Richmond Virginia School Board v Virginia Board of Education Supplemental Brief in Support of Petitions for Writs of Certiorari
Public Court Documents
October 1, 1972
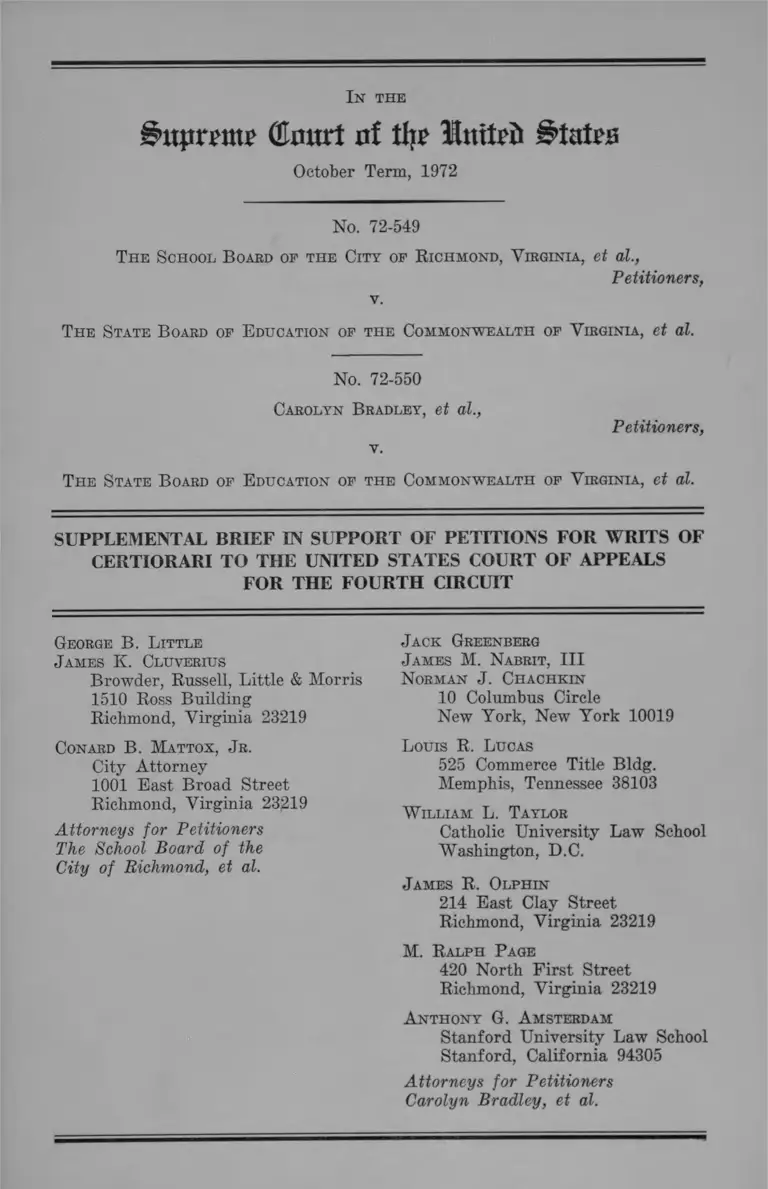
85 pages
Cite this item
-
Brief Collection, LDF Court Filings. Richmond Virginia School Board v Virginia Board of Education Supplemental Brief in Support of Petitions for Writs of Certiorari, 1972. 4272e65b-c29a-ee11-be36-6045bdeb8873. LDF Archives, Thurgood Marshall Institute. https://ldfrecollection.org/archives/archives-search/archives-item/f5360697-67ac-4c78-8b5b-7cf5eac93fef/richmond-virginia-school-board-v-virginia-board-of-education-supplemental-brief-in-support-of-petitions-for-writs-of-certiorari. Accessed February 22, 2026.
Copied!
iatpmtt? (tart of tfy? Htuteii States
October Term, 1972
No. 72-549
The School B oard of the City of R ichmond, Virginia, et al.,
Petitioners,
v.
The State B oard of E ducation of the Commonwealth of Virginia, et al.
No. 72-550
Carolyn B radley, et al.,
Petitioners,
v.
The State B oard of E ducation of the Commonwealth of Virginia, et al.
I n th e
SUPPLEMENTAL BRIEF IN SUPPORT OF PETITIONS FOR WRITS OF
CERTIORARI TO THE UNITED STATES COURT OF APPEALS
FOR THE FOURTH CIRCUIT
George B. L ittle
J ames K. Cluverius
Browder, Russell, Little & Morris
1510 Ross Building
Richmond, Virginia 23219
Conard B. Mattox, J r.
City Attorney
1001 East Broad Street
Richmond, Virginia 23219
Attorneys for Petitioners
The School Board of the
City of Richmond, et al.
J ack Greenberg
J ames M. Nabrit, I I I
Norman J . Chachkin
10 Columbus Circle
New York, New York 10019
Louis R. Lucas
525 Commerce Title Bldg.
Memphis, Tennessee 38103
W illiam L. Taylor
Catholic University Law School
Washington, D.C.
J ames R. Olphin
214 East Clay Street
Richmond, Virginia 23219
M. Ralph P age
420 North First Street
Richmond, Virginia 23219
Anthony G. Amsterdam
Stanford University Law School
Stanford, California 94305
Attorneys for Petitioners
Carolyn Bradley, et al.
1st the
$ttp:ran? (Enurt nf % Itttteii States
October Term, 1972
No. 72-549
T he S chool B oard of th e City of R ichmond,
V irginia, et al.,
P etition ers,
v.
T he S tate B oard of E ducation of the
Commonwealth of V irginia, et al.
No. 72-550
Carolyn B radley, et al.,
P etition ers,
v.
T he S tate B oard of E ducation of th e
Commonwealth of V irginia, et al.
SUPPLEMENTAL B R IEF
IN SUPPORT OF PETITIONS FOR WRITS OF
CERTIORARI TO THE UNITED STATES COURT
OF APPEALS FOR THE FOURTH CIRCUIT
Counsel for petitioners in each of these cases, presently-
pending upon petitions for writs of certiorari, file this
joint supplemental brief pursuant to Rule 24(5) of this
Court. A significant decision of another United States
Court of Appeals has been rendered since the filing of the
2
petitions for writs of certiorari, which conflicts with the
decision of which review is sought by the petitioners, and
which underscores the importance and desirability of
granting review.
On December 8, 1972, the United States Court of Ap
peals for the Sixth Circuit rendered a decision in B rad ley
v. M illiken, Nos. 72-1809, -1814, which affirmed the district
court’s decision to require a plan of desegregation for
Detroit not limited by school district boundary lines, and
upheld the power of the court to fashion such a remedy.
(The district court decision is referred to in note 36 at
page 53 of the Petition in No. 72-549 and in note 122,
page 64 of the Petition in No. 72-550.) The Court of Ap
peals’ opinion in the Detroit case, B rad ley v. M illiken, is
directly contrary to the decision below of which review
is sought. (See the Sixth Circuit’s comment at page 67
of the opinion, declining to follow the Fourth Circuit.)
The decision of the Court of Appeals for the Sixth Cir
cuit is appended hereto.
3
Respectfully submitted,
George B. L ittle
J ames K . Cltjvebius
Browder, Russell, Little
& Morris
1510 Ross Building
Richmond, Virginia 23219
Conard B. Mattox, J r .
City Attorney
1001 E ast Broad Street
Richmond, Virginia 23219
A ttorneys fo r P etition ers
T he School B oa rd o f the
City o f R ichm ond, et al.
J ack Greenberg
J ames M. Nabrit, I I I
Norman J . Chachkin
10 Columbus Circle
New York, New York 10019
Louis R. L ucas
525 Commerce Title Bldg.
Memphis, Tennessee 38103
W illiam L. T aylor
Catholic University Law School
Washington, D.C.
J ames R. Olph in
214 E ast Clay Street
Richmond, Virginia 23219
M. R alph P age
420 North F irs t Street
Richmond, Virginia 23219
A nthony G. A msterdam
Stanford University Law School
Stanford, California 94305
A ttorneys fo r P etition ers
C arolyn B rad ley , et al.
Nos. 72-1809 - 72-1814
UNITED STATES COURT OF APPEALS
FOR THE SIXTH CIRCUIT
Ronald Bradley, et al.,
Plaintiffs-Appellees,
v.
W illiam G. M illiken , Governor of
Michigan, etc.; Board of E duca
tion of the C ity of Detroit,
Defendants-Appellants,
and
Detroit F ederation of T eachers
L ocal 231, American F ederation
of T eachers, AFL-CIO,
Defendant-Intervenor-Appellee,
and
Allen Park Public Schools, et al.,
Defendants-Intervenors-Appellants,
and
Kerry Green, et al.,
Defendants-Intervenors-Appellees.
A p p e a l from the
United States District
Court for the Eastern
District of Michigan,
Southern Division.
Decided and Filed December 8, 1972.
Before Phillips, Chief Judge, E dwards and Peck, Circuit
Judges.
Phillips, Chief Judge. This is a school desegregation case
involving the metropolitan area of Detroit, Michigan.
The present appeal is the fourth time that the case has been
before tills court since the complaint was filed August 18,
2 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
1970. The earlier decisions of this court are reported at Brad
ley v. Milliken, 433 F.2d 897 (1970); Bradley v. Milliken, 438
F.2d 897 (1971); and Bradley v. M illiken,---- F .2 d ----- (1972),
cert, denied, — U.S. — , 41 U.S.L.W. 3175 (Oct. 10, 1972).
(On November 27, 1972 this Court dismissed for want of
jurisdiction an “emergency motion” by the Detroit Board of
Education that State officials be required to provide funds
to keep the Detroit public schools operating for 180 regular
days of instruction during the current school y e a r .---- F.
2 d ---- .)
No specific desegregation plan has been ordered by the
District Court. The procedural history of the litigation is set
forth below.
Before this court at the present time are four interlocutory
orders from which we have granted appeal pursuant to 28
U.S.C. § 1292(b) and one final order, viz:
1. Ruling on Issue of Segregation, dated September 27,
1971, reported at 338 F.Supp. 582;
2. Findings of fact and conclusions of law on “Detroit only”
plans of desegregation, dated March 28, 1972;
3. Ruling on Propriety of a Metropolitan Remedy to Ac
complish Desegregation of the Public Schools of the City of
Detroit, dated March 24, 1972;
4. Ruling on Desegregation Area and Development of
Plan, and Findings of Fact and Conclusions of Law in support
thereof, dated June 14, 1972; and
5. Order dated July 11, 1972, directing Michigan State
officials to purchase 295 school buses (which this court con
siders to be a final order).
On July 13,1972, following oral argument, this court granted
a motion for a temporary stay of the District Court’s order
of July 11, 1972, ordering the purchase of 295 school buses.
On July 17,1972, following oral argument, this court directed
that its stay order remain in effect until entry by the District
Court of a final desegregation order or until certification by the
Nos. 72-1809, 72-1814 Bradley, et al. v. MiUiken, et al. 3
District Court of an appealable question as provided by 28
U.S.C. § 1292(b).
Thereafter the District Court certified that the orders set
forth above involve controlling questions of law, as provided
by 28 U.S.C. § 1292(b), and made a determination of finality
under Rule 54(b ), Fed. R. Civ. P.
On July 20, 1972, this court entered an order granting the
interlocutory appeal concluding that:
“[A]mong the substantial questions presented there is at
least one difficult issue of first impression that never has
been decided by this court or the Supreme Court. In so
holding we imply nothing as to our view of the merits of
this appeal. We conclude that an immediate appeal may
materially advance the ultimate termination of the litiga
tion.”
The motion for leave to appeal was granted and the case
was advanced for oral arguments on the merits on August
24, 1972.
The July 20, 1972, order of this court included the following
stay order, which has remained in effect pending final disposi
tion of the appeal on its merits:
“The motion for stay pending appeal having been con
sidered, it is further ORDERED that the Order for Ac
quisition of Transportation, entered by the District Court
on July 11, 1972, and all orders of the District Court con
cerned with pupil and faculty reassignment within the
Metropolitan Area beyond the geographical jurisdiction
of the Detroit Board of Education, and all other proceed
ings in the District Court other than planning proceedings,
be stayed pending the hearing of this appeal on its merits
and the disposition of the appeal by this court, or until fur
ther order of this court. This stay order does not apply to
the studies and planning of the panel which has been ap
pointed by the District Court in its order of June 14,
1972, which panel was charged with the duty of pre
paring interim and final plans of desegregation. Said
4 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
panel is authorized to proceed with its studies’ and plann
ing during the disposition of this appeal, to the end that
there will be no unnecessary delay in the implementation
of the ultimate steps contemplated in the orders of the
District Court in event the decision of the District Court
is affirmed on appeal. Pending disposition of the appeal,
the defendants and the School Districts involved shall
supply administrative and staff assistance to the aforesaid
panel upon its request. Until further order of this court,
the reasonable costs incurred by the panel shall be paid
as provided by the District Court’s order of June 14, 1972.”
This court also has granted leave to appeal to various in
tervening parties and leave to file numerous amicus briefs.
Extensive oral arguments on the merits were heard August
24, 1972. The briefs and arguments of all the parties have
been considered in the disposition of this appeal.
We affirm two of the ridings of the District Court sum
marized above: (1) The Ruling on the Issue of Segregation
and (2) the Findings of Fact and Conclusions of Law on
“Detroit-only” plans of desegregation. We hold that the find
ings of fact of the District Court as set forth in these rulings
are not clearly erroneous, Rule 52(a), Fed. R. Civ. P., but to the
contrary are supported by substantial evidence.
As to the District Court’s third ruling pertaining to the pro
priety of a Metropolitan remedy, we affirm in part and re
verse in part. We vacate this and the two remaining orders
and remand to the District Court for further proceedings as
hereinafter set forth in detail in this opinion.
I. Chronology of Proceedings
On April 7, 1970, the Detroit Board of Education adopted
a plan to effect a more balanced distribution of black and
white students in the senior high schools through enactment
of changes in attendance zones involving some 12,000 pupils,
to become effective over a three year period. Three months
later this modest effort was thwarted by the legislature of
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 5
the State of Michigan through enactment of Act 48 of the
Public Acts of 1970. Section 12 of the Act delayed implementa
tion of the plan. The four members of the Board who sup
ported the April 7 plan were removed from office through a
citizen initiated recall election. The new members of the
board and the incumbent members who had originally op
posed the April 7 plan thereafter rescinded it.
The complaint in this case was filed by individual black
and white school children and their parents, and the Detroit
branch of the NAACP against the Board of Education of the
City of Detroit, its members, and the then Superintendent
of Schools, as well as the Governor, the Attorney General,
the State Board of Education and the State Superintendent
of Public Instruction of the State of Michigan.
The complaint alleged that the Detroit public school system
was and is segregated on the basis of race as the result of
actions and policies of the Board of Education and of the
State of Michigan. The complaint specifically challenged the
constitutionality of Act 48 of the Public Acts of 1970 of the
State of Michigan, which in effect repealed the April 7, 1970,
high school desegregation plan formulated by the Detroit
Board.
The case was heard originally on plaintiffs’ motion for a
preliminary injunction to restrain the enforcement of Act
48. In response to this motion the District Judge denied a pre
liminary injunction, did not rule on the constitutionality of Act
48, but granted the motion of the Governor and Attorney Gen
eral of Michigan for dismissal of the cause as to them. On
appeal this court held that § 12 of Act 48 was an unconstitu
tional interference with the lawful protection of Fourteenth
Amendment rights, that there was no abuse of discretion in
denying a preliminary injunction, and that the Governor
and Attorney General should not have been dismissed as par
ties defendant at that stage of the proceeding. The case was
remanded to the District Court for an expedited trial on
the merits. 433 F.2d 897.
On remand plaintiffs moved for immediate implementation
of the April 7 plan. On December 3, 1970, following an
evidentiary hearing on that plan and two updated plans, the
District Court ordered implementation of the “Magnet” or
“McDonald” plan effective at the beginning of the next full
school year, pending ultimate disposition on the merits. Plain
tiffs appealed and filed a motion for summary reversal. This
court again held that the District Court had not abused its
discretion in refusing to adopt the April 7 plan prior to an
evidentiary hearing on the allegations of constitutional viola
tions in the complaint. We remanded the case with in
structions to proceed to trial expeditiously on the merits of
plaintiffs allegations concerning the Detroit public school
system. 438 F.2d 945. The trial of the case on the issue of
segregation began April 6, 1971, and continued until July
22, 1971, consuming 41 trial days. On September 27, 1971,
the District Court issued its ruling on the issue of segrega
tion, holding that the Detroit public school system was racially
segregated as a result of unconstitutional practices on the part
of the defendant Detroit Board of Education and the Michigan
State defendants. 338 F.Supp. 582.
A decision on a motion to join a large number of suburban
school districts as parties defendant was deferred on the
ground that the motion was premature, in that no reasonably
specific desegregation plan was before the court. The Detroit
Board of Education was ordered to submit desegregation plans
limited to the City, while State defendants were directed
to submit plans encompassing the three-county metropolitan
area. An effort was made to appeal these orders to this
court. On February 23, 1972, this court held the orders to be
non-appealable and dismissed the appeal. — F .2 d ---- , cert.
denied, — U.S. — , 41 U.S.L.W. 3175 (Oct. 10, 1972).
After further proceedings concerning proposals for a Detroit
only desegregation remedy and the presentation of two plans
therefor, the District Judge on March 24, 1972, issued a
ruling entitled “Ruling on Propriety of Considering a Metro
6 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. I
politan Remedy,” and on March 28, 1972, he issued “Findings
of Fact and Conclusions of Law on Detroit Only Plans of
Desegregation.” He rejected all Detroit only plans, saying
in part: “Relief of segregation in the public schools of the
City of Detroit cannot be accomplished within the corporate
geographical limits of the city.”
Subsequently, the District Court issued an order on June
14, 1972, entitled “Ruling on Desegregation Area and Order
for Development of Plan for Desegregation.” In this ruling
and order the District Court established tentative boundaries
for a metropolitan remedy and provided for a panel of nine
members to design plans for integration of the Detroit schools
and those of 53 metropolitan school districts within certain
guidelines.
The panel recommended preparatory purchases of school
buses prior to implementation of an interim plan in Septem
ber 1972. Following a hearing, the District Court on July
11 ordered State defendants to purchase or otherwise acquire
295 school buses.
In view of the intervening Congressional action by the en
actment of the “Broomfield Amendment,” certification was
made to the Attorney General of the United States that the
constitutionality of § 803 of the Education Amendments of
1972, Pub. L. No. 92-318, 86 Stat. 235, had been called into
question. The Department of Justice intervened, filed a brief
and participated in the oral arguments before this court.
II. The Issues
All of the parties to this litigation in one form or another
present three basic issues which we phrase as follows:
1. Are the District Court’s findings of fact pertaining to
constitutional violations resulting in system-wide racial segre
gation of the Detroit Public Schools supported by substan
tial evidence or are they clearly erroneous?
2. Based on the record in this case, can a constitutionally
8 Bradley, et al. v. Milliken, et ah Nos. 72-1809, 72-1814
adequate system of desegregated schools be established with
in the geographic limits of the Detroit school district?
3. On this record does the District Judge’s order requiring
preparation of a metropolitan plan for cross-district assign
ment and transportation of school children throughout the
Detroit metropolitan area represent a proper exercise of the
equity power of the District Court?
III. The Constitutional Violations
(A) Constitutional violations found to have been committed
by the Detroit Board of Education:
(1) Segregative zoning and assignment practices.
(a) The District Judge found that the Detroit
Board of Education formulated and modified
attendance zones to create or perpetuate racial
segregation. He also found that the feeder sys
tem for junior and senior high schools was de
signed to maintain rather than eliminate black
or white schools at the higher levels. Its prac
tice of shaping school attendance zones on a
north-south rather than an east-west orientation
resulted in attendance zone boundaries con
forming to racial dividing lines.
(b ) He further found that the Detroit Board of
Education’s policies involved a substantial
number of instances of transporting black chil
dren past white schools with available school
space.
(2) He also found that it was the policy of the Board
of Education to create optional attendance areas
which permitted white students to transfer to all
white or predominately white schools located nearer
the city limits.
Nos. 72-1809, 72-1814 Bradley,, et al. v. Milliken, et al. 9
(3) The District Judge also found that the policies of
the Detroit Board of Education (and State Board
of Education) concerning school construction in
some instances had the purpose of segregating stu
dents on a racial basis and in many others resulted
in maintaining or increasing segregation.
(1) Segregative Zoning and Assignment Practices.
(a) The District Judge’s findings of fact pertaining to al
teration of zones and feeder patterns are as follows:
“The Board has created and altered attendance zones,
maintained and altered grade structures and created and
altered feeder school patterns in a manner which has
had the natural, probable and actual effect of continuing
black and white pupils in racially segregated schools.
The Board admits at least one instance where it pur
posefully and intentionally built and maintained a school
and its attendance zone to contain black students.
Throughout the last decade (and presently) school at
tendance zones of opposite racial compositions have been
separated by north-south boundary lines, despite the
Board’s awareness (since at least 1962) that drawing
boundary lines in an east-west direction would result in
significant integration. The natural and actual effect of
these acts and failures to act; has been the creation and
perpetuation of school segregation. There has never been
a feeder pattern or zoning change which placed a pre
dominantly white residential area into a predominantly
black school zone or feeder pattern. Every school which
was 90% or more black in I960, and which is still in use
today, remains 907 or more black.” 338 F.Supp. at 588.
The legal conclusion of the District Judge is as follows:
“5. The Board’s practice of shaping school attendance
zones on a north-south rather than an east-west orienta
tion, with the result that zone boundaries conformed to
racial residential dividing lines, violated the Fourteenth
10 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
Amendment. Northcross v. Board of Ed. of Memphis,
6 Cir., 333 F.2d 661.” 338 F.Supp. at 592-93.
* « «
“9. The manner in which the Board formulated and
modified attendance zones for elementary schools had
the natural and predictable effect of perpetuating racial
segregation of students. Such conduct is an act of de
jure discrimination in violation of the Fourteenth Amend
ment. United States v. School District 151, D.C., 286 F.
Supp. 786; Brewer v. School Board of City of Norfolk, 4
Cir., 397 F.2d 37.” 338 F.Supp. at 593.
There is, of course, other legal support for the legal con
clusions set out above. Davis v. School District o f Pontiac,
443 F.2d 573, 576 (6th Cir.), cert, denied, 404 U.S. 913 (1971);
United States v. Board of Education, Ind. School District No.
1, 429 F.2d 1253, 1259 (10th Cir. 1970); United States v.
Jefferson County Board o f Education, 372 F.2d 836, 867-68
(5th Cir. 1965), aff’d in banc, 380 F.2d 385 (5th Cir. 1966),
cert, denied sub nom, Caddo Parish School Board v. United
States, 389 U.S. 840 (1970); Clemons v. Board o f Education,
228 F.2d 853, 858 (6th Cir.), cert, denied, 350 U.S. 1006
(1956); Spangler v. Pasadena Board of Education, 311 F.
Supp. 501, 522 (C.D. Cal. 1970).
Witness Charles Wells, defendant School Board’s assistant
superintendent in charge of the Office of Pupil Personnel
Services, read into the record and testified in support of the
minutes of a meeting of the Citizens Association for Better
Schools. Mr. Wells was the president of the Citizens As
sociation at the time the meeting was conducted. His testi
mony includes the following:
“Q. (By Mr. Lucas) Go ahead, sir.
“A. ‘November 3, 1960.
‘TO: Honorable Nathan Kaufman, Chairman
Committee on Equal Education Opportunity.
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 11
‘We should like to begin our presentation by reviewing
with you briefly the development of our organization. We
feel it is significant as it represents an attempt on the
part of people who make up this organization to effective
ly deal with the frustrations historically inherent in at
tempting to provide for minority group children an ade
quate education within the Detroit Public School System.
A majority of the people of the Negro race moved into
the now Center District from other school districts with
in the limits of the City of Detroit. Although better
housing conditions were but one of the motives for such
a move, of equal importance was a desire to provide their
children with a more equitable and enriched educational
experience.
‘They were aware of the increased population within
their new geographical area, and accepted the counselling
of the then new administration of the Board of Edu
cation, to the effect that additional tax monies would
have to be made available if educational standards within
the City of Detroit were to be improved, or even main
tained. Consequently, each of them made a strong per
sonal investment in the millage campaign of Spring 1959.
In this campaign, initially, their efforts did not meet the
wholehearted approval of the Negro community, since
from past experience, particularly involving other millage
campaigns, members of the Negro community had ob
served that the results of the expenditures of monies
obtained from additional taxes, had little effect on the
facilities, the equipment, or the curriculum available to
their children.
‘Despite this resistance, they were aware that there
would be less justification for demanding adequate edu
cational opportunities for their children if they did not
accept their responsible share for the successful passing
of the millage program. As a consequence of their ef
forts, their respective schools voted overwhelmingly for
the millage program, and they logically expected that
positive results would follow their efforts.
12 Bradley, et al. v. Milliken, ct al. Nos. 72-1809, 72-1814
‘Their first disillusionment occurred only a few months,
but yet a few weeks after the passage of the millage —
they were rewarded with the creation of the present
Center District. In effect this District, with a few minor
exceptions, created a segregated school system. It ac
complished with a few marks of the crayon on the map,
the return of the Negro child from the few instances of
an integrated school exposure, to the traditional pre
dominantly uniracial school system to which he had for
merly been accustomed in the City of Detroit.
‘Their attempts to meet this threat to their children’s
educational experience through existing school organiza
tions met with little success. Their conferences with
District and City-Wide administrators including the super
intendent, Dr. Samuel Brownell, resulted in only ration
alizations concerning segregated housing patterns, and
denials of any attempts at segregation. When it was
pointed out that regardless of motivation, that segrega
tion was the result of their boundary changes, little com
promise was effected, except in one or two instances,
where opposition leadership was most vocal and ag
gressive.
Concurrent with boundary changes, it was alarming
ly noticeable that the school population within the Cen
ter District was rapidly increasing, and that the priority
building program would have little positive effect in
dealing with the problem. Attempts to discuss this prob
lem with school and district administration gave promise
of only minimal relief.
Finally, it had been earlier noted by new residents
moving into what is now the Center District that prior
to and during its change from a uniracial (predominant
ly white) to a biracial system and again to a uniracial
(predominantly Negro) school system that the quality
of their children’s previous educational experiences did
not eqiup them to compete on an equal basis with resi
dent children in the same grade and classifications.
“These experiences made them aware that no one or
ganization composed of one or several schools, could ef-
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 13
fectively coordinate the mutual concern of the many
parents residing within the Center District. Thus out of
the several discussions of groups of people whose primary
concern was the adequate and equitable education of their
children, this organization was bom. It is felt that no
better description of its purpose, its objective, and its
reason for being can be found than in the preamble to
its Constitution, which is:
‘PREAMBLE: Our interest is in equal educational op
portunities for all persons within the City of Detroit.
‘We do not believe that such opportunities are possible
within a segregated school system.
‘We oppose a policy of containment of minority groups
within specified boundaries, an example of which is the
Center District. While the above is of utmost concern
to us we are also aware that there is need for improve
ment and enrichment of the standards within this district
in practice as well as in theory.
‘We believe that once standards have become reason
ably adequate, that such standards should be maintained.
It should be further recognized that future population
shifts brought about by urban redevelopment will ad
versely affect the above goals in the Center District, unless
there is anticipation of the impact of this population
growth upon this district.
‘Since the inception of our organization we have noted
the following:
‘The public school system of the City of Detroit is
divided into nine administrative districts, one of which
is the Center District.
‘Yet, every day, when the children in this city leave
their homes to go forth to public schools, approximately
one out of every four leaves a home in the Center District.
Of the 154,969 children enrolled in public elementary
schools as of September 30, 1960, 36,264 or 23.4 percent
of these children leave a home in the Center District.
‘There are 221 elementary school buildings in the De
troit Public School System. Of these 28 are in the Center
District. This means, then, that the 23.4 percent of the
total elementary school population is accommodated in
12.7 percent of the buildings.
Fifteen percent of these children sit in classes of 40 to
44 students per class. This is in comparison to:
14 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
Sixty-two and one-half percent of all the children in
the city’s elementary schools who sit in classes of 45 to
49 are children in the Center District. These schools in
the Center District find their capacities short by 6,352
pupil stations. In other words, their capacities are over
taxed to the extent of 16 percent; and the future build
ing program, as set forth by the superintendent’s report
of October 17, 1960, will make available only 11,189 ad
ditional pupil stations within the next ten-year period.
However, this will be insufficient to meet the demands of
the Center District. Therefore, it is apparent that a
school bussing program will have to become a permanent
part of the school housing program. Thus the manner
in which the bussing program is administered becomes a
matter of acute concern.
‘Presently, children are being bussed by grades. Under
this system a number of problems are created:
1) It makes necessary a reorganization of the
bussing school, as well as the school into which the
children are bussed.
2) They are not integrated into the school into
which they are bussed, except in minor instances.
East
North
.13 percent
.05 percent
.04 percent
.08 percent
.01 percent
.01 percent
.05 percent
Northeast
Northwest
South
Southeast
West
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 15
3) There is a possibility of the separation of the
family unit.
4) Parents are unable to establish a good rapport
with the teachers and administrators in the new
school since there exists a time limit in which these
children will be members of that school.
‘It is recommended that a policy of bussing by geo
graphical areas instead of by grades be instituted so as
to eliminate the above problems.
‘The emphasis on curricula objective are not compara
ble in the various school districts of the Detroit School
System. There is a tendancy in the Center District to
stereotype the educational capacity of the children. This
means that children entering the schools in this district
whose background enables them to comprehend an en
riched educational program, are not challenged.
‘For example, one student in the Hutchins Intermediate
School who desired to prepare for entrance into an East
ern college found that Latin was not offered, and only
after considerable effort by members of the community,
along with his family, was Latin placed back in the school
curriculum. Many other instances can be cited upon
request.
‘Conversely, children whose initial capacity is retarded
by deprived socio-economic circumstances also go un
challenged. The District Administrator has admitted that
no program exists to take care of these children.
‘The curriculum and counselling as they now exist,
do not encourage students to achieve their maximum ca
pacities. We feel that the responsibility for any inequities
in the educational experience offered to any group of
children within a given school system must be assumed
by those persons charged with the overall responsibility
of administering that system.
‘Therefore, we recommend that strong policies be adopt
ed by the top administration to erase inequities of the
16 Bradley, et al. v. Milliken, et ah Nos. 72-1809, 72-1814
Detroit Public School System, and a policy of super
vision through all levels of administration be instituted
at all levels of administration to insure equal educational
opportunities to all children.
‘The Citizens’ Association for Better Schools.’
“Q. Do you join in that statement in submission to the
committee?
“A. Yes, I did.”
* O 9
Mr. Wells cited the example of the Center ( administrative)
District, where attendance boundaries were shaped in a gerry
mandered fashion to conform to the racial residential pattern.
“Q. With regard to that same situation, you were ex
pressing a problem which your committee had met in
attempting to discuss this. Can you tell me how you
came to be discussing this with the Board at that time?
“A. It was not with the Board of Education, I be
lieve it was with the administration of the school system.
“Q. The administrative staff?
“A. Including the superintendent.
“Q. All right.
“A. Our initial concern about the boundaries of the
center district grew out of the concern we had in 1960
about the changing of the attendance areas between the
Central High School and the Mackenzie High School.
“Q. Is that the optional attendance area also set up in
that?
“A. A part of that was optional. Well, let’s put it
that way, a part of it had been optional, the proposal was
to eliminate the option. In the process of eliminating the
option what it would mean would be that by and large
the few black children who had been attending Mackenzie
would have been pulled back into the Central area.
"Q. Mackenzie at that time was a majority white
school?
“A. Predominatly white.
“Q. Central by that time had become black?
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 17
“A. Predominatly black.
“Q. So the cancellation of the optional area which
had been there had the effect of preventing black chil
dren choosing Mackenzie, is that correct?
“A. That is right.
“Q. Were there any other schools — there is a ref
erence made to the establishment of the center district
boundaries — were there any other schools which had
not previously been in certain feeder patterns that were
drawn back into the center district?
“A. I am trying to remember now as I said eleven
years.
“Q. I understand.
“A. If I remember correctly, the Sherrill School which
also had been a part of it, that portion north of Tireman
had been attending Mackenzie and they in turn, the total
school then would have been returned to the Chadsey
area.
“Q. What about Tappan and that area, are you fa
miliar at all with changes that took place?
“A. Tappan was the junior high school in which Win
terhalter, the elementary school in the area south of
Davison just west of Ewald Circle attended. At that
time the students from that area attended Tappan and
all students from Tappan attended Mackenzie.
“The new change would mean that the students from
Winterhalter, and I think McKerrow which is just below
Winterhalter would have attended Tappan through the
9th grade, but then had been pulled back into the center
district to attend Central High School.
“The other students in Tappan would have gone to
Mackenzie.
“Q. The other students in Tappan, were they pre
dominatly white students?
“A. Yes. Our concern about this region really at that
time was that we could draw a line which separated the
black residents from the white residents and almost to
the alley and that in effect was the boundary line of
the center district.”
There was evidence that school feeder patterns were changed
so as to make particular junior high schools or senior high
schools either generally white or generally black, as shown
in the following testimony:
“MR. CALDWELL: Your Honor, I have copies of
the Mumford High School district in 1959 which is taken
from Plaintiffs Exhibit 78-A, and this makes it easier to
see the schools.
Q. Let s get back to the 1962-’63 overlay.
“Prior to the 1962-’63 - first of all, will you point out
to the Court where the Vandenberg and Vemor Schools
are.
A. This triangle to the northwest corner of this area.
( indicating)
Q. Prior to 1962-63 where did the Vemor and Van-
derburg youngsters go to high school?
“A. Mumford High School.
“Q. A boundary change was made in 1962-63?
“A. That’s right.
Q. Where did those youngsters go to school in that
year?
“A. Ford High School.
Q. How long did that feeder pattern continue?
A. Until 1966-67 when they returned to Mumford.
“Q. All right.
MR. CALDWELL: Plaintiffs’ Exhibit 128-A, your
Honor, reflects that in 1960 Vandenburg and Vemor were
0 percent black. Mumford was 16.1 black, Ford was .1
percent black. With regard to Vandenburg and Vemor,
there was a gradual increase in the black population until
1966 when Vandenburg was 39.5 percent black and Ver-
nor was 39.8 percent black.
Then in 1967 the change was made taking Vandenburg
and Vemor back into Mumford. Vandenburg had be
come 70 percent black, Vernor had become 63.2 percent
black. That year the change was made and Mumford
was 78.1 percent black, Ford was 4.1 percent black.
18 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 19
“Q. I believe that feeder pattern continued into the
current school year?
“A. That is right.
“Q. Those schools now feed back into Ford High
School this year?
“A. That is right.”
The effect of such a policy was attested to by Dr. Gordon
Foster of the University of Miami, director of the Florida
School Desegregation Consulting Center:
“Q. The effect, Doctor, then, of the removal of Van-
denberg and Vemor from the Ford feeder pattern into
the Mumford feeder pattern, what was the effect in terms
of race?
“A. The effect of this move in 1967-68 of the transfer
back of the two elementary schools was to increase the
segregation at Mumford, to take blacks from the Ford
High School and, therefore, increase the segregated pat
tern there, and, in my opinion, it reinforced inevitably
the perception that Ford would be kept white as a
matter of basic policy and that Mumford would be a
racially contained isolated high school attendance area.”
Similar testimony regarding the segregative effect of alter
ing school feeder patterns was given with respect to the
Jefferson and Hutchins Junior High Schools, Garfield and
Spain Junior High Schools, Burton and Irving Elementary
Schools, Higginbotham Elementary School, Jackson and Foch
Junior High Schools, Stellwagen, Keating and Clark Elemen
tary Schools, Cleveland and Nolan Junior High Schools, Cour-
ville Elementary School, Ford and Brooks Junior High Schools,
Osborne and Pershing High Schools, Parkman Elementary
School, the Ellis, Sills, Newberry and Sampson Elementary
Schools, and Northwestern and Chadsey High Schools.
(b ) The District Judge made the following findings of
fact pertaining to busing black children to black schools past
white schools:
20 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
“The Board, in the operation of its transportation to
relieve overcrowding policy, has admittedly bused black
pupils past or away from closer white schools with avail
able space to black schools. This practice has continued
in several instances in recent years despite the Board’s
avowed policy, adopted in 1967, to utilize transporta
tion to increase integration.
“With one exception (necessitated by the burning of
a white school), defendant Board has never bused white
children to predominantly black schools. The Board has
not bused white pupils to black schools despite the enor
mous amount of space available in inner-city schools.
There were 22,961 vacant seats in schools 90% or more
black.” 338 F.Supp. at 588.
The legal conclusion of the District Judge follows:
“8. The practice of the Board of transporting black
students from overcrowded black schools to other identi-
fiably black schools, while passing closer identifiably white
schools, which could have accepted these pupils,
amounted to an act of segregation by the school authori
ties. Spangler v. Pasadena City Bd. of Ed., D.C., 311
F.Supp. 501.” 338 F.Supp. at 593.
Additional support for the District Judge’s legal conclusion
includes: United States v. School District 151, 286 F.Supp. 786,
798 (N.D. 111. 1967), a f d , 404 F.2d 1125, 1131 (7th Cir.
1968), on remand, 301 F.Supp. 201, 211, 222 (N.D. 111. 1969),
aff’d, 432 F.2d 1147, 1150 (7th Cir. 1970), cert, denied, 402
U.S. 943 (1971); United States v. Board o f School Commis
sioners, Indianapolis, Ind., 332 F.Supp. 655, 669 (S.D. Ind.
1971).
The following testimony pertains to busing black children
from overcrowded black schools past white schools with
available pupil capacity to other black schools:
“Q. I am trying to anticipate, Mr. Ritchie’s question.
Have you noted some examples of the bussing of black
children from black schools to other black schools?
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 21
“A. I have.
“Q. Could you give us a couple illustrations?
“MR. BUSHNELL: While Dr. Foster is looking
through his notes, might I make the request that we
made yesterday that on conclusion of his testimony we
have access to the notes made?
“MR. LUCAS: At the conclusion, yes. We have no
objection to that.
“A. In 1960-61, and we don’t have any record for
’61-62 so I am not certain as to that year, students were
transported from Angell to Greenfield Park. This has
already been part of our testimony, I believe, 186 students
and students from Angell to Higginbotham, 118 students.
In 1969 -
“Q. Excuse me, Doctor, let me ask you if the Angell-
Higginbotham — were there white schools available with
space, from your examination of the records?
“A. Yes, there were.
“Q. Between Angell and Higginbotham?
“A. Yes, sir, I believe I testified to that before.
“Q. All right.
“A. In 1969 the Ruthruff Elementary School which
was 99 percent black transported 143 children to Herman
Elementary, 55 percent black.
0 0 0
“Q. (By Mr. Lucas, continuing) Dr. Foster, would
you step to the map.
“I think we were talking about the Ruthruff-Herman
Schools.
“A. Yes. We were testifying at recess about trans
portation of blacks past white schools. In 1969 we stated
that Ruthruff Elementary which is here in the south
eastern portion of the Mackenzie High School zone on
the large 1970-71 attendance area map, in 1969 trans
ported 143 children to Herman Elementary School which
is just below the blue area on the undermap here —
Herman Elementary School (indicating). Herman in
1969 was 55.6 percent black. Ruthruff was 99.1 percent
black and I think it is important to note that the access
22 Bradley, et a l v. Milliken, et al. Nos. 72-1809, 72-1814
to Herman goes right past the Parkman Elementary
School which at that time had 136 spaces available and
according to their capacity figures —
“Q. Parkman was what percentage?
“A. Parkman I don’t have the figure for ’69 and ’70.
Parkman was 12.8 percent black.”
O 9 O
“A. Another example was the Parker Elementary
School which is in the general center of the Mackenzie
High School zone. Parker in 1970 was 79.4 black; 61
children were bussed from Parker again to the Herman
Elementary School which at that time was 58.5 percent
black and again past the Parkman Elementary which in
1970 was 12.8 percent black.
“Q. Did Parkman have capacity at that time, Doctor?
“A. Parkman in ’70, according to my data, had 121
spaces.
* © *
“Q. Excuse me, would you give us the A. L. Homes.
“MR. BUSHNELL: I thought the Court ruled on that?
“THE COURT: He says he is pursuing a non-cumula-
tive matter here. If that be true he may go ahead.
“A. A. L. Holmes School, children were bussed from
this school over to the McGraw School which is in the
south end of the Northwestern District in center city.
In 1970-71 the Post Junior High School, which is lo
cated —
“MR. BUSHNELL: If the Court please, Mr. Lucas
just pointed out the location of Post which the witness
obviously couldn’t find on the map.
“THE COURT: Well, he hasn’t moved it.
“A. I noted the west section of Cooley instead of the
east. The Post Junior High School and Clinton Schools,
which are in the east section of the Cooley High School
attendance zone transported 54 students to the Jefferson
School which is now in the Murray zone and it is lo
cated in the eastern section of the Murray High School
attendance area. I think it is important to note that
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 23
these students who were bussed came from a consider
able distance north and there were several possibilities —
Q. Excuse me, were the Post children in a black
school or white school?
“A. The Post School this year, 1970-71 was 99.3 per
cent black. The Clinton School from which they also
came was 97 percent black.
“Q. What about Jefferson?
A. Jefferson was 87.6 percent black. There were two
or three other possibilities much closer to the Post-Clinton
area. One would have been in the western portion of the
Mackenzie district here (indicating).
“Q. What is the racial composition?
“A. At this time it had 35.4 percent black with a ca
pacity of 109 stations available. Another possibility would
have been the Vetal School in the Redford zone, the
southern portion of the Redford High School zone, which
at this time was 2 percent black with vacancies of 203
pupil stations and a third alternative could have been
the Coffey School to the east of the Ford attendance area
which at this time was 29 percent black with 69 pupil
stations available.
“Q. Did you say to the east was part of the Ford
attendance area or outside of that, Doctor?
“A. It’s in the Ford attendance area.
» * *
“THE COURT: Well, to save time why don’t we pro
ceed on the assumption that that was his testimony.
But if it proves otherwise we will strike it.
“MR. LUCAS: Thank you, sir.
“Q. (By Mr. Lucas) Doctor, I understand that the
policy of the district is that bussing to relieve overcrowd
ing would be done in such a manner as to improve in
tegration at the receiving school. From your examina
tion of the current bussing examples which you have
given, do you have an opinion as to whether or not that
policy has or has not been followed?
“A. Well, I think from the examples I have given so
far it would give an indication that integration could
24 Bradley, et al. v. Milliken, et ah Nos. 72-1809, 72-1814
have been effected in a much better way if the children,
instead of going to the schools would have been dropped
off at other schools where the racial balance was quite
different.
O » S
“Q. Are there any white schools from your examina
tion of data, Doctor Foster, between Angell and Higgin
botham which had capacity at that time?
“A. Yes, there were several which were a good deal
closer to Angell than Higginbotham. The effect of this
sort of zoning pattern was to provide segregated student
ratios at all three of the elementary schools, and in
terms of things that could be done or could have been
done at that particular time to correct the segregated
situation, it is my opinion that, first of all, the students
being bussed from Angell could have been dropped off
at any number of places on the way to Higginbotham,
schools which had the space and had a better racial
composition for this sort of input. This having been
done, zone lines could have been redrawn at these three
schools to have approached a racial balance situation
which, in my opinion, would have helped to stabilize the
situation at that time. This would have also assisted in
the overcrowding at Pasteur and a couple of classrooms
extra at Higginbotham.
“Q. Do you have an opinion, Doctor, as to the per
ception created by the maintenance of the Higginbotham
School under those circumstances, including the transpor
tation of black students from Angell into it?
“A. Well, it is obvious that if you transport black
children past white schools to an all black school that the
community is going to perceive this as a segregated in
tent, a segregated action. If you have a boundary situa
tion which isolates and enforces black students to a par
ticular area when the boundary lines could be changed
to effectuate a better pattern racially, then it seems to
me that community perception would also be that the
school is not doing what it could in terms of integration
and equal opportunity.
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 25
“Q. Doctor, from your examination of the data in
1960 are there any administrative reasons, any administra
tive problems which would indicate to you a reason
why this boundary was maintained rather than drawn
in some other fashion?
“A. In terms of school capacity there are none, no.”
Defendant’s witness (Mr. Henrickson) admitted instances
of busing black students past closer white schools to black
schools:
“Q. We find on the under and over capacity map in
the Higginbotham area that there were three schools sur
rounding Higginbotham. Vernor, which is listed as be
ing 121 over capacity; MacDowell, 103, is it? Pasteur,
90. At the same time we find that Higginbotham was
489 under capacity. Is that what the exhibit shows, sir?
“A. Yes.
“Q. We also know, do we not, that Pasteur, Mac
Dowell and Vernor were white schools?
“A. Both Pasteur and MacDowell at that time, as I
recall, had some beginning of black students as a result
of the growth of the settlement of the Higginbotham
area.
“Q. They were predominatly white schools at that
time?
“A. Yes.
“Q. Higginbotham was all or virtually all black?
“A. Yes.
“Q. Indeed, it had been the same in 1950, had it not?
“A. Yes.
“Q. At the same time that we are talking about you
were transporting youngsters from Angell to Higgin
botham, is that correct?
“A. Yes.
“Q. Those were black kids being transported from
Angell to Higginbotham?
“A. Yes.
“Q. We also know on that exhibit that they were
transported past such schools as Fitzgerald and Clinton
which had more than enough capacity to handle them?
“A. We have made no denial of that.”
For some years it was a Board of Education policy to trans
port classrooms of black children intact to white schools where
they were educated in segregated classes.
Testimony as to the intact busing practice follows:
Q- (By Mr. Lucas, continuing) Will you go into the
Detroit system, Doctor, on transportation.
A. Answering it generally, counsellor, my answer
would be that the intact bussing is the practice of trans
porting classrooms of children intact from one school to
another and leaving them intact when they are educated
at the receiving school.
Q. Doctor, when such transportation occurs from a
school which is 90 percent or more black to a school which
is predominantly a white school, what effect, if any, does
this have in terms of racial segregation on those chil
dren?
A. This would lead to what we call classroom seg
regation or segregation within a particular school. It
could be sometimes resegregation, but essentially it is a
segregated situation within a school which could be seg
regated or not segregated generally.
“Q. Doctor, in your experience with school segregation
and school desegregation plans, is this a technique which
you have had to deal with in the past?
“A. On occasion, yes, sir.
“Q. Doctor, did you examine data or relevant informa
tion with respect to the transportation practices in the
Detroit school system in connection with this type of
bussing, intact bussing?
“A. Yes, sir.
“Q. What did your examination reveal, Doctor?
“A. It is my understanding from the data that there
was intact bussing generally in the late ’50’s, as I said,
and early ’60’s.
26 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 27
“Q. How did that intact transportation operate, Doc
tor?
"A. It involved transporting classrooms in whole from
one school to another receiving school and at the receiv
ing school the classrooms were kept intact for instructional
purposes.
“Q. Was this policy changed at any time, Doctor, as
far as you know?
“A. It is my understanding it was changed in the
middle ’60s but I don’t remember the exact date.
“Q. What would the change be, Doctor? What type
of bussing would result in terms of relieving overcrowd
ing?
“A. You simply gather children up on a geographical
basis and transport them and assign them at random
to whatever grade they are in the receiving school rather
than keeping them in an intact classroom.”
Segregating children by race within schools has been held
repeatedly to be unconstitutional. Jackson v. Marvell School
District No. 22, 445 F.2d 211, 212 (8th Cir. 1970); Johnson
v. Jackson Parish School Board, 423 F.2d 1055 (5th Cir. 1970).
The record indicates that in at least one instance Detroit
served a suburban school district by contracting with it to
educate its black high school students in a Detroit high school
which was overwhelmingly black by transporting them away
from nearby suburban white high schools and past Detroit
high schools which were predominately white.
The District Judge found on this score that for years black
children in the Carver School District were assigned to black
schools in the inner city because no white suburban district
(or white school in the city) would take the children.
This finding is supported by the testimony of Detroit School
Superintendent Drachler, which follows:
“Q. When was the Carver District in existence as a
separate entity?
“A. The Carver District? The Carver is not in De
troit.
28 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
“Q. Is it a separate school district whose students at
tended some Detroit high schools, in particular Northern?
“A. Oh, I see what you’re referring to. I am told that
back in ’57, ’58, at that time I was not in Central Office,
there were some students from Carver District who did
not have a place for adequate high school facilities. An
arrangement was made with Detroit for the Carver stu
dents to come in on buses and go to Northern High
School. Now, the nearest school to Carver was Mum-
ford at the time. And they did go past Mumford towards
Northern.
“Q. Is Carver a black district?
“A. Yes, black and very poor.
“Q. Has Carver District subsequently merged with
Detroit?
“A. Oak Park.
“Q. With Oak Park?
“A. That’s right.
“Q. And at that time the transportation was termi
nated?
“A. That’s right. By the way, as a result of those
youngsters coming, there was a rumor spread that De
troit children were being bussed, say, from the Higgin
botham, which is north — Higginbotham area which is
north of Mumford High School area but in Detroit, that
they were being bussed to Northern, too, because they
were black students, people saw black students from the
Eight Mile area coming down. But to the best of my
knowledge these were outside students.
“Q. There were black children being bussed to Hig
ginbotham, weren’t they?
“A. There were black children being bussed to Hig
ginbotham.
“Q. From Angell?
“A. From Angell past some white schools. And when
the issue was brought to Doctor Brownell’s attention by
me in about ’59 or ’60 — there were a series of instances
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 29
like that. There was the Angell, there was from the
military fort in the southwest, they were bussing their
own children up to the Noble, and Doctor Brownell, as
soon as it was brought to his attention, abolished that
as well as the optional areas.
“Q. Was this so-called intact bussing, that is a class
being brought as a unit?
“A. Generally speaking, yes. That policy of changing
to geographic bussing occurred about ’62-’63 as a result
of the Equal Education Opportunities Committee.
“Q. Was all of the bussing done in the City of De
troit of an intact nature until the Equal Opportunities
study?
“A. To the best of my knowledge it was. I know
when my children were being bussed, they were bussed
intact.”
(2 ) Optional Areas.
The record demonstrates that in many instances when
neighborhoods in Detroit began to experience some inmigra
tion of black families, it was Board of Education policy to
create optional attendance zones, thereby allowing white stu
dents to change schools to all white or predominately white
schools, generally located farther toward the city limits. For
many years the record indicates this practice to have been
pervasive. It continued in at least one instance up to the
1970-71 school year.
As to optional attendance zones, the District Judge found:
“During the decade beginning in 1950 the Board cre
ated and maintained optional attendance zones in neigh
borhoods undergoing racial transition and between high
school attendance areas of opposite predominant racial
compositions. In 1959 there were eight basic optional
attendance areas affecting 21 schools. Optional attendance
areas provided pupils living within certain elementary
areas a choice of attendance at one of two high schools.
In addition there was at least one optional area either
created or existing in 1960 between two junior high
30 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
schools of opposite predominant racial components. All
of the high school optional areas, except two, were in
neighborhoods undergoing racial transition (from white
to black) during the 1950s. The two exceptions were:
(1 ) the option between Southwestern (61.6% black in
1960) and Western (15.3% black); (2 ) the option be
tween Denby (0% black) and Southeastern (30.9% black).
With the exception of the Denby-Southeastem option
( just noted) all of the options were between high schools
of opposite predominant racial compositions. The South
western-Western and Denby-Southeastem optional areas
are all white on the 1950, 1960 and 1970 census maps.
Both Southwestern and Southeastern, however, had sub
stantial white pupil populations, and the option allowed
whites to escape integration. The natural, probable, fore
seeable and actual effect of these optional zones was to
allow white youngsters to escape identifiably ‘black’
schools. There had also been an optional zone (elimi
nated between 1956 and 1959) created in ‘an attempt
. . . to separate Jews and Gentiles within the system,’
the effect of which was that Jewish youngsters went to
Mumford High School and Gentile youngsters went to
Cooley. Although many of these optional areas had
served their purpose by 1960 due to the fact that most
of the areas had become predominantly black, one op
tional area (Southwestern-Western affecting Wilson Jun
ior High graduates) continued until the present school
year (and will continue to effect 11th and 12th grade
white youngsters who elected to escape from predominant
ly black Southwestern to predominantly white Western
High School). Mr. Henrickson, the Board’s general fact
witness, who was employed in 1959 to, inter alia, elimi
nate optional areas, noted in 1967 that: ‘In operation
Western appears to be still the school to which white
students escape from predominantly Negro surrounding
schools.’ The effect of eliminating this optional area
( which affected only 10th graders for the 1970-71 school
year) was to decrease Southwestern from 86.7% black in
1969 to 74.3% black in 1970.” 338 F.Supp. at 587-88.
Nos. 72-1809, 72-1814 Bradley, et al. v. MilUken, et al. 31
From these facts the District Judge arrived at the following
legal conclusion:
“7. The Board’s policy of selective optional attendance
zones, to the extent that it facilitated the separation of
pupils on the basis of race, was in violation of the Four
teenth Amendment. Hobson v. Hansen, D.C., 269 F.Supp.
401, aff’d sub nom., Smuck v. Hobson, 408 F.2d 175.
[(D.C. Cir. 1969)].” 338 F.Supp. at 593.
Additional support for the District Judge’s legal con
clusion includes: United States v. Texas Education
Agency, — F.2d — (5th Cir. 1972); Northcross v. Board
o f Education o f Memphis, 333 F.2d 661, 665-66 (6th
Cir. 1964) (different but analogous situation); United States
v. Board o f School Commissioners o f Indianapolis, 332 F.
Supp. 655, 668 (S.D. Ind. 1971); Spangler v. Pasadena City
Board o f Education, 311 F.Supp. 501, 502 (C.D. Cal. 1970).
The effect of use of optional zones was described in Dr.
Foster’s testimony:
“The first method or technique I might cite that is
used to maintain segregation would be the use of op
tional zones.
“Would it be possible for me to step to the board to
illustrate?
“Q. Please do.
(The witness proceeded to the blackboard.)
“A. Optional zones are sometimes also referred to as
dual zones or dual overlapping zones. I think it will
be easier for me to illustrate this briefly.
(The witness drew a sketch on the board.)
“A. If you have, let’s say, two high school districts,
District X and District Y, frequently when you set up
an optional zone you carve the zone out of one district,
occasionally two, but assume we carve it out of District
Y and the children in this optional zone are then per
mitted to go to either high school X or high school Y,
this becomes in a sense an overlapping zone because
32 Bradley, et al. v. Milliken, et aJ. Nos. 72-1809, 72-1814
if we refer to the boundaries of school District X at
this point it not only includes the previous boundary but
also takes in the optional zone.
“District Y in turn would include its previous bound
aries, also including the optional zone. I think this may
explain the origin of the connotation of the word ‘over
lapping’.
“Essentially optional zones are set up for two or three
reasons, one is to allow white students or black students
the option of attending one of the two attendance areas
which make up the boundaries of the zone and another
is for, occasionally for religious purposes to provide al
ternatives for persons of different religions. Sometimes
these are set up for socio-economic reasons and I have
on occasion seen them set up by boards of superin
tendents as political gimicks in order to help pass a bond
issue or one thing or another or a school board or super
intendent will set up temporary optional zones as a favor
to certain constituents in return for assistance in helping
the school board with one thing or another.
“I think in the frame work in which we operate they
are used primarily for maintaining segregated patterns.
* * *
“Q. Dr. Foster, have you made a study and analysis
of optional zones in the Detroit school system?
“A. Yes, I have.”
Dr. Fosters analysis of the purpose and effect of each op
tional zone in existence in the Detroit School District is
exemplified in his testimony on the Mackenzie-Central option.
“Q. Doctor Foster, do you have an opinion as to the
administrative use of the optional attendance zone in
1960 between and prior to that in Mackenzie-Central
area?
“A. Yes. I think it was used primarily — you mean
as to the purpose of it?
“Q. Well, as to whether or not it had any administra
tive value that you know of. Doctor, aside from race?
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 33
“A. In terms of assignment I can see no advantage to
it.
* * O
“Q. Do you have an opinion as to its use in terms of
segregation or desegregation, Doctor Foster?
“A. In my opinion it was used as an optional zone
to allow whites during the period it was in existence in
the ’50’s and also until such time as it was done away
with in 1962 to be assigned to predominantly white Mac
kenzie High School.
“Q. Doctor Foster, from your examination of the 1950
census and in turn the 1960 census exhibits, do you have
an opinion as to the effect of such an optional zone on
the community, residence pattern in the community?
4 « 4
“A. Community people and residents in a situation
such as this generally have a perception that there is
something wrong with their school, that the whites need
an optional zone to get out into a less black situation and,
therefore, this increases their perception of racial isola
tion and, in fact, physical containment.
“Q. Does this have an effect, Doctor, in terms of the
residence pattern? I believe you testified in 1950 the
optional area was entirely white or zero to 4.9 per cent
white.
# # *
“A. In my opinion this tends to increase the instability
of the community because they generally feel this is an ad
hoc temporary interim situation and it increases white
flight in this sort of situation.
* # *
“Q. Doctor Foster, does the use of these techniques in
some areas have an effect in terms of the perception of
the community of schools besides the actual two schools
to which the option was involved?
4 4 4
“A. Thank you. Yes, I think the perception is not only
34 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
of rank and file community residents, but people of con
siderable influence in the community, along with School
Board administration people, School Board members,
School Board officials. In many cases they have sub
stantiated this perception that I have recounted; that the
optional zones did lead to greater pupil segregation
and a feeling of frustration that the school authorities
were not doing what was called for in terms of desegre
gation, and it had a generally debilitating effect on the
image of the schools as far as all of these groups were
concerned.”
Mr. Henrickson, defendant School Board’s principal wit
ness and divisional director of planning and building studies
in the School Housing Division, did not deny the discriminatory
effect of at least some of these optional zones.
Q- In 1959 optional areas frustrated integration, did
they not?
MB. BUSHNELL: Objection to the form of the ques
tion.
“THE COURT: He may answer.
“A. Some of these areas in 1959 had no effect what
ever with movement of black or white students. They
were either all black or all white. Some of them such
as the Western-Southwestern area can be said to have
frustrated integration and continued over the decade.”
(3 ) Building Construction.
The District Judge found and the record contains evidence
that the Detroit Board of Education practices in school con
struction generally tended to have segregative effect; the great
majority of schools were built in either overwhelming all
black or all white neighborhoods so that the new schools
opened as one race schools.
The District Judge’s school construction findings were as
follows:
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 35
“In 1966 the defendant State Board of Education and
Michigan Civil Rights Commission issued a Joint Policy
Statement on Equality of Educational Opportunity, re
quiring that
‘Local school boards must consider the factor of racial
balance along with other educational considerations
in making decisions about selection of new school
sites, expansion of present facilities . . . . Each of
these situations presents an opportunity for inte
gration.’
Defendant State Board’s ‘School Plant Planning Hand
book’ requires that
‘Care in site locations must be taken if a serious
transportation problem exists or if housing patterns
in an area would result in a school largely segregated
on racial, ethnic, or socio-economic lines.’
The defendant City Board has paid little heed to these
statements and guidelines. The State defendants have
similarly failed to take any action to effectuate these
policies. Exhibit NN reflects construction (new or ad
ditional) at 14 schools which opened for use in 1970-71;
of these 14 schools, 11 opened over 90% black and one
opened less than 10% black. School construction costing
$9,222,000 is opening at Northwestern High School which
is 99.9% black, and new construction opens at Brooks
Junior High, which is 1.5% black, at a cost of $2,500,000.
The construction at Brooks Junior High plays a dual seg-
regatory role: not only is the construction segregated, it
will result in a feeder pattern change which will remove
the last majority white school from the already almost
all-black Mackenzie High School attendance area.
“Since 1959 the Board has constructed at least 13 small
primary schools with capacities of from 300 to 400 pupils.
This practice negates opportunities to integrate, ‘con
tains’ the black population and perpetuates and com
pounds school segregation.” 338 F.Supp. at 588-89.
36 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
Other cases in which such findings have been held to con
stitute a de jure act of segregation include: Swann v. Charlotte-
M ecklenburg Board o f Education, 402 U.S. 1, 21 (1971);
Cisneros v. Corpus Christi Independent School Dist., — F.2d
— (5th Cir. 1972), cert, applied for, 41 U.S.L.W. 3255 (Oct.
31, 1972); Kelly v. Guinn, 456 F.2d 100 (9th Cir. 1972),
petition for cert, filed, 41 U.S.L.W. 3114 (U.S. Aug. 28, 1972);
Davis v. School District o f Pontiac, 443 F.2d 573, 576 (6th
Cir.), cert, den ied 402 U.S. 913 (1971); Sloan v. Tenth School
District, 433 F.2d 587, 590 ( 6th Cir. 1970); United States
v. Board o f Education o f Tulsa, 429 F.2d 1253, 1259 (10th
Cir. 1970); Brewer v. School Board o f N orfolk, 397 F.2d
37, 42 ( 4th Cir. 1968); United States v. Board o f Public
Instruction, 395 F.2d 66, 69 (5th Cir. 1968); Kelley v. Alt-
heimer, Arkansas Public School Dist. No. 22, 378 F.2d 483,
496-97 (8th Cir. 1967); Johnson v. San Francisco Unified School
District, 339 F.Supp. 1315, 1326, 1341 (N.D. Cal. 1971);
United States v. Board of School Commissioners o f Indianapolis,
332 F.Supp. 655 ( S.D. Ind. 1971); Spangler v. Pasadena City
Board o f Education, 311 F.Supp. 501, 522 (C.D. Cal. 1970);
United States v. School District 151, 286 F.Supp. 786, 798
(N.D. 111.), a f d , 404 F.2d 1125 (7th Cir. 1968); L ee v. Macon
County Board o f Education, 267 F.Supp. 458, 472 (M.D. Ala.),
aff’d per curiam sub nom., W allace v. United States, 389 U.S.
215 (1967).
Record evidence pertaining to Detroit Board of Education
building construction practices and their results include:
“Q. Doctor Foster, I show you a document in evi
dence, Plaintiff’s Exhibit 70. I direct your attention to
page 15 of the exhibit. The exhibit is School Planning
Handbook, Bulletin 412, revised, January, 1970, Michigan
Department of Education. Directing your attention to
Chapter 2, the School Site, and the last full paragraph in
the left-hand column on page 15, Doctor, would you read
that paragraph?
“A. ‘Care in site location must be taken if a serious
transportation problem exists or if housing patterns in
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 37
an area would result in a school largely segregated on
racial, ethnic or socio-economic lines.’
“Q. Doctor, would you step down to the map, please?
Do you have a copy, Doctor, of Plaintiff’s Exhibit 79?
“A. Yes, I do.
“Q. Doctor, would you examine Plaintiff’s Exhibit 153,
which shows new school construction, 1960 to 1970? Per
haps you had better step back here. Doctor, the black
squares on here represent schools opening 80 to 100 per
cent black in pupil enrollment. Would you direct your
attention to the Drew Junior High School on the map
and examine the exhibit and tell me when Drew was
opened?
“A. According to the exhibit, the Drew Junior High
School was opened in 1970.
“Q. And what was it opened as in terms of its en
rollment, Doctor?
“A. 1,587 students.
“Q. And its percent black?
“A. 95 per cent black.
“Q. And the Eileen Primary School, Doctor, can you
locate it on the map?
“A. The Eileen Primary is in the Cooley High School
zone, I believe.
“Q. And when did it open, Doctor?
“A. 1970.
“Q. And what was its enrollment and its pupil popula
tion in terms of black?
“A. 333 students. The per cent black was 99.1.
“Q. Would you examine the map and locate the E.
M. Turner Primary?
“A. Yes.
“Q. What year was that opened, Doctor?
“A. The Turner Primary was opened in 1969.
“Q. And its enrollment of pupil population?
“A. 362 pupils, 97.5 percent black.
“Q. Can you find the Stewart School on there, Doc
tor?
38 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
“A. The Stewart School is in the same general area
as Turner, a little to the south.
“Q. What year was it opened?
“A. 1970. '
“Q. Its population and percent black?
“A. 766 enrollment, 98.8 percent black.
“Q. Marxhausen Primary, Doctor, can you locate that
on the map?
“A. Marxhausen is in the Finney zone.
“Q. Is that near or far away from the A. L. Holmes
School, Doctor?
“A. As I remember, rather close to the Holmes School.
“Q. Can you locate the Holmes School with reference
to that?
“A. The Holmes School is the next one to the north
west.
“Q. And what was its pupil population when it
opened?
“A. Marxhausen was opened in 1970 with a pupil
population of 302, 92.4 percent black.
“Q. Would you locate Mack Primary, Doctor?
“A. Mack Primary is also in the Finney zone.
“Q. And when did it open?
“A. Mack opened in 1970 with an enrollment of 173,
98.8 percent black.
“Q. Could you locate the Angell Primary area, Doc
tor?
“A. The Angell area is in the Northwestern attendance
zone.
“Q. And what was its enrollment and percent black?
“A. Angell was 1,282 students when it opened in
1970. The percent black was 99.9
“Q. Is there an asterisk by that particular school,
Doctor?
“A. On the exhibit?
“Q. Yes.
“A. Yes, there is.
“Q. Would you refer to the cover and tell us what
that asterisk indicates?
“A. It says, ‘The racial count data included in ex
isting school with the same name.’
“Q. Can you locate the Stark School, Doctor?
“A. The Stark School is in the Southeastern zone.
“Q. And what was its enrollment?
“A. The enrollment was 822 when it opened in 1969.
“Q. And the percent black?
“A. 98.4 percent black.
“Q. Can you locate the new King Senior High School,
Doctor?
“A. The new King Senior High School?
“Q. Yes.
“A. Here.
“Q. When did it open?
“A. It opened in 1968.
“Q. What was its enrollment?
“A. 1,897 pupils.
“Q. And its percent black?
“A. 98.8 percent black.
“Q. Can you locate the Field Annex, Doctor?
“A. Just to the northeast of King, the Field Annex.
“Q. And what was its enrollment?
“A. 461.
“Q. Its per cent black?
“A. 90.5 per cent black.
“Q. Can you locate the Glazer School, Doctor Foster?
“A. The Glazer School is in the Central zone.
“Q. And when did it open?
“A. In 1967.
“Q. And what was its enrollment, Doctor?
“A. 850 students.
“Q. What was its per cent black?
“A. 100 per cent black.”
Similar testimony was given with respect to the Stevenson,
Cortez, Beaubien, Sander, St. Clair Annex, Murray, Kettering,
Krolik, Joy, Tendler, Belleville, McGraw, Knudsen, Keidan,
Jamieson, Butzel, Woodward, Tendler and Norvell Schools.
White schools built to accommodate white residential areas in
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 39
40 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
eluded Fox, Lessenger, Murphy, Taft, Fleming, Earhart,
Reeves, Brooks and McKenny Annex.
“Q. Thank you, Doctor.
“Doctor Foster, from your examination of the pattern
of construction in this school system, 1960 to 1970, do you
have an opinion as to the effect of that pattern of con
struction on segregation in the Detroit School System?
“A. My opinion is that construction practices were
followed in such a way as to increase segregation. I
say this because of the large number of schools that were
opened that were either all black or all white or with
a disproportionate number of one race or the other upon
opening.
* » *
“Q. (By Mr. Lucas) Does the location of a school
in a particular place have a long term effect on a school
system?
“A. In terms of the nature of the pupils assigned to
the school, do you mean?
“Q. Yes, sir.
“A. Yes, it does.
“Q. Are there alternatives in schoolhouse construction
which can or should be considered by a school district
in terms of affecting the racial composition of student
bodies?
“A. In terms of site selection there are, yes.
“Q. What are some of the alternatives which can or
should be utilized, in your opinion, Doctor?
“A. It is customary in this day and age to consider
the problem of integration or segregation very carefully
in selecting sites for school buildings and, well, this was
pointed out, I believe, in the bit I read from the Michigan
State Department.
“Q. What effect in terms of perception of the com
munity does it have when a school is opened with an
overwhelming enrollment of one race or the other?
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 41
“A. Generally the community perceives, in my opin
ion, that the school has been thought of as being, going
to be an all white school or all black school and in either
case generally that it is racially isolated.”
(B) The constitutional violations found to have been committed
by the State of Michigan.
(T) Under Michigan law, M.S.A. § 15.1961, school build
ing construction plans must be approved by the State Board
of Education. Prior to 1962 the State Board also had statutory
authority to supervise school site selection. The proofs con
cerning the effect of Detroit’s school construction program
are therefore largely applicable to show State responsibility
for the segregatory results.
(2 ) During the critical years covered by this record the
State of Michigan discriminated against Detroit by allowing
the Detroit School District a capital improvement bonding
authority of only two percent as compared to five per cent
for all other school districts in the State up to the year 1969.
(3 ) During the critical years covered by this record the
School District of Detroit was denied any allocation of State
funds for pupil transportation, although such funds were made
generally available to all students who lived over a mile and
a half from their assigned schools in rural outstate Michigan,
and although some suburban districts continued to receive
State transportation money because of a “grandfather clause”
which continues their status of some years ago. See S.B.
1269, REG. SESSION, Sec. 7 1 (2 ) (a ) (b ) (1972).
(4 ) In 1970 the Detroit School Board undertook imple
mentation of its April 7 desegregation plan applicable to its
high schools. On meeting considerable resistance thereto, it
nonetheless proceeded. At that point the State Legislature
intervened by Act 48 of Public Acts of 1970 specifically over-
ru'ing the Detroit Board of Education’s desegregation plan.
While this statute has since been invalidated by judgment of
42 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
this court, its contribution to preventing desegregation and to
continuing and increasing segregation of the Detroit school
system cannot be overlooked.
(5 ) Finally, the cross-district transportation of black high
school students from the Carver School, located in Ferndale
school district, to a black high school in Detroit could not
have taken place without the approval, tacit or express, of
the State Board of Education. (See supra pp. 27-29)
The District Judge’s findings pertaining to constitutional
violations by the State of Michigan are as follows:
“The State and its agencies, in addition to their gen
eral responsibility for and supervision of public education,
have acted directly to control and maintain the pattern
of segregation in the Detroit schools. The State refused,
until this session of the legislature, to provide authoriza
tion or funds for the transportation of pupils within
Detroit regardless of their poverty or distance from the
school to which they were assigned, while providing in
many neighboring, mostly white, suburban districts the
full range of state supported transportation. This and
other financial limitations, such as those on bonding and
the working of the state aid formula whereby suburban
districts were able to make far larger per pupil expendi
tures despite less tax effort, have created and perpetuated
systematic educational inequalities.
“The State, exercising what Michigan courts have held
to be is ‘plenary power’ which includes power ‘to use a
statutory scheme, to create, alter, reorganize or even
dissolve a school district, despite any desire of the school
district, its board, or the inhabitants thereof,’ acted to
reorganize the school district of the City of Detroit.
“The State acted through Act 48 to impede, delay and
minimize racial integration in Detroit schools. The first
sentence of Sec. 12 of the Act was directly related to
the April 7, 1970 desegregation plan. The remainder of
the section sought to prescribe for each school in the eight
districts criterion of ‘free choice’ (open enrollment) and
‘neighborhood schools’ ( ‘nearest school priority accep-
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 43
tance’), which had as their purpose and effect the main
tenance of segregation.
In view of our findings of fact already noted we think
it unnecessary to parse in detail the activities of the local
board and the state authorities in the area of school con
struction and the furnishing of school facilities. It is our
conclusion that these activities were in keeping, generally,
with the discriminatory practices which advanced or per
petuated racial segregation in these schools.” 338 F.
Supp. at 589.
The District Judge arrived at the following legal conclusions:
“11. Under the Constitution of the United States and
the constitution and laws of the State of Michigan, the
responsibility for providing educational opportunity to
all children on constitutional terms is ultimately that of
the state. Turner v. Warren County Board of Education,
D.C., 313 F.Supp. 380; Art. VIII, §§ 1 and 2, Mich. Con
stitution; Daszkiewicz v. Detroit Bd. of Ed. of City of
Detroit, 301 Mich. 212, 3 N.W.2d 71.
“12. That a state’s form of government may delegate
the power of daily administration of public schools to
officials with less than state-wide jurisdiction does not
dispel the obligation of those who have broader control
to use the authority they have consistently with the con
stitution. In such instances the constitutional obligation
toward the individual school children is a shared one.
Bradley v. Sch. Bd. of City of Richmond, D.C., 51 F.B.D.
139, 143.
“13. Leadership and general supervision over all pub
lic education is vested in the State Board of Education.
Art. VIII, § 3, Mich. Constitution of 1963. The duties
of the State Board and superintendent include, but are
not limited to, specifying the number of hours necessary
to constitute a school day; approval until 1962 of school
sites; approval of school construction plans; accreditation
of schools; approval of loans based on state aid funds;
review of suspensions and expulsions of individual stu
dents for misconduct [Op.Atty.Gen., July 7, 1970, No.
4/05]; authority over transportation routes and disburse
ment of transportation funds; teacher certification and
the like. M.S.A. 15.1023(1), M.C.L.A. § 388.1001. State
law provides review procedures from actions of local
or intermediate districts (see M.S.A. 15.3442, M.C.L.A.
§340.442), with authority in the State Board to ratify,
reject, amend or modify the actions of these inferior state
agencies. See M.S.A. 15.3467; 15.1919(61); 15.1919(68
b ); 15.2299(1); 15.1961; 15.3402, M.C.L.A. §§340.467,
388.621, 388.628(a), 388.681, 388.851, 340.402; Bridge-
hampton School District No. 2 Fractional of Carsonville,
Mich. v. Supt. of Public Instruction, 323 Mich. 615, 36
N.W.2d 166. In general, the state superintendent is
given the duty ‘[t]o do all things necessary to promote
the welfare of the public schools and public educational
instructions and provide proper educational facilities for
the youth of the state.’ M.S.A. 15.3252, M.C.L.A.
§340.252. See also M.S.A. 15.2299(57), M.C.L.A.
§ 388.717, providing in certain instances for reorganiza
tion of school districts.
14. State officials, including all of the defendants,
are charged under the Michigan constitution with the
duty of providing pupils an education without discrimina
tion with respect to race. Art. VIII, § 2, Mich. Constitu
tion of 1963. Art. I, § 2, of the constitution provides:
No person shall be denied the equal protection
of the laws; nor shall any person be denied the en
joyment of his civil or political rights or be discrimi
nated against in the exercise thereof because of re
ligion, race, color or national origin. The legislature
shall implement this section by appropriate legisla
tion.’ ” 338 F.Supp. at 593-94
Some of the evidence in this record supporting the District
Judge’s findings of State acts which discriminatorily affected
the Detroit Board of Education and contributed to pupil
segregation follows. The State statutory scheme of support of
transportation for school children directly discriminated against
44 Bradley, et al. v. MiUiken, et a l Nos. 72-1809, 72-1814
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 45
Detroit. Dr. John W. Porter, the State Superintendent of
Public Instruction in Michigan, testified as to the State trans
portation aid formula:
Q. (By Mr. Lucas) Dr. Porter, does the State pay
the cost of pupil transportation in the State of Michigan?
“A. The State pays roughly 75 percent of the cost.
Last year the appropriation was $29 million.
“Q. Do you know what percent of the school children
in the State of Michigan are transported to the school
at public expense?
“A. Yes, I do. 40 percent of all students in Michigan
are transported. That equates out to about 833,000 stu
dents last year.
Q. Dr. Porter, is there some formula in terms of
distance which makes a child eligible for transportation
that would be aided by the state?
“A. Yes. It is a very complicated formula that 197
computations, and we are in the process right now of
reducing this —
Q. (Interposing) You mean the financial formula is
complicated. But, in terms of distance from his home
to the school —
A. A mile and a half outside the city limits. Until
this year the legislature amended the Act based upon the
recommendations of the State Board of Education to allow
for in-city transportation which we had never had before.
The legislature did not appropriate funds for that. So,
now the funds that are now used are basically for rural
areas and suburban areas where the students live a mile
and a half from the school.
Q. When you say ‘city,’ is there some limitation?
For instance, would Grosse Pointe, Harper Woods, areas
like that that surround the City of Detroit, are they
eligible for transportation?
A. In the in-city. But, if the students come across
the city boundary lines they live more than a mile and
a half, which is quite prevalent throughout the state,
then they are eligible for the funds.
46 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
“Q. Well, I think my question may have been con
fusing. Is there some type of city — is it just anyplace
incorporated as a city that is differentiated from the rural
areas, or certain cities elegible for this state aid at the
present time and receive the funds —
“THE COURT: I think what Mr. Lucas is trying to
get at is whether under the old practice whether any
city has ceased state aid for transportation within the
city.
“A. Yes, we have a number of instances where the city
would be receiving aid for transportation, because the
law says that if the bus in order to get the students to
the school crosses outside of the city boundary, the city
is then eligible for aid, and we, and we have a number
of instances where that exists.
“THE COURT: In other words, where the student
originates his ride outside the city limits transportation is
assisted?
“A. That’s right, or where the student lives in the
city but the bus has to go outside of the city and come
back he is also eligible. This, however, does not negate
local city officials, school board officials from providing
transportation. There is no prohibition against that.
“Q. ( By Mr. Lucas) You said the legislature changed
the law but didn’t provide the money. Now, they are
eligible for state aid but it is unfunded now, is that what
you are saying?
“A. The law was changed last year to permit in-city
bus transportation but in changing the law the legislature
said our department had to disburse the funds to the
eligible existing areas which meant that since they did
not increase the amount of funds appropriated we could
not provide for in-city transportation.
“Q. If a child lives in the city and lives more than a
mile and a half from the school to which he is assigned
he may not receive the state aid because it is unfunded
at the present time?
“A. That is correct.
“Q. But if he lives the same distance away and lived
outside the City of Detroit, for example, then he could
receive state aide?
“A. That is correct, or any other area.”
The record demonstrates that the State also discriminated
against the Detroit school system by limiting Detroit’s capital
improvement bonding authority to two per cent of assessed
valuation until 1969. This compares with a bonding authority
of five per cent provided for other school districts.
“Q. Mr. Brown, one other question, sir. There has
been a good deal of discussion in the course of this trial
about bonding authority and use made of the funds that
are derived from that authority. I would like to ask
you several questions, sir, about that and see if
we can’t get it all in order. Has the district — and I
ask you this question on the basis of your experience
with the State Board of Education as well as being secre
tary and business manager of the Detroit district — has
the Detroit Board of Education always had bonding au
thority so that bonds could be issued without vote of
the people?
“A. Has it always had?
“Q. Yes, sir, if you know.
“A. I do not know always. It has for many years.
“Q. What was the level of that bonding authority?
“A. It went from 2 percent —
“Q. I am talking about originally from the time you
first knew about it. It was a 2 percent —
“A. 2 percent of equalized valuation that could be
levied by the Board, then it was changed.
“Q. All right. Now, in order to get more than 2
percent of the equalized valuation of the property within
a district what did the Board have to do?
“A. The Board of Education had to take the matter to
the taxpaying electors of the city to get approval to bond
the district beyond that capacity.
“Q. Who is eligible to vote in those bonding elections
at that time?
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 47
“A. At that time the taxpaying electors of the district.
“Q. You mean by that the property owners?
“A. Yes.
“THE COURT: Real estate property owners?
“A. Yes.
“Q. You indicate that that 2 percent authority was
increased. When and how much?
“A. I ’m sorry, I can’t tell you the exact year. It was
increased by 1 percent. It went from 2 to 3, but I
can’t quote the year.
“Q. How did that authority of 3 percent compare
to the authority granted all other districts in the state?
“A. It was less by 2 percent. In other words, all
other districts in the state had the authority to bond up
to 5 percent of the state equalized valuation while Detroit
was limited to 3.
“THE COURT: This is true at a time when Detroit
only had a 2 percent authority?
“A. This is correct.
“Q. Now, sir, when was the authority increased from
3 percent?
“A. During the last session of the Legislature; not the
current one but the one immediately preceding so that
for this year we have the 5 percent authority that the
other districts now have.
“Q. Has that extra authority been utilized by the
district?
“A. No.
“Q. As yet?
“A. Not as yet. The plans are being made and we
have to carry forward quite a program of determining
priorities and so forth, so it has not been used yet.
“Q. So the bonding authority currently being used
by the district is the authority that it had before the
1970 session of the Legislature?
“A. This is correct.
“Q. What is the state of that prior bonding authority?
Is it all exhausted or is there some reserve still available?
48 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 49
“A. It is exhausted to this extent. The Board of Edu
cation has adopted a program which uses all of that au
thority. We have presently before the Municipal Finance
Commission in Lansing the last amount of that authority
and in the amount of $22,950,000. We have not as of
today received approval of that, but the Board’s program
calls for the full authority.”
The clearest example of direct State participation in en
couraging the segregated condition of Detroit public schools,
however, is that of school construction in Detroit and the
surrounding suburban areas. Until 1962 the State Board of
Education had direct statutory control over site planning
for new school construction. During that time, as was pointed
out above, the State approved school construction which
fostered segregation throughout the Detroit Metropolitan area
(See supra pp. 34-40). Since 1962 the State Board has con
tinued to be involved in approval of school construction plans.
IV. Conclusion as to Constitutional Violations
The discriminatory practices on the part of the Detroit
School Board and the State of Michigan revealed by this record
are significant, pervasive and causally related to the substan
tial amount of segregation found in the Detroit school system
by the District Judge.
There is, of course, a significant distinction between this
record and those school segregation cases which have flooded
the courts since Brown v. Topeka, supra. This distinction is
that Michigan has never enforced segregation by State laws
which provided for separate black and white school systems,
as was the pattern prior to 1954 in many other States. As
a consequence, there always have been some instances of
actual school integration in Detroit and still more instances
of token school integration.
Defendants seek to insulate themselves from remedial action
by federal courts by pointing to the long standing public policy
50 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
oi Michigan, as expressed in its statutes, of integration of
public education. However, this court is not blind to the
fact that governments can act only through the conduct of
their officials and employees and that unconstitutional actions
of individuals can be redressed. See, e.g., Clemons v. Board
o f Education, 228 F.2d 853 (6th Cir.), cert, denied, 350 U.S.
1006 (1956).
The record in this case amply supports the findings of the
District Court of unconstitutional actions by public officials
at both the local and State level.
Historically de jure segregation has come about through
statutory command explicitly establishing dual school systems.
Michigan’s declared public policy is urged as a controlling
distinction. No matter how important this distinction may
be, it does not in our judgment negate the de jure segregation
findings entered in this case by the District Judge. The
record contains substantial evidence to support the finding
of the District Court that the segregation of the Detroit public
schools, however rooted in private residential segregation, also
was validated and augmented by the Detroit Board of Educa
tion and Michigan State Board action of pervasive influence
through the system. Even if the segregation practices were
a bit more subtle than the compulsory segregation statutes
of Southern States, they were nonetheless effective. There
should not be one law for the South and a different one
for the North.
It is our view that the findings of fact pertaining to actions
of the Detroit Board of Education and the State of Michigan
which caused or contributed to Detroit school segregation
are not clearly erroneous and that the District Court was
therefore authorized and required to take effective measures
to desegregate the Detroit Public School System. Brown v.
Board o f Education o f T opeka [I], 347 U.S. 483 (1954); Brown
v. Board o f Education o f T opeka [II] , 349 U.S. 294 (1955);
Swann v. Charlotte-M ecklenburg Board of Education, 402 U.S.
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 51
1 (1971); Davis v. Board of Commissioners, 402 U.S. 33
(1971).
This record contains a substantial volume of testimony con
cerning local and State action and policies which helped
produce residential segregation in Detroit and in the metro
politan area of Detroit. In affirming the District Judge’s
findings of constitutional violations by the Detroit Board of
Education and by the State defendants resulting in segregated
schools in Detroit, we have not relied at all upon testimony
pertaining to segregated housing except as school construction
programs helped cause or maintain such segregation.
V. The District Court’s Ruling that no Detroit
Only Desegregation Plan is Possible
Subsequent to the entry of its findings of constitutional
violations on the part of the Detroit Board of Education and
the State of Michigan resulting in system-wide segregation of
Detroit public schools, the District Court requested plans for
Detroit only desegregation. His findings of fact pertaining
to these plans warrant repetition in full:
“FINDINGS OF FACT AND CONCLUSIONS OF LAW
ON
DETROIT-ONLY PLANS OF DESEGREGATION
“In accordance with orders of the court defendant
Detroit Board of Education submitted two plans, limited
to the corporate limits of the city, for desegregation
of the public schools of the City of Detroit, which we
will refer to as Plan A and Plan C; plaintiffs submitted
a similarly limited plan, which will be referred to as the
Foster Plan. Hearings were had on said plans on March
14, 15, 16, 17 and 21, 1972. In considering these plans
the court does not limit itself to the proofs offered at the
hearing just concluded; it considers as part of the evidence
bearing on the issue ( i.e ., City-Only Plans) all proofs sub
mitted in the case to this point, and it specifically incor
porates herein by reference the Findings and Conclusions
contained in its “Ruling on Issue of Segregation,” filed
September 27, 1971.
“The court makes the following factual findings:
“PLAN A.
“1. The court finds that this plan is an elaboration and
extension of the so-called Magnet Plan, previously au
thorized for implementation as an interim plan pending
hearing and determination on the issue of segregation.
“2. As proposed we find, at the high school level,
that it offers a greater and wider degree of specialization,
but any hope that it would be effective to desegregate
the public schools of the City of Detroit at that level is
virtually ruled out by the failure of the current model to
achieve any appreciable success.
“3. We find, at the Middle School level, that the
expanded model would affect, directly, about 24,000
pupils of a total of 140,000 in the grades covered; and
its effect would be to set up a school system within the
school system, and would intensify the segregation in
schools not included in the Middle School program. In
this sense, it would increase segregation.
“4. As conceded by its author, Plan A is neither a
desegregation nor an integration plan.
“PLAN C.
“1. The court finds that Plan C is a token or part-time
desegregation effort.
“2. We find that this plan covers only a portion of
the grades and would leave the base schools no less
racially identifiable.
“PLAINTIFFS’ PLAN
“1. The court finds that Plaintiffs’ Plan would accom
plish more desegregation than now obtains in the system,
or would be achieved under Plan A or Plan C.
“2. We find further that the racial composition of
the student body is such that the plan’s implementation
52 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 53
would clearly make the entire Detroit public school system
racially identifiable as Black.
“3. The plan would require the development of trans
portation on a vast scale which, according to the evidence,
could not be furnished, ready for operation, by the open
ing of the 1972-73 school year. The plan contemplates
the transportation of 82,000 pupils and would require
the acquisition of some 900 vehicles, the hiring and train
ing of a great number of drivers, the procurement of space
for storage and maintenance, the recruitment of main
tenance and the not negligible task of designing a trans
portation system to service the schools.
“4. The plan would entail an overall recasting of the
Detroit school system, when there is little assurance that
it would not have to undergo another reorganization if a
metropolitan plan is adopted.
“5. It would involve the expenditure of vast sums of
money and effort which would be wasted or lost.
“6. The plan does not lend itself as a building block
for a metropolitan plan.
7. The plan would make the Detroit school system
more identifiably Black, and leave many of its schools
75 to 90 per cent Black.
“8. It would change a school system which is now
Black and White to one that would be perceived as
Black, thereby increasing the flight of Whites from the
city and the system, thereby increasing the Black student
population.
“9. It would subject the students and parents, faculty
and administration, to the trauma of reassignments, with
little likelihood that such reassignments would continue
for any appreciable time.
“In summary, we find that none of the three plans
would result in the desegregation of the public schools
of the Detroit school district.
“CONCLUSIONS OF LAW
“1. The court has continuing jurisdiction of this action
for all purposes, including the granting of effective relief.
See Ruling on Issue of Segregation, September 27, 1971.
“2. On the basis of the court’s finding of illegal school
segregation, the obligation of the school defendants is to
adopt and implement an educationally sound, practicable
plan of desegregation that promises realistically to achieve
now and hereafter the greatest possible degree of actual
school desegregation. Green v. County School Board,
391 U.S. 430; Alexander v. H olm es County Board of
Education, 396 U.S. 19; Carter v. W est Feliciana Parish
School Board, 396 U.S. 290; Swann v. Charlotte-M ecklen-
burg Board o f Education, 402 U.S. 1.
3. Detroit Board of Education Plans A and C are
legally insufficient because they do not promise to effect
significant desegregation. Green v. County School Board,
supra, at 439-440.
4. Plaintiffs’ Plan, while it would provide a racial mix
more in keeping with the Black-White proportions of the
student population than under either of the Board’s plans
or as the system now stands, would accentuate the racial
identifiability of the district as a Black school system,
and would not accomplish desegregation.
“5. The conclusion, under the evidence in this case,
is inescapable that relief of segregation in the public
schools of the City of Detroit cannot be accomplished
within the corporate geographical limits of the city. The
State, however, cannot escape its constitutional duty to
desegregate the public schools of the City of Detroit by
pleading local authority. As Judge Merhige pointed out
in Bradley v. Richmond, (slip opinion p. 64):
‘The power conferred by state law on central and
local officials to determine the shape of school at
tendance units cannot be employed, as it has been
here, for the purpose and with the effect of sealing
off white conclaves of a racial composition more ap
pealing to the local electorate and obstructing the
desegregation of schools. The equal protection
clause has required far greater inroads on local gov
ernment structure than the relief sought here, which
is attainable without deviating from state statutory
54 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 55
forms. Compare Reynolds v. Sims, 377 U.S. 533;
Gomillion v. Lightfoot, 364 U.S. 339; Serrano v.
Priest, 40 U.S.L.W. 2128 (Calif.Sup.Ct. Aug. 30,
1971).
‘In any case, if political boundaries amount to in
superable obstacles to desegregation because of struc
tural reason, such obstacles are self-imposed. Politi
cal subdivision lines are creations of the state itself,
after all.’
“School district lines are simply matters of political con
venience and may not be used to deny constitutional
rights. If the boundary lines of the school districts of
the City of Detroit and the surrounding suburbs were
drawn today few would doubt that they could not with
stand constitutional challenge. In seeking for solutions
to the problem of school segregation, other federal courts
have not “treated as immune from intervention the ad
ministrative structure of a state’s educational system, to
the extent that it affects the capacity to desegregate. Geo
graphically or administratively independent units have
been compelled to merge or to initiate or continue co
operative operation as a single system for school de
segregation purposes.”1
“That the court must look beyond the limits of the
Detroit school district for a solution to the problem of
segregation in the Detroit public schools is obvious; that
it has the authority, nay more, the duty to (under the
circumstances of this case) do so appears plainly an
ticipated by Brown II,2 seventeen years ago. While
other school cases have not had to deal with our exact
situation,3 the logic of their application of the command
of Brown II supports our view of our duty.
“FOOTNOTES
Bradley v. Richmond, supra [slip opinion p. 68],
“2 Brown v. Bd. of Ed. of Topeka, 349 U.S. 294, pp. 300-301.
“3 Haney v. County Board of Education of Sevier County,
56 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
410 F.2d 920 (8th Cir. 1969); Bradley v. School Board of the
City of Richmond, supra, slip opinion pp. 664-65; Hall v St
Helena Parish School Board, 197 F.Supp. 649 (E.D. La 1961)
aff’d. 287 F.2d 376 (5th Cir. 1961) and 368 U.S. 515 (1962)- Lee
v. Macon County Bd. of Educ., 448 F.2d 746, 752 (5th Cir 1971) -
Gomillion v. Lightfoot, 364 U.S. 339 (I960); Turner v. Littleton!
Lake Gaston School Dist., 442 F.2d 584 (4th Cir. 1971); United
States v. Texas 447 F.2d 551 (5th Cir. 1971); Lemon v. Bossier
Parish School Board, 446 F.2d 911 (5th Cir 1971) ”
The District Judge s finding that no Detroit only plan
can achieve desegregation of the Detroit public school system
points up another substantial distinction between this case
and the classical school segregation case. This record presents
a wholly new fact pattern in a school segregation case so far
as this Circuit is concerned. C.f. Bradley v. School Board,
City o f Richmond, 338 F.Supp. 67 (E.D. Va. 1971),
rev d, 462 F.2d 1058 (4th Cir. 1972), petition for cert, filed,
41 U.S.L.W. 3211 (U.S. Oct. 5, 1972); see Haney v. County
Board o f Education o f Sevier County, 429 F.2d 364 (8th Cir.
1970). This court never before has been confronted by a
finding that any less comprehensive a solution than a metro
politan area plan would result in an all black school system
immediately surrounded by practically all white suburban
school systems, with an overwhelmingly white majority popu
lation in the total metropolitan area.
Relevant to and supportive of the District Judge’s findings
are these school census figures showing trends toward segre
gation in the Detroit schools during the last decade:
I960 100 of 251 schools were 90% or more white
71 of 251 schools were 90% or more black
68% of all schools were 90% or more one race.
1970 69 of 282 schools were 90% or more white
133 of 282 schools were 90% or more black
71.6% of all schools were 90% or more one race.
1960-61 65.8% of the total number of black students in
regular schools were in 90% or more black schools.
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 57
1970-71 74.9% of the total number of black students in
regular schools were in 90% or more black schools.
This record reflects a present and expanding pattern of
all black schools in Detroit (resulting in part from State ac
tion) separated only by school district boundaries from near
by all white schools. We cannot see how such segregation
can be any less harmful to the minority students than if the
same result were accomplished within one school district.
The boundaries of the Detroit School district are identical to
the geographical boundaries of the City of Detroit. This means
that the Detroit school district, like the City, contains with
in its boundaries two entirely separate cities (and school
districts), Hamtramck and Highland Park, and surrounds a
third City ( and school district), Dearborn, on three sides.
Immediately adjacent to the boundaries of the Detroit school
district are seventeen school districts. An overwhelming ma
jority of these districts, other than Detroit, Highland Park,
River Rouge and Hamtramck, are entirely white or contain
only a token number of black students.
Like the District Judge, we see no validity to an argument
which asserts that the constitutional right to equality before the
law is hemmed in by the boundaries of a school district.
A. Status of School Districts under Michigan Law
This conclusion is supported by the status of school districts
under Michigan law and by the historical control exercised
over local school districts by the legislature of Michigan and
by State agencies and officials, which we now discuss.
It is well established under the Constitution and laws of
Michigan that the public school system is a State function and
that local school districts are instrumentalities of the State
created for administrative convenience.
The Northwest Ordinance of 1787 governing the Territory
of Michigan provided:
58 Bradley, et al. v. MiUiken, et al. Nos. 72-1809, 72-1814
Religion, morality and knowledge, being necessary to
good government and the happiness of mankind, schools
and the means of education shall forever be encouraged.”
Art. III.
With this genesis, Michigan’s four Constitutions have clearly
established that the public school system in that State is solely
a State function. The Constitution of 1835 in Article X,
Section 3, provided, in part: “The legislature shall provide
for a system of common schools . . .” The Constitution of
1850, Article X III, Section 4, provided, in part: “The legis
lature shall . . . provide for and establish a system of primary
schools . . .’ Section 1 of the same Article provided, “. . .
the Superintendent of Public Instruction shall have general
supervision of public instruction . . .”
The Constitution of 1908 in Article XI, Section 2, provided
that the Superintendent of Public Instruction “shall have
general supervision of public instruction in the State.” Article
XI, Section 9, provided, in part as follows:
“The legislature shall continue a system of primary
schools, whereby every school district in the State shall
provide for the education of pupils without charge for
tuition . . . ”
The Constitution of 1963, the present Constitution of the
State of Michigan, in Article VIII, Section 2, provides, in part,
as follows:
“The legislature shall maintain and support a system
of free public elementary and secondary schools as defined
by law.”
In interpereting the above educational provisions of the
Constitution of 1850, the Michigan Supreme Court stated,
“The school district is a State agency. Moreover, it is of
legislative creation . . .” Attorney General v. Low rey, 131
Mich. 639, 644, 92 N.W. 289, 290 (1902). Again, interpreting
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 59
the Constitution of 1850, the Supreme Court of Michigan in
Attorney General v. Detroit Board o f Education, 154 Mich.
584, 590, 118 N.W. 606, 609 (1908), adopted lower court
language which read:
“Education in Michigan belongs to the State. It is no
part of the local self-government inherent in the township
or municipality, except so far as the legislature may chose
to make it such. The Constitution has turned the whole
subject over to the legislature . . .”
The Supreme Court of Michigan interpreted Article XI,
Section 9, of the Constitution of 1908 to mean:
“The legislature has entire control over the schools
of the State subject only to the provisions above referred
to. The division of the territory of the State into districts,
the conduct of the school, the qualifications of teachers,
the subjects to be taught therein are all within its con
trol.” Child W elfare v. Kennedy School Dist., 220 Mich.
290, 296, 189 N.W. 1002, 1004 (1922).
In the leading case concerning construction of this section
of the Michigan Constitution of 1963, the Michigan Supreme
Court said:
“It is the responsibility of the State board of education
to supervise the system of free public schools set up by
the legislature and, as a part of that responsibility, to
promulgate regulations specifying the number of hours
necessary to constitute a school day for elementary school
students as well as for other classifications or groupings
of students, to determine the curricula and, in general,
to exercise leadership and supervision over the public
school system.” W elling v. Livonia Board o f Education,
382 Mich. 620, 624, 171 N.W.2d 545, 546 (1969).
Michigan has not treated its school districts as sacrosanct.
To the contrary, Michigan always has regarded education as
the fundamental business of the State as a whole. Local
60 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
school districts are creatures of the State and act as instru
mentalities of the State under State control. Cf. Senghas v.
L ’Anse Creuse Public Schools, 368 Mich. 557, 118 N.W.2d
975 (1962); McLaughlin v. Board o f Education, 255 Mich.
667, 239 N.W. 374, (1931).
The record discloses a number of examples of State control
over local public education in Michigan.
1. Following the holding of W elling v. Livonia Board of
Education, supra, that there was no minimum length of day
required under the 180-day school attendance rule absent a
State Board of Education regulation, the Michigan State
Board of Education, acting under its Constitutional mandate
without legislative authority, established an administrative
rule requiring local school boards to provide a minimum
number of hours per school year. See, School Districts Child
Account for Distribution o f State Aid, Bulletin No. 1005,
Michigan State Department of Education (1970).
2. Public Act 289 of 1964 (MSA § 15.2299 (1 ) et seq.,
MCLA § 388.681 et s eq .) required Michigan school districts
to operate K-12 systems. When Public Act 289 became ef
fective, 1,438 public school districts existed in Michigan. By
the beginning of 1968, this figure had been reduced to 738,
meaning that 700 school districts in Michigan have disap
peared since 1964 through reorganization. Annual Report,
Committee on School District Reorganization, 1968 Journal
of the Senate 422-423 (March 1, 1968).
3. Pursuant to Act 289 of 1964, supra, the State Board of
Education ordered the merger of the Brownstown No. 10,
Hand, Maple Grove and Carson school districts, all in Wayne
County. The action is best explained by the fact that Browns
town was, at that time, the wealthiest school district in the
State, indeed, with a property valuation of $340,000 backing
each child, perhaps the wealthiest district in the nation, while
the other three districts were extremely poor.
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 61
4. When the Sumpter School District was on the verge of
bankruptcy in 1968, the State Board of Education, acting
under Public Act 239 of 1967 (MSA § 15.2299(51) et seq.,
MCLA § 388.691 et seq .) , merged the district with four
adjoining districts, including the Airport School District.
Significantly, though Sumpter was in Wayne County, Airport
was in Monroe County, showing that county lines are not
inviolate in Michigan.
5. The Nankin Mills School District in Wayne County was
beset with financial problems and had no high school. Again,
pursuant to Act 239, the State Board of Education in 1969
ordered this school district to merge with the Livonia, Garden
City and Wayne Community schools.
6. When the Inkster School District in Wayne County was
on the verge of financial bankruptcy, the Michigan legislature
passed Public Act 32 of 1968 (MSA § 15.1916 et seq., MCLA
§ 388.201 et s eq . ) enabling the district to borrow $705,000
but on the condition that if the district could not balance its
budget, the State Board of Education could reorganize, merge
or annex the district. The legislative history of Act 32 indicates
at least two legislators voted against the bill in the House of
Representatives because of the excessive control given to the
State Board of Education:
“I voted No on House Bill No. 3332 because in setting
up the machinery to bail out distressed districts, it takes
from the local communities the control over their own
educational system by providing for excessive arbitrary
reorganization powers in the hands of the Board of
Education. . .”
“This bill certainly sets up the State Board of Educa
tion to be a dictator of all school districts that run into
financial problems.” 1968 Journal of the House of Repre
sentatives 1965.
7. Too small and too poor to operate a high school, the all
black Carver School District in suburban Oakland County
62 Bradley, et al. v. MiUiken, et al. Nos. 72-1809, 72-1814
reached a crisis in 1960 when surrounding white districts
refused to accept Carver pupils on a tuition basis. The Gov
ernor and Superintendent of Public Instruction helped to
merge the Carver district with Oak Park.
8. The State Board of Education and Superintendent of
Public Instruction may withhold State aid for failure to
operate the minimum school year. MSA § 15.3575, MCLA
§ 340.575. In 1970, funds were withheld from the City of
Grand Rapids School District. 17 Michigan School Board
Journal 3 (March, 1970). For Attorney General Opinions
holding that State aid may be withheld by the State Board of
Education from school districts for hiring uncertified teachers,
defaulting on State loans and for other reasons, see Op. Atty.
Gen. No. 880, 1949-1950 Report of the Attorney General 104
(January 24, 1949, Roth); No. 2333, 1955 Report of the At
torney General 561 (October 20, 1955, Kavanaugh); No.
4097, 1961-1962 Report of the Attorney General 553 ( October
8, 1962, Kelley).
9. The State of Michigan contributes, on the average, 34%
of the operating budgets of the 54 school districts included
in the Metropolitan Plan of Integration. In eleven of the 54
districts, the State’s contribution exceeds 50% and in eight
more, it exceeds 40%. State aid is appropriated from the Gen
eral Fund, revenue raised through state-wide taxation, and
is distributed annually to the local school districts under a
formula devised by the legislature. See, e. g., Public Act 134
(1971), MSA §15.1919(51), MCLA §388.611.
Though the local school districts obtain funds from the
assessment of local property, the ultimate authority in insur
ing equalized property valuations throughout the State is the
State Tax Commission. MSA § 7.631, et seq., MCLA § 209.101,
et seq .; MSA § 7.206, MCLA § 211.148; MSA § 7.52, MCLA
§ 211.34. The State’s duty to equalize is required by the
Michigan Constitution, Article IX, Section 3. This “State
equalized valuation” serves as the basis for calculating local
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 63
revenue yields. See, Ranking o f Michigan Public High School
— School Districts by Selected Financial Data, 1970, Bulletii
1012, Michigan State Department of Education (1971).
10. The Michigan School Code reaffirms the ultimate con
trol of the State over public education. Local school districts
must observe all State laws relating to schools,’ hold school a
minimum number of days per year,* 2 employ only certified
teachers,3 teach civics, health and physical education and
drivers’ education,4 excuse students to attend religious instruc
tion classes,5 observe State requirements when teaching sex
education,6 make annual financial and other reports to the
Superintendent of Public Instruction,7 adopt only textbooks
which are listed with the Superintendent of Public Instruc
tion8 and must follow all rules and regulations of the State
Department of Education.
Local school districts, unless they have the approval of
the State Board of Education or the Superintendent of Public
Instruction, cannot consolidate with another school district,9
annex territory,10 11 12 divide or attach parts of other districts,’ 1
borrow monies in anticipation of State aid,’2 construct, re
r MSA § 15.3252(c), M CLA § 340.252(c).
2 MSA § 15.3575, M CLA § 340.575.
3 MSA §§ 15.1023(10) (a ), 15.3570, M CLA §§ 388.1010(a ) , 340.570.
4 M SA §§ 15.1951,15.3361, M CLA §§ 388.371, 340.361; MSA §§ 15.3781-
15.3782, M CLA §§340.781-340.782; MSA § 9.2511(c), M CLA § 257.811
(c ).
5 MSA § 15.3732(g), M CLA § 340.732(g).
« MSA § 15.3789, M CLA § 340.789.
7 MSA § 15.3612, M CLA § 340.612; MSA §§ 15.3616, 15.3688, MCLA
§§ 340.616, 340.688.
8 MSA § 15.3887(1), M CLA § 340.887(1).
9 MSA § 15.3402, M CLA § 340.402.
10 MSA § 15.3431, M CLA § 340.431.
11 MSA § 15.3447, M CLA § 340.447.
12 MSA § 15.3567(1), M CLA § 340.567(a).
64 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
construct or remodel school buildings or additions to them,13
establish a program for the prevention and treatment of
behavior problems of children,14 employ a superintendent
without a bachelor’s degree from a college acceptable to
the State Board of Education,15 establish facilities and pro
grams for the day care of the physically handicapped or
initiate programs for the mentally handicapped.15
The power to withhold State aid, of course, effects enormous
leverage upon any local school district, since on the average
34 per cent of the operation budget of the 54 school districts
included in the Metropolitan Plan is paid for by the State.
In the instance of the City of Detroit, the State exhibited
its understanding of its power over the local school district
by the adoption of Act 48 of the Public Acts of 1970 which
repealed a high school desegregation plan previously adopted
by the Detroit Board of Education.
B. De Jure Acts of Desegregation
Thus, the record establishes that the State has committed
de jure acts of segregation and that the State controls the
instrumentalities whose action is necessary to remedy the
harmful effects of the State acts. There can be little doubt
that a federal court has both the power and the duty to
effect a feasible desegregation plan. Indeed, such is the
essence of Brown II. Brown v. Board o f Education, 349 U.S.
294, 300-01 (1955). In the instant case the only feasible
desegregation plan involves the crossing of the boundary lines
between the Detroit School District and adjacent or nearby
school districts for the limited purpose of providing an effective
'3 M SA §15.1961, M CLA §388.851, Op. Atty. Gen. No. 1837, 1952-
1954 Report of the Attorney General 440 (Nov. 8 1954).
14 MSA § 15.3618, M CLA § 340.616.
is MSA § 15.3573, M CLA § 340.573.
is M SA § 15.3587(1), M CLA § 340.587(a); MSA § 15.3775, M CLA
§ 340.775.
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 65
desegregation plan. The power to disregard such artificial
barriers is all the more clear where, as here, the State has
been guilty of discrimination which had the effect of creating
and maintaining racial segregation along school district lines.
See Section III B, pp. 41-49, supra. United States v. Scotland
N eck Board o f Education, 407 U.S. 484, 489 (1972); Wright
v. City o f Emporia, 407 U.S. 451, 463 (1972); United States v.
State o f Texas, 447 F.2d 441, 443-44 (5th Cir. 1971); Haney v.
County Board o f Education o f Sevier County, 429 F.2d 364,
368 (8th Cir. 1970). See also Davis v. Board o f School Com
missioners, 402 U.S. 33, 36-38 (1971).
There exists, however, an even more compelling basis for
the District Court’s crossing artificial boundary lines to cure
the State’s constitutional violations. The instant case calls
up haunting memories of the now long overruled and dis
credited “separate but equal doctrine” of Plessy v. Ferguson,
163 U.S. 537 (1896). If we hold that school district bound
aries are absolute barriers to a Detroit school desegregation
plan, we would be opening a way to nullify Brown v. Board
of Education which overruled Plessy, supra.
This court in considering this record finds it impossible
to declare “clearly erroneous” the District Judge’s conclusion
that any Detroit only desegregation plan will lead directly
to a single segregated Detroit school district overwhelmingly
black in all of its schools, surrounded by a ring of suburbs and
suburban school districts overwhelmingly white in composition
in a State in which the racial composition is 87 per cent
white and 13 per cent black. Big city school systems for
blacks surrounded by suburban school systems for whites can
not represent equal protection of the law.
VI. The District Judge’s Order to Prepare A
Metropolitan Area Desegregation Plan
The third major issue in this case pertains to the validity
of the District Judge’s ruling on desegregation area and order
for development of a plan of desegregation dated June 14,
66 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
1972, accompanied by a statement of findings of facts and
conclusions of law in support thereof.
At the outset it is obvious from what we have said pertain
ing to the inadequacy of any Detroit only desegregation plan
that this court feels that some plan for desegregation beyond
the boundaries of the Detroit School District is both within
the equity powers of the District Court and essential to a
solution of this problem. We reiterate this, keeping in mind
the admonition from Chief Justice Marshall:
“The government of the United States has been
emphatically termed a government of laws, and not of
men. It will certainly cease to deserve this high appel
lation, if the laws furnish no remedy for the violation
of a vested legal right.” Marbury v. Madison, 5 U.S.
(1 Cranch) 137, 163 (1803).
We reject the contention that school district fines are
sacrosanct and that the jurisdiction of the District Court to
grant equitable relief in the present case is limited to the
geographical boundaries of Detroit. We reiterate that school
districts and school boards are instrumentalities of the State.
See C ooper v. Aaron, 358 U.S. 1, 16 (1958). As early as
Brown II the Supreme Court pointed out that:
“[T]he courts may consider problems related to ad
ministration, arising from the physical condition of the
school plant, the school transportation system, person
nel, revision of school districts and attendance areas into
compact units to achieve a system of determining admis
sion to the public schools on a nonracial basis, . . . .” 349
U.S. at 300-01.
The Supreme Court has held that school boundary fines
cannot be changed or new school systems created where the
result is a larger imbalance in racial ratios in school systems
where all vestiges of enforced racial segregation have not been
eliminated. United States v. Scotland N eck Board o f Edu
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 67
cation, 407 U.S: 484 (1972); Wright v. Council o f the City
oj Emporia, 407 U.S. 451 (1972). This is true regardless of
“dominant purpose.” Wright v. City o f Emporia, 407 U.S. at
462.
If school boundary lines cannot be changed for an uncon
stitutional purpose, it follows logically that existing boundary
lines cannot be frozen for an unconstitutional purpose.
We therefore conclude that the District Court in the present
case is not confined to the boundary lines of Detroit in fash
ioning equitable relief.
To the extent that this opinion is in conflict with Bradley
v. School Board o f Richmond, 462 F.2d 1058 (4th Cir. 1972),
petition for cert, filed, 41 U.S.L.W. 3211 (U.S. Oct. 5, 1972),
we respectfully decline to follow that decision.
VII. Rights of Other School Districts To Be
Made Parties and To Be Heard
In his “Ruling on Propriety of Considering a Metropolitan
Remedy” the District Court defined the metropolitan area
“for the present purposes” to comprise the three counties of
Wayne, Oakland and Macomb. In his “Findings of Fact and
Conclusions of Law in Support of Ruling on Desegregation
Area and Development Plans” the District Court noted that
“the court has taken no proofs with respect to the establish
ment of the boundaries in the counties of Wayne, Oakland
and Macomb.” In his “Ruling on Desegregation Area and
Order for Development of Plan of Segregation” the District
Court defined the desegregation area to include some 53
school districts. Certain of these school districts have inter
vened in this case, but have not yet been afforded an oppor
tunity to offer proof. Some of the other school districts are
not parties to the litigation.
Under the authorities heretofore discussed, these school
districts are arms and instrumentalities of the State of Michi
gan. Nevertheless, under Michigan law, they may sue and
be sued. See 11 M.S.A. §§ 15.3154, 15.3192.
68 Bradley, et al. v. Milliken, el ah Nos. 72-1809, 72-1814
Rule 19, Fed. R. Civ. P. provides that a person who is
subject to service of process shall be joined as a party to
the action if “in his absence complete relief cannot be ac
corded among those already parties/’ Under this rule joinder
of necessary parties is required if jurisdiction over them can
be obtained and if joinder will not defeat federal jurisdiction
of the case. See Bradley v. School Board o f City o f Richmond,
51 F.R.D. 139 (E.D . Va. 1970).
We hold that school districts which are to be affected by
the decree of the District Court are “necessary parties” under
Rule 19. As a prerequisite to the implementation of a plan
in this case affecting any school district, the affected district
first must be made a party to this litigation and afforded an
opportunity to be heard.
While agreeing with the District Court in its conclusion that
it can consider a metropolitan remedy, we express no views
as to the desegregation area set forth in the orders of the
District Court.
We vacate the order of March 28, 1972, entitled “Ruling
on Propriety of a Metropolitan Remedy to Accomplish De
segregation of the Public Schools of Detroit.” For the guid
ance of the District Court on remand, however, we hold that,
in fashioning an equitable remedy in this case, it will not be
necessary for the District Court to find discriminatory' conduct
on the part of each school district, either de jure or de facto,
as a prerequisite to including such district in a desegregation
area to be defined by the court’s decree.
As said in United States v. Texas Education A g en cy ,-------
F .2 d ---- (5th Cir. 1972):
“Some schools may be the ‘result’ of state-imposed
segregation even though no specific discriminatory school
board action may be shown as to those schools. Had the
school authorities not specifically segregated the minority
students in certain schools, other schools may have
developed as desegregated facilities. Thus, though they
may not be ‘pockets of discrimination,’ these schools are
Nos, 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 69
the ‘results’ of discrimination.” United States v. Texas
Education Agency, su p ra ,-------F.2d a t -------- .
We also vacate the District Court’s Ruling on Desegrega
tion Area and Development Plan, dated June 14, 1972, except
those parts of the order appointing a panel charged with the
duty of preparing interim and final plans of desegregation.
The panel appointed by the District Court is authorized to
proceed with its studies and planning under the direction of
the District Court. Pending further orders of the District
Court or this Court, the defendants and school districts in
volved will continue to supply administrative and staff assist
ance to the panel upon its request. Until further order of
the court, the reasonable costs incurred by the panel will be
paid as provided by the District Court’s order of June 14, 1972.
The order of the District Court directing the purchase of
school buses, dated July 11, 1972, also is vacated, subject to the
right of the District Court, in its discretion, to consider the
entry of another order requiring the purchase of school buses
at the appropriate time.
VIII. Equitable Relief
In this opinion we have emphasized the broad powers of
a District Court to fashion equitable relief in school desegre
gation cases. For the guidance of the District Court on remand,
we now review the decisions on this subject in further depth.
1) The Fundamental Constitutional Holding:
“We conclude that in the field of public education the
doctrine of ‘separate but equal’ has no place. Separate
educational facilities are inherently unequal. Therefore,
we hold that the plaintiffs and others similarly situated
for whom the actions have been brought are, by reason
of the segregation complained of, deprived of the equal
protection of the laws guaranteed by the Fourteenth
Amendment.” Brown v. Board o f Education, 347 U.S.
483, 495 (1954).
70 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
2) The Supreme Court’s Initial Description of the Equitable
Remedy:
“In fashioning and effectuating the decrees, the courts
will be guided by equitable principles. Traditionally,
equity has been characterized by a practical flexibility in
shaping its remedies4 and by a facility for adjusting and
reconciling public and private needs.5 These cases call
for the exercise of these traditional attributes of equity
power. At stake is the personal interest of the plaintiffs
in admission to public schools as soon as practicable on a
nondiscriminatory basis. To effectuate this interest may
call for elimination of a variety of obstacles in making
the transition to school systems operated in accordance
with the constitutional principles set forth in our May 17,
1954, decision. Courts of equity may properly take into
account the public interest in the elimination of such
obstacles in a systematic and effective manner. But it
should go without saying that the vitality of these con
stitutional principles cannot be allowed to yield simply
because of disagreement with them.
“While giving weight to these public and private con
siderations, the courts will require that the defendants
make a prompt and reasonable start toward full compli
ance with our May 17, 1954, ruling. Once such a start
has been made, the courts may find that additional time
is necessary to carry out the ruling in an effective man
ner. The burden rests upon the defendants to establish
that such time is necessary in the public interest and is
consistent with good faith compliance at the earliest
practicable date. To that end, the courts may consider
problems related to administration, arising from the
physical condition of the school plant, the school trans
portation system, personnel, revision of school districts
and attendance areas into compact units to achieve a
system of determining admission to the public schools on
a nonracial basis, and revision of local laws and regula-
4 See A le x a n d e r v. H illm a n , 296 U.S. 222, 239.
s See H ec h t Co. v. B o w les, 321 U.S. 321, 329-330.
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 71
tions which may be necessary in solving the foregoing
problems. They will also consider the adequacy of any
plans the defendants may propose to meet these prob
lems and to effectuate a transition to a racially nondis-
criminatory school system. During this period of
transition, the courts will retain jurisdiction of these cases.”
Brown v. Board o f Education o f Topeka [11], 349 U.S.
294, 300-01 (1955)
3) Delay Is No Longer Tolerable:
“In determining whether respondent School Board met
that command by adopting its ‘freedom-of-choice’ plan,
it is relevant that this first step did not come until some
11 years after Brown I was decided and 10 years after
Brown I I directed the making of a ‘prompt and reason
able start.’ This deliberate perpetuation of the uncon
stitutional dual system can only have compounded the
harm of such a system. Such delays are no longer toler
able, for ‘the governing constitutional principles no longer
bear the imprint of newly enunciated doctrine.’ Watson
v. City o f Me?nphis, supra, at 529; see Bradley v. School
Board, supra; Rogers v. Paid, 382 U.S. 198. Moreover,
a plan that at this late date fails to provide meaningful
assurance o f prom pt and effective disestablishment o f a
dual system is also intolerable. ‘The time fqr mere
‘deliberate speed’ has run out,’ Griffin v. County School
Board, 377 U.S. 218, 234; ‘the context in which we must
interpret and apply this language [of Brown II] to plans
for desegregation has been significantly altered.’ Goss
v. Board o f Education, 373 U.S. 683, 689. See Calhoun
v. Latimer, 377 U.S. 263. The burden on a school board
today is to com e forward with a plan that promises
realistically to work, and promises realistically to work
now.” Green v. County School Board, 391 U.S. 430, 438-
39 (1968) ( Emphasis added.)
4) State Imposed Segregation Must be Completely Removed
at Earliest Practicable Date:
“The obligation of the district courts, as it always has
72 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
been, is to assess the effectiveness of a proposed plan
in achieving desegregation. There is no universal answer
to complex problem s o f desegregation; there is obvious
ly no one plan that will do the job in every case. The
matter must be assessed in light o f the circumstances
present and the options available in each instance. It
is incumbent upon the school board to establish that its
proposed plan promises meaningful and immediate
progress toward disestablishing state-imposed segregation.
It is incumbent upon the district court to weigh that
claim in light of the facts at hand and in light of any
alternatives which may be shown as feasible and more
promising in their effectiveness. W here the court finds
the board to b e acting in good faith and the proposed
plan to have real prospects for dismantling the state-
im posed dual system ‘at the earliest practicable date,’
then the plan may be said to provide effective relief.
Of course, the availability to the board of other more
promising courses of action may indicate a lack of good
faith; and at the least it places a heavy burden upon the
board to explain its preference for an apparently less
effective method. Moreover, whatever plan is adopted
will require evaluation in practice, and the court should
retain jurisdiction until it is clear that state-imposed seg
regation has been completely removed. See No. 805,
Raney v. Board o f Education, post, at 449.” Green v.
County School Board, 391 U.S. 430, 439 (1968) (Empha
sis added.)
5) The Court Has The Power and The Duty to Eliminate
Effects of Past Discrimination:
“W e bear in mind that the court has not merely the
pow er but the duty to render a decree w hich will so far
as possible eliminate the discriminatory effects o f the
past as w ell as bar like discrimination in the future.”
Louisiana v. United States, 380 U. S. 145, 154. Com
pare the remedies discussed in, e. g., NLRB v. Newport
News Shipbuilding & Dry D ock Co., 308 U. S. 241; United
States v. Crescent Amusement Co., 323 U. S. 173; Stand
Nos. 72-1809, 72-1814 Bradley, et al. v. MiUiken, et al. 73
ard Oil Co. v. United States, 221 U. S. 1. See also
Griffin v. County School Board, 377 U. S. 218, 232-234.
Green v. County School Board, 391 U.S. 430, n. 4 at 438
(relating to the remedial command of Brown II) (Em
phasis added.)
6) Resegregation is Impermissible:
“Like the transfer provisions held invalid in Goss v. Board
of Education, 373 U.S. 683, 686, ‘[i]t is readily apparent
that the transfer [provision] lends itself to perpetuation
of segregation.’ While we there indicated that ‘free-
.ransfer’ plans under some circumstances might be valid,
we explicitly stated that ‘no official transfer plan or
provision o f which racial segregation is the inevitable
consequence may stand under the Fourteenth Amend
ment.’ Id., at 689. So it is here; no attempt has been
made to justify the transfer provision as a device de
signed to meet ‘legitimate local problems,’ ibid.; rather
it patently operates as a device to allow resegregation
of the races to the extent desegregation would be
achieved by geographically drawn zones. Respondent’s
argument in this Court reveals its purpose. We are
frankly told in the Brief that without the transfer option
it is apprehended that white students will flee the school
system altogether. ‘But it should go without saying
that the vitality of these constitutional principles cannot
be allowed to yield simply because of disagreement with
them.’ Brown II, at 300.
“We do not hold that ‘free transfer’ can have no place
in a desegregation plan. But like ‘freedom of choice,’
if it cannot be shown that such a plan will further rather
than delay conversion to a unitary, nonracial, nondis-
eriminatory school system, it must be held unacceptable.
See Green v. County School Board, supra, at 439-441.
“W e conclude, therefore, that the Board ‘must be re
quired to formulate a new plan and , in light o f other
courses which appear open to the Board. . . . fashion
74 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
steps which promise realistically to convert promptly to
a system without a ‘w hite’ school and a ‘Negro’ school,
hut just schools.” Id., at 442. Monroe v. Board o f Com
missioners, 391 U.S. 450, 459-60 (1968) (Emphasis
added.)
7) The Remedial Tools:
In Swann v. Board o f Education, 402 U.S. 1, 15, Chief Justice
Burger, writing for a unanimous Court, said:
“If school authorities fail in their affirmative obligations
under these holdings, judicial authority may be invoked.
Once a right and a violation have been shown, the scope
of a district court’s equitable powers to remedy past
wrongs is broad, for breadth and flexibility are inherent
in equitable remedies.
‘The essence of equity jurisdiction has been the
power of the Chancellor to do equity and to mould
each decree to the necessities of the particular case.
Flexibility rather than rigidity has distinguished it.
The qualities of mercy and practicality have made
equity the instrument for nice adjustment and recon
ciliation between the public interest and private
needs as well as between competing private claims.’
H echt Co. v. Bowles, 321 U.S. 321, 329-330 (1944),
cited in Brown II, supra, at 300.”
a) The Flexible Ratio:
“As the voluminous record in this case shows, the
predicate for the District Court’s use of the 71%-29%
ratio was twofold: first, its express finding, approved by
the Court of Appeals and not challenged here, that a
dual school system had been maintained by the school
authorities at least until 1969; second, its finding, also
approved by the Court of Appeals, that the school board
had totally defaulted in its acknowledged duty to come
forward with an acceptable plan of its own, notwithstand
ing the patient efforts of the District Judge who, on
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 75
at least three occasions, urged the board to submit plans.
As the statement of facts shows, these findings are1
abundantly supported by the record. It was because of
this total failure of the school board that the District
Court was obliged to turn to other qualified sources, and
Dr. Finger was designated to assist the District Court to
do what the board should have done.
“We see therefore that the use made of mathematical
ratios was no more than a starting point in the process
of shaping a remedy, rather than an inflexible require
ment. From that starting point the District Court pro
ceeded to frame a decree that was within its discre
tionary powers, as an equitable remedy for the particu
lar circumstances. As we said in Green, a school authori
ty’s remedial plan or a district court’s remedial decree is
to be judged by its effectiveness. Awareness of the racial
composition of the whole school system is likely to be
a useful starting point in shaping a remedy to correct
past constitutional violations. In sum, the very limited
use made of mathematical ratios was within the equitable
remedial discretion of the District Court.” Swann v.
Board o f Education, 402 U.S. 1, 24-25 (1970).
b) Noncontiguous School Zoning:
“The maps submitted in these cases graphically dem
onstrate that one of the principal tools employed by
school planners and by courts to break up the dual school
system has been a frank — and sometimes drastic —
gerrymandering of school districts and attendance zones.
An additional step was pairing, ‘clustering,’ or ‘grouping’
of schools with attendance assignments made deliberate
ly to accomplish the transfer of Negro students out of
formerly segregated Negro schools and transfer of white
students to formerly all-Negro schools. More often than
not, these zones are neither compact nor contiguous;
indeed they may be on opposite ends of the city. As an
interim corrective measure, this cannot be said to be
beyond the broad remedial powers of a court.
76 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
“Absent a constitutional violation there would be no
basis for judicially ordering assignment of students on a
racial basis. All things being equal, with no history of
discrimination, it might well be desirable to assign pupils
to schools nearest their homes. But all things are not
equal in a system that has been deliberately constructed
and maintained to enforce racial segregation. The reme
dy for such segregation may be administratively awkward,
inconvenient, and even bizarre in some situations and
may impose burdens on some; but all awkwardness and
inconvenience cannot be avoided in the interim period
when remedial adjustments are being made to eliminate
the dual school systems.
“No fixed or even substantially fixed guidelines can
be established as to how far a court can go, but it must
be recognized that there are limits. The objective is
to dismantle the dual school system. ‘Racially neutral’
assignment plans proposed by school authorities to a dis
trict court may be inadequate; such plans may fail to
counteract the continuing effects of past school segrega
tion resulting from discriminatory location of school sites
or distortion of school size in order to achieve or main
tain an artificial racial separation. When school authori
ties present a district court with a ‘loaded game board,’
affirmative action in the form of remedial altering of
attendance zones is proper to achieve truly non-discrim-
inatory assignments. In short, an assignment plan is not
acceptable simply because it appears to be neutral.
“In this area, we must of necessity rely to a large ex
tent, as this Court has for more than 16 years, on the
informed judgment of the district courts in the first in
stance and on courts of appeals.
“W e hold that the pairing and grouping o f noncontigu
ous school zones is a permissible tool and such action is
to be considered in light o f the objectives sought. Judicial
steps in shaping such zones going beyond combinations
of contiguous areas should be examined in light of what
is said in subdivisions (1) , (2) , and (3) of this opinion
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al, 77
concerning the objectives to be sought. Maps do not
tell the whole story since noncontiguous school zones
may be more accessible to each other in terms of the
critical travel time, because of traffic patterns and good
highways, than schools geographically closer together.
Conditions in different localities will vary so widely that
no rigid rules can be laid down to govern all situations.”
Swann v. Board o f Education, supra, at 27-29. (Empha
sis added.)
c) Transportation of Students:
“The scope of permissible transportation of students as
an implement of a remedial decree has never been de
fined by this Court and by the very nature of the problem
it cannot be defined with precision. No rigid guidelines
as to student transportation can be given for application
to the infinite variety of problems presented in thousands
of situations. Bus transportation has been an integral
part of the public education system for years, and was
perhaps the single most important factor in the transi
tion from the one-room schoolhouse to the consolidated
school. E ighteen million o f the N ations public school
children, approximately 39%, were transported to their
schools by bus in 1969-1970 in all parts o f the country.
“The importance of bus transportation as a normal and
accepted tool of educational policy is readily discernible
in this and the companion case, Davis, supra. The Char
lotte school authorities did not purport to assign students
on the basis of geographically drawn zones until 1965
and then they allowed almost unlimited transfer privi
leges. The District Court’s conclusion that assignment
o f children to the school nearest their hom e serving their
grade would not produce an effective dismantling o f the
dual system is supported by the record.
“Thus the rem edial techniques used in the District
Court’s order were within that court’s pow er to pro
vide equitable relief; im plem entation o f the decree is
well within the capacity o f the school authority.
The decree provided that the buses used to implement
the plan would operate on direct routes. Students would
be picked up at schools near their homes and trans
ported to the schools they were to attend. The trips
for elementary school pupils average about seven miles
and the District Court found that they would take “not
over 35 minutes at the most.” This system compares
favorably with the transportation plan previously operated
in Charlotte under which each day 23,600 students on
all grade levels were transported an average of 15 miles
one way for an average trip requiring over an hour. In
these circumstances, we find no basis for holding that the
local school authorities may not be required to employ
bus transportation as one tool of school desegregation.
Desegregation plans cannot be limited to the walk-in
school.
“An objection to transportation o f students may have
validity when the tim e or distance o f travel is so great
as to either risk the health o f the children or significantly
impinge on the educational process. District courts must
weigh the soundness of any transportation plan in light
of what is said in subdivisions (1) , (2) , and (3) above.
It hardly needs stating that the limits on time of travel
will vary with many factors, but probably with none
more than the age of the students. The reconciliation of
competing values in a desegregation case is, of course, a
difficult task with many sensitive facets but fundamentally
no more so than remedial measures courts of equity have
traditionally employed.” Swann v. Board o f Education,
supra, at 29-31. (Emphasis added.)
In North Carolina v. Swann, 402 U.S. 43, 46, the Chief
Justice said: “As noted in Swann, supra, at 29, bus transporta
tion has long been an integral part of all educational sys
tems, and it is unlikely that a truly effective remedy could
be devised without continued reliance on it.”
78 Bradley, et al. v. Milliken, et al. Nos. 72-1809, 72-1814
Nos. 72-1809, 72-1814 Bradley, et al. v. Milliken, et al. 79
d) Equity Power to Require Payment of Tax Funds for
Integrated Schools:
In the exercise of its equity powers, a District Court may
order that public funds be expended, particularly when such
an expenditure is necessary to meet the minimum requirements
mandated by the Constitution. Griffin v. County School Board
o f Prince Edw ard County, 377 U.S. 218, 233 (1964); Eaton v.
New H anover County Board o f Education, 459 F.2d 684 (4th
Cir. 1972); Brewer v. School Board o f City o f Norfolk, 456
F.2d 943, 947, 948 (4th Cir.), cert, denied, 406 U.S. 933
(1972); Plaquemines Parish School Board v. United States,
415 F.2d 817 (5th Cir. 1969).
These and other cases cited in this opinion outline the
broad scope of equitable relief that may be fashioned by the
District Court in this case on remand after all school districts
to be affected are afforded an opportunity to be heard as
hereinabove provided.
IX. Other Issues
Numerous other issues are presented which do not require
discussion.
We do not consider it necessary to construe the “Broom
field Amendment,” Pub. L. No. 92-318, 86 Stat. 235, § 803,
known as the Education Amendments of 1972, since no final
desegregation order has been entered.
Deal v. Cincinnati Board o f Education, 419 F.2d 1387, 1392
(6th Cir. 1969), cert, denied, 402 U.S. 962 (1971) is not con
trolling. There the District Court made findings of fact that
there had been no unconstitutional conduct on the part of
the Cincinnati Board of Education. This court held that
these findings of fact were not clearly erroneous. Rule 52(a) ,
Fed. R. Civ. P.
All other contentions presented by the appellants have been
considered and are found to be without merit.
80 Bradley, et al, v. Milliken, et al. Nos. 72-1809, 72-1814
X. Conclusion
1. The Ruling of the District Court on the Issue of Segre
gation, dated September 27, 1971, and reported at 338 F.Supp.
582, is affirmed.
2. The findings of fact and conclusions of law on “Detroit-
only” plans of desegregation, dated March 28, 1972, are af
firmed.
3. The Ruling on Propriety of a Metropolitan Remedy to
Accomplish Desegregation of the Public Schools of the City
of Detroit, dated March 24, 1972, is affirmed in part, but
vacated for the reasons set forth above.
4. The Ruling on Desegregation Area and Development
of Plan, dated June 14, 1972, is vacated except as hereinabove
prescribed.
5. The order dated July 11, 1972, directing the purchase
of school buses is vacated.
The case is remanded to the District Court for further
proceedings not inconsistent with this opinion.
No costs are taxed. Each party will bear his own costs.