Planned Parenthood of Southeastern Pennsylvania v. Casey Joint Appendix Vol. 2
Public Court Documents
April 21, 1988 - August 24, 1990
Cite this item
-
Brief Collection, LDF Court Filings. Planned Parenthood of Southeastern Pennsylvania v. Casey Joint Appendix Vol. 2, 1988. e9bd4c56-c19a-ee11-be36-6045bdeb8873. LDF Archives, Thurgood Marshall Institute. https://ldfrecollection.org/archives/archives-search/archives-item/e656b5b9-1d25-4707-a258-d37866c9974b/planned-parenthood-of-southeastern-pennsylvania-v-casey-joint-appendix-vol-2. Accessed February 24, 2026.
Copied!
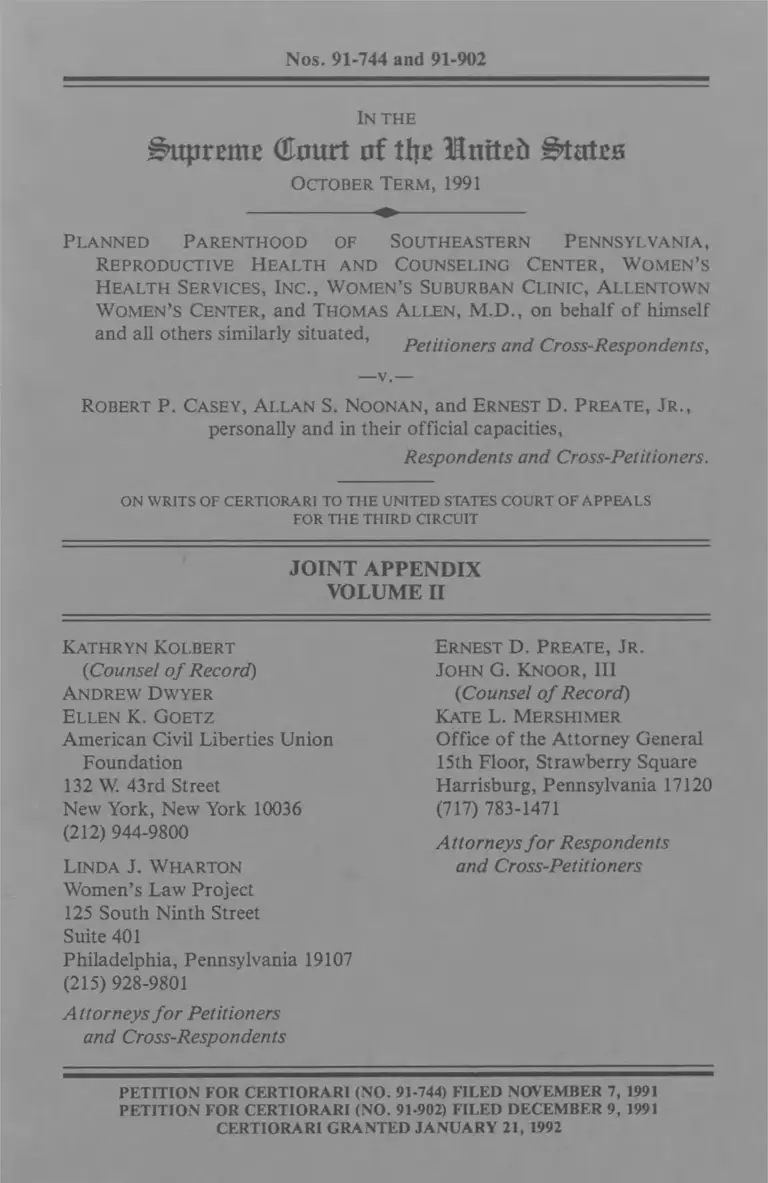
Nos. 91-744 and 91-902
In the
B>upratte (Eourt of tt\z Mnitefc ^tateo
October Term, 1991
Planned Parenthood of Southeastern Pennsylvania,
Reproductive Health and Counseling Center, Women’s
Health Services, Inc., Women’s Suburban Clinic, Allentown
Women’s Center, and Thomas Allen, M.D., on behalf of himself
and all others similarly situated, _ _ , _Petitioners and Cross-Respondents,
—v.—
Robert P. Casey, Allan S. Noonan, and Ernest D. Preate, Jr.,
personally and in their official capacities,
Respondents and Cross-Petitioners.
ON w rits of c ertio rari to th e united states court of a ppe a ls
FOR THE THIRD CIRCUIT
JOINT APPENDIX
VOLUME II
Kathryn Kolbert
{Counsel o f Record)
Andrew Dwyer
Ellen K. Goetz
American Civil Liberties Union
Foundation
132 W. 43rd Street
New York, New York 10036
(212) 944-9800
Linda J. Wharton
Women’s Law Project
125 South Ninth Street
Suite 401
Philadelphia, Pennsylvania 19107
(215) 928-9801
Attorneys fo r Petitioners
and Cross-Respondents
Ernest D. Preate, Jr.
John G. Knoor, III
{Counsel o f Record)
Kate L. Mershimer
Office of the Attorney General
15th Floor, Strawberry Square
Harrisburg, Pennsylvania 17120
(717) 783-1471
Attorneys for Respondents
and Cross-Petitioners
PETITION FOR CERTIORARI (NO. 91-744) FILED NOVEMBER 7, 1991
PETITION FOR CERTIORARI (NO. 91-902) FILED DECEMBER 9, 1991
CERTIORARI GRANTED JANUARY 21, 1992
1
TABLE OF CONTENTS
Page
Relevant Docket Entries .......................................... 1
Excerpts from Transcript of Hearing on Plaintiffs’
Motion for a Temporary Restraining Order,
April 21, 1988 ...................................................... 23
Excerpts from Transcript of Hearing on Plaintiffs’
Motion for a Preliminary Injunction,
May 9, 1988 .......................................................... 27
Order Granting Plaintiffs’ Request for Class
Certification (Oct. 25, 1988)............................... 42
Plaintiffs’ Amended Complaint for Declaratory
and Injunction R elie f.............................................44
Order Clarifying May 23, 1988, Preliminary
Injunction (Jan. 11, 1990) ................................. 72
Defendants’ Answer......................................................74
Stipulation of Uncontested Facts ............................... 86
Supplemental Stipulation of
Uncontested Facts ............................................. 102
Stipulation of Voluntary Dismissal ............................112
Excerpts from Trial Transcript,
July 30 through August 1, 1990 ..........................113
Non-Jury Trial - Day 1 ..................................... 113
Non-Jury Trial - Day 2 ..................................... 204
Non-Jury Trial - Day 3 ...................................... 315
Excerpts from Defendants’ Trial Exhibits................ 393
Defendants’ Exhibit 1: Excerpts from
Magee-Womens Hospital Informed
Consent for Termination of
Pregnancy Form ................................................. 393
Defendants’ Exhibit 2: Excerpts from
Women’s Health Services (WHS)
Individual Counseling Guidelines/
Post Abortion Group Guidelines/
Personal Counseling Guideline........................... 396
Defendants’ Exhibit 3: WHS Consent
for Abortion Form ............................................. 410
Defendants’ Exhibit 4: WHS
November 20, 1986
Memo Re Parental Notification .......................415
Defendants’ Exhibit 5: Excerpts from
WHS Patient Record Form ................................418
Defendants’ Exhibit 8:
WHS Advertisements .........................................441
Defendants’ Exhibit 9: Excerpts from
Planned Parenthood of
Southeastern Pennsylvania (PPSP)
Center Policy and Procedure Manual .............. 444
11
Ill
Defendants’ Exhibit 10: Excerpts from
PPSP Request for Abortion Form .....................451
Defendants’ Exhibit 11: Excerpts from
PPSP Fact Sheet ................................................. 453
Defendants’ Exhibit 13: Excerpts
from Guidelines of
Women’s Suburban Clinic (WSC) .....................457
Defendants’ Exhibit 14: WSC
Disclosure of Risk,
Benefits and Alternatives Form ......................... 461
Defendants’ Exhibit 17: WSC Information
Prior to Consent/Certification
by Patient Form ................................................. 464
Defendants’ Exhibit 18: WSC
Parental Involvement Form ................................465
Defendants’ Exhibit 19: WSC
Physician’s Certification Form ........................... 466
Defendants’ Exhibit 20: WSC
Protocol Regarding Minors ................................467
Defendants’ Exhibit 26: Excerpts from
Reproductive Health and Counseling
Center (RHCC) Consent Forms .......................469
Defendants’ Exhibit 30:
RHCC Advertisements ...................................... 473
IV
Defendants’ Exhibit 32: Allentown
Women’s Center (AWC)
Counseling Checklist ...........................................474
Defendants’ Exhibit 33: Excerpts
from AWC Confidential Patient
Record Form ......................................................477
Defendants’ Exhibit 35:
AWC Advertisements .........................................484
Defendants’ Exhibit 36:
AWC Consent Form ...........................................486
Defendants’ Exhibit 37:
Northeast Women’s Center
Guidelines for Informed Consent .....................487
Defendants’ Exhibit 39:
Summary Compilation of
Quarterly Reports ............................................... 488
Defendants’ Exhibit 45: Commonwealth
of Pennsylvania Department
of Health (DOH) Abortion Facility
Registration Form ............................................. 489
Defendants’ Exhibit 46: DOH
Abortion Quarterly
Facilities Report Form .......................................491
Defendants’ Exhibit 47A: DOH
Report of Induced Termination
of Pregnancy Form
(version no. 1) 493
V
Defendants’ Exhibit 47B: DOH
Report of Induced Termination
of Pregnancy Form
(version no. 2) ...................................................497
Defendants’ Exhibit 47C: DOH
Report of Induced Termination
of Pregnancy Form
(version no. 3) 500
Defendants’ Exhibit 48: DOH
Certification Regarding
Spousal Notice Form .........................................504
Defendants’ Exhibit 49: Excerpts
from DOH Directory of
Social Service Organizations
for Referrals for
Pregnant Women ............................................... 506
Defendants’ Exhibit 50: Excerpts
from DOH Printed Information
on Medical Assistance Benefits ......................... 508
Defendants’ Exhibit 51: DOH Notices
Required by Abortion Control Act ...................518
Defendants’ Exhibit 54: Deposition
Excerpts of Thomas E. Allen, M .D .....................519
Defendants’ Exhibit 55: Deposition
Excerpts of Sue Roselle .................................... 522
Defendants’ Exhibit 56: Deposition
Excerpts of Carol C. Wall .................................. 527
VI
Defendants’ Exhibit 57: Deposition
Excerpts of Sherley Hollos ................................532
Defendants’ Exhibit 58: Deposition
Excerpts of Jane S. G re e n ..................................538
Defendants’ Exhibit 59: Deposition
Excerpts of Sylvia Stengle .................................. 541
Defendants’ Exhibit 60:
Discovery Excerpts ............................................. 552
Excerpts from Plaintiffs’ Trial Exhibits......................556
Plaintiffs’ Exhibit 49: DOH Instructions
and Definitions for Report of
Induced Termination of
Pregnancy Form (July 1988) ..............................556
Plaintiffs’ Exhibit 60: Veto Message
to the Pennsylvania Senate on
S.B. 742 of Governor Dick Thornburgh
(Dec. 23, 1981) ....................................................572
Plaintiffs’ Exhibit 61: Message
to Pennsylvania Senate on Signing
of 1982 Pennsylvania Abortion
Control Act of
Governor Dick Thornburgh
(June 11, 1982) ....................................................583
Plaintiffs’ Exhibit 62: Veto Message
to Pennsylvania House of Representatives
on H.B. 1130 of Governor
Robert Casey (Dec. 17, 1987) ...........................592
VI1
Plaintiffs’ Exhibit 67: Excerpts from
The Federal Role in Determining the
Medical and Psychological
Impact of Abortion on Women,
H.R. Rep. No. 392,
101st Cong., 1st Sess. (1989) .............................599
Plaintiffs’ Exhibit 89:
Diagnostic Criteria for
Post-Traumatic Stress Disorder ......................... 606
Excerpts from Verifications Filed
in Support of Plaintiffs’
Preliminary Injunction Motion ......................... 608
Excerpts from Verification
of Sue Roselle (Apr. 19, 1988) ........................ 608
Excerpts from Verification
of Sylvia Stengle (Apr. 18, 1988) .......................615
The following opinions and orders have been omitted in
printing this Joint Appendix because they appear on the
following pages in the Appendix to the Petition for a Writ
of Certiorari in No. 91-744.
Planned Parenthood v. Casey, 947 F.2d 682
(3d Cir. 1991) .......................................................... la
Planned Parenthood v. Casey, 744 F. Supp. 1323
(E.D. Pa. 1990) ..................................................... 104a
Order of the United States District Court
for the Eastern District of Pennsylvania,
filed August 24, 1990 ............................................. 285a
393
EXCERPTS FROM DEFENDANTS’ TRIAL EXHIBITS
Defendants’ Exhibit 1:
Excerpts from Magee-Womens Hospital
Informed Consent for
Termination of Pregnancy Form
MAGEE-WOMENS HOSPITAL
Pittsburgh, PA 15213
INFORMED CONSENT FOR TERMINATION OF
PREGNANCY
I hereby authorize __________________________ ,
M.D., and/ or such associates and assistants as he/she
may select and supervise to perform the following
procedure(s):________________________ •
The doctor has explained to me the nature and
purpose of the procedure(s), the risks associated with the
treatment, the available alternatives and risks of these
alternatives, as summarized below.
1. The medical procedure to be used i s ____________ ,
which has been explained to my full satisfaction.
2. The risks involved with the procedure(s) include
severe blood loss, infection, perforation,
incompleteness, possible need for further surgery
(hysterectomy, removal of tubes and ovaries),
possible sterility, danger to subsequent pregnancies,
fatality and ________________, which have been
explained to my full satisfaction.
394
3. I understand that possible alternatives to the
abortion procedure include childbirth and possible
placement for adoption which have been explained
to my full satisfaction. I fully understand the risks of
these alternatives, which have been explained to me.
4. I fully understand that there is no guarantee that this
procedure will be successful or that it will terminate
my pregnancy.
5. If any unforeseen condition arises in the course of
the abortion which, in accordance with good medical
practice calls for procedures in addition to or
different from those contemplated, I further
authorize the above-named physician or his designee
to perform such procedures which in his professional
judgment are necessary.
6. I understand that it is my responsibility to bring to
the attention of the staff physician and Magee-
Womens Hospital any unusual symptoms following
the procedure and to report for check-ups or
pregnancy tests as recommended.
7. I have had full opportunity to ask additional
questions of the doctor(s) and staff about this
procedure and the risks and alternatives involved
and am satisfied with the answers. I have no further
questions. I understand that I am free to withhold
or withdraw my consent to perform this procedure at
any time prior to the abortion without prejudicing
my future care.
8. I understand that Pennsylvania law requires that
fetal tissue removed during an abortion be submitted
for pathological examination.
395
Magee-Womens Hospital will be responsible for fetal
tissue:
_________ Yes _________No
I certify that I have read (or had read to me) and
fully understand the above consent to abortion and
the explanations referred therein were made to me.
PATIENT SIGNATURE DATE TIME
PATIENT IDENTIFIED PRE-OPERATIVELY BY:
* *
396
Defendants’ Exhibit 2:
Excerpts from Women’s Health Services (WHS)
Individual Counseling Guidelines/
Post Abortion Group Guidelines/
Personal Counseling Guidelines
INDIVIDUAL COUNSELING GUIDELINES
Abortion Clinic
The purpose of this interview is to establish that the
woman understands her pregnancy options and desires
an abortion, has a genuinely informed consent, and to
obtain the necessary history for the medical record.
Before the interview the counselor should review the
chart, looking for LMP, any pelvic exam, age, distance
traveled, occupation, whether anyone is accompanying
her, marital status, medical history, record of prior visits
and lab work. This information is helpful to have in
mind when greeting and getting to know the woman so
that we can provide service in a manner that will meet
her needs as well as those of the people accompanying
her.
The usual interview covers steps 1 thru 14 of the
outline below and takes from ten to thirty minutes. The
average time is about twenty minutes but can vary due to
specific circumstances. In this interview the counselor
must assess the woman’s individual needs and determine
the best way to organize the session. Women who are
conflicted and unable to resolve those conflicts in a short
period of time (15 minutes) should be referred
immediately to the personal counselor or to a counseling
administrator.
There are times when all information given to the
patient including the post abortion follow up instructions
397
and the contraceptive instructions should be done in the
individual session. Women who are deaf, have
significant English language problems, adolescents under
15, those who are slow to comprehend, or who have
emotional disabilities should be given all information in
this individual session. The latter paragraphs below
describe the steps in covering this additional information.
Suggested interview outline:
1. Give an overview of what the woman will experience
during her stay--where she will be, how long she will
be in certain places.
2. Tell the woman what you will be talking about
during the interview and that you will (1) discuss any
questions or concerns the woman has about the
abortion (2) discuss the procedure (3) take her
medical history. In this way a contract is informally
set. It is important that the woman knows what to
expect from the counselor during the interview-that
the goals are clearly defined. For those who are to
have all information individually the counselor would
also include (3) care afterwards and (4) birth control
in her overview of the interview.
3. Encourage the woman to ask any questions she may
have. She will be more ready to listen if this is done
first. Find out what she knows about the abortion
procedure. Her questions, level of information and
concerns will help the counselor gauge where to
start. It is up to the counselor to decide in what
order to cover the necessary information with the
woman so that it attends to those individual needs
that are within the limits of the counselor’s goals and
capabilities.
398
4. The counselor usually describes the procedure next,
reviewing each step and what the patient will feel.
The counselor starts by making certain that the
woman understands basic reproductive anatomy and
the menstrual cycle.
5. The complications should be listed and an
explanation of how they might occur. These must be
presented in a way that is both realistic and in
perspective to the chance of occurrence. We believe
a genuinely informed consent should be part of any
medical procedure. All patients should have
infection, hemorrhage, perforation and in
completeness, the possibility of further medical
treatment or surgery, i.e. hysterectomy, removal of
tubes or ovaries resulting in sterility, as well as
fatality explained to them. Emphasize that in an EA
the most common complication is incompleteness.*
6. Assess the woman’s readiness for the abortion by
asking her if it was an easy or difficult decision, and
with whom she has been able to discuss this. If the
woman is not ready for the abortion, the counselor
should stop here, attempt to help resolve the issues
and get help from the personal counselor or
supervisor if needed. The counselor should make
sure that the woman understands all the options
available to her including abortion or a full term
delivery where she could either keep the child or put
it up for adoption.
7. Take the histories on pages 1, 2, 3, 4, 5 of the chart.
8. Take her vital signs and record them.
9. Have her read or read to her the consent. Have
399
patient sign the consent. Witness the consent.
10. All women should be given a copy of the WHS
"Guide to Birth Control Options" and asked to look
it over in preparation for the recovery group.
11. When the interview is finished, allow the patient to
stay in the counseling room, and take the chart to
the lab for the test results.
12. If the blood type is Rh Negative explain the meaning
of this before you escort her from the counseling
room.
13. Get and record her weight, instruct her to use the
restroom if possible and then have a seat in the
waiting area.
14. Counselor should take her completed chart to flow
and get her next assignment.
If the patient is to receive all information on an
individual basis the counselor will:
A. Review all information on the post abortion
instructions* after completing the histories in
step 7. The attached envelopes should be
reviewed also.
*The EA patient will be given additional
instructions in the Recovery Room. Tell her in
counseling that if the fetal tissue is less than 8
weeks LMP, she will need a pregnancy test
within 2 to 3 weeks after the abortion as well as
a check-up by 8 weeks. She should make her
check-up appointment after getting her
400
pregnancy test results. For a check-up made
after 8 weeks the woman will be charged for an
annual exam. Tell the patient that on the slight
chance she is still pregnant at the time of the
UCG, it is important that she have a repeat
procedure to terminate the pregnancy. The fetus
can be damaged by infection from the uterus
having been entered.
B. The review of the birth control methods is done
next. The goals are to give accurate birth
control information, assess the woman’s needs
for a method and usually urge the woman to
choose a method to prevent further pregnancies.
The counselor gives a brief introductory
overview to all the methods, and then,
depending on how the woman responds,
discusses all, one, or several of the methods.
Each woman is instructed in the use of foam and
condoms since it is an easily available back-up
method. If a woman states she does not plan to
use any, this is explored-complete information
on birth control is given so that she will know
about the methods for the future. If she does
not want a method, that decision is respected.
C. Complete steps 8 and 9.
* * *
Summary of Charting Inservice
5. Specific charting areas
a. Page One will no longer be reviewed in depth by
the receptionist. This will now be the
401
counselor’s responsibility. Clerical will cover the
"black dot" questions (allergies, heart, epilepsy,
seizures, diabetes, hepititis, jaundice) and the
"white dot" data needed for sizing in order to
make the necessary referrals to the NP/PA’s.
The counselor covers items 1-36 recording for
any circled items: date of occurrence and
description (original onset, degree of problem,
treatment if any). Counselor covers any
medication taken today, medications taken
previously, any allergies and allergic reactions to
medicines. The allergies are circled in red on
page one and the counselor writes the allergy in
red on page 5 on allergy line. Remember to
write N/A at any section where there is nothing
to record to indicate you covered the data.
The counselor should review any
questionable histories with NP/PA’s to
determine if any special exam or care is
necessary.
Counselor must be fully aware of the
contraindications to abortion in Medical
Standards.
b. Page 2 - It is important to record what isn’t as
well as what is (birth control history — none used
for example). The counselor checks the
appropriate box in the laboratory section when
VD culture is done in procedure.
c. Page 3 - The counseling paragraph should
summarize Relationship issues (a stress situation,
how partner, parents, friends, others of
significance have responded to decision, degree
of support wanted and available, how do parents
and/or partner see their emotional and financial
responsibility to patient; ability to communicate
(any need for special explanations due to
402
language problems, slowness); the decision
(difficulties, pros and cons, reason for
termination, any issues concerning morality of
abortion). If the woman is having the abortion
for medical reasons this must be stated and that
the option of a second opinion with genetic
counseling was offered must be recorded.
Special Cases 1) Reasons for not telling parent
if underage, 2) If patient is victim - raped or
incest - and on MA it must be recorded in
counseling paragraph as the reason for the
abortion, 3) If full interview done and reason for
doing this is to be recorded.
The counseling paragraphs should be written
in complete sentences, no slang should be used,
be descriptive, discreet and avoid the counselor’s
personal judgments about the patient or her life
style. The paragraph should only summarize
information related to the abortion decision.
All pamphlets given to her, referrals to
personal counselor, other referrals such as to
PAAR, Neighborhhod Legal Services, etc. should
be recorded under recommendations and
referrals.
When a patient is voided, the administrator
should record the related information in the box
on the bottom of page 3 so we can use the same
insert if the patient returns for termination of
that pregnancy.
403
PERSONAL COUNSELING SESSION
Interviewer:_______________ Case#_______
(Initials) (If appropriate)
Nickname: DOB:
INTRODUCTORY COMMENT: I understand that
you’ve been having a difficult time with this decision.
Perhaps by talking about your concerns and hearing the
answers to your questions, you will be better able to
decide what is best. Our discussion is intended to be of
help to you. Any time you don’t understand why I’m
asking a particular question, please feel free to ask me
about my reasons for asking that particular question.
INTERVIEW QUESTIONS:
1. When you think of pregnancy, what kinds of things
come to mind?
2. How long have you been pregnant?______________
3. Have you ever had an abortion? __ No __ Yes
(Number:__ )
4. Who have you chosen to tell about your pregnancy?
People* told. Their reaction
This person accompanied patient.
404
Partner’s reaction to pregnancy - initially:
_Positive__ Negative__ Not Told
_________ ’s current reaction is :__ Positive__ Negative
(Name of Partner)
5. What were your beliefs about abortion before this
happened?
_AB acceptable
_AB acceptable, difficult decision
_AB unacceptable, unless under cases of rape,
incest, MR, etc.
_AB unacceptable
Comment:
6. Do you have other children? __ Yes ___No
7. How do you see a child fitting into your life right
now?
8. What is your religious background?
_Christian __ Jewish __ Moslum___Catholic
_Protestant __ N/A
405
9. Have you ever been hospitalized for a nervous
disorder? No Yes Where?
10. Have you ever seen a counselor, psychologist,
psychiatrist? __ No __ Yes
11. Do you have any questions of me?
No
Client asked about procedure.
Client asked about fees.
Client asked about feelings women have post
AB.
__ Client asked if the procedure will affect
future pregnancies.
Other (specify)______________________
CLIENT ORIENTATION DURING INTERVIEW
Internal Control...........External Control
Little Denial Present...........Denial Evident
Self Esteem Present...........Poor Self Esteem
INTERVENTIONS
__ Support for assertive right to make personal
choice, whether AB, pregnancy to term,
adoption.
__ Showed pictures of early fetal development.
__ Gave reading materials.
__ Gave list of phone numbers related to religious
406
groups/individuals (client may contact)
Cognitive restructuring to establish fact(s)/realty
related to _____________
RECOMMENDA TIONS
__ None needed/none requested
Client is comfortable with her current personal
choice.
Suggested she give AB more thought.
Client is to return to another session on (date)
Client is to return for another session "when
needed"
Contact West Penn Hospital for genetic
counseling/information
Call for sizing appointment
Suggested she seek support from significant
other(s). Specify ________________________
Suggested she return for post AB session.
Suggested that AB doesn’t appear to fit within
her value system. We discussed other options
for a second time.
OTHER RECOMMENDATIONS not aforementioned
CLIENT DECISION
Keep scheduled appointment for procedure
_Very comfortable with decision
Comfortable with decision
407
Schedule procedure
_Very comfortable with decision
_Comfortable with decision
Schedule another personal counseling session
Give procedure further thought
Discuss potential decision with significant
other(s)__________________________________
Keep Pregnancy
Adoption procedure (__ gave information on
local adoption agencies)
INTERVIEW QUESTIONS WITH PERSON (S)
ACCOMPANYING CLIENT
Not applicable, no one accompanied her
Mother __ Relative
(Specify________ )
Father __ Friend
Partner Counselor
1. What are your thoughts regarding this pregnancy?
2. Flow long have you known about this pregnancy? _
3. Who else have you told?_______________________
Does the client know this? __ Yes __ No
4. What are some of your concerns?________________
5. In what areas are you willing to be helpful if she
decides to carry her pregnancy to term?
408
Emotional support, no matter what she decides.
None, she’s on her own.
Lodging, she can live with me/us
Child care (full time/part time/occasionally)
Financial
Just food for she’ll be on her own
Other (specify) ______________________ _ _
6. Have you told her how much support/help she can
expect from you? __ Yes __ No
(If "no", when do you plan to do so? __________ )
7. Do you have any questions of me?
About the procedure
Fees
AB effect on future pregnancies
Other (specify) ___________________________
8. Interview’s impression of significant others. Check
(7) all that apply.
Opinion seeker
Initator (person is appropriately assertive)
Information seeker
Opinion giver
Information giver
Elaborator
Organizer/coordinator
Evaluator/critic
Aggressor
Blocker (person avoids reality of situation)
Moralizer
Supporter
Passive
Observer
Follower
Compromises
409
Harmonizer
Recognition seeker
Self-confessor
Dominator
Help seeker
RECOMMENDATIONS TO SIGNIFICANT OTHER(S)
Not needed,
already Dresent Needed
Offer emotional support, no
matter what she decides.
Make position clear to
client
Seek counsel from other
sources,
e.g.,
Return with client for
another session
Stop enabling client’s
excessive dependency
Read the same material
given to client so topics can
be discussed.
Comments: (please use reverse side)
410
Defendants’ Exhibit 3:
WHS Consent for Abortion Form
CONSENT FOR ABORTION
I hereby authorize a Staff Physician to perform upon
me a VACUUM ASPIRATION ABORTION, including
all the mechanical aspects, which have been explained to
me.
I consent to the administration of anesthesia to be
applied by or under the direction of the staff physician,
and the use of such anesthetics as s/he may deem
advisable.
If any unforeseen condition arises in the course of
the abortion which, in accord with good medical practice,
calls for procedures in addition to or different from those
contemplated, I further request and authorize the staff
physician to perform such procedures, or administer any
medication which s/he may deem advisable or to have
me admitted to a hospital facility.
I understand that it is my responsibility to bring to
the attention of Women’s Health Services, Inc. any
unusual symptoms following the abortion and to report
for check-ups or pregnancy tests as recommended.
The nature and purpose of an abortion by vacuum
aspirations, other abortion techniques, and the
alternatives to abortion, including childbirth and
adoption, the risks involved, and the possibility of
complications and detrimental physical and psychological
effects which are not anticipated but may occur,
including by way of illustration and not limitation,
hemorrhage, infection, perforation, incompleteness as
well as the possible need for further surgery (i.e.
hysterectomy, removal of tubes and ovaries), possible
sterility and fatality, all of which have been fully
411
explained to me.
I authorize Women’s Health Services to dispose of
all fetal tissue as it sees fit.
I CERTIFY THAT I HAVE READ (OR HAD
READ TO ME) AND FULLY UNDERSTAND THE
ABOVE CONSENT OF ABORTION AND THAT THE
EXPLANATIONS THEREIN REFERRED TO WERE
MADE.
Date____ Time__
Signature of Patient
Signature of Person authorized to give consent, if not
patient
Relationship to Patient
Signature of Physician
Signature of Witness
ECTOPIC PRECAUTIONS
I certify that I have received a copy of the sheet
listing the precautions for possible ectopic pregnancy,
have read it and understand the importance of the
medical follow-up.
Date_____ Signature of
Patient
412
Alternate contact person in addition to myself:
Relationship Phone Number
Signature of Witness
EARLY ABORTION SPECIAL INSTRUCTIONS
I certify that I have received a copy of the sheet
describing the special instructions for early abortion
patients, have read it and understand the importance of
the medical follow-up.
Date____ Signature of
Patient
Signature of person authorized to give consent, if not
patient
Relationship to Patient
Signature of Witness
POST ABORTION INSTRUCTIONS
I certify that I have received a copy of the sheet
describing instructions for after the abortion, have read it
and understand the importance of the medical follow-up.
Date_____ Signature of
Patient
Signature of
Witness
413
Signature of Person authorized to give consent, if not
patient
Relationship to Patient
CONSENT FOR ORAL CONTRACEPTION
I hereby authorize a staff physician of Women’s
Health Services, Inc. and/or whomever s/he may
designate as a practitioner to perform:
Contraceptive Services and Supplies
I have received and agreed to read the patient
information on oral contraceptions provided by the
manufacturer.
I do hereby release Women’s Health Services, Inc.
from any and all claims which I may have by reason of
their providing me this service.
I understand that it is my responsibility to bring to
the attention of Women’s Health Services, Inc., any
unusual symptoms and to report for check-ups as
recommended.
I CERTIFY THAT I HAVE READ (OR HAD
READ TO ME) AND FULLY UNDERSTAND THE
ABOVE CONSENT TO CONTRACEPTIVE
SERVICES AND SUPPLIES, AND THAT THE
EXPLANATIONS THEREIN REFERRED TO WERE
MADE AND THAT ALL BLANKS OR STATEMENTS
REQUIRING INSERTION OR COMPLETION WERE
FILLED IN.
414
Date____ Signature of
Patient
Signature of person authorized to give consent, if not
patient
Relationship to Patient
Signature of Witness
I do hereby release Women’s Health Services, Inc.
from any and all claims which I may have by reason of
their providing me this service I understand that it is my
responsibility to bring to the attention of Women’s
Health Services, Inc., any unusual symptoms and to
report for check-ups as recommended.
Date____ Gynecological Exam
Signature of
Patient_________________________________________
Date____ Antibiotic Therapy
Signature of
Patient
415
Defendants’ Exhibit 4:
WHS November 20, 1986
Memo Re Parental Notification
To: All Paraprofessional Counselors, Nurse
Counselors, Clerical Staff, Administrative Staff,
Personal Counselors
From: Liz Lincoln
Date: November 20, 1986
RE: Addition to 11/23/86 memo regarding parental
notification
Please re-read the 11/23/86 memo. A copy is on
the staff lounge bulletin board for convenience.
While we are not going to ask parents to come in
when we make an appointment for an adolescent, if a
parent or parents come in on the day of the abortion we
will get their signature on the consent page of the chart
using the following guidelines.
1. Front Reception - Ahead of time, identify which
patients on the appointment list are less than 18 (up
to day before 18th birthday). When the adolescent
signs in, ask if anyone has accompanied her. If a
parent or parents are there, instruct her to tell them
not to leave the facility until they are notified the
abortion is done.
2. Counselors - Nurse/Counselors - After greeting the
patient who has parents here give her an overview of
the counseling interview and ask if the parent can sit
in on the description of the abortion and the
416
complications so the parent can sign the part of the
consent for "others authorized to give consent".
Most should agree if this is presented as described
below.
Try to include just one parent - although if both
want to come we should accommodate that. Use
one of the four rooms with windows since those
rooms are larger. Extra chairs will be put in scale
room for you to use and return when needed.
Review the procedure, possible complications, and
options to abortion with the parent and adolescent.
Answer questions. Give reassurance if needed. Get
parent’s consent on line titled "signature of person
authorized to give consent, if not patient". Write
parent on line titled "relationship to patient". Escort
parent back to front waiting areas. The patient
herself will sign on "Signature of patient" line after
the interview is completed. Counselor witnesses at
that point.
If the adolescent seems ambivalent, her decision
making process and support system should be
discussed before bringing the parents in, rather than
after they are returned to the waiting area. Any
conflicts about the decision should be resolved
before including the parent.
If the patient does not want to include the parent,
one of the counseling administrators or another
counselor if available will cover the information with
the parent and get the parent’s signature.
This instance should be rare. The discussion of the
decision, and support system, the history taking, vital
417
signs, etc. will always occur without the parents. If
this is made clear and if the adolescent wants to be
here, it will be all right with most of them to include
the parents for the description of the procedure and
complications.
If a separate discussion is needed for parent consent
use separate consent sheet to expedite time and
staple to original consent. Review procedure,
complications, and options with parent.
We are doing this to comply with our
liability insurance requirements. This is not
part of the abortion control act.
REMINDER: After the procedure is done, the
counselor accompanying the adolescent
through procedure should see parents
and tell them they can go out for an
hour at that time if they wish. Give
estimated discharge time.
418
Defendants’ Exibit 5:
Excerpts from WHS Patient Record Form
WOMEN’S HEALTH SERVICES, INC.
PATIENT RECORD
Name _________________________________
Address________________________________
City______________________ County
State_____________________ Zip Code
Home Phone (____ ) ____________________
Business Phone (____ ) __________________
Date of Birth__________________ Age __________
___ Single (Never Married) ___ Married
___ Widowed ___ Separated ___ Divorced
Name you wish to be called by __________________
Occupation____________________________________
Place of Employment___________________________
Referred to WHS by:___________________________
What is your doctor’s (clinic’s):
Name _______________________________________
Address _____________________________________
Telephone Number_____________________________
(Area Code)
First Day of last normal menstrual period:
1. 4.
2. 5.
3. 6.
419
Do you consider yourself to be in good health: Yes No
Circle the number for each of the following you have or
have ever had:
1. epilepsy or seizures
2. hepatitis or jaundice
3. heart disease
4. rheumatic fever
5. heart murmer
6. diabetes (suger)
7. sexually transmitted
disease (gonorrhea,
syphilis, herpes,
chlamydia)
8. disease or surgery of
uterus, ovaries or
tubes
9. extopic (tubal)
pregnancy
10. cesarean section
11. Pelvic Inflammatory
Disease (PID)
12. cancer
13. vaginal infection
14. urinary tract/
bladder/kidney
infection
15. asthma
16. fainting, dizzy spells
17. breast lump or
tumor
18. high blood pressure
19. sickle cell disease
20. blood transfusion
21. anemia
22. bleeding tendency
23. chest pains
24. shortness of breath
25. nausea and/or
vomiting
26. frequent headaches
27. migraines
28. double vision
29. varicose veins
30. blood clots
(phlebitis)
31. swollen feet or
ankles
32. leg cramps
33. smoking
34. ever been
hospitalized
overnight
420
Any Family history of cancer, diabetes, T.B., allergies,
epilepsy, heart problems, high blood pressure?
WHO WHAT
Have you taken medication, today:
No Yes, I took
Date Medication Time
Date Medication Time
Date Medication Time
OPTIONAL: For Research Purposes Only
Religion________ Ethnic Background_____
Education - Last Grade Completed_________
List any other Allergies such as bee stings, eggs, etc.
421
Place an (X) in the appropriate column for any
medicines you have ever used or are allergic to:
USED ALLERGIC
_____________ Doxycycline _____________
_____________ Aspriin _____________
_____________ Penicillin _____________
_____________ Tetracycline _____________
_____________ Sulfa
_____________ Codeine
____________ Demerol
_____________ Antibiotics
_____________ Tranquilizers
_____________ Sedatives
_____ ______(Novocaine) local anesthetic
_____________ Rho gam
_____________ Dilantin _____________
_____________ Anticoagulant
_____________ Other
Description of Reaction
Patient Name______________ _ _ Patient Number
HISTORY AT INITIAL VISIT:
Date:_________________
MENSTRUAL HISTORY:
Age of onset__ length of cycle___ days of flow
Amount of flow: Scant Moderate Heavy
Amount of Discomfort:
Relieved by:
422
INTERNAL EXAM:
Ever had one: Yes No Date_______
PAP SMEAR:
Ever had one: Yes No Date_______
Date_______
Date_______
Date_______
Date_______
Date_______
ANY ABNORMALITIES: Yes No Date
If Yes, explain_________________________
CONTRACEPTIVE
Dates
Used
Problem Dates
Used
Problem
Pill
IUD
Dia
phragm
Foam
Con
doms
Other
1
423
PREGNANCY: Give dates (month & year); sex, male or
female. If Cesarean section, circle dates.
Live
births
Still
births
Now
living
Spon.
AB
Induced
AB
Where
Types
Total
Preg
nancies
Complications:
Birthweight over 10 lbs.
Ectopic pregnancies
Multiple pregnancies
RH infants (jaundiced)
Molar Pregnancies
Hemorrhage
424
Patient Name Patient Number
ABORTION COUNSELING
Date ______________________________
Return Date_________________________
Time In _________________ Time Out
Referred from ______________________
Counseling received there? Yes No
1. contraceptive
2. abortion & alternatives
3. personal
Was abortion an easy or difficult decision?
(If difficult, explain below)
Able to discuss decision with concerned others:
Yes No
(If no, explain below)
With her today:
1) Name ______________________________
Relationship__________________________
2) Name ______________________________
Relationship__________________________
3) Name ______________________________
Relationship__________________________
Pregnancy Test
Date __________________________________
Place __________________________________
Positive Negative
Emergency Contact:______________________
Describe Woman’s Mood:
425
Have you ever had professional counseling?
Yes No
If yes, explain _______________________
Contact between 9-4 Monday thru Friday at:
Number Place Letter /Other
Nickname "Shelly" Yes No /Address
Check appropriate box(es):
__ Woman understands and desires termination,
appears to have no problems with this and should do
well.
__ Abortion related problems
_ Other life problems
426
Consent form signed Yes No
Physicians Signature ____________________
Counselor’s signature ___________________
Interview Group Counselor’s signature _____
Recommendations/Referrals ______________
Counselor’s signature_______________
RESCHEDULE/VOID INFORMATION,
Date
Signed
[4]
Patient Name__________________Patient Number
PHYSICAL FINDINGS
Date_______ BP___ P___ Temp____Hgt.___ Wgt._
Return date if applicable___________
BP___ P___ Temp___ Hgt.___ Wgt.___
LMP:__________ Weeks since LMP___________
Sizing_______ LMP Sonar results__________
Name____________________ NP/PA
SBE Prophalaxis__ Yes___No
Comments:
427
Contraceptive Desired 280.C. F&C
PROCEDURE
Date:____________________________
Pelvic Exam: Describe Positive Findings
External Genitalia + - _________
Vaginitis + - _________________
Acute Cervicitis + - ____________
Adnexal Mass or Tenderness + - _
Uterus: Estimated Uterine Size
Weeks from LMP
Anterior Midposition Posterior
OPERATIVE REPORT: VACUUM ASPIRATION
Date__________________________
Sound_______ cm Dilation to:____
Cannula:_____ mm KARMAN
Nesacaine 2% 12cc Carbocaine 1%
Pitressin 2.5 units or 5 units
Other ________________________
Uterine exploration: curette forceps both
I.U.D. + - Molar Degeneration + -
Tissue Volume Small Mod. Large(for gest.)
Villi Seen + - Molar Degeneration + - ?
Fetal Age______ (Weeks from LMP by tissue exam)
Embryo/Fetus: + - Incomplete ?Complete
Probably Complete
Blood Loss:______________cc. Perforation + -
Tissue to Pathology + - Rush + -
Comment:
428
Complications + - (comment below)
Patient state during procedure:
Notes and Comments:
ORDERS FOR RECOVERY AND DISCHARGE
Immune Globulin
_Yes __ No
Valium________ I.M., P.O.____________
Pitocin_____________ cc.________________
Methergine 0.2mg. I.M.___________________
Methergine 0.2mg. P.O. 6 tablets/12 tablets
Doxycycline 200mg. P.O._______________
Other _______________________________
28 day O .C .__________________________
Acetominophen 1000 mg. ______________
Ibuprofen 400 mg._____________________
Other _______________________________
Return for pregnancy test 2 weeks
_Yes __ No
Early Abortion Instructions
__ Yes __ No
Extopic Precautions
__ Yes __ No
The Standard Dilation and Vacuum
Technique was performed as stated above
Signed_______________________________
Time in___________________ Time Out _
Procedure Counselor:
Aspiration
M.D.
429
RECOVERY ROOM
Time of Admission__________ AM/PM Date
Hour
Blood
Pressure
Pulse
Bleed
ing
N Sm
Mod
Hvy
N Sm
Mod
Hvy
N Sm
Mod
Hvy
N Sm
Mod
Hvy
Pain/
Cramps
N M M
S
N M M
S
N M M
S
N M M
S
Allergies: No Yes_______________
Previous Medication
Dosage Route & Site Time By
1.
2.
RH Negative: Yes No
Immune Globulin Given: Yes No
RH Inf. and Card: Yes No
Lab Comments:
430
Medi
cation
Admin
istered
Doasage Route &
Site
Time By
l.Doxy-
cycline
200 mg. P.O.
2.1bu-
profen
400 mg. P.O.
3.
4.
5.
Medication
Dispensed
Dosage Amount By
l.Mether-
gine
0.2 mg. P.O. 6 tablets/
12 tablets
lq. 6 hours
2.Ampi-
cillin
250 mg. QID x 12
doses
3.
431
Contraceptive: 28-day O.C. Type/Amount __________
Given By ________________________ _____
F&C Tubal Vasectomy Diaphragm Has Own/None
Insurance Form Completed: Yes No
MA Forms: Yes No
Post Abortion Instructions:
Instruction Sheet: Yes No
Contraceptive Instructions: Yes No
Can read thermometer? Yes No
Thermometer given Yes No
Check-up: WHS_________ Private M.D.__________
Excuse needed fo r______________________ Yes No
No. of days_______ Given: Yes No
Transportation:
Car Cab Bus Train Plane Walk
Other___
By Self With Family/Friend
Emotional Condition:
Interacts openly Composed Withdrawn Upset
Referred for Personal Counseling
Physical Condition:
No Problems Cramps: Mild Moderate Severe
Other
M.D.
Time of Discharge AM/PM
Signed RN/LPN
Signed RN/LPN
432
Patient Name_________________ Patient Number_
REPEAT PROCEDURE/EMERGENCY CHECK
Date ________________________________________
Time of Admission
________ AM Repeat Procedure Recheck
________ PM Repeat Admission Pis. Circle
PREGNANCY TEST Positive Negative
Pelvic Exam: Describe Positive Findings
Vaginitis + - ____________________
Acute Cervicitis + - _______________
Adnexal Mass or Tenderness + - _________
Uterus: Estimated Uterine Size
(Wks from LMP)
Anterior Midposition Posterior
Carbocaine 1%____ cc Pitressin 2.5 units/5 units
Dilation: Yes to __ Fr. No
Cannula:__ mm BERKLEY KARMAN
Material Aspirated ___________________________
Blood Loss:_____________ cc Perforation + -
Tissue to Pathology + - Rush + -
Comment:
Complications: + - (comment below)
Patient state during Procedure
Notes and Comments ______
Impression: ______________
Plan:___________________________________
ORDERS FOR RECOVERY AND DISCHARGE
Methergine 0.2 mg. I.M. ________________
433
Methergine 0.2 mg. P.O. ___________
Doxycycline 200 mg. P.O. __________
Acetominophen 1000 mg. P.O. _______
Ibuprofen 400 mg. _________________
Other
Return for Pregnancy test 2 weeks Yes No
Ectopic Precautions Yes No
Signed __________________________________M.D.
Time In ________________ Time Out____________
Procedure Counselor:
RECOVERY ROOM
Hour
Blood Pressure
Pulse
Bleeding N Sm Mod Hvy N Sm Mod Hvy
Pain/Cramps N M M S N M M S
Allergies: No Yes _____________________
Previous Medication Dosage Route & Site Time By
434
1 .
Med
ication
Admin
istered
Dosage Route &
Site
Time By
l.Doxy-
cycline
200mg. P.O.
2.1bu-
profen
400mg.
3.
4.
5.
Medication Dispensed Dosage Amount By
1.
2.
Excuse needed for___________ Yes No
No. of days__ Given Yes No
Transportation:
Car Cab Bus Train Plane Walk
Other
By Self With Family/Friend
Emotional Condition:
Interacts openly Composed Withdrawn Upset
Referred for Personal Counseling
Physical Condition:
No problems Cramps: Mild Moderate Severe
Other
M.D.
Time of Discharge a m / pm
Signed RN/LPN
Signed RN/LPN
435
WOMEN’S HEALTH SERVICES, INC.
CONTRACEPTIVE CLINIC
Patient Name_________________ _ Patient Number__
Put an (X) in the appropriate column for each of the
following you have had only since your last visit to the
Women’s Health Services, Inc.
* * *
Patient Name __________________ Patient Number
Visit # Date Visit # Date
Chief Complaint: Chief Complaint:
History: History:
Temp. BP P Wt. LMP Temp. BP P Wt. LMP
Thyroid: Thyroid:
Breasts: Breasts
Heart: Heart:
Lungs Lungs
Abdomen: Abdomen:
436
Pelvic: Vulva Pelvic: Vulva
Vagina Vagina
Cervix Cervix
Corpus Corpus
Adnexa Adnexa
Rectal Rectal
Extremeties: Extremeties:
Tests: PAP GC Tests: PAP GC
Wet Prep Wet Prep
Other Other
Impression: Impression:
Plan: Plan:
Contraception: Contraception:
Next Appointment:
Wks. Mos.
Next Appointment:
Wks. Mos.
RN/PA M.D. RN/PA M.D.
437
* *
CONSENT FOR ABORTION
I hereby authorize a Staff Physician to perform upon
me a VACUUM ASPIRATION ABORTION, including
all the medical aspects, which have been explained to
me.
I consent to the administration of anesthesia to be
applied by or under the direction of the staff physician,
and to the use of such anesthetics as s/he may deem
advisable.
In the course of the abortion if any unforseen
condition arises which, in accord with good medical
practice, calls for procedures in addition to or different
from those contemplated, I further request and authorize
the staff physician to perform such procedures, and to
administer any medication which s/he may deem
advisable and to have me admitted to a hospital facility.
I understand it is my responsibility to bring to the
attention of Women’s Health Services, Inc. any unusual
symptoms following the abortion and to report for check
ups and pregnancy tests as recommended.
I understand the nature and purpose of an abortion
by vacuum aspiration. I understand that there are other
abortion techniques. I understand the alternatives to
abortion, including childbirth and adoption. I understand
the risks involved with an abortion, and the possibility of
complications and detrimental physical and psychological
effects which may occur. These include, by way of
illustration and not limitation, hemorrhage, infection,
perforation, hem atom etra, cervical damage,
incompleteness as well as the possible need for further
surgery (e.g. laparoscopy, laparotomy, hysterectomy,
removal of tubes and ovaries), possible sterility and
fatality. All of these matters have been fully explained
to me.
438
I authorize Women’s Health Services to dispose of
all fetal tissue in accordance with state and federal laws.
I CERTIFY THAT THIS ENTIRE ABORTION
CONSENT HAS BEEN READ TO ME AND THAT I
HAVE READ OR HAD THE OPPORTUNITY TO
READ THE ENTIRE CONSENT FORM AND THAT
I UNDERSTAND THE ABOVE CONSENT FOR
ABORTION AND THE THE EXPLANATIONS
HEREIN REFERRED TO WERE MADE.
Date__________ Time__________
Signature of Patient______________________________
Signature of Person authorized to give consent, if not
patient ________________________________________
Relationship to Patient________________________
Signature of Physician____________________________
Signature of Witness______________________________
ECTOPIC PRECAUTIONS
I certify that I have received a copy of the sheet
listing the precautions for possible extopic pregnancy,
have read it and understand the importance of the
medical follow-up. Date
Signature of Patient _____________________________
Alternate contact person in addition to myself:
Relationship ______ _________________________
Phone Number ___________________________
Signature of Witness _____________________________
EARLY ABORTION SPECIAL INSTRUCTIONS
I certify that I ahve received a copy of the sheet
describing the special instructions for early abortion
patients, have read it and understnad the importance of
the medical follow-up. D ate______________
Signature of Patient
Alternate contact person in addition to myself:
439
Relationship_________________________________
Signature of Witness _____________________________
POST ABORTION INSTRUCTIONS
I certify that I have received a copy of the sheet
describing instructions for after the abortion, have read it
and understand the importance of the medical follow-up
Date___________
Signature of Patient _____________________________
Signature of Person authorized to give consent, if not
patient:
Relationship ________________________________
Phone Number_______________________________
Signature of Witness _____________________________
CONSENT FOR ORAL CONTRACEPTION
I have received and agreed to read the patient
information enclosure regarding oral contraceptives
distributed by the manufacturer. I understand that it is
my responsibility to bring to the attention of Women’s
Health Services, Inc. any unusual symptoms and to report
for check-ups as recommended. I CERTIFY THAT I
HAVE READ (OR HAD READ TO ME) AND
FULLY UNDERSTAND THE ABOVE CONSENT TO
CONTRACEPTIVE SERVICES AND SUPPLIES, AND
THAT THE EXPLANATIONS HEREIN REFERRED
TO WERE MADE. Date___________
Signature of Patient _____________________________
Signature of Person authorized to give consent, if not
patient:
Relationship to patient
Phone Number______
Signature of Witness
440
I do hereby consent to have Women’s Health Services,
Inc. provide to me the service noted below.
Date_______________ Gynecological Exam
Signature of Patient_______________________
Date_______________ Antibiotic Therapy
Signature of Patient_______________________
Date_______________ Lamicel Insertion
Signature of Patient_______________________
FINANCIAL PAGE
Insurance Company ______________
Insurance Address________________
Agreement # ___________________
Group # ________________________
Subscriber_______________________
Sub. Employer___________________
HMO Center____________________
HMO M R #_____________________
HA Family I.D.# ________________
MA # __________________________
Line # _____________________ R.C.
State _________________
Exp. Date_____________ D.D.
D.D.
D.D.
D.D.
D.D.
M C/Visa#______________________
Sub. Name______________________
Exp. Date_______________________
441
Defendants’ Exhibit 8:
WHS Advertisements
The Pittsburgh Press
Ask a friend
"I was very pleased with the professionalism and
personal treatment. I would refer any of mv
friends to WHS."
About Women’s Health Services
"Counseling Services for Men & Women"
"PMS Program-Abortion Services-Gyn Care"
Fulton Building ■ 107 6th St.
Downtown Pittsburgh
(412) 562-1900
WAMO 1500 Chamber of Commerce Bldg.
FM 106 Pittsburgh, Pennsylvania 15219-1905
(412) 471-2181
WOMENS HEALTH SERVICES.....
IF Y O U ’RE C O N C E R N E D ABO U T AN
UNPLANNED PREGANCY...HELP IS JUST A
PHONE CALL AWAY....562-1900. WOMENS
H E A L T H S E R V I C E S ___ F U L T O N
BLDG...DOWNTOWN OFFERS YOU HELP IN
MAKING DECISIONS ABOUT YOUR LIFE.
WOMENS HEALTH SERVICES HAS A HIGHLY
442
SKILLED GYNECOLOGICAL STAFF AND A
COUNSELING STAFF AND YOUR VISIT WILL BE
KEPT COMPLETLY CONFIDENTIAL. IF THE
PIECES OF THE PUZZLE DON’T QUITE FIT...LET
WOMENS HEALTH SERVICES HELP....OUR
PHYSICIANS PROVIDE SKILLED MEDICAL CARE
AND YOU’LL BE TREATED IN A REASSURED
AND COURTEOUS MANNOR. FOR A GYN
APPOINTMENT..OR ANSWERS TO QUESTIONS
ABOUT AN UNPLANNED PREGNANCY CALL THE
PHONE STAFF AT 562-1900....BETWEEN 8 and 5PM
...MONDAY THRU FRIDAY....SATURDAY 8 to
4PM.....WOMENS HEALTH SERVICES...IN THE
FULTON BUILDING ...DOWNTOWN.....FREE
PREGNANCY TESTING IS AVAILABLE DAILY.
FOR MORE INFORMATION CALL WOMENS
HEALTH SERVICES AT 562-1900.....HELP IS JUST A
PHONE CALL AWAY.
THE CAMPUS
OF ALLEGHENY COLLEGE
Ask a friend
"Everyone treated me nicely. I felt comfortable
and relaxed, the procedure was explained step by
step. I liked that."
About Women’s Health Services
Where Experience Makes A Difference
Early & Later Abortions-Confidential Counseling
Fulton Building ■ 107 6th St.
Downtown Pittsburgh
443
1-800-323-4636
Phone Listing:
ABORTION SERVICES DIVISION OF
WOMEN’S HEALTH SERVICES INC
1st & 2nd Trimester Abortions in a
comfortable setting. Highest medical
standards.
107 6 St Pittsburgh PA
Toll Free Dial "1” & Then--800 426-4636
444
Defendants’ Exhibit 9:
Excerpts from Planned Parenthood
of Southeastern Pennsylvania (PPSP)
Center Policy and Procedure Manual
C. Counseling and education.
1. All pregnancy test clients will receive
appropriate options counseling if desired by patient.
Intensive counseling may be scheduled for a separate
visit if deemed necessary by client and counselor.
2. The purpose of pregnancy counseling and
referral is to support a woman in clarifying and
achieving her immediate reproductive goal. All
applicable alternatives (parenting, adoption, foster
care, infertility testing, pregnancy termination,
contraception) will be presented in an unbiased
manner. As a result of the counseling session, the
patient should understand:
a. Her alternatives, including description and
approximate cost of services, and time
constraints.
b. Advantages and disadvantages of her
alternatives.
c. Specific resources for reaching her goal,
including the support of her partner, friends
and/or family, medical care, financial aid,
transportation, bilingual services, counseling and
education.
d. Methods of contraception available if found to
be not pregnant.
e. What to do in an emergency.
f. Information about the accuracy of the test.
445
3. All counseling is confidential (within leqal
limitations) and will be conducted in privacy.
a. Results should be given to the woman alone
and the partner or significant other brought in if
desired by her.
4. Every patient age 17 and younger who is making
a decision concerning a positive pregnancy test shall
be encouraged to talk to a parent or an alternative
adult.
5. Every patient should be given the opportunity to
consider:
a. Clinical information with reqard to her
gestation of pregnancy.
b. Any aspect of her medical evaluation which
pertains to the options available to her.
c. Review of contraceptive history and plans.
d. Options available for continuing or
terminating a pregnancy, including appropriate
referrals.
e. Potential effect each option suggests for the
future.
6. A Consumer Feedback Form (#54) must be
given to each patient referred for abortion services.
a. Request the patient return the Consumer
Feedback Form within six weeks.
7. Document that pregnancy alternatives were
discussed.
8. Pregnancy options counseling may be offered
without testing if woman brings written results of a
positive pregnancy test done elsewhere. Women
who have used home pregnancy tests should have
446
another test done at the Center.
D. Referrals.
1. Prenatal care and delivery.
a. A minimum of two direct service referrals
must be provided.
b. The CHOICE Hotline can be given as an
additional resource.
2. Adoption and foster care.
a. Provide the patient with appropriate referrals.
3. Abortion.
a. A minimum of three referral sources is given
from the approved Referral Lists (#55a and
55b) as indicated and available.
4. Up to date information is maintained at each
site regardinq social services, Medicaid, drug abuse
programs, as well as all medical referrals.
5. Document all counseling, advice, and referrals
on the medical record.
6. Consumer Feedback form (#54) is given to
patient to be completed and mailed back to PPSP
center.
E. Counseling personnel.
1. Personnel suitable for pregnancy options
counseling
a. Physicians, clinicians, Center Managers,
Center Assistants, social workers, and selected,
trained and appropriately supervised volunteers.
447
2. Qualifications of counseling personnel.
a. The ability to respect, understand and
empathize with the woman as an individual.
b. A sincere belief in the right of the woman to
make her own decision after she has explored all
the options.
3. Training of counseling personnel.
a. The counselor must have a complete
knowledge of the facts regarding abortion.
These include:
1) The facts about relative risks of early
abortion as opposed to late abortion;
2) Availability of services;
3) Facility evaluation;
4) Cost of services.
b. Counselors must be thoroughly knowledgeable
about all methods of contraception and
community-wide contraceptive services.
c. Counselors must have knowledge regarding
facilities for prenatal care.
d. Counselors must have knowledge regarding
the necessary procedures for adoption and the
location of adoption agencies.
e. Counselors must have knowledge regarding
the availability of insurance coverage or other
reimbursement for abortion, and prenatal care
and delivery.
f. Counselors must have knowledge of the
availability of psychiatric consultation which may
be requested or which may be medically
advisable.
g. Counselors must be familiar with all legal
requirements for sterilization procedures which
may be requested in conjunction with abortion.
448
* *
K. Procedure for Center Assistant/Counselor.
1. Each patient will be seen individually by a
Center Assistant/Counselor. Counselors will pick up
charts, so keep completed charts in order. Keep
Center Manager informed of unusual situations that
may need special attention or patients with potential
problems.
2. Have on hand:
a. Pap slips.
b. GC slips.
c. Serology slips.
d. Medical and information forms.
e. Several pens.
f. Pencil.
g. China marker.
3. Greet patient and take her to counseling office.
Explain your role as it relates to patient visit and
Center procedure. The counselor performs role of
advocate, assistant, and support to the patient.
4. Review patient’s medical history (#16) with her.
Make special note of potential problems and consult
with appropriate staff as needed. Be sure all forms
are completed.
5. Discuss patient’s decision to have an abortion
and provide opportunity for her to explore feelings.
Let her know other options are available and you
can provide her with referrals. Involve others
accompanying client to facility, if appropriate.
Support person can be included in procedure room
449
if, in staffs judgement, their involvement would be
supportive to the client.
6. Explain, answer questions, discuss the abortion
fact sheet (#21), including risks, and consent (#18).
Have client sign and witness. Must be able to give
informed consent.
7. Review birth control methods (#42) and discuss
patient’s choice. Have patient sign contraceptive
consent and witness.
8. Review "safer sex" practices.(#99)
9. Review possible medical concerns with Center
Manager, medical support staff, and physician prior
to the procedure.
10. Ascertain that slips for GC and Pap have been
completed and are in the patient’s chart. Label Pap
slides, GC plates with client name, date, and
specimen number if appropriate. Be sure all
specimen numbers have been recorded on lab sheet
in chart.
11. Record results of pregnancy test, urine dipstick,
hematocrit, and Rh factor on lab sheet in chart.
12. Record drug allergies and significant medical
problems in red on outside of chart.
13. Provide a written social history in patient’s
record reflecting the counseling session. The
followinq questions can be used in evaluating the
abortion counseling session:
a. Do I feel I have a clear picture of the
450
woman’s intellectual and emotional status in
regard to her abortion decision?
b. Are there conflicts between her emotional and
intellectual status on the abortion decision?
c. Who else is involved in decision-making and
what are their reactions? Does this woman have
support for her decision?
d. If the woman decided alone, how did she
reach the decision to do so and what are her
feelings about it?
e. What are her contraceptive plans for the
future?
f. Were there other problems, i.e. relationship,
sexuality that were dealt with?
g. How will she react post-abortion? Does she
desire future counseling services?
h. Is she clear in regard to the abortion
procedure?
i. For extended first trimester procedures, follow
all of the above steps plus:
1) Explain laminaria insert procedure plus
possible complications.
2) Have patient sign laminaria consent
(#90) and witness.
3) Schedule abortion appointment for the
following day and review pre-abortion
instructions.
* * *
451
Defendants’ Exhibit 10:
Excerpts from PPSP
Request for Abortion Form
Planned Parenthood Southeastern Pennsylvania
Request for Abortion
Name
Address_____________________ Birth Date_______
I have received from Planned Parenthood a fact
sheet containing detailed information on the nature and
purpose of an abortion, the risks involved, and the
possibility of complications. I have read the fact sheet
which has been explained to me, and which I understand.
I have had all my questions answered. I also understand
that a doctor is available to answer any additional
questions I may have. No guarantee or assurance has
been made to me as to the results which may be
obtained and I am aware, on the basis of the fact sheet
and the explanation I received, of the risks involved in
an abortion and the possible complications.
I hereby request that a doctor authorized by Planned
Parenthood perform an abortion upon me if s/he, in
her/his medical judgment approves the performance of
the abortion. If any unforeseen condition arises in the
course of the abortion calling in her/his judgment for
procedures in addition to or different from those
contemplated, I further request and authorize her/him to
do whatever s/he deems advisable to protect my health
and welfare.
452
I consent to the administration of a local anesthetic.
To my knowledge, I am not allergic to any anesthetics.
I hereby give my permission to the employees of
Planned Parenthood Southeastern Pennsylvania and
others authorized by them to use information contained
in my medical record for statistical purposes, with the
understanding that confidentiality will be maintained.
Signature________________________ Date_________
I witness the fact that the patient received, read, and
said she understood the fact sheet.
Witness________________________________________
[ ] Physicians must sign only for minors under the age
of 18 without parental consent:
I have discussed with the patient the abortion she
has requested and I believe she is sufficiently mature and
intelligent to understand the nature and consequences of
her condition and of the procedure. I believe that the
abortion she has requested is in her best interest.
Physician
453
Defendants’ Exhibit 11:
Excerpts from PPSP Fact Sheet
Facts About Early Abortion
What It Is
A surgical procedure to end a pregnancy within 14
weeks from the first day of the last menstrual period.
How It Is Done
The standard method is vacuum aspiration (suction
curettage):
1. A local anesthetic is injected into or around
the cervix (the lower part of the uterus). You
may notice stinging or pressure, which goes away
quickly. Some women don’t feel anything.
2. The opening of the cervix is stretched slowly
by a series of narrow rods (dilators), each a little
wider than the one before. The largest dialator
may be about as thick as a fountain pen. You
may feel strong cramping during this part of the
procedure.
3. When the cervical opening is wide enough to
admit it, a cannula (a hollow plastic tube) is
inserted into the uterus. This tube is attached to
a suction machine, which is then turned on. You
may notice a pulling or tugging feeling at this
time.
4. After the uterus has been emptied by gentle
suction, an ordinary spoon-shaped curette may
be used to make sure that the uterus has been
454
emptied.
Possible Problems
As with any kind of surgery, complications can occur
with early abortion. Early abortion by vacuum aspiration
is, however, very safe. Fewer than 1 woman in 100 will
have a serious problem, including but not limited to:
Infection
Infection is caused by germs from the vagina and
cervix getting into the uterus. The risk of infection
related to early abortion is less than 1 in 100 cases.
Such infections mostly respond to antibiotics, but, in
some cases, a repeat vacuum aspiration or
hospitalization is necessary. Surgery may also be
required. You can decrease your chances of
developing an infection by not having intercourse
until after your post-abortion exam and not inserting
ANYTHING into your vagina, including tampons.
Bleeding
Bleeding from the uterus heavy enough to
require treatment occurs less than 1 in 1,000 cases.
This bleeding problem may require medications to
help the uterus contract, a repeat vacuum aspiration
or dilation and curettage, or rarely, surgery.
Cervical Tear
The cervix sometimes is torn during the
procedure. This happens in less than 1 in 100 cases.
Stitches may be required to repair the injury.
Incomplete Abortion
Sometimes, the contents of the uterus may not
be quite emptied. The frequency of this event is less
than 1 in 100 cases. This problem can lead to
455
infection, hemorrhage, or both. To remove the
tissue, it may be required to repeat the vacuum
aspiration or perform a dilation and curettage at the
clinic or in a hospital. In rare instances, surgery may
be required.
Perforation
Rarely, an instrument may go through the wall
of the uterus. This event happens in about 2 per
1,000 cases. Should this happen, hospitalization is
often required for observation and/or completion of
the abortion. To inspect the condition of the uterus
in this state, a small telescope (laparoscope) is
inserted through the navel. Sometimes, an
abdominal operation is required to repair the
damage. This can include hysterectomy (removal of
the uterus), which makes it impossible to have
children. The frequency of hysterectomy in this
setting is about 1 in 10,000 cases.
Failure to Tertninate the Pregnancy
Once in a while, the early abortion procedure
will not end the pregnancy. The chance of this event
is about 2 per 1,000 cases. This possibility is one
reason that a post-abortion examination is essential.
In such cases, another abortion procedure is
suggested, since the first attempted abortion can
harm normal development of the pregnancy. The
other possibility is that a tubal (ectopic) pregnancy
may exist, which requires an abdominal operation to
remove.
Death
Early abortion is one of the safest operations in
all of medicine. Information from the Centers for
Disease Control (CDC) shows that the risk of death
456
from an early abortion is about 1 per 100,000 cases.
In contrast, the risk of death related to tonsillectomy
is about 3 deaths per 100,000 cases. The risk of a
woman dying from full-term pregnancy and childbirth
is at least 7 times greater than that from early
abortion.
Anesthesia Reaction
Some women may be allergic to novocaine
derivatives. If you know this, it is important to tell
the doctor.
Effect of Abortion on Future Wanted Pregnancies
At this point there is no clear proof that one
early abortion carries any risk to future pregnancies.
Some studies have shown that women who have had
two or more such abortions may have an increased
risk of premature births or miscarriages in future
pregnancies. Different studies have shown otherwise.
Emotional Reactions
Strong feelings after abortion are common, and
when they happen they mostly go away quickly.
Most women report a sense of relief, although some
feel depression or guilt. Serious psychiatric
disturbances (such as psychosis or serious
depression) after abortion appear to be less frequent
than after childbirth.
Deciding whether or not to have an abortion is a
very private matter. You need to be sure and
comfortable that having an abortion is what you want to
do, even if it is a hard decision to make.
457
Defendants’ Exhibit 13:
Excerpts from Guidelines of
Women’s Suburban Clinic (WSC)
Guidelines of Women’s Suburban Clinic (WSC)
Protocol
OPTIONS COUNSELING/REFERRAL
I. ELIGIBILITY: Any woman who has
-- a positive pregnancy test
-- requests options counseling at
WSC
-- is eligible for options counseling.
II. INTAKE:
- An appointment card is used for information
on options counseling clients (see forms).
-- This card is completed as described in
abortion intake procedures except that the
medical history is not necessarily taken (if
medical history is not taken this is noted in
pencil on front of card).
-- Appointments are scheduled during the
counselor’s assigned times, as designated in
the appointment book.
-- Options counseling clients are NOT given a
"Disclosure of Risks, Benefits, and
Alternatives to Abortions" to read after they
return their medical history to the front
desk.
458
* *
V. DISPOSITION:
- If a client chooses to have an abortion, she
can be scheduled for an appointment at
WSC or referred to another appropriate
facility (see Referral Counseling). If a
woman chooses to have an abortion at WSC,
the appointment should not be made for the
same day as the option counseling.
-- If a woman chooses to continue the
pregnancy, the counselor may make a
referral to appropriate community resourses
(Examples: Pre-natal Care or Adoption
Informatian).
- Options Counseling Notes will be recorded
by the counselor (see forms-Appendix B).
* * *
ABORTION AND SUPPORT SERVICES
VII. COUNSELING
The individual counseling is provided to all women
who come to WSC for abortion services (see
Counseling Standards). This counseling, usually
done on the same day as the abortion, is not offered
for the purpose of exploring pregnancy (see Options
Counseling), although alternatives may be discussed.
Rather, this counseling session assumes that the
decision to abort has been carefully thought out
prior to the session. The objectives of this session
459
are clearly defined under "Objectives" in the
Counseling Standards section of the WSC
Guidelines.
If, in the process of the session, the counselor
determines that the client has not clearly decided to
abort, he/she will suggest that the client not proceed
with the abortion that day. The counseling session
then procedes under the protocol for "Options
Counseling, with the abortion (if chosen) being
rescheduled for another day.
c. The Counseling Session: The pre-abortion session
flows according to the clients needs and questions.
The client’s partner or other accompanying person is
also encouraged to accept information, ask questions,
and explore feelings at WSC. These "signifigant
others" may be invited to joinq the counseling
session, but only after the women has seen the
counselor alone, thus giving her the opportunity to
discuss any private concerns, (see also, Counseling
Signifigant Others).
* *
E. Limitations and Referrals: The counselors role is to
discuss the clients’ concerns primarily regarding the
abortion decision. For those women who display a
need for further counseling or assistance which is
non-abortion related, the counselor may refer the
client to an appropriate agency or individual. A
resource book is maintained by WSC under the
supervision of the head counselor. The Resource
Book includes numerous community resources.
460
F. Counseling Signifigant Others: Any person who
accompanies a client to WSC is offered the
opportunity and is encouraged to see a counselor.
This may include the client’s partner, her parents,
and/or any "Signifigant Other". The counselor may
see the Signifigant Other with the client, or after the
clients’ counseling session. This is left up to the
discretion of the client and the counselor.
* * *
461
D e f e n d a n t s ’ E x h ib it 14:
W S C D is c lo s u r e o f R is k , B e n e f it s
a n d A lte r n a t iv e s F o rm
WOMEN’S SUBURBAN CLINIC
DISCLOSURE OF RISKS, BENEFITS AND
ALTERNATIVES
Because abortion is a form of minor surgery, which, like
all surgery, has certain statistical risks, it is the policy of
Women’s Suburban Clinic to provide detailed
information regarding the risks, benefits and alternatives
to abortion so that you can make a clear and conscious
choice.
Alternatives: The alternative to ending a pregnancy is to
continue it to term and birth. This usually leads to
parenthood or adoption. Pregnancy and childbirth have
some medical and psychological risks. Both the benefits
and risks of parenthood and adoption should be carefully
considered before deciding upon an abortion.
Benefits: The benefits of early abortion depend upon the
individual. Abortion permits the planning of parenthood.
Abortion eliminates the decision between parenthood
and adoption.
Risks: 96% of all early abortions take place without any
complications at all. Complications associated with
abortion are generally less frequent than with childbirth.
In childbirth some 15 to 20 out of 100,000 women do not
survive. Abortion is 5 to 10 times safer.
462
Below is a list of possible complications to abortion.
You will be asked to sign a consent form indicating that
you understand these risks before you have an abortion.
Please read this form carefully so that you understand
that we cannot guarantee that the results obtained from
an abortion will always be perfect. Complications may
occur and require further treatment. A member of
Women’s Suburban Clinic staff is on-call 24 hours a day
for consultation; and we will assume financial
responsibility for treatment of all medical (not
psychological) complications to abortion if such
treatment is given at or recommended by Women’s
Suburban Clinic.
Medical Risks:
a) Risk of Infection: In approximately 1 in 100
cases, minor or possible major infections can occur after
an abortion. Antibiotics are necessary to treat these
infections and, very rarely, infections may lead to
reduced fertility.
b) Incomplete Abortion: Sometimes all of the tissue
may not be removed during the abortion. This happens
in approximately 1 in 100 cases, and may lead to
infection unless treatment is begun soon or the abortion
is redone.
c) Continued Pregnancy: In as many as 1 in 100
cases, a woman may still be pregnant after an abortion.
This may be due to multiple pregnancies (i.e. twins), a
double uterus, or a pregnancy in the tubes (ectopic
pregnancy). A failed abortion may be detected by
follow-up exam and pregnancy test after which the
abortion can be redone. A tubal or ectopic pregnancy is
difficult to detect and will require a hospitalization and
surgery.
463
d) Bleeding or Hemorrhage: Heavy bleeding
immediately or shortly after an abortion may happen in a
very small number of cases. This requires evaluation and
treatment, which depends upon the cause of the
bleeding.
e) Perforation or Laceration: Very rarely an
instrument may tear the cervix or puncture the wall of
the uterus. These cuts will generally heal themselves,
with no treatment, but occasionally they may require
hospitalization or surgery.
f) Anesthetic Reaction: Anesthetics do not always
eliminate all pain. In very rare instances, local
anesthetics cause extremely severe reactions, including
convulsions or cardiac arrest.
Psychological Risks:
Sometimes women express negative feelings after
having had an abortion. These feelings may include a
sense of loss, guilt, regret or sadness.
The likelihood of your experiencing these feelings
depends on many factors including your feelings about
abortion, your religious convictions, your cultural and
social norms, and the support you receive from your
family and friends.
You will have the opportunity to discuss these
factors with a counselor before the abortion to reduce
the likelihood of their causing negative feelings later. If
negative feelings do occur, you may return to Women’s
Suburban Clinic for counseling and/or referral for more
involved therapy.
464
INFORMATION PRIOR TO CONSENT
I, , certify that on
___________________ , 1988, I orally informed
_________________________ prior to her consenting to
an abortion, of the nature of the proposed procedure and
treatment of abortion and of the risks and alternatives to
abortion or treatment that a reasonable patient would
consider material to the decision whether or not to
undergo the abortion.
D e f e n d a n t s ’ E x h ib it 17:
W S C I n fo r m a t io n P r io r to C o n s e n t /
C e r t if ic a t io n by P a t ie n t F o r m
physician qual i f i ed physician
assistant
health care practitioner technician delegated by
either physician
CERTIFICA TION BY PA TIENT
I, _____________________ , certify that prior to my
consenting to an abortion at the Women’s Suburban
Clinic, the person who has signed the above statement
called INFORMATION PRIOR TO CONSENT ’ told
me about the nature of the proposed procedure and
treatment of abortion and of the risks and alternatives to
abortion and treatment.
Date:____________ , 1988
patient
465
D e f e n d a n t s ’ E x h ib it 18:
W S C P a r e n ta l In v o lv e m e n t F o r m
Parental Involvement
I , _______________________ have carefully considered
with the counselor the possibility of involving my parents
or guardians in my decision to terminate my pregnancy.
However, I choose not to do so. I understand that if,
during my abortion, I have any complications which
hospitalization, the hospital may choose to call my
parents. On the medical history form, I have given
Women’s Suburban Clinic the number where my parent
can be reached in case of emergency.
Client’s Signature
or
I am the parent/guardian o f_________
and I am aware of her decision to abort.
Signature
or
My parent/guardian is aware of my decision to abort, but
could not be present today. I have given Women’s
Suburban Clinic a number where my parent can be
reached in case of emergency.
Client’s Signature
466
Defendants’ Exhibit 19:
WSC Physician’s Certification Form
PHYSICIAN’S CERTIFICATION
I certify that prior to the abortion I had a private
medical consultation with the above client and
determined that in my best clinical judgment the
abortion was necessary.
Signature of Physician
467
Defendants’ Exhibit 20:
WSC Protocol Regarding Minors
II. STANDARDS
D. Protocol Regarding Minors
1. It is one of the underlying philosophies of Women’s
Suburban Clinic that all women capable of informed
consent be provided the opportunity to "choose".
These choices involve the decision regarding an
unplanned pregnancy, the decision regarding whom
they choose to inform about their pregnancy and
what method of birth control they choose to use. As
with any woman, this philosophy also pertains to
minors. However, in the case of a minor (any
woman under 18 years of age), the issue of whom
she chooses to inform or not inform is carefully
explored.
2. For any minor who at the time of scheduling her
abortion has not informed one of her parents of her
decision, the following will occur:
a. Anyone under 18 years of age whose parent(s)
do not know about her decision to have an
abortion is strongly encouraged to come to
Women’s Suburban Clinic for precounseling.
The reason for this is to allow the counselor on
opportunity to explore more fully with the young
woman her feelings regarding involving her
parent(s). Further, a pre-counseling session
would allow the teenager time to discuss her
pregnancy with her parent(s) in the event that
after counseling she chooses to do so. If the
young woman chooses not to involve her
parent(s) the counselor would then want to
468
explore other people (siblings, other relatives, or
friends) who could provide a support system. It
is ultimately the right of this teenager to decide
whom, if anyone, she wants to involve. In all
cases the minor will be asked on her Medical
History form the name of her parent or
guardian, and how to contact them in the event
of an emergency.
3. For those minors who choose not to inform their
parent(s) it is the role of the Women’s Suburban
Clinic staff, as with all clients, to review and educate
them regarding how to take a temperature and read
a thermometer, what is considered a complication,
and what to do in the event that a complication
occurs.
4. All minors will be asked to complete a parental
involvement form at the completion of counseling.
469
Defendants’ Exhibit 26:
Excerpts from Reproductive Health and
Counseling Center (RHCC)
Consent Forms
INFORMATION PRIOR TO CONSENT
I, __________________________________, certify
that on _________________ , 19_, I orally informed
_________________prior to consenting to an abortion,
of the nature of the proposed procedure and treatment
of abortion and of the risks and alternatives to abortion
or treatment that a reasonable patient would consider
material to the decision whether or not to undergo the
abortion.
PHYSICIAN QUALIFIED
PHYSICIAN
ASSISTANT
HEALTH CARE TECHNICIAN
PRACTITIONER DELEGATED BY
EITHER PHYSICIAN
(COUNSELOR)
470
CERTIFICATION BY PATIENT
I, _________________________ , certify that prior
to my consenting to an abortion at the Reproductive
Health and Counseling Center, the person who has
signed the above statement called "Information Prior To
Consent" told me about the nature of the proposed
procedure and treatment of abortion and of the risks and
alternatives to abortion and treatment.
________ , 19_________________________________________________
DATE PATIENT
PHYSICIAN’S CERTIFICATION
I ,_________________________ , hereby
Patient’s Signature
acknowledge that I will have a private medical
consultation with D r.________________. I have just
cause to terminate this pregnancy because of the
following reason:
471
Physical
Emotional
Psychological
Familial
__ Age
l ___________________________________________________ ,
M.D. through a private medical consultation, do hereby
certify that to the best of my clinical judgment this
abortion is necessary.
* * *
After careful consideration I have
decided:
1) I will not inform my parents of my
decision to terminate my pregnancy.
(2) Parent(s) are aware of my decision,
but are unable to be here today.
472
I understand that while I am a patient of
the Reproductive Health and Counseling
Center that all reasonable measures will
be taken to maintain my confidentiality.
However, if it is necessary for me to be
hospitalized at any time during or after
my care here, the hospital may choose
to notify my parents about any treatment
they may give me.
Name
Date
Witness
473
Defendants’ Exhibit 30:
RHCC Advertisements
REPRODUCTIVE HEALTH AND
COUNSELING CENTER
■ first and second
trimester abortion
services
■ general & local
anesthesia
■ Routine gynecology
care
■ pregnancy testing
■ counseling services
■ vd screening
■ vasectomy service
Quality reproductive health care . . .
ALL SERVICES HELD
IN STRICT
CONFIDENCE!
Call 874-4361
(Crozer Chester Medical Center Annex)
15th & Upland Av Chester, Pa.
474
Defendants’ Exhibit 32:
Allentown Women’s Center (AWC)
Counseling Checklist
COUNSELING CHECKLIST
1) Determine that patient has a clear decision to
terminate pregnancy, knows options, and determine a log
reasons for abortion (ie: financial, emotional, age, timing
factor, life circumstances, medical, doesn’t want children
or any more children).
2) If first pelvic exam, prepare patient.
3) Explain procedure, discuss pain management, assuage
fear, empower patient.
4) Obtain informed consent, explain risks.
5) Review medical history and flag problems, discuss if
abnormal menstrual period.
6) Explore birth control - pursue and explain only if
patient desires the information
7) Have patient sign appropriate consents. Must sign
abortion consent, dispensing of medication consent, and
medical records release. Oral contraceptive consent
must be signed only for those patients wanting to start
the pill immediately.
ADDITIONAL INFORMATION REQUIRED FOR
GENERAL ANESTHESIA
475
1) Provide complete aftercare instructions.
2) Explain how to take oral contraceptives for those
patients taking then for the first time.
3) Have patient sign general aneathesia consent.
4) Obtain patient’s driver’s signature.
MINORS
1) Explain that if complications develop, their
confidentiality may be broken.
2) Make certain minor knows all options.
3) Determine and record whether patient’s parent(s) are
here or know she’s here. Record reason(s) why a patient
chose not to tell her parents.
4) If a parent is here, the parent MUST co-sign for
abortion.
IMPORTANT FACTORS TO CONSIDER WHEN
DOING PRE-ABORTION
COUNSELING
1) Make no promises that there will be no problems now
or later.
2) It is better to see patient alone, at least briefly.
3) Counseling should be organic and cover concerns
patient presents. Be empathetic, nonjudgemental, and
caring.
4) Body language of counselor is just as important as
what she says.
5) Observe patient to make sure she’s listening. Do not
over inform. Her ability to process may be restricted.
6) Be nonjudgemental in recording counseling notes.
(Do NOT record anything that you wouldn’t want patient
to read, or anything that could be used against her later,
ie: court).
7) Repeat patients who have had more than one
476
abortion. Review risks, and concentrate efforts on
encouraging effective birth control use.
8) Prepare patient for being ineligible for procedure if
you suspect she could be greater that 14 weeks LMP.
9) If patient is greater than 12 weeks LMP, advise her
that she may need an ultrasound.
10) If you feel uncomfortable (for any reason) counseling
a particular patient, give that patient to another
counselor.
11) Ambivalent patient: When you have exhausted all
possible information giving and patient is still ambivalent
you can give patient these options.
a) Offer patient to leave the clinic and rethink
decision. Give her time that she must be back if she still
wants abortion that day.
b) Have patient and significant other sit together in
counseling room to discuss decision. Counsel another
patient and go back to her later.
c) If you feel patient needs more time to decide, you
have the right to tell her that we can reschedule her
appointment for another day, that she needs more time
to make her decision.
12) Time management is important with short term
counseling. If you are having a problem with a
counseling session, notify clinic supervisor so that patient
flow won’t be disturbed.
13) Take time to share, vent, and discuss counseling
cases with other counselors here.
14) If you are having any problems with a client in
counseling don’t hesitate to have another counselor or
clinic supervisor assist you with that particular client.
477
Defendants’ Exhibit 33:
Excerpts from AWC
Confidential Patient Record Form
* *
For patients under 18:
Who of the following knows of and consents to your
abortion?
Mother_______________ Father_______________
Guardian________________
If they are not aware you are here, why not?
PROCEDURE
Name_______________________ Date__________
Patient discussed need for aboriton with physician and
stated it is necessary __________________________
Physician’s Initials
BP_______ P_______ Temp.______
LMP Date_______ or_______ weeks LMP
Heart_______ Lungs_______ Abdomen_____
Comments ___________________________________
Pelvic Exam: Normal ________________________
Abnormal findings: ______________
Uterus: Anterverted__________________________
Retroverted_________________________
Midposition_________________________
Estimated duration of gestation based on uterine size:
Pap smear __________________________________
GC culture, cervix___ rectum___ urethra
478
pharynx___
Room_______________ Nurse:________________
Pre-op medication:_______________________________
OPERATIVE REPORT
Procedure Performed
Patient was placed in dorsal lithotomy position,
prepped and draped in usual manner. A
paracervical block was administered using___ cc of
___ % ____ caine. The uterus was sounded to
___ cm. The cervix was dialated to a # ___
dialation using gradually increasong dialators. A
# ___ cannula was placed in the uterus and vacuum
aspiration was performed. Uterine exploration with
a sharp curette followed. Estimated blood loss was
___ cc. Gross examination of POC Grams_______
Normal POC______ Other (describe)_______
Villi seen______ Consistent w ith____ weeks
gestation
Send specimen for microscopic pathology
Instructions
Complications:
479
Post-Operative Medication
Immune Ergotrate Other
globulin, mini
dose
Immune Birth
globulin, full-
dose
Control Pills
Pitocin Tetracycline
Notes or comments_____
Procedure Not Performed
Physician’s Signature
Referral: * *
Counselor Signature
* *
Do not sign unless you fully understand the following.
I, _______________________ being______years old,
request that my present pregnancy be terminated. I
understand that the termination of this pregnancy (i.e.
abortion) will be by vacuum aspiration and curettage as
explained to me. I understand that Dr.___________ or
a designated associated physician will be performing the
termination procedure.
I further understand and give my consent to the taking of
medical tests, cultures, and smears that are deemed
necessary.
480
I have fully and completely disclosed my medical history,
including allergies, blood conditions, prior and current
use of or reactions to medications and drugs. I
understand that a full and complete disclosure of my
medical history is important to help minimize the risks of
complications which may occur with termination of
pregnancy. I understand that the physician of Allentown
Women’s Center is relying on my disclosures as being
truthful and complete.
The first day of my last normal menstrual period
was____ 19___. I understnad that this information
concerning my last period is important to the diagnosis
and method of treatment, and that the physician’s
decision to proceed with the termination is based on the
above information as well as findings from examination.
I fully understand the purpose of the procedure is to
terminate my pregnancy. I know that I can continue the
pregnancy, but it is my choice to end it now. No one has
forced me to do so.
I consent to the administration of such local anesthesia
as may be deemed necessary or advisable by my
physician. I understand that local anesthetics do not
always eliminate all pain, that in a small number of
cases, patients can have an allergic reaction which could
result in shock or even death.
I fully understand that the practice of medicine and
surgery is not an exact science and that qualified
physicians cannot assure the results thereof. I realize
there are inherent risks of minor and major
complications which many occur in this and all surgical
procedures, without the fault of the physician. No
guarantee has been made to me. I understand that the
481
surgical procedure which I am about to undertake will in
all probability involve a certain amount of pain and loss
of blood. I also understand that the surgical procedure
which I have requested is occasionally accompanied or
followed by certain complications including, but not
limited to, perforation of the uterus (putting a hole
through the uterine muscle), hemorrage, retainded tissue
and/or infection, all of which could be severe enough to
require surgery resulting in hysterectomy (removal of the
uterus), and/or sterility (never being able to become
pregnant again). If any of the above reactions or
complication do ocurr, I further realize that I may need
to be hospitalized which would be at my own expense. I
realize that such complications can be caused by other
medical conditions and not related to the pregnancy
termination procedure, by my own failure to follow post
operative instructions, or by the treatment of the follow
up physician. I know that every effort is made to protect
my confidentiality, but that if I have a medical problem
that needs treatment, my confidentiality may be
jeopardized.
I understand that any questions I have will be answered
by my physician, nurse and/or counselor, and I will ask
any questions I have before leaving. If I have any
questions or complications after leaving, I agree to call
the Allentown Women’s Center at 215-264-5657. I
realize that immediate treatment may be necessary to
avoid more severe complications.
I understand the importance of post-operative follow-up
care and I realize that I am responsible for scheduling a
post-abortion check-up in 2-3 weeks to be certain that no
medical problem has occured, that I may be unaware of,
and to check that the procedure has been complete. I
agree to report any and all post abortion problems to the
482
Allentown Women’s Center, particularly fever, heavy
bleeding, severe cramping or pain, or the absense of a
normal period within eight weeks of the procedure.
I certify that I have read (or had read to me) and fully
understand the above consent form, regarding
termination of pregnancy, that the explanations therein
referred to were made, and that all blanks or statements
requireing insertion or completion were filled in. I
further certify that all information I have supplied, in this
entire record, is true to the best of my knowledge and
belief.
DO NOT SIGN UNTIL YOU HAVE COMPLETELY
READ AND FULLY UNDERSTAND THE ABOVE
SIGNATURE___________________________________
WITNESS_______________________________________
D A T E _________________________________________
I certify that I have explained, translated, or otherwise
informed the patient of the above.
SIGNATURE___________________________________
DATE_________________________________________
RELATIONSHIP TO THE PATIENT_______________
DRUGS DISPENSED
I request that drugs not be dispensed to me in safety
closure containers.
SIGNATURE___________________________________
WITNESS_______________________________________
DATE
CONSENT TO ORAL CONTRACEPTIVES
I have chosen to use oral contraception as a birth
control method and request the physician at Allentown
Women’s Center prescribe this method for me. I
483
understand the possible side effects to the method
include severe headaches, leg cramps, blurred vision,
blood clots, chest pain and stroke. I agree to report any
and all side effects to Allentown Women’s Center or to
my own physician or clinic. I am aware that the most
serious side effects of birth control pills can be fatal. I
have read the information sheets and fully disclosed any
risk factors in my medical history that might be
contraindications to taking oral contraceptives.
SIGNATURE
WITNESS
DATE
CONSENT FOR RELEASE OF MEDICAL RECORDS
I give permission for release of information from my
medical records from the Allentown Women’s Center to
my follow-up care provider and, if specified below, my
referral source.
Referred by
SIGNATURE
WITNESS DATE
484
Defendants’ Exhibit 35:
AWC Advertisements
DONNELLY DIRECTORY
ALLENTOWN
WOMEN’S
CENTER
ABORTION SERVICES
AWAKE OR ASLEEP
EARLY PREGNANCY TESTS
GYNECOLOGICAL CARE
VD TESTING
ALL SERVICES CONFIDENTIAL
264-5657
Rt 22 & Airport Rd. Allentown
ALLENTOWN WOMEN’S
CENTER
ABORTION SERVICES
AWAKE OR ASLEEP
EARLY PREGNANCY
TESTING
CONFIDENTIAL
COUNSELING
Rt 22 & Airport Rd Allentown
Toll Free —- 800 372-8500
485
* * *
ALLENTOWN WOMEN’S CENTER--
■ ABORTION SERVICES
■ AWAKE OR ASLEEP
■ SATURDAY HOURS
AVAILABLE
Rt 22 & Airport Rd
Allentown Toll Free — 800 372-8500
486
Defendants’ Exhibit 36:
AWC Consent Form
I, , have requested an abortion at
the Allentown Women’s Center, although I have also
stated I don’t think abortion should be legally available
to women.
I have been offered waiting time to reconsider my
decision to abort this pregnancy. I have been offered
genetic counseling, psychological counseling, and an
explanation of the resources for financial and emotional
support available to me to continue this pregnancy. I
have been asked to consider how I expect to feel after an
abortion, and urged not to take the irreversible step of
terminating my pregnancy until I have fully processed the
options before me.
I take full responsibility for my decision to terminate this
pregnancy. I acknowledge and understand that my
doctor here and the support staff are caring, responsible
people who are helping me implement my voluntary,
uncoerced request to terminate this pregnancy.
If in the future I ever publicly state that the Allentown
Women’s Center counseled me inadequately or that I
was not fully aware of the gravity of what I was doing in
terminating my pregnancy I understand that I will, by so
doing, give up all rights to confidentiality and that the
staff of the Allentown Women’s Center will defend their
non-directive counseling protocols publicly.
Signature________________________________________
D ate__________________________
Witness
4 8 7
Defendants’ Exhibit 37:
Northeast Women’s Center
Guidelines for Informed Consent
GUIDLINES FOR INFORMED CONSENT
I. Individual Counseling Session
A. Exploration of all options
B. Determination of Reason for Abortion
1. to meet qualifications for abortion control act
2. to assure that patient is sure of abortion decision
C. Review of medical history to determine medical
eligibility.
D. Distribution of follow-up & after care
instructions
E. Distribution of birth control information
F. Opertunity to explore feelings about abortion
G. Completion of State Health Dept, form
1. report of induced termination of pregnancy.
II. Group Counseling
A. Explaination of abortion procedure
B. Explaination of possible risks, and complications
C. Explaination birth control methods.
D. Explaination of written consent
E. Signing of consent form
F. Question and Answer
III. Physician Consultation
A. Determination of reasons for abortion
B. Question and answer period.
C. Abortion procedure
488
Defendants’ Exhibit 39:
Summary Compilation of Quarterly Reports
CUMULATIVE/YEARLY TOTALS: 1985 & 1986
Facilities: WHS, PPSP, WSC, AWC, RHCC
Conditions/
Indications
1985* 1986
Cardiac 59 (0.31%) 63 (0.30%)
Diabetes 27 (0.14%) 17 (0.08%)
Genetic 5 (0.03%) 5 (0.02%)
Hydatid Mole 7 (0.04%) 6 (0.03%)
Hypertension 40 (0.21%) 19 (0.09%)
Malignancy 5 (0.3%) 1 (0.005%)
Psych. 42 (0.22%) 29 (0.14%)
Radiation 11 (0.06%) 15 (0.07%)
Renal — —
Rubella — —
Incest 3 (0.016%) 23 (0.11%)
Rape 176 (0.93%) 276 (1.31%)
All Abortions 18,999 21,029
♦Includes all date except 2nd Quarter of PPSP
489
Defendants’ Exhibit 45:
Commonwealth of Pennsylvania
Department of Health (DOH)
Abortion Facility Registration Form
COMMONWEALTH OF PENNSYLVANIA
DEPARTMENT OF HEALTH
ABORTION FACILITY REGISTRATION FORM
Effective April 24, 1988, every facility at which abortions
are performed shall file this form within 30 days with the
Bureau of Quality Assurance, Pennsylvania Department
of Health, P.O. Box 90, Harrisburg, Pennsylvania 17108.
Subsequent changes should be reported immediately,
using this same form.
1. What is the name of your facility?
2. What is the mailing address of your facility
Street ________________________
Post Office ____________________
Zip Code______________________
3. In what county is your facility located?
4. Does your facility have any parent, subsidiary, or
affiliated organizations, corporations, or associations?
No ___ Yes (If yes, list names and addresses
below)
a. Name____________ b.Name______________
Address Address
5. Does your facility have any parent, subsidiary or
490
affiliated organizations, corporations or associations
which have contemporaneous commonality of
ownership, beneficial interest, directorship or
officership with any other facility? (If yes, list names
and addresses below) __ No __ Yes
a. Name________ b.Name_______
Address Address_____
6. Registration forms filed by facilities which have
received state appropriated funds during the 12
month period preceding a request to inspect or copy
such forms shall be deemed public information. Has
your facility received such funds? __ No __ Yes
7. Is this form an update of a previously submitted
Registration Form?
_No __ Yes (List items and check type of
update)
a . __________ _____ ______ _____
b . __________ __________________________
Change Add Delete
8. Date Submitted:
MO DAY YR
491
Defendants’ Exhibit 46:
DOH Abortion Quarterly Facilities
Report Form
COMMONWEALTH OF PENNSYLVANIA
Department of Health
ABORTIONS: QUARTERLY FACILITIES REPORT
Effective April 24, 1988, every facility in which an
abortion is performed within Pennsylvania during any
quarter year shall file a report with the State Health
Data Center, Pennsylvania Department of Health, P.O.
Box 90, Harrisburg, Pennsylvania 17108. Reports are
due within 30 days of the end of the quarter.
1. Reporting Period (check one):
_Jan. 1 -- Mar. 31 __ Apr. 1 -- Jun. 30
__ Jul. 1 -- Sep. 30 __ Oct. 1 -- Dec. 31
2. What is the name of your facility?
3. What is the mailing address of your facility?
Street_______________________________
Post Office__________________________
Zip Code____________________________
4. In what county is your facility located?
5. How many abortions were performed in your facility
in each trimester of pregnancy during the reporting
period?
492
First Trimester: 0-14 weeks completed from the first
day of last menstrual period _______________
Second Trimester: 15-26 weeks completed from first
day of last menstrual period _______________
Third Trimester: 27 weeks or more completed from
first day of last menstrual period ________________
TOTAL ABORTIONS PERFORMED__________
6. Did your facility receive state appropriated funds
within the 12 month period immediately preceding
filing of the report?__ NO __ YES
Date Submitted __________________________
MO DAY YR
493
Defendants’ Exhibit 47A:
DOH Report of Induced
Termination of Pregnancy Form
(version no. 1)
FORMS MUST BE SUBMITTED TO THE
PENNSYLVANIA DEPARTMENT OF HEALTH
WITHIN 15 DAYS AFTER EACH REPORTING
MONTH.
COMMONWEALTH OF PENNSYLVANIA
DEPARTMENT OF HEALTH
REPORT OF INDUCED TERMINATION
OF PREGNANCY
1. FACILITY NAME
2. COUNTY OF PREGNANCY TERMINATION
3. DATE OF PREGNANCY TERMINATION
(Month, Day, Year)
4. PATIENTS IDENTIFICATION
5. AGE LAST BIRTHDAY
6. MARRIED? __ YES __ NO
7a. RESIDENCE-STATE
7b. COUNTY______________________________
8. Of Hispanic Origin? (Specify No or Yes -- If yes,
specify Cuban, Mexican, Puerto Rican, etc .)___ NO
YES Specify:
9. RACE
__ American Indian
_Black
__ White
_Other (Specify) ____________________
494
10. EDUCATION (Specify only highest grade
completed)
Elementary/Secondary (0-12) ___________________
College (1-4 or 5 + )___________________________
11. DATE LAST NORMAL MENSES BEGAN (Month,
Day, Year) __________________________________
12. CLINICAL ESTIMATE OF GESTATION (Weeks)
13. PREVIOUS PREGNANCIES (Complete each
section)
OTHER
LIVE BIRTHS TERMINATIONS
13a Now
Living
13b Now
Dead
13c Spon
taneous
13d
Induced
Do not
include
this
termin
ation
Number
None
Number
None
Number
None
Number
None
14. TERMINATION PROCEDURES
TYPE OF TERMINATION PROCEDURES
14a. PROCEDURE THAT TERMINATED
PREGNANCY
(Check only one)
Suction Curettage
Sharp Curettage
Dilation and Evacuation (D&E)
Intra-Uterine Saline Instillation
Intra-Uterine Prostaglandin Instillation
Hysterotomy
Hysterectomy
Other (Specify)________
495
Other (Specify)________
14b. ADDITIONAL PROCEDURES USED FOR
THIS TERMINATION, IF ANY
(Check all that apply)
Suction Curettage
Sharp Curettage
Dilation and Evacuation (D&E)
Intra-Uterine Saline Instillation
Intra-Uterine Prostaglandin Instillation
Hysterotomy
Hysterectomy
Other (Specify)________
15. MEDICAL COMPLICATIONS OF PREGNANCY
_ Rubella
Hydatid Mole
Endocervical Polyp
Malignancies
Complication resulting from termination (Specify)
16. LENGTH AND WEIGHT OF THE FETUS
(Report only if termination subsequent to 19 weeks
of gestation) Length cm Weight gm
17. DID A MEDICAL EMERGENCY EXIST? (Use
back of form for explanations, if needed)
___ YES Explain basis for judgment:
___ NO Was the fetus viable prior to procedure?
(Respond only if termination subsequent
to 19 weeks of gestation)
___ YES Explain basis for determination that
the abortion is necessary, and the
reason for selected termination
procedure:
___ NO Explain basis for determination of
non-viability:
18. REFERRING PHYSICIAN, AGENCY, OR
SERVICE (If any)
NAME
496
19. ATTENDING PHYSICIAN
Name_____________________________________
Licence Number
SIGNATURE AND DATE SUBMITED
_______________________________ Mo.__Day__ Yr.
497
Defendants’ Exhibit 47B:
DOH Report of Induced
Termination of Pregnancy Form
(version no. 2)
FORMS MUST BE SUBMITTED TO THE
PENNSYLVANIA DEPARTMENT OF HEALTH
WITHIN 15 DAYS AFTER EACH REPORTING
MONTH
COMMONWEALTH OF PENNSYLVANIA
DEPARTMENT OF HEATLH
REPORT OF INDUCED TERMINATION
OF PREGNANCY
1. FACILITY NAME
2. COUNTY OF PREGNANCY TERMINATION
3. PATIENTS IDENTIFICATION (Do Not Use
Patient’s Name)
4a. RESIDENCE-STATE
4b. COUNTY
5. DATE OF PREGNANCY TERMINATION
(Month, Day, Year)
6. AGE AT LAST BIRTHDAY
7. CLINICAL ESTIMATE OF GESTATION (Weeks)
8. PREVIOUS PREGNANCIES (Complete each
section)
LIVE BIRTHS
OTHER
TERMINATIONS
498
8a Now
Living
8b Now
Dead
8c Spon
taneous
8d Induced
(Do not
include
this
termin
ation)
Number
None
Number
None
Number
None
Number
None
9. TERMINATION PROCEDURES
TYPE OF TERMINATION PROCEDURES
9a. P R O C E D U R E T H A T T E R M I N A T E D
PREGNANCY
(Check only one)
Suction Curettage
Sharp Curettage
Dilation and Evacuation (D&E)
Intra-Uterine Saline Instillation
Intra-Uterine Prostaglandin Instillation
Hysterotomy
Hysterectomy
Other (Specify)
9b. ADDITIONAL PROCEDURES USED FOR THIS
TERMINATION, IF ANY
(Check all that apply)
Suction Curettage
Sharp Curettage
Dilation and Evacuation (D&E)
Intra-Uterine Saline Instillation
Intra-Uterine Prostaglandin Instillation
Hysterotomy
Hysterectomy
Other (Specify)
10. MEDICAL COMPLICATIONS OF PREGNANCY
Rubella
499
Hydatid Mole
Endocervical Polyp
Malignancies
Other Complications Resulting From Pregnancy
(Specify)
Complication Resulting From Termination
(Specify)
11. ATTENDING PHYSICIAN
Licence Number
12. SIGNATURE AND DATE SUBMITTED
MO DAY YR
500
Defendants’ Exhibit 47C:
DOH Report of Induced
Termination of Pregnancy Form
(version no. 3)
FORMS MUST BE SUBMITTED TO THE
PENNSYLVANIA DEPARTMENT OF HEALTH
WITHIN 15 DAYS AFTER EACH REPORTING
MONTH.
COMMONWEALTH OF PENNSYLVANIA
DEPARTMENT OF HEATLH
REPORT OF INDUCED TERMINATION
OF PREGNANCY
1. FACILITY NAME
2. DATE OF PREGNANCY TERMINATION
(Month, Day, Year)
3. PATIENTS IDENTIFICATION
(Do Not Use Patient’s Name)
4. AGE LAST BIRTHDAY
5a. RESIDENCE-STATE
5b. COUNTY
6. DATE LAST NORMAL MENSES BEGAN
7.
8 .
(Month, Day, Year)
Of Hispanic Origin? (Specify No or Yes -- if yes,
specify Cuban, Mexican, Puerto Rican, etc.)
_NO YES Specify:
RACE
_American Indian
_Black
__ White
__ Other (Specify) ________________________
501
9. EDUCATION (Specify only highest grade
completed)
Elementary/Secondary (0-12) __________________
College (1-4 or 5 + ) _________________________
10. MEDICAL COMPLICATIONS
Pre-existing medical conditions which would
complicate pregnancy (Specify)
__ Complication resulting from termination
(Specify)
11. PREVIOUS PREGNANCIES (Complete each
section)
OTHER
LIVE BIRTHS TERMINATIONS
11a Now
Living
lib Now
Dead
11c Spon
taneous
lid
Induced
(Do not
include
this
termin
ation)
Number
None
Number
None
Number
None
Number
None
12. TERMINATION PROCEDURES
TYPE OF TERMINATION PROCEDURES
12a. PRO CED URE THAT TERMINATED
PREGNANCY
(Check only one)
Suction Curettage
Sharp Curettage
Dilation and Evacuation (D&E)
Intra-Uterine Saline Instillation
Intra-Uterine Prostaglandin Instillation
Hysterotomy
Hysterectomy
502
Other (Specify)________
12b. ADDITIONAL PROCEDURES USED FOR
THIS TERMINATION, IF ANY
(Check all that apply)
Suction Curettage
Sharp Curettage
Dilation and Evacuation (D&E)
Intra-Uterine Saline Instillation
Intra-Uterine Prostaglandin Instillation
Hysterotomy
Hysterectomy
Other (Specify)________
13. CLINICAL ESTIMATE OF GESTATION AT
TIME OF THE ABORTION*
(Weeks)________
DETERMINATION OF GESTATIONAL AGE
Types of inquiries/examinations/tests utilized:
Basis for diagnosis: _________________
14. DID A MEDICAL EMERGENCY EXIST?
__ NO __ YES
Explain basis for judgement below.
15. Was patient married? __ YES __ NO
IF YES, WAS NOTICE GIVEN TO THE
SPOUSE? __ YES __ NO
IF NO, CHECK REASONS FOR NO
NOTIFICATION
_ Spouse is not father of child.
Spouse, after diligent effort, could not be
located.
Pregnancy was result of a spousal sexual
assault which was reported to a law enforcement
agency.
_ Patient had reason to believe that furnishing
of notice would likely result in the infliction of
503
bodily injury by her spouse or another individual.
Medical Emergency.
16. REFERRING PHYSICIAN, AGENCY, OR
SERVICE (If any)
NAME:_____________________________________
17. ATTENDING PHYSICIAN
Name_______________________________________
Licence Number____________________________
SIGNATURE AND DATE SUBMITTED
MO DAY YR
*IF GESTATIONAL AGE IS 24 WEEKS OR
MORE, COMPLETE REVERSE OF FORM.
COMPLETE FOLLOWING ITEMS ONLY
IF GESTATIONAL AGE IS 24 WEEKS
OR MORE
18. BASIS FOR THE JU DGM ENT THAT
ABORTION WAS NECESSARY TO PREVENT
THE PATIENTS DEATH OR SUBSTANTIAL
AND IRREVERSIBLE IMPAIRMENT OF A
MAJOR BODILY FUNCTION.
19. NAME OF CONCURRING PHYSICIAN
20. NAME OF SECOND PHYSICIAN IN
ATTENDANCE_____________________
21. WEIGHT OF ABORTED FETUS
_____________ gm
504
Defendants Exhibit 48:
DOH Certification Regarding
Spousal Notice Form
COMMONWEALTH OF PENNSYLVANIA
DEPARTMENT OF HEALTH
ABORTIONS: SPOUSAL NOTICE
CERTIFICATION REGARDING SPOUSAL NOTICE
I understand that as a married woman, I am required
to notify my spouse of the fact that I am about to
undergo an abortion, prior to obtaining such abortion,
unless I am exempt from the notification requirements
due to one of the reasons set forth below. Pursuant to
this requirement, I hereby certify that:
CHECK APPROPRIATE BLANK(S)
_____ I have notified my spouse that I am about to
undergo an abortion.
_____ I have not notified my spouse that I am about to
undergo an abortion for the following reasons(s):
_____ My spouse is not the father of the child.
_____ My spouse, after diligent effort, could
not be located.
_____ The pregnancy is a result of spousal
sexual assault which has been reported
to a law enforcement agency having the
requisite jurisdiction.
505
_____ I have reason to believe that the
furnishing of notice to my spouse is
likely to result in the infliction of bodily
injury upon me by my spouse or by
another individual.
I understand that any false statement made herein is
punishable by law.
Signature/Date
NOTICE: ANY FALSE STATEMENT MADE
HEREIN IS PUNISHABLE BY LAW.
506
Defendants’ Exhibit 49:
Excerpts from DOH Directory of
Social Service Organizations for
Referrals for Pregnant Women
COMMONWEALTH OF PENNSYLVANIA
DEPARTMENT OF HEALTH
DIRECTORY OF SOCIAL SERVICES
ORGANIZATIONS
JULY, 1990
The agencies listed provide a variety of services which
may assist a woman through pregnancy, upon childbirth,
and while the child is dependent. Private physicians,
clinics, and hospitals may also offer these services.
Examples of services which may be provided directly, or
by referral, include but are not limited to counseling,
pregnancy testing, medical care, legal and financial
assistance, transportation, childbirth instruction, housing,
job placement, continuing education and adoption
information. Where the agency offers primarily a
specialized service, it has been noted. "Special Services"
have been numerically coded according to the following
index:
507
01- Abuse (Drugs, Domestic, Child)
02- Adoption
03- Book Resources on Childbirth (Childbirth
Instruction)
04- Clothing
05- Counseling (Job, General, Psychological, Prenatal,
Family)
06- Emergency Assistance
07- Food
08- Food Stamps
09- Fuel
10- Furniture
11- Hot Line Services
12- Interpreting Services
13- Job Training/Placement
14- Legal Referral
15- Nutrition
16- Information & Referral
17- Schooling/Education
18- Shelter/Housing
19- Short-term Crisis Intervention
20- Teens
21- Telephone Referral
22- Transportation
23- WIC (Women, Infants and Children)
Nutrition Program
24- Foster Care
25- Financial Assistance
26- Medical Care/Testing
27- Family Planning
28- Day Care
* * *
508
Defendants’ Exhibit 50:
Excerpts from DOH Printed Information
on Medical Assistance Benefits
COMMONWEALTH OF PENNSYLVANIA
DEPARTMENT OF HEALTH
MEDICAL ASSISTANCE BENEFITS FOR
PRENATAL CARE, CHILDBIRTH
AND NEONATAL CARE
JULY, 1990
You may or may not qualify for medical assistance
benefits, depending on your income. For persons who
qualify, the Medical Assistance Program will pay for
doctor, clinic, hospital, and other related medical
expenses so you can receive prenatal care, delivery
services, and care for your newborn baby. You can apply
for Medical Assistance benefits at your local County
Assistance Office.
Under the Healthy Beginnings Program you may be
eligible for Medical Assistance because you are pregnant.
A pregnant woman is allowed to have more income to
qualify for this benefit and may receive prenatal care
from certain providers while the formal application for
assistance is being processed.
Your County Assistance Office can tell you which
providers participate in the Medical Assistance Program
and can answer your questions about other available
509
benefits. County Assistance Offices are listed for your
information. The attached pamphlets on Medical
Assistance and Healthy Beginnings also may be of
assistance to you.
If you are pregnant or have children three years old
or younger, Healthy Beginnings could provide you free
health care for yourself and your children.
In October 1989, this program will be expanded to
include children up to four years old.
If you or your family’s income is less than or equal
to the chart on the back of this card, you should call,
toll-free 1-800-842-2020, or contact your local county
assistance office.
* * *
FAMILY
SIZE
MONTHLY
INCOME GUIDE
one person
two persons
$ 498
(or a pregnant woman)
three persons
four persons
five persons
six persons
$ 668
$ 838
$1,008
$1,178
$1,348
510
If your income is close to these figures, call 1-800-
842-2020. We may still be able to help you.
Healthy Beginnings covers all your health care needs
including prescriptions, dental care, physician, delivery
and other necessary hospital costs.
If you think you quality for Healthy Beginnings, call
1-800-842-2020, today!
* * *
FACTS
MEDICAL
ASSISTANCE
CAN
HELP
THIS BROCHURE CONTAINS SOME BASIC
INFORMATIO N ABOUT MEDICAL
ASSISTANCE. PLEASE READ IT
CAREFULLY, IT WILL TELL YOU WHAT
TO BRING WITH YOU WHEN YOU APPLY.
511
Commonwealth of Pennsylvania
ROBERT P. CASEY
GOVERNOR
Department of Public Welfare
JOHN F. WHITE, JR.
SECRETARY
OFFICE OF MEDICAL ASSISTANCE
REMEMBER -
MEDICAL ASSISTANCE
CAN HELP!
The Medical Assistance program is designed to help
you pay doctor, hospital, and other medical-related
expenses so you and your family can receive continuing
medical and dental care when your medical and dental
costs are higher than you can afford.
This brochure contains some basic information about
Medical Assistance. Please read it carefully. It will tell
you what to bring with you when you apply.
If you do have any questions, please call your local
county assistance office. They want to help.
Note: Some counties may be using health
maintenance organizations (HMOs) or health insuring
organizations (HIOs) in addition or in place of the
regular Medical .Assistance Program. If you live in one
of these counties, your local county assistance office will
be able to explain these other programs to you.
512
Facts About Medical Assistance
■ You can apply for Medical Assistance in the county
where you live in Pennsylvania.
■ You can work, and still may be able to get Medical
Assistance.
■ You can own a house and have a car and still get
Medical Assistance.
■ You don’t have to get a welfare check to get Medical
Assistance.
■ You don’t have to live with children to get Medical
Assistance.
■ You can be getting social security, unemployment or
some other kind of income and still may be eligible
for Medical Assistance.
Persons who are eligible for Medical may be eligible
for some services under Medical Assistance which
medicare does not cover. However, Medical Assistance
does not automatically pay the difference between a
medical provider’s charge and the Medicare payment.
How Does Medical Assistance Work?
If you are eligible for Medical Assistance, you may
go to a doctor, hospital, or other health-care provider for
medical services. If the health-care provider participates
in the Medical Assistance Program, and if you have no
other medical insurance which will cover the medical
service, the State will pay for the medical service.
Some services require prior authorization by the
state Office of Medical Assistance. A brochure entitled
Prior Authorization of Medical/Dental Services explains
this.
Please note that payments are made to the provider
not to the patient.
You may be asked to pay a small amount to the
provider for the service. This is called a co-pay. Ask
513
your county assistance officer for the brochure What is
Co-Pay?, which explains how co-pay works.
Out-of-State Services
The Department will pay for medical services
furnished to you while out of of state if:
■ You require emergency medical care while
temporarily away from your home.
■ You would be risking your health if you wait for the
service until you returned home
■ You live in a state border area and recipients in your
area regularly use medical resources in a neighboring
state.
■ The Department decides, based upon the medical
provider’s advice, that you have better access to the
type of medical service you need in another state.
Who Can Receive Medical Assistance?
There are three categories of Medical Assistance.
You may be eligible for one of them:
1) Categorically Needy: This is for persons who are
eligible for cash assistance, or for people who receive
Supplemental Security Income (SSI). These persons
receive a blue Medical Assistance card.
2) Medically Needy Only: Ths is for persons who are
not eligible for cash assistance or SSI but whose
income is not enough to cover their medical
expenses. These persons receive a green Medical
Assistance care.
3) State Blind Pension: This is for persons who are
eligible for and receive a check from the State Blind
Pension Program. These persons receive a pink
514
Medical Assistance card.
Ask your county assistance office for Services
Covered by the Medical Assistance Card. This shows the
benefits covered by each of the three Medical Assistance
categories.
How Do I Apply for Medical Assistance?
You must file an application with you local county
assistance office. You may pick up your application at
the local county assistance office or phone the office and
have one mailed to you.
If you are unable to apply for yourself, a relative,
friend, hospital representative or other person may apply
in your behalf.
When you return the application to your county
assistance office, a worker will look over your application
with you to make sure you have completed all items.
The worker will help you complete the application if you
need help. If there is some information you are not able
to get, your county assistance office can help you to get
this information.
When you apply for Medical Assistance, you will
need to provide information about yourself and your
family to help the county assistance office decide what
kind of help you can receive. It you don’t have it on
hand, apply anyway.
You will need:
■ Birth certificates and other forms of identification
for yourself and other family members in your home,
such as a driver’s license or school or work
identification.
■ Your social security card and social security cards for
other persons in the home for whom you are
applying (your worker can help you apply for these if
515
you do not have them).
■ Letters or forms that show how much money you and
other family members living in the home get from
social security, Supplemental Security Income (SSI),
Veteran’s pensions, unemployment compensation,
worker’s compensation, retirement or other kinds of
income.
■ Wage stubs (if you are working) and wage stubs for
other family members living in the home who are
working.
■ Health and medical insurance policies and bank
books, savings books and any other records to show
how much money you and other family members
living in the home have available.
■ Life insurance policies.
Your worker can tell you what additional
information you will need to be eligible for Medical
Assistance and help you to get this information.
After your worker determines that you are eligible
for Medical Assistance, you will receive a Medical
Assistance Card which is good through the date shown
on the card. You will receive a new card before the old
one expires. If you card is lost, stolen or destroyed, tell
your county assistance office immediately. They will
replace it so you don’t have to miss any medical
appointments.
As a recipient, you have certain rights and
responsibilities. A pamphlet titled Your Rights and
Responsibilities in Public Assistance Programs describes
them.
How Do I Find a Medical Provider Who Will Accept the
Medical Assistance Card as Payment?
First, check with your present doctor, dentist or
516
other medical provider to see if the Medical Assistance
card will be accepted. If not, you may want to ask
someone you know who receives Medical Assistance for
the name of a doctor or dentist.
If you cannot find a doctor or dentist who accepts
the Medical Assistance card, contact your caseworker at
the local county assistance office, who will help you
locate a medical provider who accepts the card.
What If I Don’t Agree With the Decision of the County
Assistance Office?
If the county assistance office determines that you
are not eligible for the Medical Assistance Program, you
will receive a notice from your county assistance office.
You have the right to appeal the decision and request a
fair hearing. If you are already receiving medical
assistance and if you appeal within 10 days from the date
of the notice, your Medical Assistance coverage will
continue pending the outcome of the fair hearing.
Your county assistance office is there to help you.
You should call them with questions you may have about
Medical Assistance eligibility or coverage.
The Mission o f the Department o f Public Welfare
is to:
Promote, improve and sustain the quality of family
life,
Break the cycle of dependency,
Promote respect for employees
Protect and serve Pennsylvania’s most vulnerable
citizens, and
517
Manage our resources effectively.
518
Defendants’ Exhibit 51:
DOH Notices Required by
Abortion Control Act
COMMONWEALTH OF PENNSYLVANIA
DEPARTMENT OF HEALTH
NOTICES REQUIRED BY
ABORTION CONTROL ACT
JULY, 1990
1. It is generally unlawful for any individual to coerce a
woman to undergo abortion.
2. Any physician who performs an abortion upon a
woman without according her a private medical
consultation may be liable to her for damages in a
civil action at law.
3. The father of a child is liable to assist in the support
of that child, even in instances where the father has
offered to pay for an abortion. The availability of
support payments will depend, in part, on the
father’s income. You may wish to consult with a
lawyer regarding the availability of support payments.
4. The law permits adoptive parents to pay costs of
prenatal care, childbirth and neonatal care.
519
Defendants’ Exhibit 54:
Deposition Excerpts of
Thomas E. Allen, M.D.
BY MS. MERSHIMER:
* * *
[9] Q. While you’ve been at Magee, have you
performed any abortions because there was a medical
emergency?
A. No.
Q. How about at WHS?
A. Not -- no.
* * *
[13] Q. All right. Now, Exhibit B attached to
Defendants’ Exhibit 1 is Magee’s informed consent form?
A. Informed consent, correct.
Q. And this, you make sure every patient signs?
A. Reads this and signs it, or has it read to her if
she can’t understand it.
Q. Now, in cases of a minor, do you have the
parent sign it, also?
A. It’s required by Magee. There’s no question
about it. You can’t do an abortion there without having
the parent’s consent.
Q. Does Magee require a parent’s consent of a non
abortion surgical procedure, also?
A. Yes. Everything except delivery of term - or a
delivery.
* * *
[28] Q. Now, Interrogatory 15, I had asked you
520
about the allegations in the Complaint that the Act
unduly restricts a woman’s access to counseling, and you
refer to various verifications in your Answer?
A. I think that was my attorney’s --
MR. ZEMAITIS: Yes. I don’t think there’s any
obligation under the Federal Rules of Civil Procedure or
otherwise that every plaintiff be able to state from his or
her own personal knowledge facts that support a
particular allegation of the Complaint.
MS. MERSHIMER: I’m not saying that there is.
[29] A. Yes.
Q. My question to you is: Do you have any
knowledge upon that aspect of the Complaint, that
allegation?
A. No, I do not.
* * *
[71] Q. Have you ever performed an abortion on
anyone without having their informed consent?
A. No.
Q. So that would include both adults and minors?
A. Right.
* * *
[78] Q. Excluding abortion, would you ever perform
a surgical procedure on somebody without their informed
consent?
A. No.
Q. And, again excluding abortion, would you ever
perform a surgical procedure on a minor without the
consent of a parent?
A. No. Probably not. I can’t think of -- except an
emancipated minor who is not considered to be a minor.
A woman who -- a teenager who has a child is not
521
considered a minor for any operative procedure, except
as defined by this Act.
Q. Okay. Let’s just clarify the question, then.
Again excluding abortion, would you ever perform a
surgical procedure on an unemancipated minor without
the consent of the parent?
A. No. But by my definition, a person who is
pregnant is emancipated to some degree.
Q. That’s your personal definition.
[79] A. That’s my personal definition, yes.
* * *
522
Defendants’ Exhibit 55:
Deposition Excerpts of Sue Roselle
* * *
[7] Q. In Paragraph 2 of your verification, you [8]
talked about the staff you’re responsible for, and you
mentioned 13 physicians.
A. Yes.
Q. Is that still the same number of physicians
currently being used by WHS?
A. I believe we have 12 physicians currently.
Q. And Dr. Allen this morning said that all the
physicians are part-time.
A. That’s correct.
Q. Is there any approximate hours that they work?
A. There is one physician who works approximately
20 hours a week, and then everyone else is what we call
as-needed, which is when we schedule them.
Q. And you perform abortions at WHS three days a
week?
A. That’s correct.
Q. For the most part, counseling occurs the same
day as the abortion service --
A. That’s correct.
Q. - is provided? It’s more difficult for her to take
us down when I’m still asking a question [9] and you
answer. I understand how it is. I have the same habit.
Also, the record reads a little easier.
What, it’s like 95 percent of all the counseling occurs
on the same day the abortion services are provided?
A. Approximately 95 percent.
* * *
Q. In Paragraph 6, which would be on Page 3, it
523
lists the prices of the abortion procedure costs depending
upon how late the pregnancy we’re talking about?
A. That’s correct.
Q. Have those prices changed since you initially
filled out this verification?
A. Yes, they have.
[10] Q. Could you tell me what the new prices are?
A. $295 if 12 weeks or less; $395 if 13 to 14 weeks;
$600 if 15 to 16 weeks; and $625 if 17 weeks.
Q. And no abortions after 17 weeks gestation —
A. That’s correct.
Q. -- are performed at WHS; is that correct?
A. That’s correct.
Q. Is there any particular reason why the prices
went up, anything you can attribute it to?
MR. ZEMATHS: You mean other than general
economic trends?
MS. MERSHIMER: Right.
Q. Other than like labor costs went up or -
A. No.
[17] Q...........WHS still encourages minors to bring a
parent or another adult with them?
A. That is correct.
Q. Is your preference to have a parent?
A. That’s correct.
Q. Is there a reason why you like the parent to
attend with a minor?
A. To encourage family communications.
Q. If a minor calls up, when she first telephones, is
that when it’s encouraged, the minor is encouraged to
bring her parent along?
A. Yes.
524
* * *
[20] Q. And the paraprofessional counselors, there’s
no education requirement to be a paraprofessional
counselor?
A. That’s correct.
* * *
Q. And what’s covered during this counseling
interview is a discussion about her options, her decision
to have an abortion, make sure she’s not unduly
ambivalent about what she’s doing and make sure she’s
not being coerced to have an abortion and [21] to talk
about future contraceptive use. Is that pretty much it?
A. That’s it.
Q. This next line talks about if a patient appears
ambivalent about her decision and the abortion is
rescheduled to give her more time to consider her
options.
A. That’s correct.
Q. And then the personal counselor is what? It’s a
more intense discussion, or what?
A. The personal counselor is prepared to at least
masters degree level and has five years post masters
experience in therapy, and it focuses on the pregnancy as
a problem in relationship to the rest of the factors in her
life.
* * *
[22] Q. When a parent does attend, does both the
minor and the parent sign the informed consent form?
525
A. That’s correct.
* * *
[43] Q. In Paragraph 35, you discuss your concern
about putting the identity of the referring [44]
performing physicians in a report to the Department of
Health, and then you state, "I can state with complete
certainty that because of the harassment and violence
directed toward physicians who refer or perform abortion
procedures, WHS will lose many of its referring
physicians and possibly some of its performing physicians
if this section goes into effect." Now, focusing on
performing physicians, that information is being provided
on the reports currently.
A. That’s correct.
Q. And have you lost any performing physicians for
that reason?
A. We have lost a couple of physicians. They have
not given that reason for them leaving. The rest of the
physicians have continued to express a lot of concern
about that information becoming available to the public.
[79] Q. I take it from your response to Interrogatory
No. 24 on Page 18 that WHS advertises in some local
newspapers in the Pittsburgh area, on radio stations, and
some college newspapers and also in the phone book?
A. That’s correct.
* * *
[80] Q. I’m looking at Interrogatory No. 2 on Page 3
focusing on WHS’ Answer. Remember you said you
weren’t sure of the percentages of minors that are
526
accompanied by an adult? Does that refresh your
recollection, 75 percent of the minors are accompanied
by an adult?
A. Yes.
Q. And that on the next page, that 50 percent of
the minors are accompanied by one or both of their
parents?
A. That’s correct.
Q. Now, when a minor is accompanied by an adult,
not necessarily their parent, does that adult participate or
is involved at all in any part of the counseling or
informed consent aspect?
[81] A. No.
Q. But if the minor is accompanied by one of the
parents, then the parent is involved in part of that
counseling session, and particularly as to informed
consent?
A. That’s correct.
* * *
[84] Q. When I asked you if any of the physicians
that had left WHS was because their identity, performing
physician’s identity was listed on the reports to the
Department of Health, you said that wasn’t the reason
they gave you?
A. That is not the reason they gave me.
Q. Did any of the reasons they gave you have [85]
to do with any of the requirements of Pennsylvania law?
A. No.
* * *
527
Defendants’ Exhibit 56:
Deposition Excerpts of Carol C. Wall
BY MS. MERSHIMER:
* * *
[10] Q. And abortions at the Center City Clinic still
occur on Wednesdays, Thursdays, Fridays, and [11]
Saturdays?
A. Yes.
Q. And what are the general hours of the clinic then?
A. They are regular medical clinic hours. Abortions
would be performed approximately four to five hours
each of those days.
* *
[12] Q. Now, the cost that you stated in your
Verification of an abortion in the first trimester if they
were not on Medical Assistance was $225.
Does that still remain the price?
A. No.
The price now is $240.
Q. Is there any specific reason why the price has gone
up?
A. Yes.
The costs have gone up.
Q. What?
A. The costs of salaries and non-salary costs have gone
up.
Q. Supplies and things like that?
[13] A. Yes
Q. And I see here that the fees cover the direct cost of
the procedure, including counseling, medical testing, and
examination, and abortion procedure, medical
528
supervision during the post-surgical recovery, and
post-abortion examination?
A. That’s correct.
* * *
[14] Q. When you said the direct cost, which is now
$240, covers these various procedures, do you know how
much of that charge covers the cost providing personal
counseling?
A. No.
The salaried costs are broken down at some point
when we are figuring what we have to [15] charge in
order to cover our costs, but I don’t know exactly how
much the counseling part of it would be.
* * *
[16] Q. At Planned Parenthood are any abortions [17]
performed because there is a medical emergency?
A. I would say no.
Could you be more specific on what medical
emergency means to you?
Q. Well, there are two definitions of medical emergency
that have been used in this lawsuit. One is the medical
emergency definition that is contained in the Act.
A. Yes.
Q. And then the other definition of medical emergency
is that which was provided by the Plaintiffs in response
to Interrogatories, which give me a second and I will find
it here. It was in response to Interrogatory NO. 18
where the Plaintiff said, "A medical emergency occurs
whenever, in the judgement of the attending physician, a
combination of circumstances presented requires
immediate medical attention to protect the life or the
health of the patient."
529
A. Yes; then my answer is definitly no as I said before.
Q. No as to either definition?
A. Yes.
[18] Q. Now, Planned Parenthood encourages minors to
involve their parents in the decision to have an abortion;
correct?
A. Yes.
Q. Do you encourage a minor to bring the parent along
to the procedure if the parent is agreeable?
A. Yes.
Q. Why does Planned Parenthood do that?
A. Our experience is that very young women need to
have the help and support of their family members and
want it.
Q. If a parent does attend with the minor, does the
parent also sign the Informed Consent Form?
A. No.
* * *
[20] Q. So you contract with the physicians?
A. Yes.
Q. How many physicians do you contract with?
[21] A. At this time three to four different physicians.
* * *
[24] Q. The counselors for Planned Parenthood, is there
any minimum education requirement?
A. No.
Q. Are there any sort of certificates or degrees that they
have to have?
A. No.
530
Q. But they must attend the training program at
Planned Parenthood?
A. Yes.
Q. Could you tell me about the training program?
A. The training program is mainly in-service at the
beginning of the time that they start working with us, and
it is carried out by the clinical staff, the management of
the clinical [25] staff.
Q. Is there any length of time that this in-service
training occurs?
A. I don’t know. It varies with the individuals and their
backgrounds. I do know that.
We do have some people who have Master’s degrees
in counseling and some have Bachelor’s degrees who
have had a major in a field that’s related. And we have
some people who have not had that kind of formal
training.
Q. You had said that the number of counselors you
have varies on how many procedures are being
performed?
A. Yes.
Q. You mean how many counselors you have coming in
on any given day?
A. That’s correct.
Q. How many counselors do you have as a pool to use?
A. I don’t know.
Q. Is it more than ten?
A. No.
I would say fewer probably.
[26] Q. And they are all paid or are there any
volunteers?
A. There are some volunteers, yes.
Q. The ones that are paid, what is their salary?
A. I don’t remember.
Q. Well, do you know the starting salary?
A. No.
531
It would be around $15,000, $16,000 a year
annualized, but I’m not sure.
* * *
[66] Item NO. 3 that states "all counseling is confidential
(within legal limitations) and will be conducted in
privacy."
MR. CIPOLLA: Where is this?
BY MS. MERSHIMER:
Q. I’m sorry, the second page of Exhibit-A.
A. Okay, thank you. You want to know - what is your
question?
Q. I just wanted to see, first of all, if you found that
statement.
A. Yes, I have it.
Q. What are the legal limitations? I just didn’t know
that there were any ones that affect counseling. What is
meant by that?
A. The one that I recall is that in the cases — in a case
of, I believe, it’s rape or incest of a minor, our facility
just, as any other helping facility, is required by law to
report that to the municipality in which our facility is
located. That is one.
* * *
[71] Q. There is a section on the bottom of this form
requiring physicians to sign for minors under the age of
18 without parental consent; is that correct?
A. Yes.
* * *
532
Defendants’ Exhibit 57:
Deposition Excerpts of Sherley Hollos
BY KATE MERSHIMER:
* * *
[4] A. I’m the Executive Director of Women’s
Suburban Clinic.
Q. Could you tell me what your job duties include as
Executive Director?
A. Well, I am responsible to the Board of Directors.
We are a 501C3, so all my department heads report to
me and I’m responsible for the overall management of
the clinic.
* * *
[7] Q. Now, abortions are performed at Women’s
Suburban Clinic on Tuesdays, Wednesdays, Thursdays
during afternoon and early evening hours?
A. That’s correct.
Q. And that is still the current situation?
A. Yes.
Q. Would you have any problem, as I ask you questions,
if I refer to Women’s Suburban Clinic as WSC?
A. No problem.
Q. Is there any other sort of shorthand form you use?
A. That’s what we always call it, WSC.
Q. Now, how many physicians are there at WSC?
A. There are two physicians that practice at WSC.
[8] Q. And do they both work those Tuesday,
Wednesday, and Thursday hours?
A. There is one physician present each day.
* * *
533
[11] Q. Now, the nurse practitioners, the RNs and the
LPNs, do they do any counseling?
A. Not exactly, but a nurse by definition deals with the
whole person. It’s a matter of definition of what you call
counseling.
Q. Well, is it fair to say that what you are talking about
with the nurses, if they are going through the procedure,
whenever there are questions presented by the patients,
they are going to take the time to answer those
questions?
A. Certainly, but a nurse is not a counselor in that they
do the formal counseling prior to the procedure.
* * *
[12] Q. And the fee was $225 at the time of the
Verification.
Is that still the same?
A. It’s $245 now.
Q. Is there any particular reason why that fee rose?
A. Inflation.
Q. Basic cost of salary increase and supplies, thing like
that?
A. Yes.
And extra papers that we have to deal with.
Q. The extra papers being the reporting forms of the
State, the Department of Health?
[13] A. Yes.
Q. Do you know how much of that $20 increase is due
to the extra reporting provisions versus just the standard
cost of salaries going up?
A. No, I don’t.
* * *
[19] Q. Now, minors are all encouraged to come in for
534
precounseling; is that correct?
A. That’s correct; if they are not coming with their
parent.
Q. And WSC encourages the parents to come; is that
correct?
A. Yes.
Q. Why is that?
A. Because it’s important for any woman having an
abortion to have a support system beyond the clinic.
And for a minor the obvious support system is the
parent.
* * *
[20] Q. Now, is that the form, the Certification by
Patient, that any patient must sign prior to having an --
A. Every patient must sign.
Q. That is to have an abortion?
A. Yes.
Q. And this is the form where they acknowledge that
they were told about the risks of [21] the abortion and
alternatives to abortion?
A. Yes.
Q. Now, if a minor has an abortion, that minor has to
sign that form?
A. I believe so. I am not a counselor. I know that you
have to sign the next form, the Parental Involvement
Form.
Q. If the parent comes with their minor to the clinic, do
they have to sign any forms?
A. Yes; then they sign the Parental Involvement Form
to the "or," "I am the parent and guardian and I am
aware of her decision to abort."
Q. Is this the way it works with the minor; if the minor
comes alone and doesn’t want to involve their parents,
they sign this first paragraph of the Parental Involvement
535
Form?
A. Yes.
Q. And if the parent or guardian does come with the
minor, then that parent or guardian must sign the second
paragraph of the Parental Involvement Form?
A. That’s correct.
Q. And then if the parent or guardian does know about
the abortion but was unable to attend, [22] then, again,
the minor would sign the last paragraph?
A. Correct.
Q. And then there is a third form called Physician’s
Certification?
A. Yes.
Q. All doctors have to sign that form?
A. Yes.
Q. Is that in the case of any patient or just minors?
A. Any patient.
Q. And are there any times where a physician refuses to
sign this form?
A. Not to my knowledge.
* * *
[30] Q . . . . When we initially got onto the exhibit, we
were talking about minors coming in for precounseling
prior to the abortion appointment?
A. Yes.
Q. Do most minors do that, come in for the
precounseling session?
A. Most - I don’t know statistically how many do, but
that’s a question that is always asked.
Q. It says here that the minors are asked to come in for
precounseling, but it is not a requirement; is that
correct?
A. All minors who have not informed a parent come in
for precounseling.
536
Q. So they must come in for precounseling?
A. Yes; unless there are very extenuating circumstances.
[31] Q. Do such minors that come in for precounseling
because they have not informed a parent, do they ever
change their mind and then bring their parent to the
abortion --
A. Yes.
Q. Do you know how much of a period of time there is
between the precounseling session and the abortion
appointment?
A. It depends. It could be anywhere from the night
before to more time.
Q. A week or two weeks?
A. It would be dependent on their LMP date. How
much, you know, how much time there is.
Q. So if they are in their thirteeth week of LMP, if they
are going to have the abortion performed at WSC, there
is not much time to wait?
A. That would be a good example.
* * *
[33] A............. The only thing that isn’t explicit - is
explicitly discussed is the alternative to having an
abortion, but you can see that that happens because in
the Disclosure of Risk Benefits and Alternatives it is
gone over orally. And they are given that piece of paper,
the Consent Form, before they see the counselor and
asked to read it but not to sign it so that they have time
to read it before sitting down in the counseling session.
* * *
[40] Q. And is it still Women’s Suburban’s estimate that
if the Parental Consent Provision goes into effect it
would require at least additional three-quarter time
537
counseling positions at a cost of about $15,000 per year?
A. I think that is accurate.
* * *
[44] Q. Now, that part of the law that requires the
performing physician’s identity to be submitted to the
Department of Health, since that has gone into effect
have you known of any doctors who perform abortions
that have stopped performing abortions because their
identity is on that form?
A. I don’t know of any personally.
538
Defendants’ Exhibit 58:
Deposition Excerpts of Jane S. Green
BY MS. MERSHIMER:
* * *
[8] Q. First trimester abortions, the price listed in, I
think it is an April ’88 Verification, list the price as two
hundred and ten dollars, is that still the price?
A. It remains the same.
* * *
Q. How about for early second trimester abortions; is it
still three sixty-five?
A. That’s correct.
* * *
[12] Q. Are abortions still performed on Wednesday and
Friday afternoons and Saturday mornings?
A. On Saturday mornings, not at this point; Wednesday
and Friday and Tuesday.
Q. Tuesday, all day Tuesday?
A. Tuesday afternoon.
Q. Is Wednesday just Wednesday afternoon or all day
Wednesday?
A. Wednesday evening. So that is wrong. That says
Wednesday from ten to three, so it is Wednesday
evening.
* *
[20] Q. Now, paragraph eleven of your Verification,
539
approximately in the middle, there is a discussion, "If the
woman already has had a postive test when she calls
RHCC and wants to terminate her pregnancy, an
abortion appointment can be scheduled usually within
one week’s time."
Is that still correct information?
A. That is correct information.
Q. Does it ever take more than a week to schedule the
abortion appointment?
A. Sometimes. It depends upon her medical history.
There are certain questions that telephone counselors
ask, in terms of medical history. And if the woman
needs to obtain a physician’s note, then it could take
longer.
* * *
[23] Q. Now, RHCC encourages parental involvement in
the abortion decision; is that correct?
A. What do you mean, in terms of that?
Q. I was just reading paragraph eighteen, it says, "In
general, RHCC supports and encourages parental
involvement in the abortion decision where possible."
A. That’s correct.
[24] Q. Why is that?
A. Well, we feel that it is important because when the
minor goes back into her home, that the parent will have
a better understanding perhaps of what the minor is
going through. Unfortunately, that is not always the
case. But that is primarily the reason why we would
want that support from the parent. We only can give
short term relationship counseling and we can’t go back
with that person.
Q. Just to go back for a minute, you said that the
parent, when he or she accompanies a minor does not
attend the group session that goes over the risks and the
540
informed consent provision.
A. That’s correct.
Q. So is the parent ever advised?
A. That’s why we have the waiting room counselling,
that’s then when the waiting room counselor would do
that with the parents.
Q. The waiting room counselor would advise the
parents of possible complications?
A. That’s correct.
* * *
541
Defendants’ Exhibit 59:
Deposition Excerpts of Sylvia Stengle
BY MS. MERSHIMER:
* * *
[6] Q. You are the executive director of Allentown
Women’s Center?
A. Yes.
Q. Do you have any problem if I refer to Allentown
Women’s Center in this deposition as AWC?
A. That sounds fine.
Q. As director, you are responsible for the overall
operation of the clinic?
A. That’s correct.
* *
[11] Q.............The items on this two page document
Counselling Checklist are the items covered during an
abortion counselling session; is that correct? Please,
review it.
Q. Yes, this is accurate.
* * *
[16] Q. - you said that pregnancy testing and counselling
was available at AWC Monday through Saturday,with
abortions being performed three to five days a week,
depending upon patient needs?
A. Uh-huh.
Q. Is that information still correct?
A. Yes.
Q. And then it says, "An appointment usually can be
542
scheduled in approximately one week’s time."
A. Yes.
Q. Is there any variation, does it ever take longer or
shorter?
A. Yes.
Q. Do you ever know how long it takes?
A. Well, if we have more appointments than we have
available slots, we attempt to add a day so we do not
need to ask patients to wait.
Sometimes if we have more appointments than we
have available slots, we get backed up and patients need
to wait more than a week, depending upon physician
availability, we either can or cannot solve that lag. If
that is how it goes.
* * *
[46] Q. Exhibit "B" we discussed earlier and that is the
counselling checklist, two page document.
[47] At the bottom of the page there is a section
concerning minors and the first statement under that
says, explain if complications develop their confidentiality
may be broken. When or why would that occur?
A. If a patient requires a hospital transfer or a visit to a
hospital, it might be that that care provider would not
honor her confidentiality or it might be that the
circumstances are such that her confidentiality is
violated. For example, if a minor would have a gush of
heavy bleeding, which sometimes happens even if there is
no complication, and it were in the middle of the night,
it might be very appropriate for her to involve her
parents and the confidentiality might then be broken.
We have no control over that.
We want our minors to understand as we provide the
service to them, that their health and care is more
important than their privacies around the abortion,
543
because that makes the overall experience safer for the
minor if she has that frame of reference.
* * *
[49] Q. The fourth statement says, "If a parent is here,
the parent must co-sign consent for abortion."
A. That’s correct.
* *
Q. Exhibit "C" is an eight page patient record; is that
correct?
A. Yes.
[50] Q. And then in the middle of that are questions
about pregnancy and history, live births, still births,
miscarriages, abortions and complications of pregnancies;
do you know why that information is gathered?
A. That information is gathered because it helps us both
as we provide surgery to that patient and as we counsel
that patient around her decision. The complications of
pregnancy is largely important medically.
* * *
[51] Q. When I was reviewing the Interrogatories and I
saw that a parent must sign the consent form;if a parent
comes with a minor, is there a specific space on this on
this paper where they sign or some separate form that
they sign?
A. They sign where it says, "Witness." There is not a
line that says,parent. There in not a provision in the
form for a line that says parent at this time.
544
* * *
[58] Q. Is it correct, is the newspaper article correct in
stating under the policy, if a woman -- I am sorry. The
policy forces women who seek abortions, but say they
think abortion should be illegal to delay the procedure?
A. That’s correct.
Q. Could you explain this policy to me?
A. Yes. We do not have a set of questions that we ask
patients about their views on whether or not abortion
should be legel. There is no quiz or sequence of
information seeking. However, some patients volunteer
to us that they believe that abortion in wrong, is murder
or should be illegal or [59] some combination of those
attitude sets. Those patients who volunteer to us that
abortion should be illegal and should not be available to
women, we suggest to those patients that perhaps they
should continue their pregnancy or consider that as a
very serious option. And we consider that to be a red
flag. That indicates that they might have difficulty with
the decision later.
And that it is important that they process their
decision making very carefully before they take the
irreversible action of terminating their pregnancy, which
sometimes women who are opposed to abortion want to
quote "just get this over with." Those patients we suggest
that they come back on another day and we explain to
them all of their options.
And we further explain to them that they must take
responsibility for their own decision making, that they
cannot suggest that we as providers are responsible for
the fact that they are having an abortion. And we ask
them to sign a consent form that indicates that they have
had full options counselling and that they take
responsibility for their own decision making.
[60] And that it has a concluding paragraph that says
545
if they would ever allege that they had not been
counselled properly when they had an abortion at the
Allentown Women’s Center and their options had not
been fully explained to them, that we would indeed
defend what we had done and open our records so that
could be shown.
MS. MERSHIMER: Could I got a copy of this
form?
MR. ZEMAITIS: We will take it under advisement.
BY MS. MERSHIMER:
Q. The newspaper article implied that a woman that
would reflect that abortion was wrong, murder, illegal,
either had to say she had changed her abortion belief or
that she had signed this consent form; is the newspaper
article summarizing that accurately?
A. No.
Q. If a woman who initially says that she feels abortion
is wrong or illegal, and you advise her to think it over
some more, and if she does and she returns to AWC,
must she sign this additional form that you just said no
matter what?
A. There are several points here you are addressing,
[61] so I cannot answer your question as phrased.
Q. Why don’t you explain the subtle points?
A. Approximately, fifteen per cent of our patients, we
become aware that they think abortion is wrong. Those
patients are not required to delay their procedure, except
in certain instances. For instance, if they exhibit extreme
ambivalence about the decision or if they are extremely
distraught.
If in the best judgment of the counselor and the
clinic supervisor, they had not adequately processed their
decision making, we suggest to them that they take some
time and come back another day.
Often they agree with us; infrequently, we turn them
away.
546
Your question also included if a patient thinks
abortion is illegal; if a patient thinks abortion is illegal,
we share information with her about its legality, we give
her accurate information. That slender number of
patients who want to affirm the right to have an
abortion, want to exercise the right to have an abortion
without affirming it for other women who say, I believe
abortion should not be legal. That patient, we say, [62]
let’s talk this over. And that patient, as of our new
policy, we suggest that she come back another day for
her procedure and process her own decision making and
the difficulty we have with that position.
Our concern as a clinic is largely that we want it to
be very clear for the record and to her, that all of her
options have been explored and that this is a decision
that she must take responsibility for. And that she must
process before she makes an irreversible act.
Q. You said that this consent form, that such a woman
must sign at the end has a paragraph about how if she
ever says that she was not counselled properly,, that you
will release the information publicly to the extent to
defend it or maybe not to the extent, but to defend that
you indeed counselled her?
A. Yes. If she says one, she had an abortion and two, it
was at the Allentown Women’s Center, and three,
indicates in some way she did not have her options
explained to her or was inadequately counselled or that
in any way we were not non-directive or in some way
coerced her into a rushed decision, we will then defend
ourselves against those mistruths [63] by opening the
record.
Q. The newspaper article, it said that two women were
told to wait and they said that you had made that
statement.
A. That’s correct.
Q. Is it true that you had said since the policy was
547
started in April, that indeed two women were told to
wait?
A. The first woman was in April. We had a staff
meeting following her visit to our clinic. She indeed was
asked to wait, but at that time the form had not been
developed. It was developed as the result of her visit to
our clinic. But functionally, she was asked to wait and
went through the clarification of her options having been
explained and so forth and so on, as we discussed in the
form.
The form was then developed and then was used
with the second patient, who came in, who volunteered
to us that she felt that abortion should be illegal, but
indeed that she did want one.
Q. The newspaper article said that both women came
back, one saying she had dropped her opposition to legal
abortion and the other signed a consent [64] form. The
woman they are saying, dropped her opposition of legal
abortion, is that the first woman in April?
A. Yes, yes.
Q. Is that accurate what the newspaper stated that she
dropped her opposition to legal abortion?
A. It’s accurate, she said that. I think it is also
important that you have a complete picture, that had she
not said that we still would have given her an abortion
on the second visit, if it was clear to us that that is what
she wanted.
Q. Do you know how long a period of time was
between her first visit to AWC and her second visit when
she had the abortion?
A. No, but it was short.
Q. Less than a week, more than a week, do you know?
A. That is retrievable. I don’t even know if that is
retrievable at this point. It was short. It was probably
not more than a week, but I can’t guarantee it. I could
say with pretty well absolute certainty that it was two
548
weeks.
Q. With the second woman who signed the consent
form, do you know the period of time between when [65]
she first came to AWC and when she returned and
signed the consent form?
A. The same, it was short.
Q. With the same, probably under a week, but definitely
under two weeks.
You had said early on, and correct me if I am wrong,
that women who say they believe abortion is wrong or
murder or illegal, that raises a red flag to AWC that they
might have some trouble or some ambiguity or
uncertainty with the abortion decision; is that fair?
A. It raises a red flag about more than that. It raises a
red flag about that they might possibly have more guilt
or more damaged self-worth or some kind of adverse
psychological sequelae is more likely in those instances.
So all of those things are taken, you know, addressed by
the counselor in her thinking process.
* * *
[66] Q. Who has to sign the consent form?
A. Let’s take this very slow. If approximately fifteen
per cent of our patients we become aware without asking
that they believe in some way that abortion is wrong or
murder or something to that effect, but still wish to have
one. Less than one per cent of our patients volunteer to
us that they believe that abortion should not be available
to other women, it should be illegal, which is stronger
and more extreme. But that they would like to exercise
the option of having a legal abortion and they would also
like to cutoff that option for other women.
Those women in the fifteen per cent category,
sometimes we ask patients to wait, because they are so
ambivalent or so distraught as they present themselves to
549
us that we want to give them or sometimes they are
coerced. Those women we want to give the opportunity
to further process their decision making before they take
an irreversible act. That is for the best interest of the
patient.
That slender number of patients [67] who say that
abortion should be illegal, not only for their sake, but
also because we want to share with them that we need to
make it clear that they must take responsibility for their
own decision making and not lay it at the feet of the
provider, that we are going to ask them to delay their
abortion and return on another day after they have fully
processed that they have explored their options and that
they understand that they must take responsibility for
their decision making.
MR. ZEMAITIS: Let me just ask a question, which
I think will help clear it up.
The fifteen per cent, the larger group of women,are
all of those women required to sign this new form?
THE WITNESS: None of them. This form has only
been used twice and we see over four thousand patients
a year.
MR. ZEMAITIS: The only time the form is used is
in that much smaller group of people, where the woman
thinks that abortion should be illegal and she returns on
a second visit; is that right?
[68] THE WITNESS: She then returns on a second visit
and she then -- to date, all of these women have
remained steadfast in their desire to terminate their
pregnancy.
There may be many more women who come to our
clinic who think that abortion should be illegal, but we
do not ask questions about that.
BY MS. MERSHIMER:
Q. So it is this one per cent or even smaller group --
MR ZEMAITIS: Much smaller.
550
BY MS. MERSHIMER:
Q. -- that feel abortion should not be available for all
women that are asked to sign a consent form?
A. Correct.
Q. Or what is this form called, because I do not want to
call it a consent form?
A. It’s so new, it doesn’t have a name.
I would just like to say that there is an error in this
article. We never say, you may return if you change your
mind. We do not attempt [69] to change people’s minds.
* * *
[70] Q. For the record, we have had marked as
Defendant’s Exhibit-21 the form that we have been
discussing for the last few minutes; that has no caption to
it, correct?
A. Yes.
Q. You had said that one woman had returned to the
clinic;that second women, and she had signed this form?
A. Yes.
Q. If she had not signed the form,had refused to sign
the form, could she have received an abortion at AWC?
A. I think not. But I think the form functions largely as
an information sharing and educational device. So I
think it’s extremely unlikely that such a situation would
arise.
Q. In the last paragraph --
MR. ZEMAITIS: You have not had to face that
situation yet?
THE WITNESS: That’s correct.
BY MS. MERSHIMER:
In the last paragraph, one of the statements [71] is that,
"If in the future I
A. There should be an "If."
Q. "If in the future I ever publicly state that the
551
Allentown Women’s Center counselled me inadequately
or that I was not fully aware of the gravity of what I was
doing in terminating my pregnancy, I understand that I
will by so doing, give up all right to confidentiality and
that the staff of the Allentown Women’s Center will
defend their non-directive counselling protocols publicly."
My question to you is: What is meant by "all right to
confidentiality?"
A. We are affirming our right to confirm that this
patient who has already said that she had an abortion at
the Allentown Women’s Center, to give our version of
that event and to represent it accurately, specifically the
counselling component.
Q. So you would not release her entire patient record
then?
A. No, we would not do that and that is not made clear
or unclear by this statement. But we would not, in fact,
consider that to be relevant. We would only correct any
misinformation that she might be giving out about our
facility.
* * *
552
Defendants’ Exhibit 60:
Discovery Excerpts
PLAINTIFF’S OBJECTIONS AND RESPONSES
TO DEFENDANTS’ REQUESTS FOR ADMISSIONS
Plaintiffs respond to Defendants’ Requests for
Admissions as follows:
* * *
Request for Admission No. 2:
While delay in the performance of an abortion may
increase the risks to the patient from both a mortality
and a morbidity standpoint, the increased risks may be
negligible and are dependent upon the stage of gestation
(first, second, or third trimester). A week delay in the
first trimester will not likely result in a harm while there
may be greater risks in the second trimester, with the
risks more worthy of consideration in the latter part of
the second trimester and throughout the third trimester.
Response to Request for Admission No. 2:
Request for Admission No. 2 is admitted.
* * *
Request for Admission No. 8:
Some early abortions may be more dangerous than
later abortions due to the condition of the patient, the
type of procedure used in performing the abortion, or
the skill of the performing physicians.
Response to Request for Admission No. 8:
Request for Admission No. 8 is admitted.
* * *
553
DEFENDANTS’ RESPONSES TO PLAINTIFFS’
REQUESTS FOR
ADMISSION AND INTERROGATORIES
ADDRESSED TO DEFENDANTS
* *
Request for Admission No. 10
Adolescents have one of the highest suicide rates of
any segment of the population.
RESPONSE:
Defendants object to this interrogatory as being
irrelevant to the constitutionality of the Act, particularly
in that this admission does not distinguish between males
and females and in that it does not relate to pregnant
teens. Without waiving this objection, Admission No. 10
is DENIED.
ANSWER TO INTERROGATORY NO. 10:
The attached two tables (Exhibits 2 and 3)
demonstrate that in Pennsylvania and the United States,
teenagers have the lowest rate of suicide among the age
groups.
* * *
554
Commonwealth of Pennsylvania - Department of Health
State Health Data Center
Resident Suicide Deaths by Age and Sex,
Number and Rate, Pennsylvania, 1987 (Provisional)
BY NUMBER:
AGE
GROUP
TOTAL MALES FEMALES
All Ages 1,489 1,210 279
Under 10 0 0 0
10-14 14 12 2
15-19 89 72 17
20-24 145 127 18
25-34 319 269 50
35-44 219 173 46
45-54 180 129 51
55-64 178 131 47
65-74 194 165 29
75 + 151 132 19
555
BY RATE:*
AGE
GROUP
TOTAL MALES FEMALES
All Ages 12.5 21.3 4.5
Under 10 - - -
10-14 1.8 3.0 0.5
15-19 9.8 15.6 3.8
20-24 14.8 25.8 3.7
25-34 16.4 27.9 5.1
35-44 14.1 22.9 5.8
45-54 15.4 23.2 8.3
55-64 14.2 22.6 6.9
65-74 19.7 39.6 5.1
75 + 20.6 51.3 4.0
Rate per 100,000 estimated 1986 population for each
specified age group.
* * *
556
EXCERPTS FROM PLAINTIFFS’ TRIAL EXHIBITS
Plaintiffs’ Exhibit 49:
DOH Instructions and Definitions
for Report of Induced
Termination of Pregnancy Form
(July 1988)
INSTRUCTIONS AND DEFINITIONS
REPORT OF INDUCED TERMINATION
OF PREGNANCY
INTRODUCTION
Pennsylvania
Department of Health
State Health Data Center
July, 1988
Purpose: These instructions and definitions are designed
as an aid to acquaint hospital and clinic personnel,
physicians, and others with responsibilities related to
completing and filing reports of induced termination of
pregnancy (induced abortion), The purpose is to achieve
improved reporting by promoting better understanding of
the forms and of the uses of information entered on
them.
Generally the person in charge of the institution or
facility where the induced abortion is performed has the
overall responsibility for obtaining the required data,
preparing the report, and filing the report with the
Department of Health. For abortions performed outside
a hospital, clinic, or other institution, the physician
performing the abortion is responsible for preparing and
filing the report.
557
State Reporting Requirements: The reports shall be
completed by the hospital or other licensed facility,
signed by the physician who performed the abortion and
transmitted to the Department of Health within 15 days
after each reporting month. Mail to the
Department of Health
State Health Data Center
ISSR Unit
P. 0. Box 90
Harrisburg, PA 17108
Specific Responsibilities: The hospital, clinic or other
institution or facility where the induced abortion is
performed is responsible for obtaining the necessary
data, completing the form, and filing it with the State
within the time period specified by law. To ensure the
proper performance of these responsibilities, it is
preferable that one staff member be given the overall
responsibility and authority to see that the reports are
completed and filed on time. Specifically, the hospital,
clinic, or other institution should:
o Develop efficient procedures for prompt preparation
and filing of reports.
o Collect and record the information required by the
report.
o Prepare a correct and legible report, making certain
that every item is completed.
o File the report within the time specified in the
Abortion Control Act (15 days after each reporting
month).
558
o Cooperate with State officials concerning queries on
report entries.
o Call on the State Health Data Center at (717)
783-2548 for advice and assistance when necessary.
Physician: For induced abortions performed in a
hospital, clinic, or other institution, the physician
performing the abortion is responsible for providing the
medical information required by the report. When an
induced abortion is performed outside a hospital, clinic,
or other institution, the physician performing the
abortion is responsible for obtaining all of the necessary
data, completing the form, and filing it with the State
within the time period specified by law.
PART I - GENERAL INSTRUCTIONS FOR
COMPLETING REPORTS
The data necessary for preparation of the induced
termination of pregnancy report are obtained from the:
o Patient
o Attending physician
o Hospital or clinic records
The data obtained from these reports are very important
from both a demographic and a public health viewpoint.
Therefore, it is essential that these reports be prepared
accurately. These general rules should be followed:
o File the original report with the Department of
Health. These reports have sequential file numbers.
Do not reproduce or duplicate these forms.
559
o Avoid abbreviations except those recommended in
the specific item instruction.
o Spell entries correctly.
o Refer problems not covered in these instructions to
the State Health Data Center.
o Use the current form designated by the State.
o Type all entries whenever possible. Do not use worn
typewriter ribbons.
o If a typewriter cannot be used, print legibly in black
ink.
o Complete each item following the specific
instructions for that item.
PART II - COMBATING THE REPORT OF
INDUCED TERMINATION OF PREGNANCY
These instructions pertain to the 1988 Report of Induced
Termination of Pregnancy.
1-2 PLACE OF TERMINATION
1. FACILITY NAME
Enter the full name of the hospital or clinic where the
induced termination of pregnancy occurred.
If the induced termination of pregnancy occurred in a
hospital or a clinic that is physically situated within a
hospital or is administratively a part of a hospital, enter
the full name of the hospital.
560
If the induced termination of pregnancy occurred in a
freestanding clinic, a clinic that is physically and
administratively separate from a hospital, enter the full
name of the clinic.
If the induced termination of pregnancy occurred in a
physician’s office or some other place, enter the name of
the office or place.
In the coding boxes, enter the five-digit number found on
the first line of your mailing label, as shown below.
8-0228
WOMENS HEALTH SERVICES
107 SIXTH STREET
FULTON BUILDING 3RD FLOOR
PITTSBURGH, PA 15222
ATTN: PATRICIA MADDEN
2. COUNTY OF PREGNANCY TERMINATION
Enter the name of the county where the pregnancy
termination occurred. In the coding boxes, enter the
correct county code. See Appendix A.
3. PATIENTS IDENTIFICATION
Enter the hospital, clinic, or other patient identification
number. This number must be one that would enable
the facility or physician to access the medical file of this
patient. Do not use the patient’s name.
561
4 a-b. RESIDENCE OF PATIENT
The patient’s residence is the place where her household
is located. This is not necessarily the same as her "home
State." "voting residence," "mailing address," or "legal
residence." The State and county should be that of the
place where the patient actually lives. Never enter a
temporary residence such an one used during a visit,
business trip, or a vacation. Residence for a short time
at the home of a relative or friend is considered to be
temporary and should not be entered here. Place of
residence during a tour Of military duty or during
attendance at college is not considered temporary and
should be entered an the place of residence of the
patient on the report.
If the patient has been living in a facility where an
individual usually resides for a long period of time, such
as a group home, mental institution, nursing home,
penitentiary, or hospital for the chronically ill, this facility
should be entered as the place of residence.
4 a. RESIDENCE - STATE
Enter the name of the State where the patient lives.
This may differ from the State in her mailing address. If
the patient is not a resident of the United States, enter
the name of the country and the name of the unit of
government that is the nearest equivalent of a State.
4 b. RESIDENCE - COUNTY
Enter the name of the county where the patient lives.
In the coding boxes, enter the correct county code. See
Appendix A. For counties outside Pennsylvania, leave
562
5. DATE OF PREGNANCY TERMINATION
Enter the exact month, day, and year of the pregnancy
termination.
The date the pregnancy was actually terminated should
be entered. This may not necessarily be the date the
procedure was begun.
Enter the full name of the month - January, February,
March, etc. Do not use a number or abbreviation to
designate the month.
6. AGE LAST BIRTHDAY
Enter the age of the patient in years at her last birthday.
7. CLINICAL ESTIMATE OF GESTATION
Enter the length of gestation as estimated by the
attending physician in completed menstrual weeks. Do
not compute this information from the date last normal
manses began and date of termination. If the attendant
has not done a clinical estimate of gestation, enter
"None."
8. PREVIOUS PREGNANCIES (complete each
section)
8 a. Now Living
Enter the number of children born alive to this patient
who are still living at the time of this termination. Do
not include children by adoption. Check "None" if the
blank.
563
patient has had no previous pregnancies, or if all
previous children are dead.
8 b. Now Dead
Enter the number of children born alive to this patient
who are no longer living at the time of this termination.
Do not include children by adoption. Check "None" if
the patient has had no previous pregnancies or if all
previous children are still living.
8 c. Spontaneous
Enter the number of previous pregnancies that ended
spontaneously and did not result in a live born infant.
This should not include induced terminations. Check
"None" if the patient has had no previous pregnancies or
if all previous pregnancies ended in live born infants.
8 d. Induced
Enter the number of previous induced terminations
(induced abortions) that this patient has had. Do not
include this termination. Check "None" if the patient has
had no previous induced terminations.
9 a-b. TYPE OF TERMINATION PROCEDURES
(Definitions of certain abortion procedures can be found
in Appendix B)
9 a. Check the box that describes the primary
procedure that actually terminated this pregnancy.
Check only one box. If more than one procedure was
used, identify the additional procedure(s) in item 9b. If
a procedure not listed was used, check "Other" and
564
specify on the line provided.
9 b. Check the box(es) that describe the additional
procedure(s) used. If no additional procedures were
used, leave all boxes blank. If a procedure not listed was
used, check "Other" and specify on the line provided.
10. MEDICAL COMPLICATIONS OF PREGNANCY
Check all that apply. If none apply, leave item blank.
11. NAME OF ATTENDING PHYSICIAN
Enter the full name of the attending physician. Be sure
to spell it correctly and verify correct spelling. This item
is used to query for missing or additional information.
Complete the license number of the physician, the
signature, and the date submitted to the Department of
Health.
565
APPENDIX A
PENNSYLVANIA COUNTY CODES
COUNTY COUNTY
CODE COUNTY CODE COUNTY
01 Adams 35 Lackawanna
02 Allegheny 36 Lancaster
03 Armstrong 37 Lawrence
04 Beaver 38 Lebanon
05 Bedford 39 Lehigh
06 Berks 40 Luzerne
07 Blair 41 Lycoming
08 Bradford 42 McKean
09 Bucks 43 Mercer
10 Butler 44 Mifflin
11 Cambria 45 Monroe
12 Cameron 46 Montgomery
13 Carbon 47 Montour
14 Centre 48 Northampton
15 Chester 49 Northumberland
16 Clarion 50 Perry
17 Clearfield 51 Philadelphia
18 Clinton 52 Pike
19 Columbia 53 Potter
20 Crawford 54 Schuylkill
21 Cumberland1 55 Snyder
22 Dauphin 56 Somerset
23 Delaware 57 Sullivan
24 Elk 58 Susquehanna
25 Erie 59 Tioga
26 Fayette 60 Union
27 Forest 61 Venango
28 Franklin 62 Warren
566
29 Fulton 63 Washington
30 Greene 64 Wayne
31 Huntingdon 65 Westmoreland
32 Indiana 66 Wyoming
33 Jefferson 67 York
34 Juniata
567
APPENDIX B
DEFINITIONS OF INDUCED ABORTION
PROCEDURES
Suction curettage (Also known an vacuum aspiration). -
In this procedure the cervical canal is dilated by the
successive insertion of instruments of increasing diameter
called dilators. When the opening is large enough, a
flexible tube (cannula) is inserted into the uterine cavity,
and the fetal and placental tissues are then suctioned out
by an electric vacuum pump.
Sharp curettage (Also known as dilatation and curettage,
D & C, or surgical curettage). - This procedure involves
the dilation of the cervix an in suction, although usually
to a larger diameter. The fetal and placental tissues are
then scraped out with a curette, which resembles a small
spoon.
Dilation and evacuation (D & E). - This procedure, used
most frequently in the second trimester, involves opening
the cervix (dilation) and using primarily sharp
techniques, but also suction and other instrumentation
such an forceps for evacuation.
Intrauterine saline instillation (Also known as saline
abortion and saline amniotic fluid exchange). - This
procedure entails withdrawing a portion of the amniotic
fluid from the uterine cavity by a needle inserted through
the abdominal wall and replacing this fluid with a
concentrated malt solution. This process induces labor,
which results in the expulsion of the usually dead fetus
approximately 24 to 48 hours later.
Intrauterine prostaglandin instillation. - This procedure
involves injecting a prostaglandin - a substance with
568
hormonelike activity - into the uterine cavity through a
needle inserted through the abdominal wall. The
interval between injection and expulsion tends to be
shorter than in a saline abortion.
Hysterotomy. - This procedure involves surgical entry
into the uterus, as in a cesarean section, that removes a
fetus that is too small to survive even with extraordinary
life support measures. It is usually performed only if
other abortion procedures fail.
Hysterectomy. - In this procedure, the uterus is removed
either with the fetus inside or after the fetus has been
removed. It is usually performed only when a
pathological condition of the uterus, such as fibroid
tumors, warrants its removal or when a woman desires
sterilization.
All definitions, except for D & E, are from Legalized
Abortion and the Public Health (Institute of Medicine,
1975). The definition of D & E is based on national
Center for Health Statistics consultation with the Center
for Health Promotion and Education, Centers for
Disease Control.
Ail other procedures should be shown an "Other" and the
specific procedure listed. This category includes
procedures using a combination of agents, such as urea
and prostaglandin, prostaglandin and oxytocin, or
prostaglandin and saline.
569
APPENDIX C
DEFINITIONS
The following definitions are included in the 1977
revision of the Model State Vital Statistics Act and
Regulations. The definitions of live birth and fetal death
conform to the definitions adopted by the Assembly of
the World Health Organization.
Live birth is the complete expulsion or extraction from its
mother of a product of human conception, irrespective of
the duration of pregnancy, which after such expulsion or
extraction, breathes, or shows any other evidence of life
such an beating of the heart, pulsation of the umbilical
cord, or definite movement of voluntary muscles,
whether or not the umbilical cord has been cut or the
placenta is attached.
Note - If an infant breathes or shows any other evidence
of life after complete delivery, even though it may be
only momentary, the birth must be registered as a live
birth and a death certificate must also be filed.
Fetal death is death prior to the complete expulsion or
extraction from its mother of a product of human
conception, irrespective of the duration of pregnancy; the
death is indicated by the fact that after such expulsion or
extraction, the fetus does not breathe or show any other
evidence of life, such as beating of the heart, pulsation of
the umbilical cord, or definite movement of voluntary
muscles.
Induced termination of pregnancy is the purposeful
interruption of pregnancy with the, intention other than
to produce a live-born infant or to remove a dead fetus
and which does not result in a live birth.
570
Note - If an induced termination is performed on a fetus
of 16 weeks gestation or longer, a Certificate of Fetal
Death as well as a Report of Induced Termination of
Pregnancy must be filed.
571
REPORT OF INDUCED TERMINATION OF
PREGNANCY MONTHLY TRANSMITTAL FORM
Please return this page with all of your completed
Report of Induced Termination of Pregnancy forms for
the reporting period of AUGUST 25-31 by September
15, 1988. Also, complete the requested information
below for your facility:
FACILITY I.D .__ -_____________
NAME OF FACILITY____________________________
CONTACT PERSON/TITLE_______________________
TELEPHONE NUMBER ( ) ____ - __________
DATE SUBMITTED______________________________
NUMBER OF COMPLETED FORMS ENCLOSED
Please complete and return this page even if you do not
have any procedures to report.
MAIL TO: Pennsylvania Department of Health
State Health Data Center
ISSR Unit
PO Box 90
Harrisburg, PA 17108
572
Plaintiffs’ Exhibit 60:
Veto Message to the Pennsylvania Senate
on S.B. 742
of Governor Dick Thornburgh
(Dec. 23, 1981)
December 23, 1981
To the Honorable, the Senate
of the Commonwealth of Pennsylvania
I have before me for action Senate Bill 742, Printer’s
No. 1535, which would establish a number of detailed
procedures and requirements with respect to the
performance of medical abortions.
Perhaps no issue in recent times has generated more
concern, conflict and passion than the issue of what, if
any, restrictions should be imposed upon the ability to
obtain an abortion. Perhaps, then, it should not be
surprising that this bill has led to a considerable amount
of public passion and controversy. Unfortunately, it also
appears to have generated a considerable amount of
misinformation and misunderstanding.
Many who favor stringent limitations on abortion
appear to perceive this bill as a means of furthering that
objective. Many who oppose most or all restrictions on
abortion appear to perceive this bill as preventing
virtually all abortions.
I have carefully studied this bill and those opinions
of the United States Supreme Court and other federal
courts which establish the legal and constitutional
parameters for the performance of medical abortions. I
also have reviewed similar laws in other states and a
variety of relevant materials and opinions reflecting all
573
points of view on the cluster of issues related to the
abortion question.
I have concluded that this bill does far less to restrict
the ability of a woman to elect to have an abortion than
its proponents perceive or its opponents fear.
I have stated a number of times in the past my
personal opposition to abortion on demand, and my view
that abortion should not be employed as an alternative
to birth control techniques. I have also expressed my
concern that too many abortions are too casually
undertaken. This is a matter of particular concern with
regard to teen-agers who are usually less equipped than
adults to independently evaluate the decision to have an
abortion or understand the consequences it may later
entail.
On the other hand, I also have stated in the past my
personal view that abortion should be a permissable
medical option in certain narrowly restricted situations,
including threat to the life of the mother, rape, incest or
serious and irreparable harm to the health of the mother.
While this bill contains a number of proposed
requirements with which I am in agreement, I have
concluded that it really does little, if anything, to prohibit
abortions which can now be performed in the
Commonwealth.
What this bill would do is erect a series of hurdles
which would have to be cleared by a pregnant woman
interested in obtaining an abortion.
Any competent, pregnant, adult intent upon
obtaining an abortion who could negotiate those hurdles,
could obtain one, much as she now could in this state. It
must be assumed that the same services now available to
assist and counsel women considering abortion would be
available to provide assistance to any such woman in
negotiating the procedural hurdles contained in this bill.
On the other hand, for those women, often minors,
574
who face the dilemma of an unwanted pregnancy with
fear or ignorance, some of these proposed procedures
would provide certain valuable information and
protection.
Specifically, the bill would permit a pregnant woman
to elect an abortion before the fetus is viable - that is,
capable of surviving outside the body of the mother — if
her physician made a medical determination that it was
necessary in light of all factors relevant to the well-being
of the woman, including physical, emotional,
psychological, age and family circumstances.
The bill would, however, require women seeking
such abortions to be counselled on the options with
regard to an unwanted pregnancy and the consequences
of each, including the medical risks involved in both
proceeding with an abortion and with carrying the fetus
to term. It would then require a waiting period of one
day, which would provide the woman with an opportunity
to assess and reflect upon this information. This waiting
period would not apply where a medical emergency
compelled the performance of an abortion.
The bill would require minors and adjudged
incompetents to obtain the consent of a parent or
guardian for an abortion if so desired. In the alternative,
such a pregnant woman could obtain a court order
authorizing the performance of an abortion upon a
finding either that the woman is mature and capable of
giving her informed consent, or that the performance of
an abortion would be in the woman’s best interests. In
such a proceeding, the pregnant woman would be
entitled to court-appointed counsel, and all proceedings
would be confidential. In assessing the best interests of a
minor seeking an abortion, I must assume that any court
would rely heavily on the best medical judgment of the
petitioner’s physician.
The bill would require that any abortion after the
575
first trimester of pregnancy be performed in a hospital.
The bill would require certain precautions to help
insure the survival of an aborted fetus which was viable.
Where a physician has determined prior to an abortion
that the fetus is, in fact, viable, an abortion could only be
performed upon a determination by the woman’s
physician that the abortion was necessary to preserve her
life or health, and then, to the extent medically feasible,
by the method most likely to preserve the viability of the
fetus. I am advised that this is already the case pursuant
to current normal medical practice.
The bill would require that physicians performing
abortions file reports setting forth certain detailed
information relating to the facts and circumstances
involved in the abortion. Such records would not contain
the identity of the pregnant woman, but would be
available for public inspection.
The bill would place restrictions an abortion-related
coverage that could be provided in health care and
disability insurance policies.
The bill provides for an annual review by the state
Health Advisory Board of the standards and criteria for
assessing viability, While the specific question of viability
in any particular case appears to be left to the medical
determination of the attending physician, the regularly
revised standards devised by this board would appear to
constitute a presumption against which each physician’s
determination could be judged. I have reservations
about this provision. It has the potential to further
politicize and complicate the whole issue of abortion. It
will focus undue attention on a small board that may not
reflect the consensus in the medical community at any
given time on an issue that seems best left to the
unfettered determination of individual treating physicians
on a case-by-case basis. This is particularly troublesome
since, by law, only half of that board’s members are
576
physicians. I do not object to a periodic review and
revision of criteria of viability. I believe, however, that
this should be the responsibility of the recognized
organizations of the medical community -- not of
government.
Finally, this bill defines human life as beginning at
the moment of fertilization. Much of the intent and
purpose of the bill appears to flow from that assertion.
I do not believe that I have the scientific or
theological expertise to affirm or refute that premise, nor
do I believe that the members of the General Assembly
do. The U.S. Supreme Court has noted the consensus
among medical practitioners and theologians over a long
period of time that human life does not begin until the
time of viability or even later. The court has noted that
this has been the predominant view in the Jewish and
Protestant communities, and was also "official Roman
Catholic dogma" until the last century.
It has been argued by many that the extremely
detailed nature of some of the counselling and reporting
requirements, when combined with the stringent criminal
penalties that are provided for virtually any violation, is
intended to deter women from seeking abortions and
physicians from performing them, even under
circumstances where the courts have made clear that
abortions cannot be constitutionally restricted. I believe
that these provisions, combined with the "human life"
definition and power of a small state board to set
standards of viability, have given rise to most of the
concern and consternation expressed over this bill.
In performing my responsibility to properly evaluate
this bill, I must carefully weigh not only the literal
substance of the bill but what its effects could be. There
is no bill to which I have given more careful
consideration or undertaken more precise review and
reflection. I have reached the following conclusions.
577
The medical necessity test for obtaining an abortion
prior to the viability of a fetus, is consistent with U.S.
Supreme Court holdings and is, in my view, reasonable.
The requirement for counselling and assessment are,
in my view, reasonable for someone confronting a
surgical procedure of this type and a personal decision of
this magnitude -- one which studies show could have
lasting emotional impact. Requiring a physician to
provide such counselling or medical advice is, in my
view, reasonable and comparable to the kinds of things
physicians do in other similar situations. Indeed, I would
think that any thoughtful and sensitive physician, under
any circumstances, would agree that it is appropriate to
apprise a patient of the various potential medical,
psychological and other risks and effects associated with
such a procedure. Further, I think it is right to explain
to a pregnant woman that there are alternatives to
abortion if her only objection is raising the child or her
only fear is the inability to support the child. An
abortion that would not be performed but for ignorance
or fear is perhaps an abortion best not performed.
On the other hand, I doubt that requiring the
preparation and availability of detailed color photographs
of a fetus at various gestational increments is necessary
to an informed abortion decision. Moreover, their
presentation would likely cause many women
considerable anguish and distress.
While I personally believe that a brief, so-called
"waiting period" is reasonable, I must note that
comparable provisions in other bills have been held
unconstitutional by a number of federal appeals courts.
I feel that the provision for parental or guardian
consent, or in the alternative, court review, is reasonable
and consistent with traditional and legal parental
responsibilities for the welfare of their minor children,
and with the traditional role of the courts to determine,
5 7 8
when necessary, the best interests of minor children. At
no time is a minor more likely to need or stand to
benefit from the guidance and support of a responsible
adult than when facing the emotional trauma and
dilemma of an unwanted pregnancy. I believe, however,
that if the alternative of a court determination is to meet
constitutional standards of reasonableness, it should
include a specific, limited time period within which the
court must act rather than the more general and
undefined term, "promptly", as the bill now provides.
I do not believe that the requirement that an
abortion on a woman beyond the first trimester of
pregnancy be performed in a hospital is unreasonable.
In fact, the great majority of abortions are performed in
the first trimester. Abortions performed beyond that
period are more likely to entail greater risks,
complications and care. However, I have serious
reservations about the proposed requirement that all
such abortions be performed on an in-patient basis. The
necessity of proceeding on an in-patient basis, in my
view, should be determined on a case-by-case basis by
the attending physician. Clearly, proceeding on an
in-patient basis would involve a greater burden and cost
to the woman involved. Where the need to proceed on
an in-patient basis is not reasonably related to maternal
health or the protection of a potentially viable fetus, this
requirement would appear to be unduly restrictive and
thus unconstitutional.
The provisions which limit the aborting of a fetus
medically determined to be viable and which require
precautions to preserve the life of an aborted fetus which
is in fact viable are, in my view, right and reasonable. In
fact, the overwhelming majority of abortions are
performed before any question of viability arises. I
cannot disregard a recent Philadelphia Inquirer
investigative feature which exposed the fact that in at
579
least some cases of more advanced pregnancy, viable
fetuses were being aborted and permitted to die. If a
fetus is capable of living and growing outside the womb,
it is difficult for me to accept that it does not embody a
human life. If we are to regard ourselves as a
humanitarian society, I believe that we must take every
reasonable precaution in favor of the preservation of
innocent life. This would include, in my view,
requirements such as the ones in this bill for the
presence of a second physician where an aborted fetus
may be viable and utilization of the abortion technique,
where consistent with maternal life and health, most
likely to preserve a viable fetus.
I am troubled, however, by the provision in Section
3212 (B) of the bill which, when read in conjunction with
the definitions of "born alive" and "viability" in Section
3208, would appear to require the use of every
scientifically possible means, including artificial
sustenance, to maintain in a technical state of life,
presumably indefinitely, an aborted fetus or organism,
however defective, deficient, or diseased, that does not
embody any prospect of human life as we know it.
While this may not have been the intent of the
legislation, this provision could require a physician, under
the risk of severe criminal penalties, to artificially
maintain even an aborted anencephalic fetus, that is, one
with no head or brain. Such cases have been
documented.
The provision would establish a higher standard of
care for a viable fetus or human organism than is
required in the case of a diseased or failing adult.
Whether and when artificial means of sustenance should
be employed is a decision which, in my view, is best left
to the affected family and their physician.
I believe that some general reporting requirements
are reasonable and could provide the kind of data that
580
would be beneficial in enabling us to make more
informed judgments about the continuing questions
related to the matter of abortion. Indeed, 30 other states
have enacted legislation with some type of reporting
requirements. However, I have reservations about
several of the specific reporting requirements proposed
in this bill, and a particular concern about the availability
of such reports for general public inspection. I am
concerned that this could lead to the compromising of
the identities and privacy of women who have obtained
abortions, and of the doctor-patient relationship.
I also have some reservations about the
constitutionality of some of the restrictions in the
insurance provision and on the use of public health
facilities in performing abortions. Where the latter are
the only accessible facilities for women who are seeking
abortions under circumstances where they would be
permitted in private facilities, the application of this
restriction seems unfair and has been held
unconstitutional.
I have reviewed the history and development of this
bill, it appears to me that the various amendments and
revisions to the bill as initially proposed reflect a genuine
effort to adopt procedures to insure informed consent by
adults and reasonable protection for the well-being of
minors considering abortion, as well as standards and
procedures for protecting and preserving, to the extent
possible and consistent with the life and health of the
mother, the potential for new human life, and to do so
within the constitutional limitations prescribed by the
U.S. Supreme Court.
The U.S. Supreme Court has recognized the interest
of a state in reasonably regulating abortion in ways
related to maternal health and well-being, and for the
purpose of protecting the "potentiality of human life." I
believe that many provisions of the bill, as I have
581
indicated, are consistent with those interests and are
reasonable, particularly with regard to those women who,
because of their circumstances, would benefit from the
guidance and protection afforded by them.
On the other hand, I am concerned that other
provisions, and to some extent, the overall tone and
tenor of the bill, would have the effect of imposing an
undue and, in some cases, unconstitutional burden upon
even informed, mature adults intent upon obtaining an
abortion under circumstances in which the U.S. Supreme
Court has determined they are entitled to do so. For
example, Section 3213 would preclude the victim of a
rape who has made an informed and mature decision
that she absolutely does not want to bear any child that
might result from that rape from exercising the option of
menstrual extraction, and would force her to wait the
five weeks or more that is required for the fact of
pregnancy to be determined. This requirement would
appear to needlessly subject a woman in such a stressful
situation to additional trauma.
Likewise, I am concerned that some of the detailed,
complex, and burdensome requirements of the bill,
accompanied as they are by severe criminal penalties,
could well foster an atmosphere in which many
physicians would be deterred from providing the kind of
abortion-related medical services to which the U.S.
Supreme Court has held their patients are
constitutionally entitled. This could well disrupt the
traditional doctor-patient relationship and impinge upon
the right of physicians to practice. Of even greater
concern is the potential for more experienced and
conscientious physicians to refrain from involvement in
even medically necessary abortions, and to abandon the
field to marginal practitioners. It could even lead to a
resurgence of "back alley" abortions, which no thoughtful
person would wish to happen. I believe that this concern
582
could be alleviated by reduced criminal sanctions which
would still be sufficient to deter physicians from willful
violations.
I am also concerned that in its entirety the bill in its
current form goes further than is necessary in protecting
the state interests in this area to which I have referred.
In so doing, it threatens to create additional regulation
and bureaucracy and to unduly involve government in
the private lives of its citizens.
Accordingly, and after extensive consideration and
deliberation, I am returning this bill without my
signature. In so doing, I wish to indicate the availability
of my office to work with the General Assembly in
developing revised legislation to effectuate the provisions
with which I have indicated my agreement consistent
with the objections I have expressed.
N .
Dick Thornburgh
Governor
583
Plaintiffs’ Exhibit 61:
Message to Pennsylvania Senate on Signing of
1982 Pennsylvania Abortion Control Act
of Governor Dick Thornburgh
(June 11, 1982)
June 11, 1982
To the Honorable, the Senate
of the Commonwealth of Pennsylvania
I have before me for consideration Senate Bill 439,
Printer’s No. 2049, which would require the
Commonwealth to provide to criminal justice agencies
certain criminal record information, upon appropriate
request, free of charge. This bill has been subject to a
number of unrelated amendments, the most important,
and only controversial, one of which has to do with the
procedures related to the performance of abortions in
the Commonwealth.
I was confronted with such a measure in the form of
S.B. 742 last December. That bill contained 11
provisions to which I objected. In addition, the overall
tone and tenor was such that I felt it could have a
chilling effect in a constitutionally-protected area, and
created an aura of undue government intrusion into
private lives which conflicted with my convictions and
philosophy. On Dec. 23, 1981, I vetoed that bill, setting
forth in detail those concerns and objections.
My careful review of this revised measure reveals
that the statement of the bill’s sponsor that the new
measure was "tailored" to meet my objections appears to
be accurate. My review reveals that virtually every item
in the initial bill to which I objected has been removed
or appropriately revised in the current measure.
Key among the 11 provisions to which I objected in
584
the original bill were:
*A definition of "human life" as commencing at
the instant of fertilization. I objected to this, and it
has been removed from the current bill.
*A requirement that the state Health Advisory
Board set standards of fetus viability and, moreover,
review and revise such standards on an annual basis.
I objected to this and expressed the view that the
question of viability was more properly determined
on a case-by-case basis by an attending physician.
This provision has been removed from the current
bill.
*A provision requiring that detailed color
photographs depicting the incremental development
of the human fetus in the womb be made available
for showing to women contemplating abortion. I
objected to this and expressed the view that if
imposed an unreasonable and potentially anguishing
burden on women contemplating abortion. This
provision has been removed from the current bill.
*A requirement that all abortions after the first
trimester be performed on an in-patient basis. I felt
that this was a matter better left to the judgment of
the woman involved and her treating physician. I
objected to this provision, and it has been removed
from the current bill.
*A prohibition of menstrual extraction, even in
cases of rape. I found this objectionable. This has
now been eliminated in the bill currently before me.
*A provision prohibiting the inclusion of
abortion coverage in standard medical insurance
policies issued in the Commonwealth. I objected,
and this provision has been removed from the
current bill.
'Provisions which would have required the use
of heroic efforts and artificial sustenance to maintain
585
in a technical state of survival any fetus once aborted
which was capable of being so maintained, however
deformed and regardless of its prospects for any
meaningful life as we know it. This would even have
included anancephalic fetuses (i.e., those literally
born without a head or brain). I objected to this. It
has been eliminated in the current bill before me.
Under the current bill, physicians would only be
required to provide the same types of treatment to
an infant aborted alive that they would to a live
adult under comparable circumstances. This is
totally consistent with existing medical standards and
legal obligations.
‘Certain reporting requirements relative to the
performance of abortions which in my view did not
adequately protect the confidentiality of the
doctor-patient relationship and the right of personal
privacy. I objected, and the relevant provisions have
been eliminated in the current measure.
*A provision effectively preventing the
performance of abortions in state-owned or operated
hospitals. I objected to this, and expressed the view
that it would discriminate against women seeking
abortions who did not have access to private
hospitals. This provision has been eliminated. The
new bill would permit abortions to be performed in
state-owned or operated hospitals unless there was
another nearby hospital in which such an abortion
could be performed.
Severe criminal penalties on doctors who
violated even the ministerial provisions of the act. I
objected to this. The penalty structure has been
drastically altered in the current bill. In certain
cases, criminal sanctions have been removed
altogether. In the other instances, the criminal
sanctions imposed are now consistent with penalties
586
that already exist for comparable conduct and in
laws similar to this one as enacted in many other
states.
*A provision for court review of requests by a
juvenile for an abortion that failed to impose any
time limit within which the court must act, and thus
created the prospect of an indefinite and
unappealable delay in the process. I objected to this
omission, and the current bill would now impose a
requirement for speedy action in such court
proceedings.
This bill does contain eight provisions concerning
abortion procedures which were contained in the original
bill presented to me. At the time I vetoed that bill, I
stated that I did not approve of abortion on demand, and
had become convinced "too many abortions are too
casually undertaken." I also stated that I had become
convinced by reports, including an investigative account
by the Philadelphia Inquirer, that a need existed to
provide better protection for viable fetuses, particularly
those aborted alive. Indeed, it is worth noting that even
one of the most vocal legislative opponents of regulating
abortion procedures acknowledged during recent floor
debate on this bill that ". . . there is an abortion
problem."
I believe that society has in obligation to provide
certain basic protection for pregnant women
contemplating or confronting the abortion process,
particularly juveniles, and for a viable fetus which
embodies human life. I believe that this interest of
society in ensuring informed consent and protecting
human health and life should be achieved with the
minimum possible intrusion into the private lives of our
citizens, and with the least possible interference in a
decision-making process which should essentially be
between a woman and her treating physician.
5 8 7
I recognize that both proponents and opponents of
this bill have contended that it would limit or prohibit
abortions. Even the original bill, with its excessive and
objectionable provisions, would not in my view have
prevented anyone intent upon obtaining an abortion
from doing so. I believe that the provisions in the
current bill address the legitimate interests of society in
providing the basic protections I have referred to in a
minimally intrusive -- and acceptable - manner.
Under this bill, any abortion could be performed,
prior to the viability of the fetus, if it is found to be
medically or otherwise "necessary." The determination of
necessity is left strictly to the judgment of a treating
physician. The definition of "necessary" permits the
physician to consider a wide array of criteria, including
physical, emotional, psychological, and even familial
factors and the age of the woman seeking the abortion.
Under the necessity test as defined in this bill, it clearly
appears that very few, if any, abortions which can now be
performed under existing legal and medical standards
would be prohibited. The necessity test as articulated in
this bill is totally consistent with the express language of
the United States Supreme Court on this subject in Doe
vs. Bolton.
This bill would impose a requirement that a woman
contemplating abortion be counselled on all available
options and the medical consequences of each. I believe
this requirement to be reasonable for someone
confronting a surgical procedure of this type and a
personal decision of this magnitude -- one which studies
show could have a lasting emotional impact. Indeed, I
would think that any thoughtful and sensitive physician,
under any circumstances, would agree that it is
appropriate to apprise a patient of the various potential
medical psychological and other risks and effects asso
ciated with such procedure. Further, I think it is right to
588
explain to a pregnant woman that there are alternatives
to abortion if her only objection is raising the child or
her only fear is the inability to support the child. An
abortion that would not be performed but for ignorance
or fear is perhaps an abortion best not performed.
It is important to note that, unlike the previous bill,
this bill would not require physicians to personally
provide all aspects of such counselling, but rather only
those respecting medical matters. Other information and
counselling may be provided, as is now practiced in
responsible facilities, by knowledgeable counselors.
This bill would require a 24-hour "waiting period"
between the counselling and the actual performance of
an abortion. This period would provide a woman with
an opportunity to assess and reflect upon this
information. I believe this to be a reasonable
requirement, particularly since this waiting period would
not apply where a medical emergency compelled the
performance of an abortion. Absent such medical need,
I can foresee no harm arising from such a brief period of
delay and reflection. Indeed, I would think that such a
period of reflection is normal and reasonable whenever
someone is evaluating and confronting surgical
procedures that are even less imbued with stress and
risk.
This bill would require minors and adjudged
incompetents seeking an abortion to obtain the consent
of a parent or guardian. In the alternative, such a
pregnant woman could obtain a court order within a
fixed brief time period, authorizing the performance of
an abortion upon a finding either that the woman is
mature and capable of giving her informed consent, or
that the performance of an abortion would be in the
woman’s best interests. In such a proceeding, the
pregnant woman would be entitled to free,
court-appointed counsel, and all proceedings would be
589
kept confidential. In assessing the best interests of a
minor seeking an abortion, I must assume that any court
would rely heavily on the best medical judgment of the
petitioner’s physician. I continue to feel that this
provision is reasonable and consistent with traditional
and legal parental responsibilities for the welfare of their
minor children, and with the traditional role the courts
have played in determining the best interests of minor
children. At no time is a minor more likely to need or
stand to benefit from the guidance and support of a
responsible adult than when facing the emotional trauma
and dilemma of an unwanted pregnancy. Moreover, the
justification for such guidance is certainly as compelling
in the case of an abortion as that of current consent
requirements for such comparatively routine surgical
procedures as the removal of an appendix or tonsils.
This bill would require that any abortion after the
first trimester of pregnancy be performed in a hospital,
although not necessarily on an in-patient basis. Of all
abortions performed last year in this state, 94.4 percent
were performed during the first trimester. Abortions
performed beyond that period are more likely to entail
greater risks, complications and care. I believe this
provision represents a reasonable and responsible
precaution.
The bill would require certain precautions to help
ensure the survival of an aborted fetus which was viable.
Where a physician has determined prior to an abortion
that the fetus is, in fact, viable, an abortion could only be
performed upon a determination by the woman’s
physician that the abortion was necessary to preserve her
life or health, and then, to the extent medically feasible,
by the method most likely to preserve the viability of the
fetus. I am advised that this is already the case pursuant
to current normal medical practice.
The bill would require the presence of a second
590
physician to attend to the fetus should it be aborted
alive. If a fetus is capable of living and growing outside
the womb, it is difficult for me to accept that it does not
embody a human life. If we are to regard ourselves as a
humanitarian society, I believe that we must take every
reasonable precaution in favor of the preservation of
innocent life. I do believe these precautionary provisions
to be reasonable and responsible.
While protecting the identities of individuals seeking
abortions, physicians performing abortions, and those
associated with facilities providing abortion, this bill does
require that reports be filed with the state Health
Department regarding abortions.
I believe that these reporting requirements are
reasonable and could provide the kind of data that would
be beneficial in enabling us to make more informed
judgments about the continuing questions related to the
matter of abortion. Indeed, 30 other states have enacted
legislation with these types of reporting requirements.
Twenty-two other states have enacted laws
comparable to Senate Bill 439, without evidence of the
extreme effects predicted by both proponents and
opponents of this measure.
I recognize that there is a legitimate difference of
opinion, and, in some cases, a conflict among courts,
over the constitutionality of some of these provisions --
most notably, the waiting period and parental consent
requirements. While I believe firmly that issues such as
this, which touch upon questions of life itself, must be
resolved as a matter of conscience and conviction, I also
recognize that, as Governor, I have an obligation to
reject legislation which is patently unconstitutional. I do
not, however, feel that I must undertake to resolve all
possible Constitutional contentions in evaluating
legislation. This is the province of the courts.
In this regard, I note that the U.S. Supreme Court
591
has agreed to review a number of lower court decisions
on statutes related to abortion and thus to provide final
and definitive judgments on the constitutionality of a
number of state laws which encompass virtually all of the
provisions in the measure now before me about which
questions have been raised. The bill before me would
not take effect for six months. Thus, it is highly likely
that the Supreme Court will provide clear guidance for
all the states in this area before this bill would take
effect. Obviously, any provisions in this bill which are
inconsistent with the determination about to be made by
the Supreme Court could not and would not take effect.
With that understanding, and consistent with my
convictions on this issue as explained in my message of
December 23, 1981, I am herewith signing this bill.
N _________________________
Dick Thornburgh
Governor
592
Plaintiffs’ Exhibit 62:
Veto Message to Pennsylvania House
of Representatives on H.B. 1130
of Governor Robert Casey
(Dec. 17, 1987)
December 17, 1987
TO THE HONORABLE THE HOUSE OF
REPRESENTATIVES OF THE COMMONWEALTH
OF PENNSYLVANIA
I am returning without my approval House Bill 1130,
Printer’s No. 2546, entitled "AN ACT amending Title 18
(Crimes and Offenses) of the Pennsylvania Consolidated
Statutes, limiting the defense of justification in certain
cases; PROVIDING FOR DISTRICT ATTORNEYS’
STANDING AND INTEREST IN PRISONER
LITIGATION; adding provisions relating to the
establishment and operation of the Pennsylvania
Commission on Sentencing; REGULATING MATTERS
RELATING TO THE PERFORMANCE AND
FUNDING OF ABORTIONS, THE PROTECTION OF
WOMEN WHO UNDERGO ABORTION AND
THEIR SPOUSES, AND THE PROTECTION OF
CHILDREN SUBJECT TO ABORTION; increasing the
penalties for false reports to law enforcement authorities;
making an editorial change; and making repeals."
I was elected Governor of Pennsylvania to carry out
the pledges I made to the people of this Commonwealth,
and I will not break faith with those people, or break my
promises to them. I have stated repeatedly that I am
opposed to abortion on every moral ground. I believe
that our society must not tolerate the destruction of
593
human life, and that we have a moral obligation to work
to end this tragedy. This legislation, if corrected in the
manner discussed below, will provide us with an
opportunity to take a step forward in limiting this
destruction.
In its present form, however, I have concluded that it
is not constitutional and that I must veto it. But I
strongly reaffirm today my commitment to joining with
the clear majority of the Legislature who voted for this
bill, and the majority of Pennsylvanians who voted for
me on the basis of my clearly stated agenda for this
state, to sign into law the strongest possible measure
controlling abortion consistent with the Constitution and
my oath to it.
There are two considerations that the gubernatorial
role in the process compels me to interject into the
legislation at this point. These two concerns intersect.
The first is simply this: In order to ensure that the
measures we adopt actually take effect and contribute to
the reduction and someday, I hope, the elimination of
abortions in our state, they must be not only
well-intentioned but well-drafted and able to withstand
the constitutional challenges that will be mounted against
them.
The second consideration may be just as simply
stated: I promised the people of Pennsylvania, and I
took an oath, that I would uphold the Constitution. The
legitimacy of our system of government, the finest on
earth, depends not just upon our pursuit of the moral
good, but also upon our adherence to the rule of law.
Our law, and my oath as Governor, require that I
execute those laws -- including the Constitution -- as
interpreted by the courts, until such time as we are
successful, through the democratic process, in changing
the courts or the law they interpret.
These tasks are not ones that I take lightly. I would
594
do both the people, and the values I cherish and seek to
promote, a grave disservice were I not to give them my
fullest attention and care. Given the magnitude of the
issue, and its importance to so many Pennsylvanians, I
have taken it as a solemn duty to review this matter, and
the state of the law, in considerable depth. The adoption
of concrete, final language by the Legislature enabled
me, beginning last week, to undertake a comprehensive
study of that language and the United States Supreme
Court’s rulings on the subject of abortion. I have
wrestled continuously over the past few days with each of
the questions potentially raised by the state of the law
and its application to this bill. It is only after this
searching analysis that I am ready to discuss this
legislation fully with the Legislature and the people of
this state.
A few sections of the bill call for our particular
attention. The first of these is the informed consent
provision that would be included in Section 3205 of the
new law. The United States Supreme Court has ruled
that a state cannot prohibit a physician from delegating
to another qualified individual the counseling task in the
informed consent context. The wording of the proposed
Section 3205 is, however, potentially ambiguous on that
point, and may possibly be read by some as requiring
that counseling be carried out only by the performing or
referring physician.
I do not believe that the legislation suffers from such
a constitutional defect, however. When read in pari
materia with the Medical Practice Act of 1985 governing
all medical procedures in the Commonwealth, it is clear
that, absent an express legislative declaration otherwise,
physicians may delegate the functions in question to
individuals qualified to perform such counseling. A
statute is to be read so as to render it constitutional, and
with such a reading Section 3205 is constitutional. I
595
therefore believe that this section of the bill must be so
construed and thus passes constitutional muster.
Section 3209 requires that, except as provided in that
section, before an abortion may be performed the
woman must verify that she has notified the child’s father
of her decision to seek an abortion. To the extent that
our law continues to allow the termination of the
procreative process once set in motion, a decent society
ought to do everything possible to promote participation
and prudence in that decision by both the mother and
father.
The Supreme Court has consistently adhered to a
legal framework established in Roe v. Wade, and which
may be summarized as follows: The right to obtain an
abortion is derived from the right of privacy. This right
of privacy protects various facets of an individual’s life
against government intervention and surveillance. While
some of the concerns that give rise to this right of
privacy grow out of such contexts as marriage,
procreation, family relationships, and child-rearing - all
of which involve more than one individual -- the right of
privacy is an individual right, accruing to each and every
person individually and beyond the reach of the state. It
was on this basis that the Court struck down a
requirement that a woman obtain her spouse’s consent
before she could undergo an abortion.
Other rulings by the Court have declared that a state
may not compel disclosure of information protected by
an individual’s right of privacy to any third-party; that a
state lacks a legally justifiable interest in simply knowing
the identity of a woman seeking an abortion; and that a
state cannot intervene in the marital relationship to
dictate the relations between husband and wife. In
striking down spousal consent requirements, the Court
held that a state cannot delegate to any third-party -
even a husband -- a power that the state cannot exercise
596
itself.
Moreover, in the one context in which the Court has
upheld the involvement of others in an individual
abortion decision - parental consent and notice laws
regulating minors seeking abortions -- the Court has
permitted states to require such involvement only as a
mature substitute for an immature minor’s decision. The
Court has mandated that a mature minor must be able
to pursue an abortion without parental consent, or even
notice. The case law makes plain that the Court treats
consent and notice requirements equivalently in regard
to their impingement upon the individual exercise of the
abortion decision to which the Court has extended
privacy protection.
I strongly disagree with this reasoning as a matter of
morality, wisdom, and constitutional interpretation. My
duty, however, requires me to pursue our objectives
within the Constitution. The Supreme Court’s decisions
make it clear that the paternal notice requirement will
be struck down as unconstitutional if enacted. Moreover,
every state statute requiring merely spousal notice that
has been taken before a federal court has been struck
down. I am forced to conclude that this provision poses
the almost certain and unacceptable prospect of
invalidation, and costly, unsuccessful, and avoidable
litigation.
In addition, Section 3214, which requires the
reporting of information to the Department of Health,
remains substantially unchanged from the version
summarily struck down by the Supreme Court less than
two years ago. The Court has indicated that the
government has a sustainable interest in the collection of
health-related data in the abortion control context.
However, where information concerning identifiable
individuals is maintained by the government, sufficient
safeguards against its release must exist under the law;
597
the government must, of course, have a legitimate
health-related concern for knowing the specific identity
of the individuals to whom that data pertains. In its
Thornburgh decision striking down this Section, the Court
explicitly found substantial portions of the data required
under the Act not to be health-related and therefore to
be constitutionally infirm.
While eliminating the public copying provision that
the Court struck down, the bill as drafted neither
provides the types of confidentiality safeguards required
and which are utilized for other sensitive health data, nor
excludes any of the data — such as method of payment,
the woman’s personal history, and the bases for medical
judgment -- that the Court specifically singled out as
unwarranted. In that light, the provision unnecessarily
invites invalidation and would not represent responsible
legislation.
Finally, I must note that our concerns cannot end
with protecting unborn children, but must extend to
protecting, and promoting the health, of all our children,
and their mothers. The right to life must mean the right
to a decent life. Our concern for future mothers must
include a concern for current mothers. Our respect for
the wonders of pregnancy must be equaled by a
sensitivity to the traumas of pregnancy. This
Administration has called for significantly increased
support for child and maternal health programs, for
education, for rape counseling and support services. And
we will continue to advance more programs born of the
recognition that our moral responsibility to mothers and
children does not end at birth. Those proposals deserve
to receive the same overwhelming vote of approval in
the Legislature that this bill received.
Let me restate in summary the distinction between
personal belief and constitutional duty as it applies to
this legislation. I believe abortion to be the ultimate
598
violence. I believe strongly that Roe v. Wade was
incorrectly decided as a matter of law and represents a
national public policy both divisive and destructive. It
has unleashed a tidal wave that has swept away the lives
of millions of defenseless, innocent unborn children. In
according the woman’s right of privacy in the abortion
decision both exclusivity and finality, the Supreme Court
has not only disregarded the right of the unborn child to
life itself, but has deprived parents, spouses, and the
state of the right to participate in a decision in which
they all have a vital interest. This interest ought to be
protected, rather than denied, by the law. This policy
has had, and will continue to have, a profoundly
destructive effect upon the fabric of American life. But
these personal beliefs must yield to the duty, imposed by
my oath of office, to follow the Constitution as
interpreted by the Supreme Court of the United States.
In light of these conclusions imposed upon me by my
oath and obligation as Governor, I am returning this bill
to the Legislature without my signature, for revision
along the lines indicated. Most importantly, I emphasize
again that we must — and we will - enact a strong and
sustainable Abortion Control Act that forms a humane
and constitutional foundation for our efforts to ensure
that no child is denied his or her chance to walk in the
sun and make the most out of life. I will sign this bill
when it reaches the end of the legislative process and
attains those standards.
N
Robert Casey
Governor
599
Plaintiffs’ Exhibit 67:
Excerpts from The Federal Role
in Determining the Medical and
Psychological Impact o f Abortion on Women,
H.R. Rep. No. 392, 101st Cong., 1st Sess. (1989)
THE FEDERAL ROLE IN DETERMINING THE
MEDICAL AND PSYCHOLOGICAL IMPACT OF
ABORTION ON WOMEN
[6] Although CDC researchers have concluded that
abortion is generally safe, Dr. Willard Cates, Jr., and Dr.
David Grimes, both former directors of the CDC
Abortion Surveillance Branch, have re[7]ported that the
earlier an abortion is performed, the safer it is for the
woman.31 For example, Dr. Cates and Dr. Grimes
reported that the risk of death to the pregnant woman
obtaining an abortion doubles for every two weeks’ delay
after eight weeks of gestation.32 However, they
concluded that "once pregnant, a woman encounters an
increased risk of death, no matter what her choice of
outcomes," and that before 16 weeks gestation, legal
abortion is safer than any other alternative outcomes.33
In concluding that abortion does not cause long-term
31 Cates, W., Jr. and Grimes, D A . (1981). Morbidity and Mortality
of Abortion in the United States, in Hodgson, J.E. (Ed.) Abortion and
Sterilization: Medical and Social Aspects. London: Academic Press
Inc., p. 158; in subcommittee files.
32 Ibid., p. 171.
33 Ibid., p. 170.
600
health problems, the Surgeon General’s draft report
apparently rejected the medical reports that linked
abortion to later reproductive hazards. Similarly, CDC
researchers have criticized some of the research
presented as evidence of medical problems resulting
from abortion as having obvious methodological flaws.34
For example, the National Right-to-Life Committee
presented the subcommittee with a chapter written by
Matthew J. Bulfin from New Perspectives on Human
Abortion as evidence of the dangers of abortion.35 In
the chapter, Dr. Bulfin, a physician in private practice,
documented the number of patients who came to him
with infections, anxiety, and other problems resulting
from a prior abortion. He concluded that 159 (20
percent) of 802 abortion patients that he saw had suf
fered from serious complications (including marital
break-up).
CDC researchers have stated that it is not
scientifically appropriate to assume that these kind of
statistics are representative of abortion patients, since
Dr. Bulfin’s patients apparently came to see him because
they had medical problems.36 The weakness of these
statistics is that they do not compare the number of
abortion patients with problems to the total number of
women who have had abortions. Therefore, when a
34 Cates, W., Jr. (1979). Late effects of induced abortion, Journal of
Reproductive Medicine, Vol. 22, pp. 207-212.
Bulfin, M.J. (1981). Complications of Legal Abortion: A
Perspective From Private Practice, in Hilgers, T.W., Horan, D.J., and
Mall, D. Frederick, MD: Altheia Books, pp. 145-150; available in
subcommittee files.
36 This kind of research was criticized in: Cates, W., Jr. (1979). Late
effects of induced abortion: Hypothesis or knowledge? Journal of
Reproductive Medicine, Vol. 22, pp. 207-212.
601
study is based on patients seeking treatment in one
doctor’s office, it is considered anecdotal data, rather
than scientific research. Dr. Koop rejected anecdotal
evidence as unscientific in his review of the medical
evidence.37 Moreover, studies reported in book
chapters, such as Dr. Bulfin’s, are not peer reviewed by
scientists, and are therefore not considered scientific
evidence.38 * * * * * *
* * *
[10] In their review paper presented to the Surgeon
General, the American Psychological Association
concluded that, despite the flaws in the research, there is
so little evidence of psychiatric problems following
abortion, and so much evidence of relief, that therefore
abortion does not cause more psychiatric problems than
unwanted pregnancy.53 They also argued that given the
large number of abortions, any significant psychiatric
problems would have become very obvious to the mental
health system in the last 15 years.54 Dr. Henry David,
who represented the American Public Health Association
in his meetings with Dr. Koop and in his Congressional
testimony, acknowledged that some women have psychi
atric problems following abortion. However, his research
37 Hearing, testimony of Dr. C. Everett Koop, p. 232.
38 Hearing, testimony of Dr. Jaroslav F. Hulka, pp. 3, p. 331.
Testimony on the Psychological Sequelae of abortion, on behalf of
the Public Interest Directorate of the American Psychological
Association, presented to the Office of the U.S. Surgeon General,
December 2, 1987, pp. 25, 29; document available in subcommittee
files.
54 Ibid. p. 3.
602
results indicate that the numbers are small, and there is
no conclusive evidence that those psychiatric problems
necessarily resulted from the abortion itself, rather than
from the breakup of the relationship (which resulted in
the unwanted pregnancy) or other factors.55 *
* *
[11] The National Right-to-Life Committee "white
paper" also summarized the psychological research and
concluded that the evidence was unclear but possibly
showed more negative effects for abortion compared to
maintaining the pregnancy.
One major study quoted by both the pro-choice
advocates and the anti-abortion advocates helps illustrate
the controversies. Dr. Henry David conducted a study of
more than one million women in Denmark, to determine
whether women who had obtained abortions 3 months
earlier were more likely to be treated in psychiatric
hospitals than were women who have given birth 3
months earlier or women who had not been pregnant.
Dr. David’s research was cited as one of the best
studies of the psychiatric impact of abortion by the
Right-to-Life white paper and by pro-choice
advocates.62 Dr. David reported that approximately 12
women per 10,000 abortions or deliveries were
hospitalized, compared to 7 per 10,000 for all women of
reproductive age. He also reported that separated,
divorced, or widowed women who obtained abortions
were much more likely to be hospitalized in a psychiatric
facility than divorced, separated or widowed women who
give birth, perhaps because it "may have been an
55 Hearing, testimony of Dr. Henry David, p. 144.
Hearing, testimony of Dr. Wanda Franz, p. 144.62
603
originally wanted pregnancy."63
In contrast, the Right-to-Life white paper
misrepresented this study, quoting statistics for divorced,
separated, and widowed women having abortions (63.8
per 10,000) as if they applied to all women having
abortions. When asked to explain this error or mis
representation, Dr. Wanda Franz, vice president of the
National Right-to-Life Committee, testified "The issue
here is that the direction of the findings are that those
women who had abortions had higher rates" and
speculated that the abortion decision may have caused
the breakup of the relationship.64 She did not answer
the question of why the psychiatric rates that applied to
the less than 10 percent of the women who were
divorced, separated, or widowed were incorrectly cited as
if they applied to all of the more than 27,000 women
who had obtained abortions.65
The major focus of the "white paper" was a meta
analysis, which is a statistical comparison that includes
the data from several previously conducted research
studies. The white paper was the one [12] new research
paper for which Dr. Koop and his staff requested de
tailed criticisms. The paper was vehemently criticized by
CDC scientists and other researchers who were asked to
review the quality of their scientific evidence. For
example, scientists at the Center for Health Promotion
and Disease Prevention at CDC reported the following
63 Hearing, testimony of Dr. Henry David, p. 97.
64 Hearing, testimony of Dr. Wanda Franz, pp. 144-145.
65 The statistics are clearly presented in the published article, which
was reviewed by the Surgeon General and his staff: David, H.P.,
Rasmussen, N.K., and Holst, E. (1981). Postpartum and postabortion
psychotic reactions, Family Planning Perspectives, Vol. 13, pp. 88-93.
604
problems with the meta-analysis:
"1. The authors combine outcomes that are not
well defined and are probably not comparable;
"2. The comparison groups used in the studies
that were analyzed are inappropriate;
"3. The analysis was based on studies that,
according to the authors of the report, are largely
flawed as to design and methodology; and,
"4. The authors’ assumptions] . . . cannot be
justified from the data."
The CDC scientists concluded that "Since the meta
analysis used a combination of studies with disparate
results, the conclusions based on such analysis have little
value."66
Scientists from the National Center for Health
Statistics who were asked to review the white paper for
the Surgeon General concluded that "the meta-analysis
has no value" and that "The conclusions drawn by the
authors seem to be based on a priori beliefs rather than
on objective review of the evidence."67
* * *
[14] For example, in his meeting with the American
Council on Science and Health, Dr. Koop stated ". . .
there is no doubt in my mind that there are physical
effects of abortion and mental effects of abortion. They
are, I think, a very tiny percentage of the number of
people that are aborted. . . . I don’t think there is any
way that one could do an honest report and come up
with such overwhelming statistics that you could use it as
66
67
This review document is in Hearing, pp. 151-155.
Hearing, p. 156.
605
a weapon against abortion itself."83 Similarly, in his
meeting with the National Organization of Episcopalians
for Life, he stated "The problems that truly present
health problems are someplace down here. They’re
quite minuscule."84
* * *
83 Transcript of meeting of Dr. C. Everett Koop with the American
Council on Science and Health, February 4, 1988, p. 7.
M Transcript of Dr. C. Everett Koop’s meeting with the National
Organization of Episcopalians for Life, March 31, 1988, p. 8; available
in subcommittee files.
606
Plaintiffs’ Exhibit 89:
Diagnostic Criteria for
Post-Traumatic Stress Disorder
A. The person has experienced an event that is outside
the range of usual human experience and that would
be markedly distressing to almost anyone, e.g.,
serious threat to one’s life or physical integrity;
serious threat or harm to one’s children, spouse, or
other close relatives and friends; sudden destruction
of one’s home or community; or seeing another
person who has recently been, or is being, seriously
injured or killed as the result of an accident or
physical violence.
B. The traumatic event is persistently reexperienced in
at least one of the following ways:
(1) recurrent and intrusive distressing recollections
of the event (in young children, repetitive play in
which themes or aspects of the trauma are
expressed)
(2) recurrent distressing dreams of the event
(3) sudden acting or feeling as if the traumatic event
were recurring (includes a sense of reliving the
experience, illusions, hallucinations, and
dissociative [flashback] episodes, even those that
occur upon awakening or when intoxicated)
(4) intense psychological distress at exposure to
events that symbolize or resemble an aspect of
the traumatic event, including anniversaries of
the trauma
C. Persistent avoidance of stimuli associated with the
trauma or numbing of general responsiveness (not
present before the trauma), as indicated by at least
three of the following:
(1) efforts to avoid thoughts or feelings associated
607
with the trauma
(2) efforts to avoid activities or situations that
arouse recollections of the trauma
(3) inability to recall an important aspect of the
trauma (psychogenic amnesia)
(4) markedly diminished interest in significant
activities (in young children, loss of recently
acquired developmental skills such as toilet
training or language skills)
(5) feeling of detachment or estrangement from
others
(6) restricted range of affect, e.g., unable to have
loving feelings
(7) sense of a foreshortened future, e.g., does not
expect to have a career, marriage, or children, or
a long life
D. Persistent symptoms of increased arousal (not
present before the trauma), as indicated by at least
two of the following:
(1) difficulty falling or staying asleep
(2) irritability or outbursts of anger
(3) difficulty concentrating
(4) hypervigilance
(5) exaggerated startle response
(6) physiologic reactivity upon exposure to events
that symbolize or resemble an aspect of the
traumatic event (e.g., a woman who was raped in
an elevator breaks out in a sweat when entering
any elevator)
E. Duration of the disturbance (symptoms in B, C, and
D) of at least one month.
Specify delayed onset if the onset of symptoms was at
least sue months after the trauma.
608
EXCERPTS FROM VERIFICATIONS FILED IN
SUPPORT OF PLAINTIFFS’
PRELIMINARY INJUNCTION MOTION
Excerpts from Verification of Sue Roselle
(Apr. 18, 1988)
VERIFICATION OF SUE ROSELLE
* * *
6. WHS provides approximately 11,800 free
pregnancy tests and 7,600 first and early second trimester
abortions each year. The abortion procedure costs as
follows: $275 if twelve weeks or less from the last
menstrual period; $375 if thirteen to fourteen weeks
from the last menstrual period; and $500 if fifteen to
sixteen weeks from the last menstrual period. The fee
includes the abortion procedure, laboratory testing,
personal counseling including contraceptive care,
pathological examination and medical supervision during
the post-surgical recovery period.
7. If our clients are eligible for medical assistance,
WHS takes the necessary information and seeks
reimbursement from the Commonwealth. Medical
assistance is available only where the abortion is
necessary because of a life-threatening condition, or
because the patient was a victim of rape or incest. In
1987, WHS was reimbursed for 249 such abortions.
Where a client receives medical assistance from the
state, but is not eligible for medical assistance for an
abortion, WHS nevertheless will discount the cost of the
abortion. Last year WHS accomodated 1,470 clients who
were unable to pay the full amount. WHS has never
turned away any client seeking an abortion merely
because of inability to pay.
609
* * *
9. Our patients come primarily from Allegheny
County. In 1987, however, 761 of our abortion patients
came from areas in excess of two hours traveling time
(100 miles) from the clinic.
* * *
11. When they present themselves at the clinic, if
indicated, women are examined by a nurse practitioner
or physician’s assistant and everyone receives a
pregnancy test and blood tests. In addition, all women
are required to have an individual interview with a
counselor on the day their abortion is to be performed.
These interviews routinely last twenty minutes to an
hour. During this interview, a woman is counseled with
respect to her options and her decision to have an
abortion. In that connection, the counselor seeks to
ensure that the woman is not unduly ambivalent about
her decision and that she is not being coerced. In
addition, the counselor discusses future contraceptive use
with the patient. If the patient appears ambivalent about
her decision, the counselor will refer her to one of our
staff therapists and the abortion will be rescheduled to
give the patient more time to consider her options. On
occasion, the clinic will refuse to perform the abortion if
convinced of a patient’s continued ambivalence. This is
rare, however, because the great majority of our patients
have absolutely decided to have an abortion before
seeking medical care.
* *
20. In general, WHS supports and encourages
parental involvment in the abortion decision where
610
possible.
21. Under Section 3206, WHS will require the
presence of a parent in order to give counseling to that
parent sufficient to assure the parent is able to give his
or her informed consent. We foresee no circumstances
in which we would secure parental informed consent
over the telephone, by mail, or means other than by an
in-person visit to our clinic. This, in turn, may cause
serious delays in the abortion even in cases where the
parent is prepared to consent. Many parents will find it
difficult to come to the clinic for the necessary
counseling because of their work schedules, illness or
other commitments.
22. The implementation of the parental consent
requirement will cause administrative and scheduling
nightmares inasmuch as at present, we normally do
parental counseling on the day of the abortion
procedure, which are performed only three days a week.
* * *
24. Some parents may not be able to come to the
clinic for many days, or possibily even weeks, after their
minor daughter has decided to seek an abortion. This
would be true even in cases where the parent fully
consents to the minor’s having an abortion. The
resulting delay caused by this could be both dangerous
and prohibitive since most minors decide to have an
abortion much later in their pregnancies than adults.
25. The additional costs incurred for minors and
their parents who must come long distances -- whether
together or separately -- could also be extremely
burdensome and may result in the minor’s effectively
being deprived of her right to have an abortion.
26. Another problem with Section 3206 is that it
does not state what procedures and documentation are
611
necessary for obtaining legally valid parental consent.
Thus, because this section is so vague and uncertain,
WHS will have to be extremely conservative in deciding
on the kind of identification that will be required from
the parent, resulting in further delay of the abortion
procedure. If the parent does not have the proper
documentation of parentage, the abortion would have to
be rescheduled.
27. WHS also is greatly concerned about the effect
the parental consent and judicial bypass provisions will
have on minors themselves. Adolescents as a group are
reluctant to establish contact with unfamiliar
organizations. It is a difficult enough chore to call the
clinic. The additional burden of being forced to go to a
parent when reluctant to face a court may have one of
several disastrous results for the adolescent: (a) the teen
will come in later for her abortion because of the greater
time it will take her to resolve the higher level of fear
and confusion created by the legal requirements. The
later she has an abortion, the more likely she is to have
complications; (b) the teen will tell no one until the
pregnancy is so advanced that someone else finally
confronts her. The parents and teen may then have no
options because the advanced stage of the pregnancy at
this time precludes an abortion; (c) the teen will attempt
a self-induced or illegal abortion with resulting
permanent damage to her reproductive system or death;
(d) the teen will run away from home; or (e) the
situation will be deemed unresolvable by the teen and
suicide will be viewed as the only escape. (Adolescents
have been documented to have one of the highest suicide
rates of any segment of the population).
28. Sections 3207(b) and 3214(f) will require WHS,
respectively, to file annual reports identifying our facility
and quarterly reports showing the total number of
abortions performed per trimester of pregnancy. Under
612
the Act, these reports, if filed by facilities receiving any
state-appropriated funds, will be open to public
inspection.
29. WHS does receive state-appropriated funds in
the form of state medical assistance funding for the
victims of rape and incest and for patients whose
pregnancy must be terminated because of physical
conditions that are life-threatening. Additionally, WHS
receives federal funds that are appropriated by the state
for the purpose of counseling and testing clients who are
in high risk groups for exposure to the Human
Immunodeficiency Virus (HIV), the precursor of AIDS.
30. Inasmuch as WHS does receive state-
appropriated funds, we are extremely troubled that our
reports will be open for public inspection and copying.
Over the years, WHS has been the target of continued
harassment and violence by anti-abortion groups. On
many occasions we have discovered anti-abortion
advocates going through our trash to find any scraps of
information they might put to use. Public disclosure of
the information filed in the reports required by the Act
is certain to enhance the frequency and intensity of the
harassment and violence. In turn, women will be further
intimidated from using our clinic for fear of being
subjected to verbal and physical abuse. The intimidation
deters all of our clients, and not just those pursuing their
legal right to have an abortion. Many women intending
to have an abortion in our clinic have also told me of
their fear that the procedure itself will be interrupted by
demonstrations, bomb scares and similar activities.
Finally, such anti-abortion activities adversely effect the
ability of WHS to operate its business and offer its
services to the public.
31. In addition, Sections 3207(b) and 3214(f) provide
that confidentiality of the required reports is conditioned
upon whether a facility has received state-appropriated
613
funds within the 12-month period preceding the filing of
the report. The retroactivity of this provision is
disturbing to WHS because, at least with respect to
reports we must file during the coming year, we have
been deprived of a choice of whether to protect the
confidentiality of our records no longer accepting state-
appropriated funds. In 1987, WHS received medical
assistance reimbursement for the treatment of only 249
patients. Had we known that receipt of such a relatively
small amount of money would threaten the
confidentiality of WHS records, we may well have
decided to discontinue accepting medical assistance.
Similarly, it was only in March of 1988 that WHS
contracted for state-appropriated federal funding of HIV
testing and counseling. Before that time WHS had been
offering HIV testing and counseling for a small fee. Had
we known of the confidentiality implications of our
accepting the federal funds, we may have decided not to
enter into the contract.
* *
34. The identification of facilities in Department
reports is certain to open the door to increasing
anti-abortion harassment and violence. In addition,
some of the information that is required to be reported,
coupled with the Department’s right to identify facilities,
exacerbates the risk. For example, under 3214(h), all
physicians are required to report complications that they
judge to have resulted from an abortion or attempted
abortion. The definition of "complication" is vague; and
the reporting requirment could permit physicians to
exploit, abuse, or even inadvertently misconstrue the
complications reporting procedure to the derogation of
facilities such as WHS.
35. The second grave risk of section 3214 is the risk
614
posed by the requirement that the names of all referring
and performing physicians must be reported to the
Department. I can state with complete certainty that
because of the harassment and violence directed toward
physicians who refer or perform abortions procedures,
WHS will lose many of its referring physicians and
possibly some of its performing physicians if this section
goes into effect.
36. Many of our referring physicians in particular,
are extremely protective of their anonymity because of
legitimate fears (often based on past experience) that any
kind of documentation or record-keeping connecting
them with any phase of the abortion decision could cause
them to lose their medical practice, hospital and other
professional privileges, as well as the ability to reside in
their communities peacefully and without harassment.
37. For example, I personally know two medical
doctors who, although they do not perform abortions, do
refer clients to WHS for abortions on the strict condition
that we not use their names in any WHS reports. They
insist upon this because in the past, each has been
subjected to public abuse, picketing and pamphleteering
based on their having performed or referred abortions
during their medical residencies. Each of these doctors
has told me emphatically that under no circumstances
would he refer any abortions to WHS or any other clinic
under the new Act — even if there were no risk of public
disclosure at all. The mere requirement that their names
appear on reports filed with a Commonwealth agency is
sufficient, based on their past experience, to deter them
from making any future referrals.
38. The net effect of this will be that women will be
unable to find physicians willing to refer or to perform
abortions for them, which in turn, operates to deny them
their right to choose to have an abortion.
* * *
615
Excerpts from Verification of
Sylvia Stengle (Apr. 18, 1988)
VERIFICATION OF SYLVIA STENGLE
* *
7. For patients who receive medical assistance from
the Commonwealth, AWC’s fee for an abortion is $195.
In the case of those medical assistance patients who
require an abortion because of a life-threatening disease
or because they were victims of rape or incest, AWC --
in the past -- has received reimbursement from the state,
so that no fee was charged directly to the patient. The
amount involved is relatively small. In 1987, AWC
received less than $4,000 in medical assistance funds.
8. With the passage of this Act, AWC has decided
to stop taking medical assistance funds from the state
immediately.
* *
10. Our patients come primarily-from an 18-county
area in northeastern Pennsylvania encompassing the
counties of Lehigh, Northampton, Carbon, Schuylkill,
Luzerne, Lackawanna, Lebanon, Berks, Bucks, Pike,
Chester, Lancaster, Susquehanna, Wayne, Monroe,
Montgomery, Columbia and Wyoming. Many of these
counties have no local services available to women
seeking abortions, AWC being the closest facility to
which the women can turn. In 1987, 138 (3.26%) of our
abortion patients came from areas in excess of two hours
traveling time (100 miles) from the clinic; 1,220 or 29%
came from areas in excess of lh hours traveling time (75
miles); and 2,276 or 54% came from areas in excess of 1
616
hour traveling time (50 miles).
* * *
17. If the patient appears ambivalent about her
decision to have an abortion, the counselor will review
options and suggest that the patient take more time to
consider her decision before terminating the pregnancy.
On occasion, the clinic has refused to permit an abortion
if, after consultation, the counselor and the clinic
supervisor are convinced of the woman’s extreme
ambivalence, coercion, or that she is otherwise overly
distraught. Sometimes, we will refer these women to
outside counselors. Such instances are infrequent,
however, because the great majority of our patients have
absolutely decided to have an abortion before making an
appointment here.
* * *
24. Section 3206 requires that in order for a minor
who is less than 18 years old and not emancipated to
obtain an abortion, either one parent must give his or
her informed consent to the abortion, or the minor must
go through a judicial bypass procedure. This is certain to
cause dangerous delays which could effectively deprive
many minors of their right to have an abortion. Often,
minors are overwhelmed by the prospect of involving
parents because of fears of retaliation or rejection by the
parents. Even where parents are involved and willing to
consent, they may have scheduling problems making it
difficult for them to come to the clinic.
25. Under the parental consent provision of the Act,
AWC will have to insist upon a personal visit to the
clinic by a parent so that we can give the counseling
necessary to assure that the parent’s (and minor’s)
617
consent is informed. Normally, we will want the parent
and daughter to come together for counseling, although
this will not always be possible.
26. Requiring a consenting parent to come to the
clinic for counseling and consent will most certainly
cause serious delays -- even in cases where a parent is
willing to consent. Many parents will find it difficult to
visit the clinic because of work schedules, illness,
burdensome travel distances and costs, or other
commitments.
* * *
28. Some parents may not be able to get to the
clinic for days, even weeks, after the daughter has
decided to seek an abortion. Ensuing delays could be
both dangerous and prohibitive since it is
well-documented that minors as a group decide to have
abortions much later in their pregnancies than do adults.
29. The likelihood of dangerous delay is particularly
great in our part of the state because AWC services such
a large (18-county) area. Furthermore, travel time and
costs for minors and their parents will surely increase in
cases where the parent and minor will not be able to
come for joint counseling on the day of the procedure,
the delay and costs will be even greater.
30. An antecedent, and perhaps more serious delay
arises from the minor’s fear and hesitation in divulging to
her parents that: first, she has been sexually active;
second, that she is pregant; and third; that she wishes to
have an abortion. The prospect of the disruption and
trauma erupting from such disclosure may cause the
minor to delay telling her parents for days and even
weeks. It is well-known that the risk of complications
from an abortion increase dramatically with each day’s
delay, particularly after the 10 to 12 weeks gestation
period.
618
31. Another disturbing aspect of 3206 is that it does
not state what procedures and documentation are
necessary for obtaining legally valid parental consent.
This vagueness leaves AWC uncertain as to what we
must require. We are concerned that no matter what
identification procedures we adopt, we may be subject to
civil liability. We are even more concerned about the
penalties to our physicians who may be subject to
suspension or revocation of their medical licenses. In
any event, because the Act fails to provide guidance, we
will be forced to implement stringent documentation
requirements which, in turn, will cause further delays in
the abortion procedure.
* * *
34. Second trimester abortions involve far more risks
of complications than earlier abortions, and each passing
day enhances these risks. At some point, the minor will
suddenly find herself with no options and be forced to
continue the pregnancy. Some will respond by trying to
obtain illegal abortions or by attempting to self-induce an
abortion. Others may resort to suicide. Problem
pregnancy is a leading cause of suicide among adolescent
women. In the past, AWC has had to do suicide
counseling with pregnant minors. The new Act will only
exacerbate the trauma and risks for these young women.
35. AWC is also troubled by sections 3207(b) and
3214(f) of the Act. Under these sections, AWC’s annual
reports (identifying our facility and its affiliates) and
quarterly reports (stating the total number of abortions
performed per trimester of pregnancy) to the
Department of Health will be open for public inspection
and copying as long as AWC receives state-appropriated
funds.
* * *
619
37. During the past 12 months, AWC has received
stateappropriated funds in the form of reimbursements
for services to patients who are under state medical
assistance. We are therefore extremely concerned about
the prospect of our reports having no confidentiality.
Over the years, AWC has been the target of continued
harassment and threats of violence by anti-abortion
groups. These groups are eager to obtain as much
information as possible to fuel their activities. Public
disclosure of the information filed in the reports is
certain to intensify their activities. Women, in turn, will
be even more intimidated from using our clinic for fear
of being subject to verbal or even physical abuse. Too,
anti-abortion harassment severely cripples AWC’s ability
to operate the clinic and offer its services to the public.
Had we known that receipt of a relatively small amount
of state funds would compromise the confidentiality of
AWC’s records, we could have decided to discontinue
accepting state medical assistance as a means of
containing the level of harassment we now endure.
38. As to the future, AWC has decided that with the
enactment of the Act, it will terminate immediately all
receipt of state-appropriated funding so that in 12
months time, the confidentiality of our records can be
protected. This will mean that AWC will have to insist
that patients who are on medical assistance must pay for
our services or else be turned away. Thus, in the final
analysis, it will be poverty-level women who will be the
real victims of the Act.
39. AWC also finds it sadly ironic that while on the
one hand, the Commonwealth reimburses the cost of
abortions for medical assistance patients who were
victims of rape, incest or have life-threatening conditions,
and on the other, it penalizes providers of those
abortions by depriving them of the right of confidentiality
over their records.
620
40. Section 3214(a) sets out additional reporting
requirements including, among other things,
identification of all physicians who refer for, or perform
abortions, and the reporting of complications that may
have resulted from an abortion or attempted abortion.
In addition, Section 3214(e) permits the Department of
Health to issue an annual report based upon this
information, and provides only that the report shall not
lead to the disclosure of the identity of any person filing
a report or about whom the report is filed.
41. These two provisions seriously threaten the
availability of referring and performing physicians to
AWC, and therefore affect its ability to continue
providing services to our patients. Many of our
physicians are highly protective of their anonymity
because of legitimate fears of anti-abortion activities.
Many physicians who would otherwise work for AWC,
will not because of legitimate fears of anti-abortion
harassment, picketing and violence. Likewise, referring
physicians have told me that any kind of documentation -
- even if only state-filed reports not open to the public -
connecting them with any aspect of the abortion decision
could cause them to be subject to harassment in the
communities in which they reside.
42. For example, several of AWC’s present referring
physicians will not permit us to send correspondence to
their offices for fear that members of their own staffs
will divulge to anti-abortion groups that they refer
patients for abortions. One has told me that the new
record-keeping provisions of 3214 would mean that many
doctors will stop referring for abortions altogether.
Thus, patients coming to these doctors for help would
have to go elsewhere for information about AWC or
similar facilities, even though the information is at the
doctors’ fingertips.
43. Another doctor who has performed abortions for
621
AWC in the past has told me that in light of the new
Act, he would not consider working for the clinic any
longer for fear of public exposure and harrassment. At
one time, this doctor had performed abortions in his
private practice but stopped doing so after receiving
threats that anti-abortionists would begin picketing his
home.
44. A third doctor with whom I have spoken, and
who also stopped performing abortions because of
threats from anti-abortionists, has told me that he too
would be unwilling to refer patients to AWC for fear of
reprisal and harassment. He also told me that he
believes the hospitals, in order to preserve the
confidentiality of their records, will stop performing
abortions, and that private doctors who perform
abortions will stop accepting patients on state medical
assistance. This will have serious repercussions for many
women on medical assistance.
45. For example, women with serious health
problems cannot normally go to a clinic to have an
abortion. Rather, they would have to go to a hospital for
the procedure. If the woman is on public assistance,
however, and the doctor and/or hospital refuse to
perform her abortion, the woman will have no options
whatsoever -- other than to lie about her physical
condition so as to secure an abortion at a clinic (and
thereby take the risk of serious medical complications).
These women will be effectively and wholly deprived of
their right to choose to have an abortion.
46. In my opinion, the sole purpose of the Act’s
various reporting requirements, along with the attendant
risks of public disclosure of certain information in these
reports, is to harass and deter physicians and clinics.
* * *
RECORD PRESS, INC., 157 Chambers Street, N.Y. 10007 (212) 619-4949
83365 • 58