Plaintiff's Proposed Findings of Fact and Conclusions of Law on USA's Motion for Summary Judgement
Public Court Documents
December 11, 1992
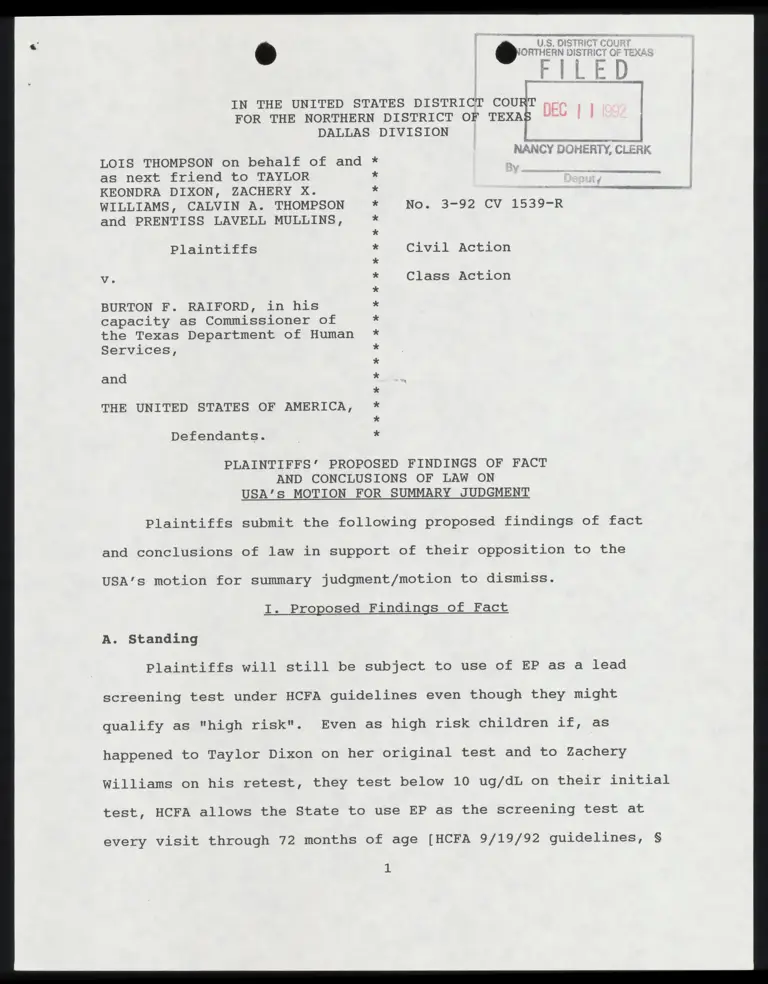
21 pages
Cite this item
-
Case Files, Thompson v. Raiford Hardbacks. Plaintiff's Proposed Findings of Fact and Conclusions of Law on USA's Motion for Summary Judgement, 1992. 031318e7-5c40-f011-b4cb-002248226c06. LDF Archives, Thurgood Marshall Institute. https://ldfrecollection.org/archives/archives-search/archives-item/f8a66d97-0586-4326-ad83-c5bb2799b195/plaintiffs-proposed-findings-of-fact-and-conclusions-of-law-on-usas-motion-for-summary-judgement. Accessed February 12, 2026.
Copied!
FOR THE NORTHERN DISTRICT OF TEXAS “~~ | |
DALLAS DIVISION
I.
NANCY DOHERTY, CLERK
LOIS THOMPSON on behalf of and
as next friend to TAYLOR
KEONDRA DIXON, ZACHERY X.
WILLIAMS, CALVIN A. THOMPSON
and PRENTISS LAVELL MULLINS,
A —— i.
No. 3-92 CV .1539~R
Plaintiffs Civil Action
Vv. Class Action
BURTON F. RAIFORD, in his
capacity as Commissioner of
the Texas Department of Human
Services,
and
THE UNITED STATES OF AMERICA,
%
%
%
%
%
%
N
O
X
%
%
%
OX
%X
%
¥
¥
X
¥
%*
*
Defendants.
PLAINTIFFS’ PROPOSED FINDINGS OF FACT
AND CONCLUSIONS OF LAW ON
USA’s MOTION FOR SUMMARY JUDGMENT
Plaintiffs submit the following proposed findings of fact
and conclusions of law in support of their opposition to the
USA’s motion for summary judgment/motion to dismiss.
I. Proposed Findings of Fact
A. Standing
Plaintiffs will still be subject to use of EP as a lead
screening test under HCFA guidelines even though they might
qualify as "high risk". Even as high risk children if, as
happened to Taylor Dixon on her original test and to Zachery
Williams on his retest, they test below 10 ug/dL on their initial
test, HCFA allows the State to use EP as the screening test at
every visit through 72 months of age [HCFA 9/19/92 guidelines, §
1
5123.2 D.1.c.(2)]. Using the HCFA guidelines, Taylor Dixon will
be screened using the admittedly ineffectual EP test during the
period of her life when the most rapid rate of increase in blood
lead levels will occur. "Blood lead concentrations increase
steadily up to at least 18 months of age. The most rapid rate of
increase occurs between 6 and 12 months of age." [CDC 1991, page
42]
The USA’s argument that the HCFA guidelines clearly require
the use of the blood lead test is contradicted by the plain
wording of the HCFA guidelines.
The Sept. 19, 1992 HCFA guidelines for "High Risk" children
specifically distes: "If the initial blood lead level test
results are less than (<) 10 micrograms per deciliter (ug/dL), a
screening EP test or blood lead test is required at every visit
prescribed in your EPSDT periodicity schedule through 72 months
of age." [HCFA 9/19/92 guidelines 5132.2 c. Screening Blood
Tests. (2) High Risk].
The HCFA guidelines plainly state :"States continue to have
the option to use the EP test as the initial screening blood
test."
"As part of the nutritional assessment conducted at each
periodic screening, an EP blood test may be done to test for iron
deficiency. This blood test may also be used as the initial
screening blood test for lead toxicity."
These statements are completely consistent with the position
that the States are still allowed to use the EP test even for
high risk children.
The HCFA guidelines do not support a finding that plaintiffs
will not still be subject to the use of the EP test as a lead
screening blood test.
The USA also argues that there has been a change in the
Texas procedures for lead screening which demonstrates
plaintiffs’ lack of standing. The State’s memorandum in opposi-
tion to the class motion alleges that EP was discontinued as a
screening device as of Oct. 23, 1992. Therefore, the USA argues,
plaintiffs have lost standing if they ever had it. The State has
not introduced any evidence that EP will not be used as screening
device. The only evidentiary material filed by the State is the
Cook affidavit filed with the opposition to motion for class
certification. That affidavit says only that the State of Texas
has obtained and put into use, as of Oct. 23, 1992, the equipment
to conduct blood lead tests on all specimens received for blood
lead testing. The State introduced no evidence to show that the
EP test has been eliminated or under what circumstances even high
risk children will receive blood lead tests.
Plaintiffs introduced the State of Texas January 1992 EPSDT
Screening Manual [copy attached to Beshara declaration]. If the
State follows the periodicity schedule or the follow-up care
guidelines in that manual, then neither Taylor Dixon nor Zachery
Williams will receive another blood lead test as part of their
EPSDT screening. The other two plaintiff children will only be
considered for rescreening. All four plaintiffs will receive EP
tests at every screening interval.
Plaintiffs also introduced the State of Texas "Laboratory
Screening Services" publication [copy attached to Beshara decla-
ration]. The State of Texas January 1992 EPSDT Screening Manual
refers to the Laboratory Screening Services publication stating
"The Handbook provides supplementary information on required
laboratory test procedures, interpretation of lab test results,
guidelines and criteria for referral and follow-up and instruc-
tions on specimen collection and handling." The Handbook re-
quires the use of the EP test as the "primary screening test for
lead" [page 6]. The Handbook provides for the use of a blood lead
test only if the EP level is greater than 35 ug/dL. This is
exactly the procedure that the State of Texas has been following
even though the January 1992 EPSDT Screening Manual has required
at least one blood lead test [Kelley letter, copy attached to
Beshara Declaration, page 2 and attachment "Lead Blood Tests"].
The State’s evidence that it has its own blood lead testing
equipment and that it will use it on all specimens marked for
blood lead testing does not negate or contradict the proposition
that plaintiffs will receive only one blood lead test if that
initial test results in a blood lead level < 10 ug/dL. If the
periodicity schedule and follow-up care guidelines are followed,
the only specimens which will be marked for blood lead testing
will be the initial test. If that test result is < 10 ug/dL, no
subsequent specimens will be marked for blood lead testing.
The summary judgment evidence demonstrates that at least two
of the plaintiffs, Taylor Dixon and Zachery Williams, will
continue to be subject to the use of the EP test as a screening
test for lead poisoning.
B. Merits
The USA argues that its new HCFA guidelines comply with the
CDC guidelines and therefore comply with the Medicaid Act provi-
sion at issue, 42 U.S.C. 1396d(r)(1)(B)(iv). Even if this was a
good legal argument, the facts do support the assertion. There
are substantial differences between the relevant CDC childhood
lead poisoning prevention and treatment provisions and the HCFA
guidelines.
The chart attached to these findings compares the CDC, HCFA,
Texas January 1992 EPSDT Medical Screening Manual, and the Texas
"Laboratory Screening Services" handbook provisions on the timing
and type of blood test for children under 72 months of age shows
that there are considerable differences between the CDC screening
guidelines and the screening which children such as plaintiffs
will receive under either the HCFA or the Texas EPSDT guidelines.
There are other critical differences between the CDC State-
ment and the HCFA guidelines.
The USA alleges that the HCFA guidelines are compatible with
the CDC’s 1991 position on the use of verbal questions to deter-
mine whether a child is at high or low risk. The USA then uses
this fact to imply that the HCFA guidelines allowing the use of
the EP test for "low risk" children are also compatible with the
1991 CDC statement. This implication is false. The CDC 1991
statement allows the use of verbal questions to determine high or
low risk only if the child is given a blood lead level test no
matter what the risk characterization.
Page 42 of the October 1991 CDC statement unequivocally
states "The questions are not a substitute for a blood lead
test." (emphasis in the original).
HCFA itself has recognized the need to confirm the verbal
screening with a blood lead test no matter what category of risk
the answers would seem to justify. "We agree that responses to
questions are not a substitute for a blood lead test." [Aug. 6,
1992 letter from Christine Nye, Director Medicaid Bureau, to
Julius Chambers, Director-Counsel NAACP Legal Defense and Educa-
tional Fund, Inc. attached to interveners’ complaint].
The Federal Centers for Disease Control states "Screening
should be done using a blood lead test. Since erythrocyte proto-
porphyrin (EP) is not sensitive enough to identify more than a
small percentage of children with blood lead levels between 10
and 25 ug/dL and misses many children with blood lead levels > 25
ug/dL (McElvaine et al., 1991), measurement of blood lead levels
should replace the EP test as the primary screening method."
[CDC, "Preventing Lead Poisoning in Young Children", 1991, page
417+
The new HCFA guidelines allow the use of EP testing for the
follow up screening of high risk children whose initial blood
lead level test results in a finding < 10 ug/dl. "If the initial
blood lead test results are less than (<) 10 micrograms per
deciliter (ug/dL), a screening EP test or blood lead test is
required at every visit prescribed in your EPSDT periodicity
schedule through 72 months of age." [HCFA 5123.2.D.c(2) High
Risk]. CDC 1991 requires all subsequent screening to be done
using the blood lead test [CDC 1991 page 44].
The EP test does not provide for the assessment of blood
lead levels.
The USA alleges as a fact that the continued use of the EP
test is based on the USA’s taking into account the current
advances in scientific knowledge about lead screening procedures.
This allegation is disputed by the significant sources of scien-
tific knowledge about the use of EP as a lead screening procedure
which contradict the USA’s position. One of these scientific
sources is a study and report authored in part by the USA’s
affiant, Sue Binder, MD.
Dr. Binder is an author of the article "Evaluation of the
erythrocyte protoporphyrin test as a screen for elevated blood
lead levels" October 1991, Journal of Pediatrics, 548-550 [copy
attached to Declaration of Laura Beshara]. Dr. Binder’s study
reported that the EP test was able to detect only 26% of the
children with elevated blood lead levels > 10 ug/dL [table page
549]. The report concludes "For identification of the children
with BPb levels of 10 to 24 ug/dl, another screening method,
probably BPb measurement, will be needed" [page 550].
The federal Agency for Toxic Substances and Disease Registry
[ATSDR] filed its "The Nature and Extent of Lead Poisoning in
Children in the United States: A Report to Congress" in 1988. The
Report analyzed the existing research on the reliability of the
EP test as a screening test for lead poisoning. "Analysis of data
from the second National Health and Nutrition Examination Survey
(NHANES II) by Mahaffey and Annest (1986) indicates that Pb-B
levels in children can be elevated even when EP levels are
normal. Of 118 children with Pb-B levels above 30 ug/dl (the CDC
criterion level at the time of NHANES II), 47% had EP levels at
or below 30 ug/dl, and 58% (Annest and Mahaffey, 1984) had EP
levels less than the current EP cutoff value of 35 ug/dl (CDC,
1985)". HHS concluded "This means that reliance on EP level for
initial screening can result in a significant incidence of false
negatives or failures to detect toxic Pb-B levels."[copy attached
to Beshara Declaration page II-9].
The 1991 U.S. Department of Health and Human Services
"Strategic Plan for the Elimination of Childhood Lead Poisoning"
correctly forecast the 1991 CDC actions lowering the level of
blood lead which should be taken as a symptom of lead poisoning.
"In 1991 CDC will likely issue new recommendations suggesting
that screening programs attempt to identify children with blood
lead levels below 25 ug/dL." HHS, "Strategy", 1991, page 23. The
HHS "Strategic Plan" correctly stated that the CDC action should
mean an end to the use of EP testing for childhood lead screen-
ing. "This change will mean that blood lead measurements must be
used for childhood lead screening instead of EP measurements."
HHS, "Strategy", 1991, page 23 (emphasis added) [attached to
Declaration of Laura Beshara].
The USA knows that the EP test is not an appropriate lead
blood level assessment for any age and risk factors. The 9/19/92
HCFA amendment acknowledges this. "The erythrocyte protoporphyrin
(EP) test is not sensitive for blood lead levels below 25 ug/dL."
The HHS "Strategic Plan for the Elimination of Childhood
Lead Poisoning", 1991 states "At present it is much cheaper and
easier to perform an EP test than a blood lead measurement;
however, the EP test is not a useful screening test for blood
lead levels below 25 ug/dL." [Page 40, attached to Beshara
Declaration]. The USA’s affiant, Sue Binder, MD., is a principal
author of the "Strategic Plan".
The Hiscock Geciavaiicn admits that the EP test does not
measure blood lead levels and that only the blood lead test
directly measures blood lead levels [Hiscock Declaration q 9.,
page 5]. The EP test measures only the level of erythrocyte
protoporphyrin in the blood [Hiscock Declaration { 9; Binder
Declaration q 14].
If the EP test is used as an assessment of blood lead
levels, only 27% of the children whose actual blood lead levels >
10 ug/dL will be identified [Binder study table page 549, at-
tached to Beshara declaration].
The EP test does not provide an assessment of blood lead
levels at any level [Rosen affidavit pages 8-9]. The EP test
discovered only 73% of the high risk children with blood lead
levels > 25 ug/dl in the Binder study area. The EP test accurate-
ly assessed only 26%, 42%, and 50% of the high risk children with
elevated lead levels in other national and local studies [Binder
study page 549, results of NHANES II overall and high risk
subset, and Oakland study [attached to Beshara Declaration].
C. Capacity
The USA argues that an alleged lack of capacity to conduct
blood lead testing by some unspecified number of unnamed states
justifies its continued support for the use of the EP test.
Whether or not such a lack of capacity would legally justify the
violation of the Medicaid Act, there is no evidence to support a
finding that there is any such lack of capacity.
The USA’s only evidence are the general allegations in its
pleadings and affidavits that there is a lack of capacity. The
plaintiffs’ and interveners’ evidence in response to this allega-
tion furnishes specific and concrete evidence that there is ample
blood lead testing laboratory capacity throughout the country.
For any location without inhouse capacity for blood lead testing,
the current nationwide laboratory testing services provide the
capacity for the blood lead level testing. These laboratories
are available to any location with express mail service [Nicar
Declaration; Rosen affidavit].
Plaintiffs also introduced, in support of their class
certification motion, a federal "OSHA List of Laboratories
Approved for Blood Lead Analysis Based on Proficiency Testing"
[plaintiffs’ class certification exhibit #11]. This list pro-
vides the name and address of CDC certified proficient blood lead
10
testing laboratories in 46 states and Washington, D.C.
There is no lack of "capacity" if HCFA is really willing to
pay for blood lead level testing for all Medicaid eligible
children.
II. Proposed Conclusions of Law
A. Standing
At least two of the plaintiffs will continue to be subject
to the use of the EP test as part of the EPSDT lead poisoning
screening procedures. This satisfies the injury in fact element
of standing.
There is no doubt that the USA’s support for the use of the
EP test is a factor in the States continued use of the test. The
structure of the Medicaid Program is such that if the USA had
disapproved of the EP test and refused to reimburse the States
for its use, the States would not use EP in the Medicaid EPSDT
program. The causation element is satisfied.
Here the redressability and causation requirements are
corollaries. Just as the USA’s continued support for the EP test
has been a causal factor in the States’ use of the test, if the
USA would cease its support for the EP test and pass regulations
requiring the use of the blood lead test for childhood lead
poisoning screening, the injury to the plaintiffs and the plain-
tiff class would be remedied. The injunctive relief requested
seeks such a remedy.
B. Adequate Remedy Under APA
The USA argues, for the first time in its reply to
11
plaintiffs’ response to the motion for summary judgment, that the
APA, 5 U.S.C. § 704, prohibits this action against the USA
because the plaintiffs have an adequate remedy against the State
in a § 1983 claim. The reply was not received by plaintiffs
until December 9, 1992 when plaintiffs’ counsel called and asked
for a copy to be FAXed. The mailed copy was received on December
10, 1992. The reply to a response to a motion for summary
judgment filed less than a week before argument on the motion is
not the appropriate time to raise an entirely new legal argument.
The USA’s reply should have been just that, a reply brief, not a
new basis alleged at a time when plaintiffs have no opportunity
to research, brief and respond. If the USA wants to make this
argument, it must do so in the proper procedural framework.
In at least one area of the relief requested, the retesting
and follow-up treatment for children screened by use of the EP
test, the remedy against the State defendant will not be ade-
quate. Plaintiffs have requested that the federal government
finance the retesting, using the blood lead test, of all Medicaid
children who have been $1legally screened using the EP test. The
federal government’s financial support for such retesting would
be required in order for such relief to be granted. A suit only
against the state would provide no basis to compel the federal
government to provide this support.
C. Does the statute require a blood lead test?
The Medicaid Statute Prohibits any use of the EP test.
The Medicaid Act requires "lead blood level assessment
12
appropriate for age and risk factors" for children who are
screened under the EPSDT program. 42 U.S.C. § 1396d(r)(1)(B) (iv).
The statute’s plain and unambiguous language requires the
use of "lead blood level assessment." No where in the statute or
in the legislative history does Congress express an intention for
the states to use the Erythrocyte Protoporphyrin (EP) test. As
plaintiffs’ response indicates and as defendant USA admits, the
EP test does not measure the lead in a child’s blood at all.
The USA’s policy argument is that the states should be
allowed to use the EP test as a device for lead poisoning screen-
ing for the poor children of our country until some unknown
future date. The policy argument of the USA acting through HCFA
must be rejected. Administrative interpretation of a statute
contrary to the plain language of the statute is not entitled to
deference by the courts. Demarest v. Manspeaker, __ U.S. 184,
112 L.Ed.2d 608, 616 (1991); see Public Employees Retirement
System of Ohio v. Betts, = U.S. _ , 106 L.Ed.2d 134, 150-151
(1989). If Congress had wanted to the states to use a test that
did not detect for levels of lead in the blood Congress could
have said so in the statute. Congress did not choose to do that.
Instead, Congress made a policy decision to have EPSDT children
screened with a blood lead level test. The policy decision has
been made by Congress and defendant USA should not be allowed to
change it.
when the language of the statute is unambiguous, judicial
inquiry is complete except in rare and unusual circumstances.
13
Demarest v. Manspeaker, U.S. _ , 112 L.Ed.2d 608, 616 (1991);
Burlington Northern R. Co. v. Oklahoma Tax Comm’n, 481 U.S. 454,
461 (1987); Rubin v. United States, 449 U.S. 424, 430 (1981).
The language of the Medicaid Act is unambiguous. It states that
"laboratory tests (including lead blood level assessment appro-
priate for age and risk factors)" are required for EPSDT chil-
dren. 42 U.S.C. § 1396d(r)(1)(B)(iv). From the face of the
statute, a laboratory test that detects levels of lead in the
blood is required and not a test that does not even detect levels
of lead such as the EP test.
The USA contends that EP is "appropriate for age and risk"
and that it therefore is consistent with the statute. The record
of the EP test, as set out in plaintiffs’ response, shows that it
is not an appropriate test for any person at risk. There is more
to the statute than that selective phrase. The entire statute
states that EPSDT screening must provide for "laboratory tests
(including lead blood level assessment appropriate for age and
risk factors)." 42 U.S.C. § 1396d(r)(1)(B)(iv). The entire
statute makes it clear that blood lead tests are required.
This is not one of those rare circumstances as in Griffin v.
Oceanic Contractors, Inc., 458 U.S.564, 571 (1982), where the
literal or usual meaning of the statute would thwart the purpose
of the statute. The literal or usual meaning of the statute at
issue here would require a blood lead level assessment that would
detect the level of lead in a child’s blood in order to determine
14
if that child had lead poisoning.? The purpose of the EPSDT
statute and the 1989 amendments is to provide health care to poor
children. 42 U.S.C. §§ 1396d(r); Report of the House Budget
Committee, Explanation of the Energy and Commerce and Ways and
Means Committees Affecting Medicare-Medicaid Programs, 101 Cong.
1st. Sess., p. 398 (September 20, 1989). The literal or usual
meaning of the statute is consistent with that purpose and would
require a blood lead test that could detect levels of lead so
that poor children with lead poisoning could be diagnosed and
treated. The EP test is inappropriate with the overall purpose
of the Medicaid Act and the EPSDT scheme. The EP test does not
detect levels of lead in the body and as is evident through
defendant ’s many admissions, is a useless screening test for
childhood lead poisoning.
The USA contends that since the legislative history of the
Medicaid Act is silent on the issue of whether a blood lead test
or EP should be required then this silence supports its argument
that the USA can allow the use of the EP test by the states.
Legislative history, however, is irrelevant where the language of
the statute is plain. While "legislative history can be a
legitimate guide to a statutory purpose obscured by ambiguity, in
the absence of a clearly expressed legislative intention to the
contrary, the language of the statute itself must ordinarily be
1 The definition of lead poisoning has been recently changed
by the Centers for Disease Control (CDC). The new level of
concern is 10 ug/dL of lead in the blood for even at this low
level adverse health effects can occur in young children.
15
regarded as conclusive." Burlington Northern R. Co. v. Oklahoma
Tax Comm’n, 481 U.S. 454, 461 (1987). Lack of legislative
history does not prevent the Court from applying the plain
language of the statute and requiring the USA to support a blood
lead test for EPSDT children.
Congress enacted amendments to the Medicaid Act in 1989.
Those amendments included the addition of blood lead testing for
EPSDT children. OBRA ‘89 § 6403, now 42 U.S.C. § 1396d(r). The
addition of a "lead blood level assessment" was made after the
1998 Report to Congress, "The Nature and Extent of Lead Poisoning
in Children in the United States," by the U.S. Dept. of Health
and Human Services Agency for Toxic Substances and Disease
Registry, which indicated that EP was not a useful screening
device for detecting levels of lead in the blood of children.
The USA now argues that the statute does not have the "narrow,
technical meaning" of a blood lead test in spite of the plain
words of the statute. The USA would like to ignore the plain
language of the 1989 amendment in favor of the earlier version of
the statute that does not have the language requiring "lead blood
level assessment." It is not the function of the courts,
however, to decide whether or not the amendment is better. The
plain language of the statute controls. West Virginia Univ.
Hospitals, Inc. v. Casey, U.S. , 113 L.E4.2d 68, 84 (1991).
As Justice Brandeis has explained, the expansion of a
statute beyond its plain language is not a role for the courts:
[The statute’s] language is plain and unambiguous. What the
Government asks is not a construction of a statute, but, in
16
effect, an enlargement of it by the court, so that what was
omitted, presumably by inadvertence, may be included within
its scope. To supply omissions transcends the judicial
function.
Iselin v. United States, 270 U.S. 245, 250-51 (1926). The USA
should not be allowed to expand the clear language of the statute
requiring a blood lead test to include a useless test that does
not detect lead.
D. Lack of Capacity
The lack of capacity argument by the USA is both a factual
argument and a legal argument. The USA argues that there are
states that do not have the capacity to perform blood lead
testing. The argument never proceeds beyond the statement of the
ultimate cohcludion: The USA provides no particulars. The USA
names no specific states without "capacity." The USA does not
explain why any state cannot or does not have this "capacity."
This bald, unsupported general allegation does not prove, or tend
to prove, any facts.
The USA's legal argument is not made but must rather be
implied from the factual argument. Assume that there are,
somewhere, states without the capacity to draw small amounts of
blood from little children, put it in a tube, and deliver it to a
laboratory inside or outside the state. The USA must be arguing
that this lack of capacity excuses performance from the statute.
It is a lame excuse for noncompliance with the statute. The
U.S. Congress, in 1989, told each state that if it was going to
participate in the federal Medicaid/EPSDT program that it had to
provide such blood lead testing in return for the federal funds
17
necessary to do the testing. 42 U.S.C. § 1396d(r)(1)(B)(iv). A
state’s refusal to provide the capacity to collect and analyze
blood samples for lead content should not be a defense to a clear
violation of the statute. This is the last decade of the twenti-
eth century. We have put persons on the moon. The USA is not a
third world country which needs to import United Nations medical
teams to test its children for lead poisoning.
Unwillingness or self-imposed inability to provide a re-
quired service does not excuse a state from compliance with the
Medicaid statute. "Texas, like most states, has taken a bite out
of the carrot of cooperative federalism and is, accordingly,
subject to the federal stick -- the minimum mandatory require-
ments set forth in the Medicaid legislation." Mitchell v. Johnst-
on, 701 F.2d 337, 340 (5th Cir. 1983) (state could not limit
EPSDT dental care to checkups every three years).
The lack of capacity argument also fails as an argument
against plaintiffs having standing. The USA argues that if the
requested relief is granted (blood lead tests for all regardless
of high or low risk) then the lack of capacity means that high
risk kids will be delayed in getting the blood lead tests because
they may be behind low risk kids waiting for the tests. The lack
of capacity argument really boils down to the USA not wanting to
follow the statute.
If the USA wanted poor children to have the benefit of a
blood lead test then there are several national laboratories
willing and available to do such analysis. See Declaration of Dr.
18
Michael J. Nicar; affidavit of Dr. Rosen. The lack of capacity
is a camouflage for the federal government’s real interest in
promoting the use of the EP test -- saving money. See Dr. Bind-
er’s article [copy attached to Beshara declaration].
The capacity argument, if accepted, would also negate the
other part of the USA’s argument -- the states must use blood
lead testing for high risk children. If a state lacks capacity
to perform blood lead tests for low risk children and that lack
is excused, the same lack of capacity would prevent the use for
high risk children and would also be excused. The USA should not
be allowed to hide behind the ambiguities of the word "capacity"
to avoid the statute’s mandate.
E. HCFA guidelines and CDC
The United States says in its brief that the delay in the
HCFA guidelines for a "transition" period for the states to
change over to blood lead testing is consistent with the October
1991 CDC statement.
Plaintiffs have a simple reply. To the extent that the
October 1991 CDC statement calls for a transition period then the
CDC statement is inconsistent with the Medicaid statute. The
statute mentions nothing about a transition period. 42 U.S.C. §
1396d(r)(1)(B) (iv). The statute mentions nothing about allowing
a transition period for these poor children because this would be
a good area for the federal government and the states to save
some money by using a useless screening test. The CDC statement
is an official publication of defendant United States. The
19
extent to which the CDC statement is inconsistent with the
statute is simply more evidence that the United States continues
to harm the plaintiffs and the class.
III. Conclusion
The USA has failed to show that it is entitled, as a matter
of law, to a judgment dismissing the case. The motions for
summary judgment and to dismiss should be denied.
Respectfully Submitted,
MICHAEL M. DANIEL, P.C.
3301 Elm Street
Dallas, Texas 75226-1637
(214) 939-9230
(214) 939-9229 (FAX)
oo) on /
| \ 4
By: am Uo. Nero oo”
Michael M. Dani@l
State Bar No. 05360500
) ¢ ATR TH 3 By: XNA (SNR
“Laura B. Beshara
State Bar No. 02261750
ATTORNEYS FOR PLAINTIFFS
CERTIFICATE OF SERVICE
I certify that a true and correct copy of the above doclment
A
was served upon counsel for defendants by FAX on this the //Aday
of December, 1992.
Suna Fin} Kehaia
““T,aura B. Beshara
20
CDC October 1981 Screening requirements * HCFA 9/19/92 guidelines * Texas January 1992 EPSDT Medical Screening * Texas "Laboratory Screening Services"
[plaintiffs' exhibit #14, page 44] * [plaintiffs' exhibit #3] * [plaintiffs' exhibits # 10—10C] * [plaintiffs’ exhibit #5, pages 5—13]
I. High risk according to questions * |. High risk according to questions * |. High risk according to questions * Primary screening test for lead is EP.
= - - : mk . - - - - 4 = - -* A blood lead level is run only when
Initial blood lead level test at 6 months * Initial blood lead level test at 6 months * Initial blood lead level test at 6 months * EP = or > 35 ug/dL.
* %* *
If test < 10 ug/dL, * |ftest < 10 ug/dL, * |f test < 10 ug/dL, then * All of the retesting standards are in
then blood lead level test every 6 months. * then blood lead level OR EP test according * no rescreening required under periodicity or followup care * terms of the EP test results.
* to State's periodicity schedule [In Texas, never]. * guidelines. * There is no high or low risk determination.
* * * Atleastas of July, 1992, Texas was still
If test = or > 10 ug/dL but <15, * |f test = or >10 ug/dL, then * |f initial blood lead test 10—14, then * following these standards.
then blood lead test every 3 or 4 months until level decreases, * follow up "blood tests" left to professional _* "consider rescreening" under follow-up care guidelines. *
* judgment with reference to CDC Statement. * *
If test = or >15 but <20, then * Both blood lead and EP are "blood tests". * |f initial blood lead test 15—19, then :
then blood lead test every 3 or 4 months until level decreases, * * rescreen in 3 months under follow —up care guidelines. *
* * *
If test = or > 20, then & * |f initial blood lead test 20—69, then *
then blood lead test every 3 or 4 months until level decreases, * * "monitor blood lead" under follow—up care guidelines. *
* * *
Il. Low risk according to questions * |. Low risk according to questions * |I. Low risk according to questions *
- - - x ————— — pv. J -— - -%
initial blood lead level test at 12 months. * |nitial EP OR blood lead test at 12 months. * |nitial blood lead level test at 6 months, x
% * no other blood lead level test required at *
If test < 10 ug/dL, then * * any age under Texas periodicity schedule. The EPtestis *
blood lead level test at 24 months. * * mandatory for each nutritional assessment. *
* * *
If test 10—14 ug/dL, then * * ®
then blood lead test every 3 or 4 months until level decreases, * * Li
* * *
If test = or >15 ug/dL, then x : *
blood lead level test every 3 or4 months. * * x
* * *
Second blood lead level test at 24 months. * Second EP OR blood lead test at 24 months. 3 *
* *
* %* Ill. Rescreening of plaintiffs given initial blood lead test results and assuming high risk status
Taylor's first test was 9 ug/dL [ plaintiffs’ exhibit #9].
Under CDC, she would receive a blood lead
test within 6 months.
Zachery's first test was 21 ug/dL but
he was retested at 7 ug/dL [plaintiffs' ex. #8A]. Under CDC
he would receive another blood lead
test not later than 6 months and possibly
within 3 to 4 months until level decreases.
Calvin's first test was 19 ug/dL but
he was retested at 14 ug/dL [plaintiffs’ ex #9B]. Under CDC
he would receive another blood lead
test within 3 to 4 months until level decreases.
Prentiss’ first test was 18 ug/dL but
he was retested at 14 ug/dL [plaintiffs’ ex #9C]. Under CDC
he would receive another blood lead
test within 3 or 4 months until level decreases. *
%
%
%*
%
%
%
%
%
X
%
%
%
%
%
%
%
*
»
-
(O
F
JA
S
C
E
RE
RE
E
E
S
E
BR
i
N
E
E
L
a
E
BE
BE
ER
SU
L
SS
aE
|
Under HCFA, Taylor could receive a retest
using EP or blood lead according to
the State periodicity schedule.
Under HCFA, Zachery could recieve a retest
using EP or blood lead according to
the State periodicity schedule.
Under HCFA, any followup tests for Calvin
would be "blood tests" with “reference
to CDC statement" and professional
judgment.
Under HCFA, any followup tests for Prentiss
would be "blood tests" with "reference
to CDC statement" and professional
judgment.
Under this State standard, Taylor will
receive no rescreening except for the EP test given as
part of the nutritional assessment.
Under this State standard, Zachery will
receive no rescreening except for the EP test given as
part of the nutritional assessment.
Under this State standard, Calvin will only
be considered for rescreening other than the EP test
given as part of the nutritional assessment.
Under this State standard, Prentiss will only
be considered for rescreening other than the EP test
given as part of the nutritional assessment.
* Under this standard, none of the plaintiffs
* will receive any rescreening except for the
* periodic EP test.
*
*
0%
%*
%
%
%
%
%*
%
¥
%
%
¥
¥
%*