and, in certain areas of the dwelling (that
is, next to furnaces and stoves and in common hallways),
fire retardant. Wallpaper painted with lead paint should
be stripped off to the maximum extent possible.
Woodwork
Lead-based paint in unsound condition on both interi-
or and exterior wood rim (for example, window units,
door units, stair risers, bannisters, and railings) presents
considerable danger for children. Paint can be removed
from wood surfaces by heat (from gas torches and heat
guns), sanding, scraping, and with liquid paint removers.
All of these methods are hazardous. Most solvents in
liquid paint removers evaporate rapidly and are flamma-
ble and toxic. These removers must be used with the
utmost caution and only in well-ventilated areas with
proper protective clothing and equipment. When the un-
derlying wood has rotted, no attempt should be made to
remove the paint. Instead, the wood should be replaced,
including, when necessary, entire window units and
doors or door frames. Exterior rotted wood should also
t replaced. When torches, heat guns, and sanding
¢ vices are used to remove paint, air lead levels increase
enormously in the work area. Of these, sanding is by far
t* = worst offender. It also produces the greatest deposi-
¢ n of lead in dust, with rates as high as 10 mg of lead/sq
fi/hour (Inskip and Attenbury, 1983). Therefore, fine
sanding down to the bare wood surface is not recom-
i ended. Scraping the surface afier a heal gun has been
L.ed will probably produce fewer fine particles than
sanding.
"The above information emphasizes the urgency of
oper cleanup afler lead-based paint has been removed.
After the dust has settled, the entire area, including
+-alls, floors, and ceiling, should be vacuumed, preferably
th an industrial vacuum cleaner. All surfaces should be
wel-scrubbed with phosphate-containing detergents. Im-
mediately thereafier, all surfaces from which paint has
en removed should be repainted with lead-free paint.
{ or safe disposal the debris should be placed in a toxic
waste dump approved by the Environmental Protection
gency, not in an ordinary landfill or storm or sanitary
wer system. For best results, the wet cleaning proce-
dures should be repeated (Milar and Mushak, 1982).
Workers who remove the paint should be responsible for
e cleanup, inasmuch as many of the affected families
t.ave neither the equipment nor the resources to carry
oul an adequate cleanup.
["upplemental Addresses
| . Children often spend substantial amounts of time with
relatives or babysitters who live at a different address. If
*-ad-based paint in unsound condition is found at these
~ idresses, it should be removed in the manner described.
‘Similarly, day-care centers and other facilities may be
located in old buildings with lead-based paint. These, too,
: 1ould be checked and handled accordingly.
.ollowup
The effectiveness of the initial abatement can be deter-
i rined only through coordinated medical and environ-
{ental followup. When the initial abatement has been
inadequate, a high recurrence rate of blood lead levels
~bove 50 ug/dl has been found (Chisolm, 1983). Ideally,
{ communitywide code-enforcement program should be
‘ueveloped to remove all lead-based paint in housing. But,
until then, the appropriate governmental unit in which
{ 1e child lives is responsible for identifying and abating
i ;ad hazards for children with lead toxicity. Removing
lead hazards in housing is the major factor in the success
© [alead poisoning prevention program.
"AIRBORNE LEAD
Blood lead levels are decreasing as the use of leaded
asoline decreases (Annest et al., 1983). In terms of
-reducing background blood lead levels, removing lead
from gasoline as rapidly as feasible is probably rie most
mportant public health measure.
Emissions from industrial sources should be reduced
sufficiently to achieve the current ambient air lead stan-
dard. New factories, as part of their licensing specifica-
tions, should be required to have minimal lead emissions.
The public should be informed about the hazards asso-
ciated with burning old battery casings, colored news-
print, waste oil, and lead-painied wood.
SOIL AND DUST
The optimal goal is 10 prevent lead from being trans-
ferred from any source to soil and dust. For the goal to be
reached, air lead levels must be reduced to near zero. For
those areas where concentrations of lead in soil and dust
are high, large-scale excavation of soil or relocation of
populations is the ideal means of reducing the exposure
of children to lead.
When the lead content of household dust is high, wet-
mopping and other cleanup measures help reduce chil-
dren’s blood lead levels (Charney et al., 1983). These
measures provide a reasonable, shori-term and mid-term
solution to the problem of contaminated house dust.
In severely contaminated residential areas, unless an
effective barrier can be established between the children
and the soil, surface soil must be removed and replaced
with soil having a low lead content. :
FOOD AND WATER
The lead content of air and soil, important contributors
to the contamination of food and water, should be re-
duced. Food cans should be made so that lead does not
leach from soldered seams. Lead is also added inadver-
tently to foods during processing and handling (Wolnik
et al., 1983). Although the percentage of canned foods
packaged in cans with lead-soldered side seams has de-
clined substantially, some are still packaged this way.
These foods should not be stored in the opened cans be-
cause, after the cans have been opened, even more lead
migrates from the side seam into the food.
When feasible, lead plumbing and lead water mains
should be replaced. Water from taps in the home should
be assessed for lead content. If a hazard is found, consum-
ers should be educated to run water for several minutes
before drinking it and not to drink water from the “hot”
side of the tap. Acidic water supplies should be alkalinized
to help prevent leaching.
OCCUPATIONAL
Ideally, engineering features should prevent workers
from being exposed to lead dust »..d vapors. When work-
ers are exposed, compliance with Occupational Safety
and Health Administration (OSHA) regulations appears
to be effective in protecting them and in preventing them
from transporting lead home to children. Under the
OSHA lead standard, factories that use lead must provide
workers with facilities for showering and changing
clothes and shoes before going home from work. This
standard now applies only to industries covered by OSHA
regulations. For the protection of children, it should be
extended to all industries that_use lead. The prevention
of lead exposure to the fetus needs special emphasis.
Women of childbearing age should be excluded from
working at jobs where significant lead exposure occurs.
21
LEAD-GLAZED POTTERY
All glazed pottery used for foodstuff should be free o
leachable lead. Hobbyists and consumers should be
educated to the risks associated with pottery glazes
Consumers should not use pottery for cooking or for stor
ing food or beverages unless the pottery has recent!
been determined to be free of leachable Jead.
¢
$
Fn
p
r
r
e
r
e
e
n
VIII. Health Education
The community and especially parents of preschool
children who live in older, deteriorating neighborhoods
should be informed at every available opportunity of the
need to have children screened periodically for lead
poisoning. Basic preventive measures should be empha-
sized. These include frequent wet mopping and vacuum-
ing of accessible paint flakes and dust to reduce potential
lead hazards in the child's environment. The danger of in-
gesting paint chips, dust, and soil should be stressed.
Older siblings of children at high risk should also be in-
formed about the sources and risks of lead poisoning be-
cause they often take care of younger children.
If a child is screened and the lead level is not elevated,
the risk remains, and until the sixth birthday, rescreening
is required, particularly during the summer. Until hazard-
free housing is available for all and other high-risk
sources of lead are removed, periodic screening will
reduce the risk of lead poisoning.
Education should start when the child is screened, and
physicians, nurses, environmentalists, and aides should
reinforce it at every opportunity. When a child is found to
have lead toxicity, education of the family is essential for
successful followup of the child. The family must be fully
informed about the condition and the clinical and envi-
ronmental actions to follow. Health professionals must
emphasize the importance of the family’s understanding
the child’s condition, its cause, and the possible result of
lead toxicity. In addition, they should stress the impor-
tance of the child’s having a balanced diet that includes
enough calcium and iron.
IX. Reporting Lead Toxicity and
Elevated Blood Lead Levels
Primary care physicians and persons in charge of
- screening programs should report both presumptive and
confirmed cases of lead toxicity to the appropriate health
22
agency, and laboratories performing blood lead or EP
tests should report any abnormal results to the appropri-
ate health agency.
X. References
Angle CR, McIntire MS. Low level and inhibition of
erythrocyte pyrimidine nucleotidase. Environ Res
1978,17:296-302.
Annest JL, Pirkle JL, Makuc D, Neese JW, Bayse DD,
Kovar MG. Chronological trend in blood lead levels
between 1976 and 1980. N Engl J Med 1983;
308:1373-7.
Baker EL Jr, Folland DS, Taylor TA, et al. Lead poison-
ing in children of lead workers: home contamination
with industrial dust. N Engl J Med 1977;296:260-1.
Baker EL Jr, Hayes CG, Landrigan PJ, et al. A nationwide
survey of heavy metal absorption in children living
near primary copper, lead, and zinc smelters. Am J
Epidemiol 1977;106:4.
Barltrop D. The prevalence of pica. Am J Dis Child
1966;112:116-23.
Barltrop D, Khoo HE. The influence of nutritional factors
on lead absorption. Postgrad Med J 1975;51:795-800.
Beattie AD, Moore MR, Devenay WT, et al. Environ-
mental lead pollution in an urban soft water area. Br
Med J 1972;2:491.
Beloian A. Use of a food consumption mode! to estimate
human contaminant intake. Proceedings of the Inter-
national Workshop on Exposure Monitoring. Las
Vegas, Nev., USA, Oct. 19-22, 1981. Environ Monit
Assess 1982;2(1-2):115-28.
Benignus BA, Otto DA, Muller KE, Seipie KJ. Effects of
age and body lead burden on CNS function in young
children: Il. EEG spectra. Electroencephalogr Clin
Neurophysiol 1981;52:240-8.
Billick IH, Shier DR, Curran AS. Relation of pediatric
blood lead levels to lead in gasoline. Environ Health
Perspect 1980;34:213-7.
Blumberg WE, Eisinger J, Lamola AA, Zuckerman DM.
The hematofluorometer. Clin Chem 1977;23(2):
270-4.
Buhrmann E, Mentzer WC, Lubin BH. The influence of
plasma bilirubin on zinc protoporphyrin measurement
by a hematofluorometer. J Lab Clin Med 1978;91(4):
710-6.
Burchfiel JL, Duffy FH, Bartels PH, Needleman HL. The
combined discriminating power of quantitative elec-
troencephalography and neuropsychologic measures
in evaluating central nervous system effects of lead at
low levels. In: Needleman HL, ed. Low level lead
exposure: the clinical implications of current research.
New York: Raven Press: 1980:75-89.
3
Byers RK, Lord EE. Late effects’ of lead poisoning on
mental development. Am J Dis Child 1943:66:471.
Caprio RJ, Margulis HL, Joselow MM. Lead absorption
in children and its relation to urban traffic densities.
Arch Environ Health 1974;28:195-7.
Cavalleri A, Baruffini A, Minoia C, Bianco L. Biological
response of children to low levels of inorganic lead.
Environ Res 1981;25:415-23.
Center for Disease Control (CDC). Increased lead ab-
sorption and lead poisoning in young children: a state-
ment by the Center for Disease Control. Atlanta: US
Department of Health, Education, and Welfare, 1975.
Center for Disease Control (CDC). Preventing lead
poisoning in young children: a statement by the
Center for Disease Control: April 1978. Atlanta: US
Department of Health, Education, and Welfare, 1978.
Charney E, Kessler B, Farfel M, Jackson D. Childhood
lead poisoning: a controlled trial of the effect of dust-
control measures on blood lead levels. N Engl J Med
1983;309(18):1089-93.
Chisolm JJ Jr. Treatment of lead poisoning. Modern
Treatment 1967,4(4):710-28.
Chisolm JJ Jr. The use of chelating agents in the treat-
ment of acute and chronic lead intoxication in child-
hood. J Pediatr 1968;73(1):1-38.
Chisolm JJ Jr. Lead poisoning. Sci Am 1971:224:15-23.
Chisolm JJ Jr. Relationship between level of lead absorp-
tion in children and type, age, and condition of housing
in Baltimore, Maryland, USA. In: Proceedings of the
International Conference on Heavy Metals in the Envi-
ronment: Heidelberg, West Germany. Edinburgh:
CEP Consultants, 1983:vol 1, 282-5.
Daliman PR. Blood and blood forming tissues: red blood
cells. In: Rudolph JM, Hoffman JIE, eds. Pediatrics.
Norwalk, Connecticut: Appleton Century Crofts,
1982:1035-87.
De la Burde B, Choate MS Jr. Does asymptomatic lead
exposure in children have latent sequelae? J Pediatr
1972,81:1088-91.
De la Burde B, Choate MS. Early asymptomatic lead
exposure and development at school age. J Pediatr
1975,87:638-42.
Facchetti S, Geiss F. Isotopic lead experiment: status
report. Brussels-Luxembourg: Office for Official Publi-
cations of the European Communities, 1982.
' JlJdman RG, Hayes MK, Younes R, Aldrich FD. Lead
neuropathy in adults and children. Arch Neurol
. 1977:34:481-8. %
i ammond PB, Bornschein RL, Succop P. Dose-effect
* and dose-response relationships of blood lead to eryth-
rocytic protoporphyrin in young children. Environ Res
(in press), 1984.
skip M, Attenbury N. The legacy of lead-based paint:
potential hazards to “do-it-yourself” enthusiasts and
children. In: Proceedings of the International Confer-
ence on Heavy Metals in the Environment: Heidel-
berg, West Germany. Edinburgh: CEP Consultants,
1983:vol 1, 286-9.
hnson DE, Tillery JB, Prevost RJ. Levels of platinum,
palladium, and lead in populations of southern Califor-
nia. Environ Health Perspect 1975;12:27-33.
aul B, Davidow B, Eng YM, Gewirtz MH. Lead, eryth-
{ rocyte protoporphyrin, and ferritin levels in cord
blood. Arch Environ Health 1983;38:296-300.
Yaul B, Slavin G, Davidow B. Free erythrocyte proto-
porphyrin and zinc protoporphyrin measurements
compared as primary screening methods for detection
of lead poisoning. Clin Chem 1983;29(3):1467-70.
lein M, Namer R, Harpur E. Earthenware containers as
a source of fatal lead poisoning: case study and public
health considerations. N Engl J Med 1970;283:669-72.
Timm SH, Cole BL, Glynn KL, Ullmann WW. Lead con-
¢ tent of milks fed to infants, (971-1972. N Engl J Med
1973,289:574-6.
Tamola AA, Joselow M, Yamane T. Zinc protoporphyrin
(ZPP): a simple, sensitive, fluorometric screening test
for lead poisioning. Clin Chem 1975;21(1):93-7.
Landrigan PF, Baker EL, Himmelstein JS, Stein GF,
. Weddig JP, Straub WE. Exposure to lead from the
Mystic River bridge: the dilemma of deleading. N Engl
J Med 1982,306:673-6.
{ane RE. The care of the lead worker. Br J Ind Med
© 1949;6:125-43.
Langer EE, Haining RG, Labbe RF, Jacobs P, Crosby
EF, Finch CA. Erythrocyte protoporphyrin. Blood
1972;,40(1):112-28.
cin-Fu JS. Preventing lead poisoning in children. Chil-
dren today. Rockville, Maryland: Maternal and Child
Health Service, 1973; DHEW publication no. (HSM)
73-5113.
Mahaffey KR. Nutritional factors in lead poisoning. Nutr
Rev 1981;39(10):353-62.
..ahaffey KR, Annest JL, Roberts J, Murphy RS. Nation-
al estimates of blood lead levels: United States
1976-1980: association with selected defnographic and
socioeconomic factors. N Engl J Med 1982,307:573-9.
Mahaffey KR, Michaelson IA. The interaction between
lead and nutrition. In: Needleman HL, ed. Low level
lead exposure: the clinical implications of current re-
search. New York: Raven Press, 1980:159-200.
Mahaffey KR, Rosen JF, Chesney RW, Peeler JT, Smith
CM, Deluca HF. Association between age, blood lead
concentration, and serum 1,25-dihydroxycholecal-
ciferol levels in children. Am J Clin Nutr 1982:35:
1327-31.
Mahaffey-Six KR, Goyer RA. The influence of iron defi-
ciency on tissue content and toxicity of ingested lead
in the rat. J Lab Clin Med 1972;,79:128-36.
Mantere P, Hanninen H, Hernberg S. Subclinical neuro-
toxic lead effects: two-year follow-up studies with psy-
chological test methods. Neurobehav Toxicol Teratol
1982:4:725-7.
Markowitz ME, Rosen JF. Assessment of lead stores in
children: validation of an 8-hour CaNa;EDTA pro-
vocative test. J Pediatr 1984;104:337-41.
Mielke HW, Anderson JC, Berry KJ, Miclke PW,
Chaney RL, Leech M. Lead concentrations in inner-
city soils as a factor in the child lead problem. Am J
Public Health 1983;73(12):1366-9.
Milar CR, Mushak P. Lead contaminated housedust:
hazard, measurement and decontamination. In: Chi-
solm JJ Jr, O'Hara DM, eds. Lead absorption in chil-
dren: management, clinical, and environmental as-
pects. Baltimore-Munich: Urban & Schwarzenberg,
1982:143-52.
Morse DL, Watson WN, Housworth J, Witherell LE,
Landrigan PJ. Exposure of children to lead in drinking
water. Am J Public Health 1979,69:711-2.
National Academy of Sciences (NAS), Committee on
Toxicology. Recommendations for the prevention of
lead poisoning in children. Washington, D.C.: National
Research Council, July 1976.
National Center for Health Statistics (NCHS). Blood lead
levels for persons ages 6 months-74 years: United
States, 1976-80. Hyattsville, Maryland: US Depart-
ment of Health and Human Services, 1984.
Needleman HL, Gunnoe C, Leviton A, et al. Deficits in
psychologic and classroom performance of children
with elevated dentine lead levels. N Engl J Med
1979;300:689-95.
Needleman HL, Rabinowitz M, Leviton A, Linn S,
Schoenbaum S. The relationship between prenatal
exposure to lead and congenital anomalies. JAMA
1984;251:22.
Osterud HT, Tufts E, Holmes MA. Plumbism at the
Green Parrot Goat Farm. Clin Toxicol 1973;6:1-7.
Otto D, Benignus V, Muller K, et al. Effects of low to
moderate lead exposure on slow cortical potentials in
young children: two-year follow-up study. Neurobehav
Toxicol Teratol 1982;4:733-7. :
Paglia DE, Valentine WN, Fink K. Further observations
on erythrocyte pyrimidinenucleotidase deficiency and
intracellular accumulation of pyrimidine nucleotides. J
Clin Invest 1977,60:1362-6.
Perlstein MA, Attala R. Neurologic sequelae of plumbism
in children. Clin Pediatr 1966,5:292.
Piomelli S. Free erythrocyte porphyrins in the detection
of undue absorption of Pb and of Fe deficiency. Clin
Chem 1977,23(2 Pt 1):264-9.
Piomelli S. Blood lead concentrations in a remote Himala-
yan population. Science 1980;210:1135-7.
Piomelli S, Rosen JF, Chisolm JJ, Graef JW. Manage-
ment of childhood lead poisoning. J Pediatr
1984,105(4):523-32.
Piomelli S, Seaman C, Zullow D, Curran A, Davidow B.
Threshold for lead damage to heme synthesis in urban
children. Proc Natl Acad Sci USA 1982;79:3335-9.
Rabinowitz MB, Needleman HL. Temporal trends in the
lead concentrations of umbilical cord blood. Science
1982;216:25.
Rabinowitz MB, Needleman HL. Petrol lead sales and
umbilical cord blood lead levels in Boston, Massachu-
setts. Lancet 1983;63(1):8314-5.
Rabinowitz MB, Wetherill GW, Kopple JD. Kinetic anal-
ysis of lead metabolism in healthy humans. J Clin
Invest 1976,58:260- 70.
Reeves JD, Yip R, Kiley VA, Dallman PR. Iron deficien-
cy in infants: the influence of mild antecedent infec-
tion. J Pediatr (in press), 1984.
Reigart JR, Whitlock NH. Longitudinal observations of
the relationship between free erythrocyte porphyrins
and whole blood lead. Pediatrics 1976,57:54.
Roels H, Buchet JP, Lauwerys R, et al. Impact of air pol-
lution by lead on the heme biosynthetic pathway in
school-age children. Arch Environ Health
1976,31(6):310-5.
Rosen JF, Chesney RW, Hamstra A, DeLuca HF, Mahaf-
fey KR. Reduction in 1,25-dihydroxyvitamin D in
children with increased lead absorption. N Engl J Med
1980;302:1128-31.
25
Royal Commission on Environmental Pollution. Ninth
report: lead in the environment. Presented to Parlia-
ment by command of Her Majesty. London: Her
Majesty’s Stationery Office, April 1983.
Saenger P, Rosen JF, Markowitz M. Diagnostic signifi-
cance of edetate disodium calcium testing in children
with increased lead absorption. Am J Dis Child
1982;136:312-5.
Sayre JW, Charney E, Vostal J, Pless IB. House and hand
dust as a potential source of childhood lead exposure.
Am J Dis Child 1974;127:167. *
Seppalainen AM, Hernberg S. A follow-up study of nerve
conduction velocities in lead exposed workers. Neuro-
behav Toxicol Teratol 1982:4:721-3.
Winneke G. Neurobehavioural and neuropsychological
effects of lead. Letter. Lancet. Sept 4, 1982:550.
Wolnik KA, Fricke KL, Caspar SG, et al. Elements in
major raw agricultural crops in the United States. I.
Cadmium and lead in lettuce, peanuts, potatoes, soy-
beans, sweet corn and wheat. J Agric Food Chem
1983;31:1240-4.
World Health Organization (WHO), Task Group on En-
vironmental Health Criteria for Lead. Environmental
health criteria 3: lead. Geneva: WHO, 1977,
Yip R, Schwartz S, Deinard AS. Screening for iron defi-
ciency with the erythrocyte protoporphyrin test.
Pediatrics 1983;72:214-9. .
Yule W, Lansdown R, Millar IB, Urbanowicz MA. The
relationship between blood lead concentrations, intelli-
gence and attainment in a school population: a pilot
study. Dev Med Child Neurol 1981:23:567-76.
Appendn
Reprinted by the
U.S. DEPARTMENT oS HEALTH AND HUMAN SERVICES
PUBLIC HEALTH SERVICE
from the Journal of Pediatrics, Volume 105, October 1984, Number 4, pp. 523-832
SPECIAL ARTICLE
Management of childhood lead poisoning
Sergio Piomelli, M.D., John F. Rosen, M.D, J. Julian Chisolm, Jr., M.D,,
and John W. Graef, M.D. New York, New York, Baltimore, Maryland,
and Boston, Massachusetts
CHELATION TREATMENT for childhood lead poisoning
may be life-saving and decreases the body burden of lead
far more rapidly than normal excretory processes can.'
Furthermore, chelating agents markedly enhance removal
of that fraction of body lead that is readily mobile and
considered to be the most toxic.'* However, lead poisoning
is a wholly preventable disorder caused by the wide
dissemination of lead into the emvironment.’' Medical
treatment with chelating agents must not be considered a
substitute for dedicated preventive efforts to eradicate
controllable sources of lead (e.g., substandard housing that
contains lead-bearing paints, combustion of leaded gaso-
line). Although repeated courses of chelation therapy may
be necessary for medical reasons, the source(s) of enviroa-
mental lead must be identified and removed for preventive
reasons.
This review is based on our experience in four different
lead poisoning treatment clinics and reflects our consensus
on current management criteria.
PHARMACOLOGIC CONSIDERATIONS
Lead poisoning is treated with drugs capable of binding
(chelating) lead and of enhancing its excretion. These
From the Division of Pediatric Hematology/Oncology. Depari-
ment of Pediatrics. Columbia University, College of Physicians
and Surgeons; the Department of Pediatrics and Clinical
Research Center, Albert Einstein College of Medicine. Monte-
fiore Medical Center: the Department of Pediatrics, John Hop-
kins University School of Medicine and the John F. Kennedy
Institute, and the Baltimore City Hospitals; and the Division of
Clinical Pharmacology and Toxicology, Department of Pediat-
rics, Children’s Hospital Medical Center.
Supported by Grant ES02343 from the National Institutes of
Health, and by a grant from the Francis Florio Fund of the New
York Community Trust (S.P.); by Projects 917 and MCJ-240458.
Maternal and Child Health, Department of Health and Human
Services (J.J.C.); and by Grants ES01060-09 and RR-53 from the
National Institutes of Health, and by Project MCJ-360488-01,
Maternal and Child Health, DHHS (J.F.R.).
Reprint requests: Sergio Piomelli, M.D., Columbia University,
College of Physicians and Surgeons, Division of Pediatric Hema-
tology/Oncology, 630 West 168th St., New York. NY 10032.
26
drugs deplete the soft tissues of lead and may thus reduce
its acute toxicity. They are also used, in asymptomatic
children, to reduce a potentially dangerous body burden of
lead. All drugs are used to enhance the slow process of
natural lead excretion. All drugs have potential side effects
and should be used carefully. A brief description of the
essential pharmacologic aspects of the various drugs fol-
lows. Detailed guidelines for specific situations are given in
the next section.
BAL
Mechanism of action. Two molecules of BAL combine
with one atom of heavy metal to form a stable complex.
BAL enhances fecal as well as urinary excretion of lead
and diffuses well into erythrocytes. It can be administered
in the presence of renal impairment because it is predomi-
nantly excreted in bile.’
BAL (British anti-lewisite) Dimercaptopropanol
CaNa,-EDTA Disodium calcium-edetate
EP Erythrocyte protoporphyrin
G-6-PD Glucose-6-phosphate dehydrogenase
Route of administration and dosage. BAL is available
only in oil for intramuscular administration. It must be
given every 4 hours. Dosages are discussed below.
Toxicity. Mild febrile reactions may occur, and tran-
sient elevation of hepatic transaminase activities may be
observed. Other minor adverse effects include, in order of
frequency, nausea and occasional vomiting, headache,
mild conjunctivitis, lacrimation, rhinorrhea, and salivation.
Most side effects are transient and rapidly subside as the
drug is metabolized and excreted.
Precautions. In patients with G-6-PD deficiency, BAL
should be used only in life-threatening situations, because
it may induce hemolysis. Medicinal iron should never be
administered during BAL therapy, because the combina-
tion is very toxic. If iron deficiency coexists, its manage-
ment should be postponed until BAL therapy is concluded.
In cases of extreme anemia blood transfusions are prefer-
able.
CaNa,-EDTA**
Only CaNarEDTA (calcium disodium versenate)
should be used for treatment of lead poisoning. Na,
EDTA (endrate disodium) should never be used Jor
treatment of lead poisoning, because it may induce fatal
hypocalcemia and tetany.
Mechanism of action. CaNa,-EDTA increases urinary
lead excretion 20- to 50-fold. CaNa,-EDTA does not enter
the cells; thus it removes lead from the extracellular
compartment. Indirectly, lead is reduced in the soft tissue,
central nervous system, and red blood cells.’
Route of administration and dosage. CaNa,-EDTA
may be given intravenously or intramuscularly. The pre-
ferred and most effective route is a continuous intravenous
infusion; a given dose is most effective if infused over 6
hours." CaNa,-EDTA should be diluted to a concentration
<0.5% in dextrose and water or 0.9% saline solution. When
administered intravenously as a single dose, it should be
similarly diluted and administered by slow infusion over 15
to 20 minutes. Intramuscular administration of CaNa,-
EDTA is extremely painful and should be given with
procaine (0.5%) by deep injection.
CaNa,-EDTA should not be given orally, because it may
enhance absorption of lead from the gastrointestinal
tract.
Dosages vary in different situations and are discussed
below. In all cases, courses should be limited to § days,
followed by at least 2- to 5-day intervals to allow recovery
from zinc depletion.
Toxicity. The kidney is the principal site of toxicity.
Renal toxicity is dose related, reversible, and rarely occurs
at doses <1500 mg/m’. The renal toxicity may be reduced
by assuring adequate diuresis. CaNa,-EDTA should never
be given in the absence of an adequate urine flow. Before
administering it intramuscularly in children in good clini-
cal condition, adequate oral intake of fluids must be
assured.
Precautions. Dermg chelation with CaNa,-EDTA,
urine and its sediment, BUN, serum creatinine, and liver
function tests must be carefully monitored. The appear-
ance of protein and formed elements in urinary sediment,
and rising BUN and serum creatinine values signify
impending renal failure, the serious toxicity associated
with excessive or prolonged administration of EDTA.
Inasmuch as CaNa,-EDTA may deplete zinc stores and
cellular injury may be associated with zinc depletion,
CaNa,-EDTA should be used with great caution.
CaNa,-EDTA, used alone without concomitant BAL
therapy, may aggravate symptoms in patients with very
high blood lead levels. Thus it should be used exclusively in
conjunction with BAL when the blood Jead level is >70
ug/dl or clinical symptoms consistent with lead poisoning
are present. In such cases the first dose of BAL should
always precede the first dose of CaNa,-EDTA by at least 4
hours.
D-Pesicillamine. D-Penicillamine is not licensed by the
Food and Drug Administration for the treatment of lead
poisoning. Its use for this indication is thus to be consid-
ered experimental. It is the only commercially available
oral chelating agent. It can be given over a long period
(days). Toxic side effects may occur in as many as 20% of
patients given the drug."
Mechanism of action. D-Penicillamine enhances erin
excretion of lead, although not as effectively as CaNa,-
EDTA. Its specific mechanism of action is not well
understood.
Route of administration and dosage. D-Penicillamine is
administered orally. It is currently available in capsules
(125 and 250 mg). These capsules may be opened and
suspended in liquid, if necessary. The usual dose is 30
mg/kg. Side effects can be minimized by initiating therapy
with small doses, for example, 25% of the desired final
dose, increased after | week 10 50% and again after | week
to the full dose, while monitoring for possible toxicity.
Toxicity. The main side effects of D-penicillamine are
reactions resembling those of penicillin sensitivity, includ-
ing fevers, rashes, leukopenia, thrombocytopenia, and
eosinophilia. Rarely, more severe and even life-threatening
reactions (autoimmune hemolytic anemia, Stevens-John-
son syndrome) have been observed. Anorexia, nausea, and
vomiting are infrequent. Of most concern, however, are
isolated reports of nephrotoxicity, possibly from hypersen-
sitivity reactions. For these reasons, patients should be
carefully and frequently monitored for clinically obvious
side effects, and frequent blood counts, urinalysis, and
renal function tests should be performed. In particular,
blood counts and urinalysis should be done twice weekly, at
least in the first 3 weeks of treatment. If the absolute
neutrophil count falls to <1500/ul it should be immediate-
ly rechecked, and treatment should be stopped if it falls to
<1200/ul. D-Penicillamine should therefore not be given
on an outpatient basis if there is any question about
compliance with appointments.
D-Penicillamine should not be administered in patients
with known penicillin allergy.
New agents. Dimercaptosuccinic acid and 2-3-dimer-
capto-propane-i-sulphonate are both water-soluble deriva-
tives of BAL. Although both appear promising and safe
and have been used successfully in treatment of other
heavy-metal poisoning, ‘these drugs are presently in the
investigative stage for the treatment of lead poison-
ing.'*"
ACUTE LEAD ENCEPHALOPATHY
Acute lead encephalopathy is characterized clinically by
some or all of the following symptoms: coma, seizures,
bizarre behavior, ataxia, apathy, incoordination, vomiting,
alteration in the state of consciousness, and subtle loss of
recently acquired skills. Any cae or a matrix of these
symptoms associated with an elevated biocod lead concen-
tration constitutes an acute medical emergency. Lead
encephalopathy is almost always associated with a8 blood
lead concentration >100 wg/dl, although it has been
reported at blood lead levels as low as 70 4g/dl."*
Geoeral supportive management. All oral intake is pro-
hibited initially until the child's condition has significantly
improved. Parenteral fluid therapy is begun immediately;
volume is restricted to basal requirements plus a careful
assessment of continuing losses. Excessive intravenous
fluid administration must be avoided. Once urine flow is
established by administering dextrose in water (10 to 20
ml/kg body weight), chelation treatment, already begun
with BAL alone for one dose, is continued with simulta-
neous administration of CaNa, EDTA. An adequate flow
of urine must be established before intravenous chelation
therapy. Parenteral fluid therapy minimizes vomiting that
may accompany administration of BAL and ensures
prompt excretion of CaNa,-EDTA, a drug excreted exclu-
sively by the kidney. For imitial comtrol of seizures,
diazepam or paraldechyde is the preferred drug. Barbitu-
rate and phenytoin are reserved for the long-term manage-
ment of recurring seizures, only after the acute episode is
managed and consciousness has been fully recovered.
Although it is desirable to evacuate any residual lead from
the bowel, this should not delay the start of chelation
therapy. Surgical decompression and hypertonic solutions
to relieve intracranial pressure and cerebral edema are
contraindicated.
The diagnosis of acute lead encephalopathy can usually
be made without lumbar puncture, which is extremely
risky because of the presence of increased intracranial
pressure. In fulminant lead encephalopathy, increased
intracranial pressure may be present in the absence of any
of the usual preliminary signs (changes in blood pressure,
pulse or respiration, retiral hemorrhage or edema). If
examination of the CSF is absolutely cesential for the
differential diagnosis, the very least amount of fluid, not
exceeding a few drops, should be carefully obtained.
Chelation therapy. Treatment is begun with a priming
dose of 75 mg/m? BAL only, given by deep intramuscular
injection; BAL is administered at a dose of 450 mg/m?/24
hours, in divided doses of 75 mg/m?’ every 4 hours. Once
the priming dose is given and an adequate urine flow is
established, administration of CaNa,-EDTA is begun at a
28
dose of 1500 mg/m?/24 hours. CaNa,;-EDTA is given by
continuous intravenous drip in dextrose and water or 0.9%
saline solution. The concentration of CaNa;-EDTA should
not exceed 0.5% in the parenteral fluid. (In the treatment
of acute encephalopathy, restriction of parenteral fluids
takes precedence, so that CaNa;-EDTA may have to be
given intramuscularly if fluid overload is 10 be avoided.)
Combined BAL-CaNa,- EDTA therapy is given for a to-
tal of S days. During treatment, renal and hepatic func-
tion and serum electrolyte levels should be monitored
daily.
A second course of chelation therapy with CaNa,
EDTA alone or with BAL, depending on the blood lead
concentration, may be required after a 2-day interval. A
third course is required only if the blood lead concentration
rebounds to a value =50 ug/dl within 48 hours after
treatment. Unless there are compelling clinical reasons, it
is desirable to wait at least 5 to 7 days before beginning a
third course of CaNa,EDTA.
SYMPTOMATIC LEAD POISONING
WITHOUT ENCEPHALOPATHY
Symptomatic lead poisoning without encephalopathy is
characterized by one or several of the following symptoms:
decrease in play activity, lethargy, anorexia, sporadic
vomiting, intermittent abdominal pain, and constipation.
Symptomatic lead poisoning is usually associated with a
blood lead concentration >70 ug/dl, although occasionally
may be associated with a blood lead concentration as low
as 50 ug/dl. If the blood lead concentration is <50 ug/dl,
other diagnostic possibilities should be vigorously sought.
Because all symptomatic children potentially have acute
lead encephalopathy, treatment and supportive mea-
sures must be instituted immediately on an emergency
basis.'*
Genera) supportive management. All oral intake is pro-
hibited and the guidelines of parenteral fluid therapy are
followed as noted above for the treatment of lead enceph-
alopathy. Intravenous fluids are given at a rate consistent
with basal requirements plus ongoing losses. Excessive
fluid administration must be avoided.
Chelation therapy. Treatment is begun with a priming
dose of 50 mg/m? BAL by deep intramuscular injection;
BAL is administered at a dose of 300 mg/m?/24 hours in
divided doses of 50 mg/m’ every 4 hours. Once the priming
dose is given and an adequate urine flow is established,
administration of CaNa,-EDTA is begun at a dose of 1000
mg/m?/24 hours. CaNa,-EDTA is given by continuous
intravenous drip in dextrose and water or 0.9% saline
solution. Although continuous infusion of CaNa,-EDTA is
preferable, it may be replaced by doses of 175 mg/m’ every
4 hours, given either intravenously over 15 to 20 minutes
through a heparin lock or by deep intramuscular injection
mixed with procaine. The concentration of CaNa,-EDTA
should not exceed 0.5% in the parenteral fluid. Combined
BAL-CaNa,-EDTA therapy is given for a total of S
days.
During treatment, renal and hepatic function and serum
electrolyte levels should be monitored daily. It is advisable
to measure the blood lead concentration daily. (It will be
necessary 10 interrupt the CaNa,-EDTA infusion for 1
hour before this sample is obtained, to avoid a spuriously
high value). If the blood lead concentration reaches <$0
ug/dl, as it may within 3 days of combined BAL-
CaNa.-EDTA therapy, BAL may be safely discontinued
and CaNa,-EDTA continued for a full 5-day course of
treatment. If measurements of blood lead cannot be
obtained in time, it is safe to continue BAL for the full
5-day course. Except under highly unusual circumstances,
CaNa,-EDTA should not be administered for more than 5
consecutive days.
A second course of chelation therapy may be required
after a 2- 10 4-day interval, to be started with CaNa.-
EDTA alone or with concomitant BAL, depending on the
blood lead concentration. A third course may be required if
the blood lead concentration rebounds to a value =50
#g/dl within 7 to 10 days after treatment. Unless there are
compelling clinical reasons, it is highly desirable to allow $
to 7 days before beginning a third course of CaNa.-
EDTA.
ASYMPTOMATIC CHILDREN WITH
INCREASED BODY BURDEN OF LEAD
Although children with increased body burden of lead
are clinically asymptomatic, it is likely that they have
pervasive metabolic effects involving heme synthesis,”
red cell nucleotide metabolism, vitamin D and cortisol
metabolism’ and renal function," * and subclinical neu-
robehavioral effects." Some of these profound metabolic
and cellular effects of lead have been observed at blood
lead concentrations <25 ug/d1.? 3 0
Diagnostic assessment. In asymptomatic children it is
essential to have a firm diagnosis based on an elevated
blood lead level before treatment is initiated. Measure-
ments of blood lead concentration in capillary samples are
subject to contamination and should never be the only basis
for treatment. Treatment should be initiated only after a
confirmatory measurement of the venous blood lead con-
centration. Even when there is strong additional evidence
of lead poisoning. such as paint flakes in the abdomen or
lead lines in the bones on x-ray examination, it is prefera-
ble to wait for a confirmatory measurement of venous
blood lead. Although measurements of erythrocyte proto-
porphyrin may be helpful in evaluating overall toxicity,
29
blood lead measurement is the criterion on which to base a
decision as to whether chelation therapy should be consid-
ered. (The EP may increase initially during chelation
therapy.) Therapeutic decisions should also be based on
the results of the CaNa,-EDTA provocative test.
Chelation therapy
Blood lead concentration 270 ug/dl. If the blood lead
level is =70 ug/dl, BAL and CaNa,-EDTA shouid be
given, in the same doses and with the same guidelines as
for treatment of symptomatic lead poisoning without
encephalopathy.
A second course of chelation therapy with CaNa,-
EDTA alone may be required if the blood lead concentra-
tion rebounds to a value = 50 ug/dl within Sto 7 days after
treatment. Unless there are compelling clinical reasons, it
is highly desirable to allow at least § to 7 days before
beginning a second course of CaNa,-EDTA.
Blood lead concentration 56 to 69 ug/dl. If the blood
lead value is between 56 and 69 ug/dl. treatment shoild be
limited to CaNa,-EDTA only.
CaNa,-EDTA is given for 5 days at a dose of 1000
mg/m’/day, preferably by continuous infusion (or in
divided doses intravenously as above). Alternatively, how-
ever, if environmental control of the lead hazards has been
achieved, this treatment may be given on an outpatient
basis, at a dose of 1000 mg/m?/day, preferably by intrave-
nous infusion over | hour, with adequate hvdration (250
ml/m’). As a least preferable option, CaNa.-EDTA may
be administered intramuscularly mixed with procaine, at
the same single daily dose of 1000 mg/m’ for 5 consecu-
tive days. This route of administration may represent a
painful but practical alternative, when circumstances dic-
tate it.
During treatment, renal and hepatic function and serum
electrolyte levels should be monitored. A blood lead
concentration should bec obtained at 72 hours of treatment
(it will be necessary to interrupt the CaNa,-EDTA infu-
sion for 1 hour before this sample is obtained. to avoid a
spuriously high value) to monitor the effectiveness of
treatment.
CaNa.-EDTA treatment should be continued for days.
Except under highly unusual circumstances, it should nat
be administered for more than S consecutive days.
A second course of chelation therapy, with CaNa.-
EDTA alone, may be required if the blood lead concentra-
tion rebounds 10 a value > 50 ug/dl within Sto 7 days after
treatment. Unless there are compelling clinical reasons, it
is highly desirable to allow a period of S to 7 days before
beginning a second course of CaNa,-EDTA.
Blood lead concentration 25 to 55 ug/dl. When the
blood lead value is persistently between 25 and 55 ug/dl
and accompanied by EP persistently >35 ug/dl, the
decision to proceed with chelation therapy should be based
Table. Choice of chelation therapy based on symptoms and blood lead concentration
Comments
Clinical presentation Treatment
Symptomatic children
Acute encephalopathy
BAL 450 mg/m?/day
CaNa,-EDTA 1500 mg/m’/day
Other symptoms
BAL 300 mg/m?/day
CaNa,-EDTA 1000 mg/m?/day
Asymptomatic children
Before treatment, measure venous blood lead.
Blood Pb >70 ug/dl
BAL 300 mg/m?/day
CaNa,-EDTA 1000 mg/m?/day
Blood Pb 56 to 69 ug/dl
CaNa, EDTA 1000 mg/m*/day
Biood Pb 25 to SS ug/dl
If ratio >0.70
If ratio 0.60 to 0.69
Age <3 years of age
Age >3 years of age
CaNa,-EDTA 1000 mg/m?!/day
CaNa,-EDTA 1000 mg/m?/day
No treatment
If ratio <0.60 No treatment
Start with BAL 75 mg/m? im every 4 hours.
Alter 4 hours start continuous infusion of CaNa,-EDTA 1500
mg/m’/day.
Therapy with BAL and CaNa;-EDTA should be continued for
S$ days.
Interrupt therapy for 2 days.
Treat for S$ additional days, including BAL if blood Pb remains
high.
Other cycles may be needed depending on blood Pb rebound.
Start with BAL 50 mg/m? im every 4 hours.
After 4 hours start CaNa,-EDTA 1000 mg/m?/day, preferably
by continuous infusion, or in divided doses Iv (through a
heparin lock).
Therapy with CaNa,-EDTA should be continued for S days.
BAL may be discontinued after 3 days if blood Pb <50 ug/dl.
Interrupt therapy for 2 days.
Treat for § additional days, including BAL if blood Pb remains
high.
Other cycles may be needed depending on blood Pb rebound.
Start with BAL 50 mg/m? iM every 4 hours.
After 4 hours start CaNa,-EDTA 1000 mg/m?/day, preferably
by continuous infusion, or in divided doses iv (through a
heparin lock).
Treatment with CaNa,-EDTA should be continued for 5 days.
BAL may be discontinued after 3 days if blood Pb <50 ug/dl.
Other cycles may be needed depending on blood Pb rebound.
CaNa,-EDTA for S days, preferably by continuous infusion, or
in divided doses (through a heparin lock).
Alternatively, if lead exposure is controlled, CaNa,-EDTA may
be given as a single daily outpatient dose Im or Iv.
Other cycles may be needed depending on blood Pb rebound.
Perform CaNarEDTA provocation test 10 assess lead excretion ratio (see text).
Treat for S days iv or Im, as above.
Treat for 3 days iv or IM, as above.
Repeat blood Pb and CaNa,-EDTA provocation test
periodically.
Repeat blood Pb and CaNa,-EDTA provocation test
periodically. :
on positive findings of a carefully performed CaNa,-
EDTA provocation test. (It must again be emphasized that
chelation therapy should complement, not replace, abate-
ment of controllable lead sources.)
CsNs,-EDTA PROVOCATION TEST. First, a repeated base-
line blood lead level is obtained and the patient is asked to
empty the bladder. Then CaNa,-EDTA is administered at
a dose of 500 mg/m’ intravenously in 250 ml/m’ of 5%
dextrose, infused over 1 hour. (A painful but practical
hn
alternative is to administer the same dose intramuscularly
mixed with procaine and to encourage the child to drink as
much as possible in the first 2 hours). All urine must be
collected with lead-free equipment over 8 hours. The urine
volume should be carefully measured, and aliquots should
be sent to the laboratory for measurement of the concen-
tration of lead. Extreme care should be exercised to use
only lead-free equipment. If this is not available in the
clinic, it may be best that the entire urine volume be sent to
bet
O
o
Le
ad
E
x
c
r
e
t
e
d
/
E
D
T
A
A
d
m
i
n
i
s
t
e
r
e
d
(u
g/
mg
)
O
o
o
0
O
O
N
Ww
W
b
w
1 hd 1 1
40.0 500 60.0 700
Blood Lead (ug/dl)
Figure. Lead excretion ratio as a function of blood lead. Data ex
ratio (ug lead excreted/mg EDTA administered) versus
Data shown were obtained by different techniques. At Columbia
a dose of 50 mg/kg. followed by 250 ml/m? 5% dextrose
pressed as decimal logarithm of CaNa,-EDTA excretion
blood lead. There is a significant correlation (r = 0.466, P < 0.001), with a slope of 0.014 and an intercept of —0.95.
received CaNa,-EDTA as a 20-minute intravenous infusion at
over | hour; urine was collected for 7 to 8 hours. At Albert
hospitalized children received CaNa,-EDTA intramuscularly
for 8 hours. At John Hopkins University School of M
intramuscularly at a dose of 25 mg/kg at 0 and 12 hours: urin
Center, 46 children in the outpatient clinic received CaNa,
University, 77 children in an outpatient setting
Einstein College of Medicine (Montefiore Hospital), 37
with procaine at a dose of S00 mg/m’; urine was collected
edicine. 50 hospitalized children received Ca Na,-EDTA
¢ was collected for 24 hours. At Children’s Hospital Medical
-EDTA intramuscularly with procaine at a dose of 50 mg/kg: urine was collected for 6 10 7 hours. Despite these differences, slopes and intercept of regression lines were remarkably similar: excretion ratio makes the CaNa,-EDTA provocation test independent of both the dose administered and the child's age and body weight. Therefore, data could be poo
to the best of our knowledge, the largest series of CaNa
a laboratory where the volume can be measured with
lead-free equipment and aliquots for lead and creatinine
measurements can be taken without contaminating the
sample.
INTERPRETATION OF CaNa,-EDTA PROVOCATION TEST.
The concentration of lead in the urine (in micrograms per
milliliter) is multiplied by the volurhe (in milliliters), to
obtain the total excretion (in micrograms). The total
urinary excretion of lead (micrograms) is divided by the
amount of CaNa,-EDTA given (milligrams) to obtain the
“lead excretion ratio”:
Lead excreted (ug)
CaNa,-EDTA given (mg)
The CaNa,-EDTA provocation test is considered positive
if the lead excretion ratio exceeds 0.60.
The recommendations of the authors are based on their
experience with 210 provocation tests'’ $2.1 (Figure).
31
led together in a single regression line. Combined data represent,
+-EDTA provocation tests in children.
Inspection of the Figure shows that a ratio >0.60 is never
obtained in 12 children with blood lead level <30 ug/dl,
and is always obtained in 19 children with blood lead level
>60 ug/dl. At blood lead level 30 to 39 ug/dl, the ratio is
>0.60 in six (11.5%) of 52 children; at blood lead level 40
to 49 ug/dl the ratio is >0.60 in 25 (37.9%) of 66 children;
and at blood level 50 to 59 ug/di the ratio is >0.60 in 30
(49.2%) of 61 children.
It appears, therefore, that a ratio <0.60 represents an
appropriate cutoff point to distinguish children with
“markedly increased” excretion. (It is not possible to
define a normal excretion range because no data are
available and it would be unethical to obtain them in
children with blood lead values <25 ug/dl. In addition,
even the lower blood lead levels observed in children from
industrialized countries are significantly higher than those
in children from remote areas uncontaminated by lead,
which most likely represent the truly normal blood lead
level. However, extrapolation from these data predicts, at
blood lead level 1 ug/dl, an excretion ratio of 0.1, six times
lower than the proposed cutoff of 0.60).
GUIDELINES FOR TREATMENT BASED ON CaNa,-EDTA
PROVOCATION TEST. If the lead excretion ratio is >0.70, a
5-day course of CaNa,-EDTA 1000 mg/m’ intramuscu-
larly or intravenously should be given, as above.
If the lead excretion ratio is between 0.60 and 0.69, (1)
children younger than 3 years should receive treatment for
3 consecutive days with 1000 mg/m’ CaNa,-EDTA, as
discussed above; and (2) in children older than 3 years the
test should be repeated every 2 to 3 months and treatment
started if the lead excretion ratio increases to >0.70 (in
which case treatment shall consist of 3 days with 1000
mg/m? CaNa,-EDTA, as above).
In children who have received chelation therapy, re-
peated cycles are indicated if the blood lead concentration
rebounds to within § ug/dl of the original value, 7 to 10
days after treatment.
In all children, regardless of age, with elevated blood
lead and EP values but with an excretion ratio <0.60,
blood lead and EP should be monitored frequently. If the
elevation of blood lead values persists, the CaNa,-EDTA
provocation test should be repeated periodically (every 2 to
3 months).
IMMEDIATE TREATMENT FOLLOW-UP
The goal of chelation therapy is to permanently reduce
the blood lead level to <25 ug/dl and that of EP to <35
ug/dl. To achieve this goal it may be necessary to give
several courses of treatment. It cannot be overemphasized,
however, that repeated courses of therapy are counterpro-
ductive unless the source of lead has been identified and
eradicated. Children receiving chelation therapy should
not be released from the hospital until all lead hazards in
their homes and elsewhere have been controlied and
eliminated and, if necessary, suitable alternative housing
has been arranged. With vigorous public health measures
complete and safe abatement should be achieved during
the treatment period.® If a child with elevated blood lead
concentration cannot be moved to new housing, multiple
repeated courses of CaNa,-EDTA in a clinically asymp-
tomatic child with stable blood lead values may be coun-
terproductive; parents may despair at the ineffectiveness of
therapy and fail to return to the clinic. It is more important
in these unfortunate situations to maintajn follow-up so
that a rise in blood lead concentrations is detected prompt-
ly.
At the end of each treatment cycle the blood lead
concentration usually declines to values <25 ug/dl. How-
ever, within a few days reequilibration takes place and
results in a rebound; thus the blood lead level must be
rechecked 7 to 10 days after the end of treatment.
32
If the blood lead level rebounds to within S ug/dl of the
value before the last cycle, additional treatment cycles are
indicated (unless the concentration after rebound is <25
ug/dl). A blood lead concentration that rebounds to above
the pretreatment value is evidence of renewed and exces-
sive intake. :
If the blood lead level remains low, its measurement
must be repeated, initially biweekly, then at monthly
intervals, to assure that the decreased level is permanent.
Iron deficiency states, which may accompany lead
poisoning, require therapeutic doses of iron in addition to
the correction of other possible nutritional deficiencies.
LONG-TERM CLINICAL FOLLOW-UP AND
MANAGEMENT
The vast majority of children with lead poisoning now
referred to pediatricians from screening clinics are asymp-
tomatic. Acute lead encephalopathy is rare. Lead poison-
ing (with or without clinical symptoms) should be re-
ported to the local health authorities, who usually have
prime responsibility for environmental investigation and
abatement of lead hazards in the home or elsewhere.
Because lead has been widely disseminated into the
environment, thereby providing multiple opportunities for
repeated overexposure, lead poisoning should be managed
as a chronic disorder. A team approach involving public
health personnel, pediatrician, pediatric nurse practitioner,
and social worker is likely to be the most effective.
Commonly this can be accomplished best if children with
lead poisoning are referred for long-term follow-up to a
special clinic where all phases of clinical management can
be coordinated and continuity of care is maintained.
At the outset, a long-term plan of management is
developed. Age, the intensity of hand-to-mouth activity,
pica, diet modification, environmental exposure, and serial
laboratory data are taken into account. The objectives are
to reduce the body burden of lead and to prevent recur-
rences. All preschool-aged housemates of index cases
should be examined. All cases should be reported to social
service for assistance in obtaining safe housing. Extended
follow-up to at least 6 years of age is usually necessary.
Identification of lead source(s). In all cases, first priority
is given to identification of important sources of excess
lead in the child's environment and prompt separation of
the child therefrom.* A thorough history can facilitate the
identification and abatement of thr most important
sources of lead. Although this crucial part of therapy
(abatement) is usually performed by health department
personnel, not uncommonly information obtained in the
clinic provides clues to unsuspected sources. The environ-
mental history obtained in the clinic should include a list of
all dwellings currently or recently visited by the child
(primary residence, homes of relatives and baby sitters,
schools, daycare centers) and evaluation of each building's
age and state of repair. In the United States a high
proportion of buildings constructed prior to 1960 have
lead-bearing paints and putty on both exterior and interior
areas accessible to the child. Structures in poor repair often
have lead-containing chips er pulverized fragments in the
household dust. Play areas, especially urban playgrounds
near vehicular traffic, dirt playgrounds and dm yards,
painted metal fences and walls, and vacant lots formerly
containing lead-painted structures should be identified as
potential lead sources. Occupational histories for all adults
in various dwellings should be ascertained to learn if any
are working in lead-related industries. Lead trades include,
but are not limited to, secondary lead smelting (recovery of
lead from old storage batteries), lead scrap smelting,
storage battery manufacturing and repair, metal founding,
ship breaking, automobile assembly and body and radiator
repair, demolition of painted metal structures (such as
bridges), and demolition and renovation of old houses and
other structures. Adults who work in lead industries must
shower before coming home and must leave all work
clothes, including shoes, at the work place; these clothes
must not be cleaned or washed at home. Thus lead-bearing
dust from the place of employment will not contaminate
the house. Additional sources may include old lead-painted
cribs and beds and the burning of iead-painted wood in
wood-burning stoves. Proximity to lead smelters, ingestion
of lead-containing dust, and inhalation of lead from the
combustion of gasoline contribute to the overall body
burden of lead in children, but the high concentration of
lead that ultimately results in clinical lead poisoning is
most frequently associated with ingestion of Jead-bearing
paint. Uncommon causes of poisoning include ingestion
and retention in the stomach of metallic lead (fishing
weights, curtain weights, shot, jewelry painted with lead to
simulate pearl), contamination of acidic foods and bever-
ages from improperly lead-glazed ceramic pitchers, pots,
and cups and from opened lead-soldered food cans, and the
home burning of battery casings. Inhalation of fumes
(sniffing) from small leaded-gasoline containers has
occurred in older children. Poisoning has also been traced
to oriental cosmetics (surma, a black eyeliner containing
up to 85% lead) and to Mexican and Oriental folk
remedies (azarcon, greta, paylooah).
Medical management during abatement of lead paint
hazards. If the source of lead is limited to such items as
retention of a metallic lead object in the stomach or an
improperly lead-glazed food or beverage container, the
child can be promptly separated from the source. Such is
not the case when lead paint in the home is the principal
source. Several methods are used to remove old lead-based
33
paint from walls and woodwork. Some methods, particu-
larly removal by burning and sanding, greatly increase the
amount of air and dustborne lead in the home. Very fine
lead-bearing particulates settle out slowly over many hours
after burning and sanding is completed. 1 is of the utmost
importance to remove all young children and pregnant
women from a dwelling until the abatement process is
completed. They should live elsewhere day and night, and
should not return until removal of all lead-bearing paint
has been completed and the dwelling has been thoroughly
vacuumed and scrubbed with high-phosphate-detergent
solutions. The sources that have been denuded during the
abatement process should be repainted to seal any residual
lead behind the surface. Children should be removed from
the home during abatement whether or not they have
increased lead absorption. When this procedure is not
followed, it is not uncommon to observe 30 to 50 ug/dl
increments in whole blood lead concentration within a
matter of a few days or weeks.
Long-range dust control. /t must be understood that
dust control is not a substitute for abatement. In areas
heavily contaminated with lead, such as deteriorating old
housing and dwellings adjacent to lead-emitting industrial
plants or heavy vehicular traffic, it may be helpful to
institute a regular program in and about the home to
control lead-bearing dust, which constantly reaccumulates.
Because hand-to-mouth activity is common in young
children, parents must institute a specific type of cleaning
program; vacuuming and wet cleaning are recommended.
Sweeping with a broom, although it may remove large
fragments, serves only to stir up smaller particulates. It is
recommended that all floors and woodwork be scrubbed
weekly with high-phosphate detergents such as Tide or
Spic and Span. For all surfaces that the child can touch,
the weekly scrubbing should be supplemented with daily
damp dusting with a cloth rinsed in a solution of high-
phosphate detergent. Although such cleaning programs
may be helpful, the definitive way to prevent recurrences is
for affected children and their families to move into
housing free of lead paint hazards.
Dietary factors. Although reduction in exposure to
environmental lead must receive first priority, steps should
be taken to identify and correct deficient dietary intake,
particularly of calcium? ™ and iron as well as excessive
dictary fat, each of which may increase the absorption and
retention of lead. A diet adequate in minerals and limited
in fat should be assured. For those intolerant of cow milk,
lactose-free milk products such as yogurt or some alterna-
live source are necessary to ensure adequate calcium
intake. The use of low-fat milk and the avoidance of fried
foods should limit excessive dietary fat. Acidic foods such
as fruits, fruit juices, tomatoes, sodas, and cola drinks may
leach lead from cans with leaded-soldered seams. Dietary
lead intake may be reduced if the above items are
purchased fresh, frozex, or packaged in aluminum, glass,
cardboard, or plastic contamers.
Neurobehavioral considerstions. A major problem is
presented by the high level of hand-to-mouth activity of
many preschool-aged children. If hand-to-moutk activay
or pica (ingestion of nonfood items) is particularly severe,
a behavioral psychologist can be helpful in developag a
program to reduce the activity.
For children given any combination of chelating agents,
neurologic and psychologic assessment should be obtained
at the time of initial diagnosis and during the following
years. This will facilitate appropriate school placement for
children with learning handicaps, if they are identified
through thorough psychometric evaluation prior to the
child’s entry into the school system. For the child who has
had acute lead encephalopathy, long-term anticonvulsant
therapy with phenytoin (or phenobarbital) is indicated if
there were seizures or coma during the encephalopathic
episode. Additional clinica) and Isboratory evaluation may
be indicated to detect other sequelae of chronic fead
poisoning, such as renal impairment. Metabolic disorders
associated with acute lead poisoning are reversible after
chelation therapy and substantial reduction of lead expo-
sure.
Frequency of follow-up. When the results of initial
venous blood lead and EP values and CaNa2-EDTA
testing indicate the need for chelation therapy, long-term
follow-up is indicated. For those children who have not
received chelation therapy, follow-up at 3-month intervals,
together with abatement and dust control in the home and
correction of dietary deficiencies, should be continued until
the child has maintained normal blood lead and EP values
for 1 year.
Those children who initially received a course of chela-
tion therapy require more intensive follow-up. Abatement
of environmental lead hazards in the home is rarely
accomplished within a matter of a few days, so that as 2
general rule the first course of chelation therapy is given in
the hospital. Outpatient chelation therapy while a child is
still overexposed to lead is counterproductive and likely to
be associated with enhanced absorption and retention of
lead. In children who have received a course of chelation
therapy, blood lead and EP determindtions should be
repeated 5 to 7 days after therapy and then after another |
to 4 weeks, depending on the progress. If some improve-
ment is observed, follow-up may be scheduled at 2- to
4-week intervals for 6 months. Thereafter, blood lead and
EP tests should be repeated at 3-month intervals until the
child is 6 years of age. At each visit the environmental and
housing situations arc updated and reevaluated and dust
control and diet are reviewed. If serial blood lead and EP
data show continued improvement, it may be assumed that
new assimilation of new lead is not occurring; rising blood
lead concentrations, which may be followed by a rising EP
level, indicate increased ingestion of lead. Often, reinvesti-
galion reveals new sources of environmental lead not
previously detected. When a child with earlier elevated
blood lead concentrations approaches school age, psycho-
metric evaluation may be indicated. even though the blood
lead concentration at the time is <25 ug/dl.
Summary. Increased body lead burden must be managed
as a chronic disorder. The final evaluation and disposition
of each case must take into account the entire prior record.
It is prudent to observe mentally or developmentally
handicapped children with persistent pica during school
years, because recurrences after the age of 6 years are most
likely to occur in these children. The need to remove
infants, young children, and pregnant women from a home
during abatement of lead paint hazards is crucial to
prevent acute episodes of sharply increased lead toxicity.
We thank Ms. Barbara Cirella. P.N.P., for performing the
CaNs-EDTA provocation studies, and Ms. Carol Seaman for
statistical analysis of the data; Dr. Morri E. Markowitz, and the
CRC staff at Albert Einstein College of Medicine: Ms. Barbara
Mahan. and the nursing staff in the Pediatric Lead Clinic at
Children's Hospital, and Ms. Victoria Sadoff for careful and
painstaking assistance with preparation of the manuscript.
REFERENCES
1. Chisolm JJ Jr: The use of chelating agents in the treatment of
acute and chronic lead intoxication in childhood. J PEDIATR
73:1, 1968.
Markowitz ME. Rosen JF: Assessment of lead stores in
children: Validation of an 8-hour CaNa,-EDTA provocation
test. J PEDIATR 104:337, 1984.
_ Chisolm JJ Jr. Mellits ED. Barrett MB: Interrelationship
among blood lead concentration, quantitative daily ALA-U
and urinary lead output following calcium EDTA. In Nord-
berg GF. editor: Effects and dose-response relationship of
toxic metals. Amsterdam, 1976, Elsevier Scientific.
_ Chisolm JJ Jr. Barlirop D: Recognition and management of
children with increased lead absorprion. Arch Dis Child
54:249. 1979.
_ Gracf SW. Kopito L. Shwachman H: Lead intoxication in
children. Postgrad Med 50:133, 1971).
. Sacnger P. Rosen JF, Markowitz ME: Diagnostic significance
of edetate disodium calcium testing in children with increased
lead absorption. Am J Dis Child 136:312. 1983.
_ Mahaffey KR, Anncst JI, Roberts J. Murphy RS: National
estimates of blood lead levels. United States 1976-1980:
Association with selected demographic and $0CI0ECoNOMIC
factors. N Engl J Med 307:573, 1982.
_ Preventing lead poisoning in young children: A statement by
the Centers for Discase Control. J PEDIATR 93:709. 1978.
Emmerson BT: Chronic lead nephropathy: The diagnostic use
of calcium EDTA and the association with gout. Aust Ann
Med 12:310, 1963.
gv
{
#
22.
23.
. Hammond PB: The effects of chelating agents on the tissue
distribution and excretion of lead. Toxicol Appl Pharmacol
18:296, 1971.
. Leckie WJH, Tompsett SL: The diagnostic and therapeutic
use of edathamil calcium disodium (EDTA. versene) in
excessive inorganic lead absorption. Q J Med 27:65, 1958.
. Whittaker JA, Austin W, Nelson JD: Edathamil calcium
disodium (versenate) diagnostic test for lead poisoning. Pedi-
atrics 29:384, 1962.
. Teisinger J, Srbova J: The value of mobilization of lead by
calcium ethelene diaminetetraacetate in the diagnosis of lead
poisoning. Br J Ind Med 16:148, 1959.
. Hansen JPB, Dossing M, Paulev PE: Chelating lead body
burden (by calcium-disodium EDTA) and blood lead concen-
tration in man. J Occup Med 23:39, 198].
. Lahaye D, Roosels D, Verwilghen R: Diagnostic sodium
calcium edetate mobilization test in ambulant patients. Br J
Ind Med 25:148, 1968.
. Chiesura P: Remarks on the use of shortened procedures in
evaluating EDTA-induced urinary lead excretion. Lavoro
Umano 28:97, 1976.
. Vitale LF, Rosalinas-Bailon A, Folland D, Brennan JF,
McCormick B: Oral penicillamine therapy for chronic lead
posioning in children. J PEDIATR 83:1041, 1973.
. Graziano JH, Leong JK, Freidhcim E: 2,3-Dimercaptosuc-
cinic acid: A new agent for the treatment of lead poisoning. J
Pharmacol Exp Ther 206:696. 1978.
. Aposhian VH: DMSA and DMPS water-soluble antidotes for
heavy-metal poisoning. Ann Rev Pharmacol Toxicol 23:193.
1983.
. Piomelli S, Seaman C, Zullow D. Curran A, Davidow B:
Threshold for lead damage to heme synthesis in urban
children. Proc Natl Acad Sci 79:333S, 1982.
. Piomelli S: A micromethod for free erythrocyte porphyrins:
The FEP test. J Lab Clin Med 81:932, 1973.
Chisolm JJ Jr: Heme metabolites in blood and urine in
relation to lead toxicity and their determination. Adv Clin
Chem 20:225, 1978.
Alessio L, Bertazzi PA, Toffoletto F, Foa V: Free erythrocyte
protoporphyrin as an indicator of the biological effect of lead
in adult males. Int Arch Occup Environ Health 37:73.
1976.
35
24.
25.
26.
27.
28.
29.
31.
32.
33.
34.
3s.
Angle CR, Mclintire MS, Swanson MS, Stohs SJ: Erythro-
cyte nucleotides in children: Increased blood lead and cytidine
triphosphate. Pediatr Res 16:331, 1980.
Rosen JF, Chesney RW, Hamstra A, DeLuca HF, Mahaffey
KR: Reduction in 1,25-dihydroxyvitamin D in children with
increased absorption. N Engl J Med 302:1128, 1980.
Mahaffey KR, Rosen JF, Chesney RW, Peeler JT. Smith
CM. DeLuca HF: Association between age. blood lead
concentration and serum 1,25-dihydroxycholecalciferol levels
in children. Am J Clin Nutr 35:1327, 1982.
Saenger P, Markowitz ME, Rosen JF: Depressed excretion of
6B-hydroxycortisol in lead-toxic children. J Clin Endocrinol
Metab $8:363, 1984.
Needleman H, Gunnoe C, Leviton A, Reed R, Peresic H,
Maher C, Barrett P: Deficits in psychologic and classroom
performance of children with elevated dentine lead levels. N
Engl J Med 300:689, 1979.
Winneke G, Kramer U, Brochkaus E, Ewers U, Kajanek G.
Lechner H, Janke W: Neuropsychological studies in children
with elevated tooth-lead concentrations: Extended study. Int
Arch Occup Environ Health $1:232, 1983.
. Otto DA, Benignus V, Muller K, Barton CN: Effects of age
and blood lead burden on CNS function in young children. I.
Slow cortical potentials. Electroencephalogr Clin Neurophy-
siol $2:229, 1981.
Otto DA, Benignus V, Muller K, Barton CN, Seiple K, Prah
J. Schroeder S: Effects of low to moderate lead exposure on
slow cortical potentials in young children: Two-year follow-up
study. Neurobchav Toxicol Teratol 4:733, 1982.
Graef JW: Outpatient use of a six-hour lead mobilization test
in chelation therapy [abstract]. Pediatr Res 10:330, 1976.
Chisolm JJ Jr. Barrett MB, Harrison HV: Indicators of
internal dose of lead in relation to derangement in heme
synthesis. Johns Hopkins Med J 137:6, 1975.
Piomelh S, Corash L. Corash MB. Seaman C, Mushak P,
Glover B, Padgett R. Blood lead concentrations in a remote
Himalayan population Science 210:1135, 1980.
Sorell M, Rosen JF, Roginsky M. Interations of lead. calci-
um, vitamin D and nutrition in lead-burdened children. Arch
Environ Health 32:160, 1977.
+ U.S. COVERNMENT PRINTING OFFICE 988 30 -009/ 88769