State Medicaid Manual Part 5 - Early and Periodic Screening, Diagnosis, and Treatment
Unannotated Secondary Research
April, 1990
20 pages
Cite this item
-
Case Files, Matthews v. Kizer Hardbacks. State Medicaid Manual Part 5 - Early and Periodic Screening, Diagnosis, and Treatment, 1990. 3b498589-5c40-f011-b4cb-7c1e5267c7b6. LDF Archives, Thurgood Marshall Institute. https://ldfrecollection.org/archives/archives-search/archives-item/f7d5b8ae-daed-41b6-8a38-eaad9b06e182/state-medicaid-manual-part-5-early-and-periodic-screening-diagnosis-and-treatment. Accessed February 22, 2026.
Copied!
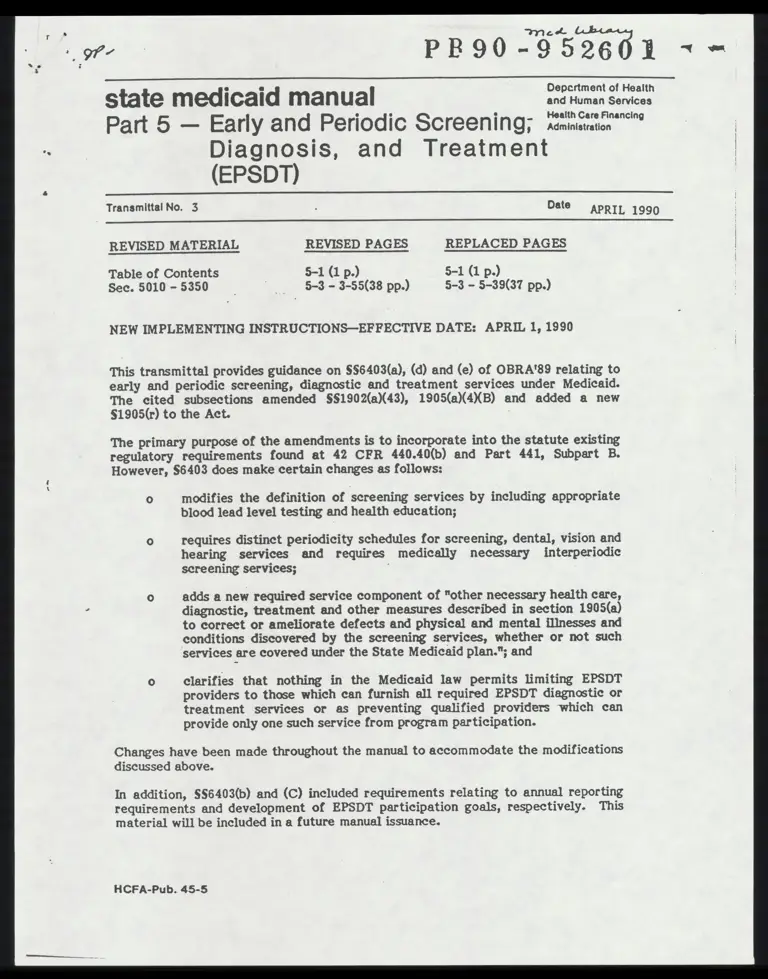
PR90 "052601 ~ =
state medicaid manual ERRAL
Part 5 — Early and Periodic Screening; mstton
Diagnosis, and Treatment
(EPSDT)
Transmittal No. 3 ; Date
APRIL 1990
REVISED MATERIAL REVISED PAGES REPLACED PAGES
Table of Contents $-1(1p.) 5-1 (1 p.)
Sec. 5010 -5350 ~~ 5-3 -3-55(38 pp.) 5-3 - 5-39(37 pp.)
NEW IMPLEMENTING INSTRUCTIONS—EFFECTIVE DATE: APRIL 1, 1990
This transmittal provides guidance on §§6403(a), (d) and (e) of OBRA'89 relating to
early and periodic screening, diagnostic and treatment services under Medicaid.
The cited subsections amended §§1902(a)(43), 1905(a)(4XB) and added a new
§1905(r) to the Act.
The primary purpose of the amendments is to incorporate into the statute existing
regulatory requirements found at 42 CFR 440.40(b) and Part 441, Subpart B.
However, $6403 does make certain changes as follows:
0 modifies the definition of screening services by including appropriate
blood lead level testing and health education;
requires distinct periodicity schedules for screening, dental, vision and
hearing services and requires medically necessary interperiodic
screening services;
adds a new required service component of "other necessary health care,
diagnostic, treatment and other measures described in section 1905(a)
to correct or ameliorate defects and physical and mental illnesses and
conditions discovered by the screening services, whether or not such
services are covered under the State Medicaid plan."; and
clarifies that nothing in the Medicaid law permits limiting EPSDT
providers to those which can furnish all required EPSDT diagnostic or
treatment services or as preventing qualified providers which can
provide only one such service from program participation.
Changes have been made throughout the manual to accommodate the modifications
discussed above.
In addition, §§6403(b) and (C) included requirements relating to annual reporting
requirements and development of EPSDT participation goals, respectively. This
material will be included in a future manual issuance.
HCFA-Pub. 45-5
CHAPTER V
EARLY AND PERIODIC SCREENING, DIAGNOSTIC AND TREATMENT (EPSDT) SERVICES
Introduction
OVRLViEWs ss sevice nsasss
snassatsssss
tnessssssare
nssnnnss sy 5010 5-3
Program Requirements and Methods
Basic RequirementS.eeseceecccesss
ccacsssaaassconcocssssots
5110 5-5
Informing Families of EPSDT ServiCeSeececccccscscsccccccsccce
S121 S=7 .
EPSDT Service RequirementScecececccccceseccscc
cscccnncscossts 5122 5=9
Screening Service Delivery and Contentecececccccscsccccccne
5123 5-10
Minimum Standards and RequirementScecececscecccccc
cccnsts 5123.1 5-10 |
Screening Service CONteNtecsccsccoscsscssssssos
cscossscccs 5123.2 5-11
Diagnosis and TreatmenNtsecccceccescsessccss
sscscecconcccccccccs 5124 5-17
Periodicity SoReAU1B es cossssstessssessssasssss
ssssissses 5140 5-20
Transportation and Scheduling AssistanCecccecccescscccses
5150 5-23
Utilization of Providers and Coordination with Related Programs
Referral for Services Not Covered Under Medicaideesccecescs 5210 5-25
Utilization Of ProviderSeececececccccccccccss
enaccscssrss 5220 5-26
Coordination with Related Agencies and ProgramSeececcceces 5230 5-27
Relations With State Maternal and Child Health
’
~ PrOGraMSeececsseseosssscsos
csssssoncrocsecaccsssss
5230.1 5-28
> other Agencies and PrOGramSesssceseocscscsccss
occcccs 5230.2 5-30
Continuing CAL@. tress esssasetsessncvasasncn
nnsgssatansss 5240 5-33
Administration
Program Monitoring, Planning, and EvaluatioNeccecccccceces
5310 5-35
Information Needs and Reportingecescccecccccccscc
cccssces 5320 5-38
Administrative Information RequirementSecececccscacsces
5320.1 5-38
Records or Information on Services and Recipients..... 5320.2 5-38
; PimalinesGec esses rravssssiavssssssssnsnssnsgsaas
aptagessr 5330 5-45
RELUDUL SERENE cast sssssecnsshsnsssnsssansnnns
nsnsssnnsy, 5340 5-51
Confidentiality ss csessesscsssssssssrasssssnss
snsssnnnsss, 5350 5-55
{ Rev. 3
5-1 :
EARLY AND PERIODIC SCREENING,
04-90 DIAGNOSTIC AND TREATMENT SERVICES 5010
Introduction
5010. OVERVIEW
A. Early and Periodic Screening, Diagnostic and Treatment Benefit.—Early and
periodic screening, diagnostic and treatment services (EPSDT) is a required service under
the Medicaid program for categorically needy individuals under age 21. The EPSDT
benefit is optional for the medically needy population. However, if the EPSDT benefit is
elected for the medically needy population, the EPSDT benefit must be made available to
| ell Medicaid eligible individuals under age 21.
B. A Comprehensive Child Health Program.--The EPSDT program consists of two,
mutually supportive, operational components:
o assuring the availability and accessibility of required health care resources
and
o helping Medicaid recipients and their parents or guardians effectively use
them.
These components enable Medicaid agencies to manage & comprehensive child health
program of prevention and treatment, to systematically:
a o Seek out eligibles and inform the benefits of prevention and the
h
ealth services and assistance available,
o Help them and their families use health resources, including their own
talents and knowledge, effectively and efficiently, LY
“g
r o Assess the child's health needs through initial and periodic examinations and
evaluation, and :
o Assure that health problems found are diagnosed and treated early, before
they become more complex and their treatment more costly. Although "case
management" does not appear in the statutory provisions pertaining to the EPSDT benefit, |
the concept has been recognized as a means of increasing program efficiency and |
- effectiveness by assuring that needed services are provided timely and efficiently, and
that duplicated and unnecessary services are avoided.
[= C. Administration.--You have the flexibility within the Federal statute and
regulations to design an EPSDT program that meets the health needs of recipients within
your jurisdiction. Title XIX establishes the framework, containing standards and
requirements you must meet.
Bg!
Rev. 3
5-3
EARLY AND PERIODIC SCREENING, .
0490 DIAGNOSTIC AND TREATMENT SERVICES 5110
Program Requirements and Methods
5110. BASIC REQUIREMENTS
[oBra 89 amended §51902(a)(43) and 1905(a)(4)(B) and created §1905(r) of the Social
Security Act (the Act) which set forth the basic requirements for the program. Under the
EPSDT benefit, you must provide for screening, vision, hearing and dental services at
intervals which meet reasonable standards of medical and dental practice established
after consultation with recognized medical and dental organizations involved in child
health care. You must also provide for medically necessary screening, vision, hearing and
dental services regardless of whether such services coincide with your established
periodicity schedules for these services. Additionally, the Act requires that any service
which you are permitted to cover under Medicaid that is necessary to treat or ameliorate
a defect, physical and mental illness, or a- condition identified by a screen, must be
provided to EPSDT participants regardless of whether the service or item is otherwise
included in your Medicaid plan.
The statute provides an exception to comparability for EPSDT services. Under this
exception, the amount, duration and scope of the services provided under the EPSDT
program are not required to be provided to other program eligibles or outside of the
EPSDT benefit. Services under EPSDT must be sufficient in amount, duration, or scope to
reasonably achieve their purpose. The amount, duration, or scope of EPSDT services to
recipients may not be denied arbitrarily or reduced solely because of the diagnosis, type
of illness, or condition. Appropriate limits may be placed on EPSDT services based on
C medical necessity.
Rev. 3
5-5
EARLY AND PERIODIC SCREENING,
04-930 DIAGNOSTIC AND TREATMENT SERVICES 5121
5121. INFORMING FAMILIES OF EPSDT SERVICES
A. General Information.—Section 1902(a)(43) of the Act requires that the State plan
provide for informing all eligible Medicaid recipients under 21 about EPSDT. The intent
of the statute is to allow flexibility of process as long as the outcome is effective, and is
achieved in a timely manner, generally within 60 days.
-
[: The informing process, which may begin at the intake interview, extends to no later than |
60 days following the date of a family's or individual's initial eligibility determination, or
of a determination after a period of ineligibility. A combination of face-to-face, oral, ~
and written informing activities is most productive.
PE
2 c
at
The regulation requires you to assure that your combination of written and oral informing
methods are_effective. Use methods of communication that recipients can clearly and
easily understand to ensure that they have the information they need to utilize services to
which they are entitled. HCFA considers "oral" methods to include face-to-face
informing by eligibility case workers, health aides and providers as well as public service
announcements, community awareness campaigns, audio-visual films and film strips.
1t is effective and efficient to target specific informing activities to particular "at risk" ;
groups. For example, mothers with babies to be added to assistance units, families with
infants, or adolescents, first time eligibles, and those not using the program for over
\ 2 years might benefit most from oral methods. i
B. Individuals to Be Informed.—
o Inform all Medicaid-eligible families about the EPSDT program.
o Inform newly eligible families, either determined eligible for the first time,
or determined eligible after a period of ineligibility if they have not used EPSDT services
for_at least 1 year. Use a combination of written and oral methods, generally within
60 days following the date of the eligibility determination.
Families that go on and off the rolls do not have to be informed more than once in a
12-month period.
Bd
o There is no distinction between title IV-E foster care families and others.
For title IV-E foster care individuals, informing must be with the unit receiving the cash
assistance (e.g., foster parent, administrator of institution). Many title IV-E foster care
individuals are rotated frequently through foster care homes or institutions, and, in some
cases, there are changes in foster parents, institution administrators, or responsible
social workers. It is to the individual's benefit that informing be done initially, not only
with the unit receiving the cash assistance, but with parties who have legal authority over
or custody of the individual.
Rev. 3 5-7
EARLY AND PERIODIC SCREENING, ® ) 5121(Cont.) DIAGNOSTIC AND TREATMENT SERVICES -90
Informing about EPSDT encourages appropriate planning for the health needs of children. When informing foster parents or administrators of institutions encompass all title IV-E foster care individuals in their care. Inform institutions or homes having a number of individuals annually or more often when the need arises, such as when changes in administrators, social workers or foster parents occur. If an individual is rotated through foster care homes, inform the responsible parties at the homes, unless previously done within the year for other foster care individuals. Annual contact establishes a relationship with the facilities to resolve any problems arising.
.
P
e
J, 0 - Inform a Medicaid eligible pregnant woman about the availability of EPSDT services for children under age 21 (including children eligible as newborns). A Medicaid eligible woman's positive response to an offer of EPSDT services during her pregnancy, which is medically confirmed, constitutes a request for EPSDT services for the child at birth. For a child eligible at birth (i.e., as a newborn of a woman who is eligible Tor and receiving Medicaid), the request for EPSDT services is effective with the birth of the child. The parent or guardian of an infant who is not deemed eligible at birth as a |_newborn must be informed at the time the infant's eligibility is determined.
C. Content and Methods.—
o Use clear and nontechnical language, provide a combination of oral and written methods designed to inform all eligible individuals (or their families) effectively describing what services are available under the EPSDT program; the benefits of preventive health care, where the services are available, how to obtain them; and that necessary transportation and scheduling assistance is available. [ Inform eligible individuals whether services are provided without cost. States may impose C premiums for Medicaid on individuals (i.e., pregnant women and infants) whose family income exceeds 150 percent.of Federal poverty levels as described in §3571 and, for medically needy participants, may impose enrollment fees, premiums or similar charges |_for participation in the medically needy program.
© Provide assurance that processes are in place to effectively inform individuals, generally within 60 days of the individual's Medicaid eligibility determination and, if no one eligible in the family has utilized EPSDT services, annually thereafter.
o. Utilize accepted methods for informing persons who are illiterate, blind, deaf, or cannot understand the English language. For assistance in developing appropriate procedures, contact agencies with established procedures for working with such individuals, e.g., State or local education departments, employment security offices, handicapped programs.
0 You have the flexibility to determine how information may be given most appropriately while assuring that every EPSDT eligible receives the basic information necessary to gain access to EPSDT services.
5-8
Rev. 3
EARLY AND PERIODIC SCREENING,
04-90 DIAGNOSTIC AND TREATMENT SERVICES 5122
[ 5122. EPSDT SERVICE REQUIREMENTS
The EPSDT benefit, in accordance with §1905(r) of the Act, must include the services set
forth below. The frequency with which the services must be provided is discussed in
§5140.
A. Screening Services.—Screening services include all of the following services:
o A comprehensive health and developmental history (including assessment of
both physical and mental health development);
o A comprehensive unclothed physical exam;
o Appropriate immunizations according to age and health history;
o Laboratory tests (including lead blood level assessment appropriate to age
and risk); and ;
o Health education (including anticipatory guidance).
Immunizations which may be appropriate based on age and health history but which are
medically contraindicated at the time of the screening may be rescheduled at an
appropriate time.
B. Vision Services.—At a minimum, include diagnosis and treatment for defects in
vision, including eyeglasses.
C. Dental Services.—At a minimum, include relief of pain and infections,
restoration of teeth and maintenance of dental health. Dental Services may not be
limited to emergency services.
D. Hearing Services.—At a minimum, include diagnosis and treatment for defects in
hearing, including hearing aids.
E. Other Necessary Health Care.—Other necessary health care, diagnostic services,
treatment and other measures described in §1905(a) of the Act to correct or ameliorate
defects, and physical and mental illnesses and conditions discovered by the screening
services.
F. Limitation of Services.—The services available in subsection E are not limited to
those included in your State plan.
o Under subsection E, the services must be "necessary . . . to correct or
ameliorate defects and physical or mental illnesses or conditions . . ." and the defects,
Rev. 3 5-9
EARLY AND PERIODIC SCREENING, .
5123 DIAGNOSTIC AND TREATMENT SERVICES 04-90
illnesses and conditions must have been discovered or shown to have increased in severity
by the screening services. You make the determination as to whether the service is
: necessary. You are not required to provide any items or services which you determine are
‘not safe and effective or which are considered experimental.
; = © 42 CFR 440.230 allows you to establish the amount, duration and scope of
: services provided under the EPSDT benefit. Any limitations imposed must be reasonable
: and services must be sufficient to achieve their purpose (within the context of serving the
i needs of individuals under age 21). Yolu may define the service as long as the definition
comports with the requirements of the statute in that all services included in §1905(a) of
the Act that are medically necessary to ameliorate or correct defects and physical or
mental illnesses and conditions discovered by the screening services are provided.
o All services must be provided in accordance with both §1905(a) of the Act
and any State laws of general applicability that govern the provision of health services.
Home and community based services which are authorized by §1915(c) of the Act are not
included among the other health care under subsection E because these services are not
included under §1905(a) of the Act.
9123. SCREENING SERVICE DELIVERY AND CONTENT
5123.1 Minimum Standards and Requirements, —
A. State Standards.--Set standards and protocols which, at a minimum, meet the
standards of §1905(r) of the Act for each component of the EPSDT services, and maintain C
written evidence of them. The standards must provide for services at intervals which : :
meet reasonable standards of medical and dental practice and be established after
consultation with recognized medical and dental organizations involved in child health
care. The standards must also provide for EPSDT services at other intervals, indicated as
medically necessary, to determine the existence of certain physical or mental illnesses or
conditions. The intervals at which services must be made available are discussed in
§5140.
B. Services.—
0 Provide an eligible individual requesting EPSDT services required screening
services listed in §5122. This initial examination(s) may be requested at any time, and
must be provided without regard to whether the individual's age coincides with the
established periodicity schedule. Sound medical practice requires that when children first
enter the EPSDT program you encourage and promote that they receive the full panoply
[of screening services available under EPSDT.
o It is desirable that a parent or other responsible adult accompany the child
to the examination. When this is not possible or practical, arrange for a followup worker,
social worker, health aide, or neighborhood worker to discuss the results in a visit to the
home or in contacts with the family elsewhere.
9-10 Rev. 3
>
EARLY AND PERIODIC SCREENING, !
DIAGNOSTIC AND TREATMENT SERVICES 9123.2
C. Who Screens/Assesses?—
o Examinations are performed by, or under the supervision of, a certified :
Medicaid physician, dentist, or other provider qualified under State law to furnish primary
medical and health services. These services may be provided within State and Tocal health ;
departments, school health programs, programs for children with special health needs,
Maternity and Infant Care projects, Children and Youth programs, Head Start programs, A
community health centers, medical/dental schools, prepaid health care plans, a private i
practitioner and any other licensed practitioners in a variety of arrangements.
o The use of all types of providers is encouraged. Recipients should have the
greatest possible range and freedom-of choice. It is required, in the case of title V, and
encouraged, tithe case of the primary care projects (i.e., community health centers), that
maximum use be made of these providers. Day care centers may provide sites for
examination activities. Encourage cooperation when and where other broad-based
assessment programs are unavailable. |
o Providers may not be limited to those which have an exclusive contract to
perform all EPSDT services. Service providers may not be limited to either the private or
public sector or because the provider may not offer all EPSDT services or because it
offers only one service. Assure maximum utilization of existing resources to more
effectively administer and deliver services.
B
C
E
C
C
Y
Medicaid providers who offer EPSDT examination services must assure that the services
they provide meet the agency's minimum standards for those services in order to be |
reimbursed at the level established for EPSDT services.
5123.2 Screening Service Content.—
A. Comprehensive Health and Developmental History.—Obtain this information ;
from the parent or other responsible adult who is familiar with the child's history and
include an assessment of both physical and mental health development. Coupled with the
| prysical examination, this includes:
1. Developmental Assessment.—This includes a range of activities to
determine whether an individual's developmental processes fall within a normal range of
achievement according to age group and cultural background. Screening for
developmental assessment is a part of every routine initial and periodic examination.
Rev. 3 5-11
r
o
a
S
3
fi
e
Z
A
C
-
ps
W
e
”
te
bt
;
$e
gf
A
a
*
re
3
EARLY AND PERIODIC SCREENING,
5123.2(Cont.) DIAGNOSTIC AND TREATMENT SERVICES 0%90
Developmental assessment is also carried out by professionals to whom children are
referred for structured tests and instruments after potential problems have been
identified by the screening process. You may build the two aspects into the program so
that fewer referrals are made for additional developmental assessment.
a. Approach.—There is no universal list of the dimensions of development
for the different age ranges of childhood and adolescence. In younger children, assess at
least the following elements:
o Gross motor development, focusing on strength, balance,
locomotion;
o Fine motor development, focusing on eye-hand coordination;
o Communication skills or language development, focusing on
expression, comprehension, and speech articulation;
o Self-help and self-care skills;
o Social-emotional development, focusing on the ability to engage in
social interaction with other children, adolescents, parents, and other adults; and
o Cognitive skills, focusing on problem solving or reasoning.
As the child grows through school age, focus the program on visual-motor
integration, visual-spacial organization, visual sequential memory, attention skills
auditory processing skills, and auditory sequential memory. Most school systems provide
routines and resources for developmental screening. :
For adolescents, the orientation should encompass such areas of special concern as
potential presence of learning disabilities, peer relations, psychological/psychiatric
problems, and vocational skills.
b. Procedures.—No list of specified tests and instruments is prescribed for
identifying developmental problems because of the large number of such
instruments, development of new approaches, the number of children and the
complexity of developmental problems which oceur, and to avoid any connotation that
only certain tests or instruments satisfy Federal requirements. However, the
following principles must be considered:
o Acquire information on the child's usual functioning, as reported by
the child, parent, teacher, health professional, or other familiar person.
5-12
Rev. 3
EARLY AND PERIODIC SCREENING,
0490 DIAGNOSTIC AND TREATMENT SERVICES 5123.2(Cont.)
o In ‘screening for developmental assessment, the examiner
incorporates and reviews this information in conjunction with other information gathered
during the physical examination and makes an objective professional judgement whether
the child is within the expected ranges. Review developmental progress, not in isolation,
but as a component of overall health and well-being, given the child's age and culture.
o Developmental assessment should be culturally sensitive and valid.
Potential problems should not be dismissed or excused improperly on grounds of culturally
appropriate behavior. Do not initiate referrals improperly for factors associated with
cultural heritage.
o Programs should not result in a label or premature diagnosis of a
child. Providers should report only that a condition was referred or that a type of
diagnostic or treatment service is needed. Results of initial screening should not be
accepted as conclusions and do not represent a diagnosis.
o Refer to appropriate child development resources for additional
assessment, diagnosis, treatment or follow-up when concerns or questions remain after
the screening process.
9. Assessment of Nutritional Status.—This is accomplished in the basic
examination through:
o Questions about dietary practices to identify unusual eating habits (such
as pica or extended use of bottle feedings) or diets which are deficient or excessive in one
or more nutrients.
o A complete physical examination including an oral dental examination.
Pay special attention to such general featurés as pallor, apathy and irritability.
o Accurate measurements of height and weight are among the most
important indices of nutritional status.
o A laboratory test to screen for iron deficiency. HCFA and PHS
recommend that the erythrocyte protoporphyrin (EP) test be utilized when possible for
children ages 1-5. It is a simple, cost-effective tool for screening for iron deficiency
Where the EP test is not available, use hemoglobin concentration or hematocrit.
o If feasible, screen children over 1 year of age for serum cholesterol
determination, especially those with a family history of heart disease and/or hypertension
and stroke. » a
Rev. 3 5-13
EARLY AND PERIODIC SCREENING,
5123.2(Cont.) DIAGNOSTIC AND TREATMENT SERVICES 04-90
If information suggests dietary inadequacy, obesity or other nutritional problems, further
assessment is indicated, including:
o Family, socioeconomic or any community factors,
o Determining quality and quantity of individual diets (e.g, dietary
intake, food acceptance, meal patterns, methods of food preparation and preservation,
and utilization of food assistance programs),
o Further physical and laboratory examinations, and
o Preventive, treatment and follow-up services, including dietary
counseling and nutrition education.
B. Comprehensive Unclothed Physical Examination:—Includes the following:
1. Physical Growth.—Record and compare the child's height and weight with
those considered normal for that age. (In the first year of life head circumference
measurements are important). Use a graphic recording sheet to chart height and weight
over time.
2. Unclothed Physical Inspection.—Check the general appearance of the child
to determine overall health status. This process can pick up obvious physical defects,
including orthopedic disorders, hernia, skin disease, and genital abnormalities. Physical
inspection includes an examination of all organ systems such as pulmonary, cardiac, and
gastrointestinal.
C. Appropriate Immunizations.—Assess whether the child has been immunized
against diphtheria, pertussis, tetanus, polio, measles, rubella, and mumps, and whether
booster shots are needed. The child's immunization record should be available to the
provider. When an immunization or an updating is medically necessary and appropriate,
provide it and so inform the child's health supervision provider.
Provide immunizations as recommended by the American Academy of Pediatrics (AAP)
and/or local health departments.
D. Appropriate Laboratory Tests.—Identify as statewide screening requirements,
the minimum laboratory tests or analyses to be performed by medical providers for
particular age or population groups. Physicians providing screening/assessment services
under the EPSDT program use their medical judgement in determining the applicability of
the laboratory tests or analyses to be performed. If any laboratory tests or analyses are
medically contraindicated at the time of screening/assessment, provide them when no
longer medically contraindicated. As appropriate, conduct the following laboratory tests:
fF 1. Lead Toxicity Screening.—Where age and risk factors indicate it is
medically appropriate to perform a blood level assessment, a blood level assessment is
mandatory.
EARLY AND PERIODIC SCREENING,
DIAGNOSTIC AND TREATMENT SERVICES 5123.2(Cont.)
2. Anemia Test.—The most easily administered test for anemia is a microhematocrit determination from venous blood or a fingerstick.
3. Sickle Cell Test.—Diagnosis for sickle cell trait may be done with sickle cell preparation or a hemoglobin solubility test. If a child has been properly tested once for
sickle cell disease, the test need not be repeated.
4. Tuberculin Test.—Give a tuberculin test to every child who has not received
one within a year. |
9. Others.—In addition to the tests above, there are several other tests to
consider. Their appropriateness are determined by an individual's age, sex, health
history, clinical symptoms and exposure to disease. These include a urine screening, pinworm slide, urine culture (for girls), serological test, drug dependency screening, stool
specimen for parasites, ova, blood, and HIV screening.
E. Health Education.—Health education is a required component of screening
services and includes anticipatory guidance. At the outset, the physical and dental
assessment, or screening, gives you the initial context for providing health education.
Health education and counselling to both parents (or guardians) and children is required
and is designed to assist in understanding what to expect in terms of the child's development and to provide information about the benefits of healthy lifestyles and
practices as well as accident and disease prevention.
F. Vision and Hearing Screens.—Vision and hearing services are subject to their own D periodicity schedules (as described in §5140). However, where the periodicity schedules
coincide with the schedule for screening services (defined in §5122 A), you may include : vision and hearing screens as a part of the required minimum screening services.
1. Appropriate Vision Secreen.—Administer an age-appropriate vision
assessment. Consultation by opthalmologists and optometrists can help determine the type of procedures to use and the criteria for determining when a child should be referred
for diagnostic examination.
. 2. Appropriate Hearing Screen.—Administer an age-appropriate hearing assessment. Obtain consultation and suitable procedures for screening and methods of
administering them from audiologists, or from State health or education departments.
EARLY AND PERIODIC SCREENING, : $123.2(Cont.) DIAGNOSTIC AND TREATMENT SERVICES 04-90
G. Dental Screenin Services.——Although an oral screening may be part of a physical examination, it does not substitute for examination through direct referral to a dentist. A direct dental referral is required for every child in accordance with your
.OBRA 89, HCFA in consultation with the American Dental Association, the American Academy of Pediatrics and the American Academy of Family Practice, among other organizations, required direct referral to a dentist beginning at age 3 or an earlier age if determined medically necessary. The law as amended by OBRA 89 requires that dental
0 Especially in older children, the periodicity schedule for dental examinations is not governed by the schedule for medical examinations. Dental examinations of older children should occur with greater frequency than is the case with physical examinations. The referral must be for an encounter with a dentist, or a professional dental hygienist under the supervision of a dentist, for diagnosis and treatment. However, where any screening, even as early as the neonatal examination, indicates that dental services | are needed at an earlier age, provide the needed dental services.
© The requirement of a direct referral to a dentist can be met in settings other than a dentist's office. The necessary element is that the child be examined by a dentist or other dental professional under the supervision of a dentist. In an area where dentists are scarce or not easy to reach, dental examinations in a clinic or group setting may make the service.more appealing to recipients while meeting the dental periodicity schedule. If continuing care providers have dentists on their staff, the direct referral to a dentist requirement is met. Dental paraprofessionals under direct supervision of a dentist may perform routine services when in compliance with State practice acts.
0 Determine whether the screening provider or the agency does the direct referral to a dentist. You are ultimately responsible for assuring that the direct referral is made and that the child gets to the dentist's office in a timely manner.
5-16
Rev, 3
ose sli
5140(Cont.)
EARLY AND PERIODIC SCREENING,
DIAGNOSTIC AND TREATMENT SERVICES 04-90
SENSORY SCREENING
Vision
DEVEL/BEHAV.'
ASSESSMENT
PHYSICAL EXAMINATION®
PROCEDURES
Hered Metabolic”
Screening
immunization’
Tubercuiin Test’
Hematocrit or Hemoglobin
Urinatysis®®
ANTICIPATORY"?
GUIDANCE
INITIAL DENTAL"
REFERRAL
ej oo je | @ e|o je |e oe jojo | @®@ | @ @® ®
ej oe | oo | @ ej{o je | @ oe joeje | oO | @® ® ®
ojo | © ei © . ®
Ts a
v
| Le] Lal} km a
\d *— @ J
eo |e |e | @® elo joj e ® ®
suUpeMSIOn.
time.
and individual need.
dons according to state law.
"1. Adolescent related issues (0.¢., pSychosocial, emotional, substance
Usage, and reproductive health) may necesscate More frequent heakh
2 it a child comes under care for the first time at any point on the
schedule, or if any items are not accomplished at the suggested age,
the schedule should be brought up to date at the eartiest possible
3. At these points. history may suffice: if problem sugQested., a standard
testing method shouid be empioyed.
4. By history and appropriate physical examination: if suspicious. by
specific objective developmental testing.
S. At each visit. a compiete physical examination is essential, with in-
fant totally unciothed, older child undressed and suitably draped.
8. Thess may be modified, depending upon entry point into schedule
7. Metabolic screening (e.g.. thyroid. PKU, galactosemia) should be
8. Schedules) per Report of Commies on infectious Disease, 1936
Red Book.
9. For low risk groups, the Commitee on infectious Diseases recom-
no routine tesung or Plesting &t
and adolescence. For high risk
mends the following options: ©
three times—infancy,
suggested
is left 10 the individual PACTCE BXPeINCe.
12 Appropriate discussion and counseling shouid be en integral pan
of each visit for care.
(6.5. inbom errors of mecadoksm, cide disease, lead) are aSCretonary ;
with the plrysican.
Key: ® =10 be performed: S=subjective. by history: O=objective. by a standard testing mechod.
Present medical evidence suggests the need for reevaluation of the
frequency and timing of urinalyses. One determination i therefore
during each time penod. Performance of additional tests
Seotember 1887
=
p
—
—
EARLY AND PERIODIC SCREENING,
:
04-90 DIAGNOSTIC AND TREATMENT SERVICES 5230
5230. COORDINATION WITH RELATED AGENCIES AND PROGRAMS
Interagency collaborative activities address several goals simultaneously:
o Containing costs and improving services by reducing service overlaps or
duplications, and closing gaps in the availability of services;
o Focusing services on specific population groups or geographic areas in need
of special attention; and
.
o Defining the scope of the programs in relation to each other.
Regulations require Medicaid agencies to coordinate services with title V programs, and
enter into arrangements with State agencies responsible for administering health services
and vocational rehabilitation services and with title V (Maternal. and Child Health)
grantees.
:
sordination’includes child health initiatives with other related programs, such as Head
Start, the Special Supplemental Food Program for Women, Infants and Children (WIC),
school health programs of State and local education agencies (including the Education for
all Handicapped Children Act of 1975), and social services programs under title XX.
Federal financial participation (FFP) is available to cover the costs to public agencies of
providing direct support to the Medicaid agency In administering the EPSDT program.
There is no single "list of approved roles", but cooperating agencies provide a variety of
outreach, screening, diagnostic or treatment services, health education and counseling,
case management, facilities, funding, and other help in achieving an effective child health
program. State and local program managers can help identify available child health
resources and make appropriate cross referrals. Active child health coordinating
committees, with representation from providers, private voluntary and public agencies are
helpful in promoting cooperation in providing health services.
Written agreements are essential to effective working relationships between the Medicaid
agency and agencies charged with planning, administering or providing health care to low-
income families. Although agreements by themselves do not guarantee open
communication and cooperation, they can lay the groundwork for collaboration and best
use of each agency's resources.
Successful relationships are based upon detailed planning, clearly identified roles and
responsibilities, program monitoring, periodic evaluation and revision, and constant
communication. Agreements are formal documents signed by each agency's
representative or written statements of understanding between units of a single
department. Whatever their form, it is essential that their content be developed by all
parties involved and that they provide a clear statement of each agency's responsibilities.
Rev. 3
5-27
‘
BERT et en TRY TERT QR Cro LT IO pr Pd
EARLY AND PERIODIC SCREENING
5230(Cont.) DIAGNOSTIC AND TREATMENT SERVICES 04-90
Each agreement must specify the participating parties, their intent, and the date upon
which the agreement becomes effective, and must be signed by persons who can make it
binding. Agreements need periodic review to determine if they continue to be
applicable to the organization, functions, and program of the participating agencies.
Reevaluate them annually and whenever a major reorganization occurs. Although
the specific content of each agreenient varies, they must specify:
o The mutual objectives‘and responsibilities of each party to the arrangement;
o The services each party of fers and in what circumstances;
The cooperative and collaborative relationships at the State level;
The kinds of services provided by local counterparts; and
Methods for —
- Early identification of individuals under 21 needing health services;
- Reciprocal referrals;
- Coordinating plans for health services provided or arranged
recipients;
Payment or reimbursement;
Exchange of reports of services furnished;
Periodic review and joint planning for changes in the agreements;
- Continuous liaison between the parties, including designation of State
and local liaison staff; and
- Joint evaluation of policies that affect the cooperative work of the
parties.
7 230.1 Relations With State Maternal and Child Health (MCH) Programs.—Title V (MCH
block grant) grantees and Medicaid share many of the same populations, providers,
and concerns for child health. Assure that each MCH grantee and the State Medicaid
agency have in effect a functional relationship via a written interagency
agreement which:
o provides for the maximum utilization of the care and services available under
MCH programs; and
o utilizes MCH grantees to develop a more effective use of Medicaid resources in
financing services to Medicaid-eligible children.
The overall goal of a State MCH-Medicaid agreement is to improve the health status
of children by assuring the provision of preventive services, health examinations, and the
necessary treatment and follow-through care, preferably in the context of an ongoing
provider-patient relationship and from comprehensive, continuing care
providers. Medicaid agencies reimburse title V providers for these services even if
they are provided free of charge to low-income uninsured families.
5-28
EARLY AND PERIODIC SCREENING,
04-90
DIAGNOSTIC AND TREATMENT SERVICES 5230.1(Cont.)
Inform recipients eligible for title V services of the available services and refer them, if
they desire, to title V grantees that offer appropriate services. However, such referral
does not relieve you of your obligations to assure the timely delivery of EPSDT services.
For further information, consult Promoting the Health of Women and Children Through
Planning, prepared by Lorraine V. Klerman, A. Yvonne Russell, and Isabelle Valadian.
A. Organization and Administration of EPSDT Programs.—HCFA encourages State
programs to enlist providers who can deliver to children a broad array of services on &
continuing basis. State MCH programs can help in a number of ways:
a di
o Recruitment of providers from both the private and public sectors to
provide comprehensive, continuing care to children.
o Provision of outreach and referral services at the local levels;
o Utilization of Maternity and Infant Care and Children and Youth Projects,
and other specialty and primary care programs as providers of comprehensive, continuing
care;
o Delegation of tasks by the Medicaid agency t
assure that Medicaid-eligible children have access to an
assessment, diagnostic, and treatment services. Such delegation can
Statewide.
o Development of health services policies and standards and assessment of
quality of care issues. These include implementation of professionally recognized
protocols and standards of care, integration of services at local and regional levels within
a State, and continuity of care. Assessment should be jointly agreed upon with a view
toward: eliminating unnecessary services; duplication; providing acceptable quality of
care; and integrating and providing all necessary services.
o Assurance of continuing
ted primary care projects provide
continuing care to all child clients,
ent status. State MCH
programs develop linkages with these projects to assure
levels of care for
mothers, infants, and children including those with special heal
B. Financing and Pa ment Arrangements for Services Provided by or Thro MCH
Programs to Medicaid Beneficiaries.—Statu
tory authority exists in the Social Security Act
for Medicaid to reimburse title V programs for the covered services they provide to
Medicaid beneficiaries. Each interagency agreement refers to the services and
circumstances under which Medicaid reimburses MCH programs.
Describe the payment mechanism. If it is no different than that used for other providers,
merely note that the Medicaid fee schedule or reasonable charge structure is employed.
Alternative payment arrange ments may include:
o Prospective interprogram transfer of funds with retrospective adjustments
based upon the volume of services actually delivered;
Rev. 3
TT a a
~ = at ee
EARLY AND PERIODIC SCREENING,
DIAGNOSTIC AND TREATMENT SERVICES 04-90
5320.2(Cont.)
O
N
o Where a claims.form or provider certification is absent or does not provide
contradictory evidence, the recipient's documentation that an examination was received,
is acceptable. Documentation must be made of any conditions found needing treatment.
When arrangements are made with continuing care providers, whether they are private
physicians, HMOs, title V grantees, Indian Health Service clinics, hospitals or group
4 medical practices for the delivery of EPSDT services, assure compliance with the EPSDT
Records must be available for your auditing. You provide the methods to be
%
C. Documentation of Referral Effort.—The agency must be able to demonstrate
that it attempts to reier recipients needing services which Medicaid does not cover to a
provider willing to furnish uncovered treatment at little or no cost, or document that a
= good faith effort was made to locate willing providers and the dates The agency does
not have to keep the names(s), address(es) and telephone number(s) of providers if,
according to written agency procedures, recipients are given that information at the time 5
|
of referral. Examples of acceptable documentation include:
| ; o A dated letter to the ‘recipient which gives name(s), address(es),
and telephone number(s) of providers willing to furnish uncovered treatment services at
By little or no expense; Or,
t
h
Ba
de
o A dated record of a home visit or telephone contact.
D. Program Reports.—The quarterly report (HCFA-420) helps meet State and
Federal program accountability needs by providing nationwide baseline information on
See Part 2, §2700.4. The HCFA-420 a
children in Medicaid's child health program.
contains only that universe and utilization data which can be reliably aggregated for So
national totals, by two age groups, 0-5 and 6 and over:
i
o Number eligible for EPSDT.
o Total number of eligibles enrolled in continuing care arrangements --
- Number of individuals enrolled in continuing care arrangements where
” services are not reported.
- Number of individuals enrolled in continuing care arrangements where |
“4 services are reported.
o Number of initial and periodic examinations.
o Number of examinations where at least one referrable condition was
identified.
P
E
L
E
$
h
o
I
,
3
0
.
-—
eo
‘e
:
iy
4
N
a
t
a
oe
?
Td
tr
al
ia
.
Pe
dd
ie
L
A
yd
h
i
H
e
~
.
5-40
Rev. 3
A
a
m
.
F
i
S
e
e
d
”
ra
:
.
EARLY AND PERIODIC SCREENING
s
04-90 DIAGNOSTIC AND TREATMENT SERVICES 5320.2(Cont.)
%
bo . State managers may collect and analyze more detailed information about eligible
children, their services utilization and health status, as part of ongoing program
evaluation and planning. For example:
o Number of individuals, under health supervision, for whom examinations
were not due according to your periodicity schedule;
o Number of individuals found with health problems for whom treatment was
initiated during a given time period;
o Major health problems and their relative significance;
o Provider participation, practice and utilization patterns.
o Geographic and demographic utilization analyses to determine outreach or
health problem targets; :
o Costs and effects studies comparing the Medicaid expenditure experience of
participants and nonparticipants.
Rev. 3
541
s
1
[]
{
TT TT TE Ch Df Sh Tg $17 aL RE EN oF AS BS A ins AS SEA o 577, 85 AAR ATINENS (OS Pe Sr TE OI SS he
> EA iE MCE EE SR OF ET REE ANE 3, NX Ny CGO RE: TAY ST Ri ME IaH, 1 3 ir a Ee ASS on 3" Rn 1 NN Seokal <
. d aE LE lic La A I ii at ae 3 i 4 EEE ~—- 7s Bs = $s’ Be
——————
tlre : FE LBA ik LE Le he -*.
Ee RY Rs