Declaration of Michael M. Daniel in Support of Motion for Tro Against the USA with Certificate of Service and Attached Manuals
Public Court Documents
September 2, 1992
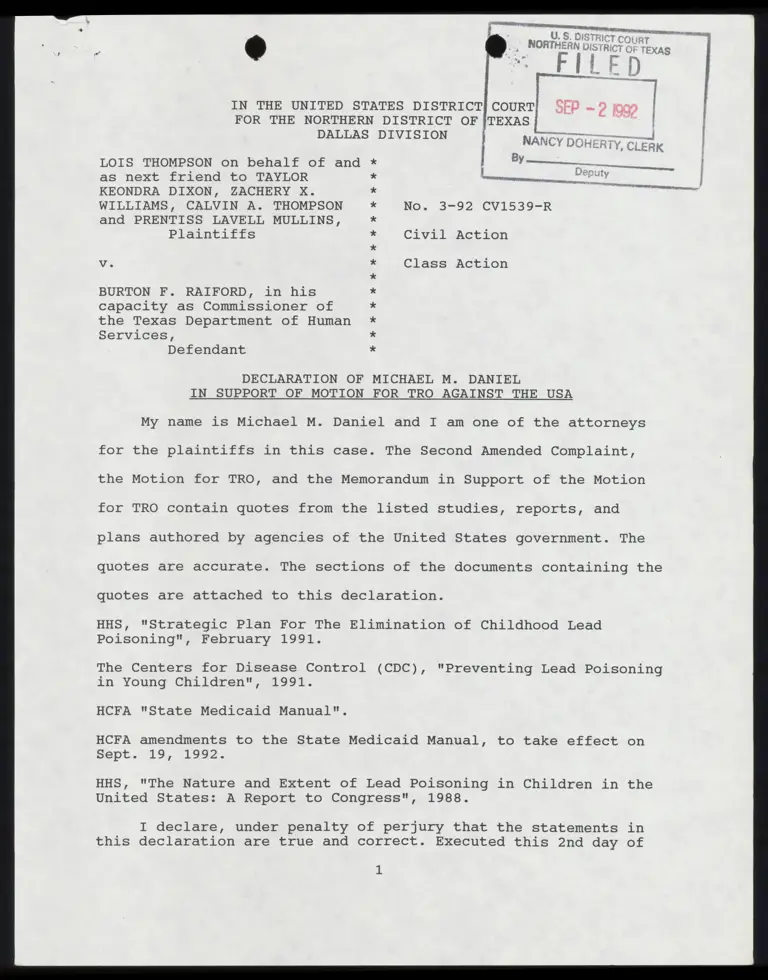
27 pages
Cite this item
-
Case Files, Thompson v. Raiford Hardbacks. Declaration of Michael M. Daniel in Support of Motion for Tro Against the USA with Certificate of Service and Attached Manuals, 1992. 87610cfb-5d40-f011-b4cb-002248226c06. LDF Archives, Thurgood Marshall Institute. https://ldfrecollection.org/archives/archives-search/archives-item/f92f99ae-d961-42a2-b6dc-a833acd600b7/declaration-of-michael-m-daniel-in-support-of-motion-for-tro-against-the-usa-with-certificate-of-service-and-attached-manuals. Accessed February 12, 2026.
Copied!
A
{ | JUR T
y ¢
IN THE UNITED STATES DISTRICT
FOR THE NORTHERN DISTRICT OF
DALLAS DIVISION |
—
NANCY DOHERTY, CLERK
BY
A S——————
D 5 : . y : v a ————
LOIS THOMPSON on behalf of and *
as next friend to TAYLOR
KEONDRA DIXON, ZACHERY X.
WILLIAMS, CALVIN A. THOMPSON
and PRENTISS LAVELL MULLINS,
Plaintiffs
TS.
:
BRS
— J mar
No. 3-92 CV1539-R
Civil Action
Vv. Class Action
BURTON F. RAIFORD, in his
capacity as Commissioner of
the Texas Department of Human
Services,
Defendant ¥
OX
OX
¥
OX
XH
XH
¥
XX
¥
¥
¥
¥*
DECLARATION OF MICHAEL M. DANIEL
IN SUPPORT OF MOTION FOR TRO AGAINST THE USA
My name is Michael M. Daniel and I am one of the attorneys
for the plaintiffs in this case. The Second Amended Complaint,
the Motion for TRO, and the Memorandum in Support of the Motion
for TRO contain quotes from the listed studies, reports, and
plans authored by agencies of the United States government. The
quotes are accurate. The sections of the documents containing the
quotes are attached to this declaration.
HHS, "Strategic Plan For The Elimination of Childhood Lead
Poisoning", February 1991.
The Centers for Disease Control (CDC), "Preventing Lead Poisoning
in Young Children", 1991.
HCFA "State Medicaid Manual".
HCFA amendments to the State Medicaid Manual, to take effect on
Sept. 19, 1992.
HHS, "The Nature and Extent of Lead Poisoning in Children in the
United States: A Report to Congress", 1988.
I declare, under penalty of perjury that the statements in
this declaration are true and correct. Executed this 2nd day of
1
=~ rg »
September, 1992.
WM. \
Michael M. Daniel
Respectfully submitted,
MICHAEL M. DANIEL, P.C.
3301 Elm Street
Dallas, Texas 75226-1637
(214) 939-9230 (telephone)
(214) 939-9229 —-
By: Tho ar OW
Michael M. Daniel
State Bar No. 05360500
By: Xora A. Rapala
Faura B. Beshara
State Bar No. 02261750
ATTORNEYS FOR PLAINTIFF
CERTIFICATE OF SERVICE
I certify that a true and correct copy of the above document
was served upon counsel for defendants by FAX and by being placed
in the U.S. Mail, first class postage prepaid, on the 044 day
of Seotemfeh ; 1992.
Ca loo. favfprg
Laura B. Beshara
State Medicaid Manual
Part 5 - Early and Periodic Screening
Diagnosis, and Treatment (EPSDT)
HCFA Pub 45-5
09-92
Rev. 5
Retrieval Title: R5.SM5
REVISED MATERIAL REVISED PAGES REPLACED PAGES
Sec. 5123.2. (Cont .)58-13.~ 5-16.1 (5 pp.) 5-13 - 5-16 (4 pp.)
CHANGED IMPLEMENTING INSTRUCTIONS--EFFECTIVE DATE: 09/19/92
Section 5123.2, Screening Service Content.--Part D of this
section, Appropriate Laboratory Tests, has been revised to update
HCFA policies and provide guidance to States for lead toxicity
screening through the Early and Periodic Screening, Diagnosis and
Treatment (EPSDT) program after considering the October 1991
statement of the Centers for Disease Control (CDC), Public Health
service, Preventing Lead Poisoning in Young Children. The CDC
statement lowered the blood lead level threshold at which followup
and interventions are recommended for children from 25 micrograms
per deciliter (ug/dL) of whole blood to 10 ug/dL.
Given the current state of the art of lead poisoning-related
technology instrumentation and the limitations in resources
available to States for lead poisoning prevention and treatment
efforts, HCFA is issuing this first phase of guidance. In many
States, the public health agency is leading the effort to
implement the new CDC guidelines. HCFA intends to provide enough
flexibility in the screening guidelines to allow State Medicaid
agencies to function within the overall plan of their State health
department.
while HCFA wants to stress that blood lead testing is the
screening test of choice, HCFA acknowledges that it will take some
time for States to make a transition to blood lead testing. The
erythrocyte protoporphyrin (EP) test is not sensitive for blood
lead levels below 25 ug/dL. However, HCFA recognizes that the
capacity may not exist in every community for analyzing blood lead
for every Medicaid eligible child. States continue to have the
option to use the EP test as the initial screening blood test.
However, elevated EP tests must be confirmed with a blood lead
test. Additionally, while HCFA recommends venous blood lead
tests, HCFA understands the hesitation of some practitioners to
perform venous blood tests on small children. In these
circumstances, a capillary specimen may be used for the initial
blood lead test to be followed, if necessary, with a venous blood
lead test. HCFA will consider guidelines for a next phase based
on State or community laboratory testing capacities and any
further revisions to CDC's statement.
A change has been made to Part C, Appropriate Immunizations, by
listing two additional immunizations which should be provided when
medically necessary and appropriate.
:
EARLY AND PERIODIC SCREENING,
09-92 DIAGNOSTIC AND TREATMENT SERVICES 5123.2 (Cont.)
o In screening for developmental assessment, the
examiner incorporates and reviews this information in conjunction
with other information gathered during the physical examination
and makes an objective professional judgement whether the child
is within the expected ranges. Review developmental progress, not
in isolation, but as a component of overall health and well-being,
given the child's age and culture.
o Developmental assessment should be culturally
sensitive and valid. Do not dismiss or excuse improperly
potential problems on grounds of culturally appropriate behavior.
Do not initiate referrals improperly for factors associated with
cultural heritage.
o Programs should not result in..a label or
premature diagnosis of a child. Providers should report only that
a condition was referred or that a type of diagnostic or treatment
service is needed. Results of initial screening should not be
accepted as conclusions and do not represent a diagnosis.
o Refer to appropriate child development resources
for additional assessment, diagnosis, treatment or follow-up when
concerns or questions remain after the screening process.
2. Assessment of Nutritional Status.--This is accomplished
in the basic examination through:
o Questions about dietary practices to identify unusual
eating habits (such as pica or extended use of bottle feedings)
or diets which are deficient or excessive in one or more
nutrients.
o A complete physical examination including an oral
dental examination. Pay special attention to such general features
as pallor, apathy and irritability.
o Accurate measurements of height and weight are among
the most important indices of nutritional status.
o A laboratory test to screen for iron deficiency.
HCFA and PHS recommend that the erythrocyte protoporphyrin (EP)
test be utilized when possible for children ages 1-5. It is a
simple, cost effective tool for screening for iron deficiency.
Where the EP test is not available, use hemoglobin concentration
or hematocrit.
lo) If feasible, screen children over 1 year of age for
serum cholesterol determination, especially those with a family
history of heart disease and/or hypertension and stroke.
If information suggests dietary inadequacy, obesity or other
nutritional problems, further assessment is indicated, including:
o Family, socioeconomic or any community factors,
EARLY AND PERIODIC SCREENING,
5123.2 (Cont.) DIAGNOSTIC AND TREATMENT SERVICES 09-92
o Determining quality and quantity of individual diets
(e.g., dietary intake, food acceptance, meal patterns, methods of
food preparation and preservation, and utilization of food
assistance programs),
o Further physical and laboratory examinations, and
o Preventive, treatment and follow-up services,
including dietary counseling and nutrition education.
B. Comprehensive Unclothed Physical Examination: --This
includes the following:
1. Physical Growth.--Record and compare the child's height
and weight with those considered normal for that age. (In the
first year of life, head circumference measurements are
important). Use a graphic recording sheet to chart height and
weight over time.
2. Unclothed Physical Inspection.--Check the general
appearance of the child to determine overall health status. This
process can pick up obvious physical defects, including orthopedic
disorders, hernia, skin disease, and genital abnormalities.
Physical inspection includes an examination of all organ systems
such as pulmonary, cardiac, and gastrointestinal.
C. Appropriate Immunizations.--Assess whether the child has
been immunized against diphtheria, pertussis, tetanus, polio,
measles, rubella, mumps, Haemophilus b Conjugate (HIB) and
hepatitis B and whether booster shots are needed. The child's
immunization record should be available to the provider. When an
immunization or an updating is medically necessary and
appropriate, provide it and so inform the «child's health
supervision provider.
Provide immunizations as recommended by the American Academy of
Pediatrics (AAP) and/or local health departments.
D. Appropriate Laboratory Tests .--Identify, as statewide
screening requirements, the minimum laboratory tests or analyses
to be performed by medical providers for particular age or
population groups. Physicians providing screening/assessment
services under the EPSDT program use their medical judgement in
determining the applicability of the laboratory tests or analyses
to be performed. If any laboratory tests or analyses are medically
contraindicated at the time of screening/assessment, provide them
when no longer medically contraindicated. As appropriate, conduct
the following laboratory tests:
1. Lead Toxicity Screening.--All children ages 6 months to
72 months are considered at risk and must be screened for lead
poisoning. Complete lead screening consists of both a verbal risk
assessment and blood test(s). Each State establishes its own
periodicity schedule after consultation with medical organizations
involved in child health. These periodicity schedules and any
other associated office visits must be used as an opportunity for
anticipatory guidance and risk assessment for lead poisoning. As
part of the nutritional assessment conducted at each periodic
screening, an EP blood test may be done to test for iron
deficiency. This blood test may also be used as the initial
screening blood test for lead toxicity.
a. Risk Assessment. All children from 6 to 72 months
of age are considered at risk and must be screened, unless it can
be shown that the community in which the children live does not
have a childhood lead poisoning problem. Only an official State
or local health authority can declare that a
5-14
Rev. 5
EARLY AND PERIODIC SCREENING,
09-92 DIAGNOSTIC AND TREATMENT SERVICES 5123.2
{Cont .)
geographic community, or part of a community, does not have a
problem. However, all children moving into ‘a "lead-free
community" must be screened. Regardless of their risk, all
families must be given detailed lead poisoning prevention
counselling as part of the anticipatory guidance during the
screening visit.
Beginning at six months of age and at each visit thereafter, the
provider must discuss with the child's parent or guardian
childhood lead poisoning interventions and assess the child's risk
for exposure. Ask the following types of questions at a minimum.
o Does your child live in or regularly visit an old house
built before 19607? was your child's day care
center/preschool/babysitter’'s home built before 1960? Does the
house have peeling or chipping paint?
o Does your child live in a house built before 1960 with
recent, ongoing or planned renovation or remodeling?
o Have any of your children or their playmates had lead
poisoning?
o Does your child frequently come in contact with an adult
who works with lead? Examples are construction, welding, pottery,
or other trades practiced in your community.
o Does your child live near a lead smelter, battery recycling
plant, or other industry likely to release lead such as (give
examples in your community)?
o Do you give your child any home or folk remedies which may
contain lead?
o Does your child live near a heavily travelled major highway
where soil and dust may be contaminated with lead?
o Does your home's plumbing have lead pipes or copper with
lead solder joints?
Ask any additional questions that may be specific to situations
which exist in a particular community.
b. Determining Risk.--Risk is determined from. the
response to the questions which your State requires for verbal
risk assessment.
o If the answers to all questions are negative, a child is
considered low risk for high doses of lead exposure, but must
~
I~
receive blood lead screening by EP or blood lead test at 12 months
of age.
lo) If the answer to any question is positive, a child is
considered high risk for high doses of lead exposure. A blood
lead test must be obtained at the time a child is determined to
be high risk.
Subsequent verbal risk assessments can change a child's risk
category. Any information suggesting increased lead exposure for
previously low risk children must be followed up with a blood lead
test.
Rev. 5
5-15
EARLY AND PERIODIC SCREENING,
5123.2 (Cont.) DIAGNOSTIC AND TREATMENT SERVICES 09-92
Cc. Screening Blood Tests.--The term screening blood
tests refers to blood tests for children who have not previously
been tested for lead with either the EP or blood lead test or who
have been previously tested and found not to have an elevated EP
or blood lead level. If a child is determined by the verbal risk
assessment to be at:
(1) Low Risk.--A screening EP test or a blood lead
test is required at 12 months and a second EP test or a blood lead
test at 24 months.
(2) High Risk.--A blood lead test is required when
a child is identified as being high risk, beginning at six months
of age. If the initial blood lead test results are less than (<)
10 micrograms per deciliter (ug/dL), a screening EP test or blood
lead test is required at every visit prescribed in your EPSDT
periodicity schedule through 72 months of age.
If a child between the ages of 24 months and 72 months has not
received a screening blood test, then that child must receive it
immediately, regardless of being determined at low or high risk.
An elevated EP test must be confirmed with a blood lead test. A
blood lead test result equal to or greater than (>) 10 ug/dL
obtained by capillary specimen (fingerstick) must be confirmed
using a venous blood sample.
d. Diagnosis, Treatment and Follow-up.--If a child is
found to have blood lead levels equal to or >10 ug/dL, providers
are to use their professional judgment, with reference to CDC
guidelines covering patient management and treatment, including
follow up blood tests and initiating investigations to the source
of lead, where indicated. Determining the source of lead may be
reimbursable by Medicaid.
e. Coordination With Other Agencies. Coordination with
WIC, Head Start, and other private and public resources enables
elimination of duplicate testing and ensure comprehensive
diagnosis and treatment. Also, public health agencies' Childhood
Lead Poisoning Prevention Programs may be available. These
agencies may have the authority and ability to investigate a lead-
poisoned child's environment and to require remediation.
2. Anemia Test.--The most easily administered test for
anemia is a microhematocrit determination from venous blood or a
fingerstick.
3. Sickle Cell Test.--Diagnosis for sickle cell trait may
be done with sickle cell preparation or a hemoglobin solubility
test. If a child has been properly tested once for sickle cell
EARLY AND PERIODIC SCREENING,
09-92 DIAGNOSTIC AND TREATMENT SERVICES 5123.2
{Cont )
(or guardians) and children is required and is designed to assist
in understanding what to expect in terms of ‘the “child's
development and to provide information about the benefits of
healthy lifestyles and practices as well as accident and disease
prevention.
F. Vision and Hearing Screens.--Vision and hearing services
are subject to their own periodicity schedules (as described in
§5140) . However, where the periodicity schedules coincide with
the schedule for screening services (defined in §5122A), you may
include vision and hearing screens as a part of the required
minimum screening services.
1. Appropriate Vision Screen.--Administer an age-
appropriate vision assessment. Consultation by ophthalmologists
and optometrists can help determine the type of procedures to use
and the criteria for determining when a child is referred for
diagnostic examination.
2. Appropriate Hearing Screen.--Administer an age-
appropriate hearing assessment. Obtain consultation and suitable
procedures for screening and methods of administering them from
audiologists, or from State health or education departments.
G. Dental Screening Services.--Although an oral screening may
be part of a physical examination, it does not substitute for
examination through direct referral to a dentist. A direct dental
referral is required for every child in accordance with your
periodicity schedule and at other intervals as medically
necessary. Prior to enactment of OBRA 1989, HCFA in consultation
with the American Dental Association, the American Academy of
Pediatrics and the American Academy of Family Practice, among
other organizations, required direct referral to a dentist
beginning at age 3 or at an earlier age if determined medically
necessary. The law as amended by OBRA 1989 requires that dental
services (including initial direct referral to a dentist) conform
to your periodicity schedule which must be established after
consultation with recognized dental organizations involved in
child health care.
Especially in older children, the periodicity schedule for dental
examinations is not governed by the schedule for medical
examinations. Dental examinations of older children should occur
with greater frequency than is the case with physical
examinations. The referral must be for an encounter with a
dentist, or a professional dental hygienist under the supervision
of a dentist, for diagnosis and treatment. However, where any
screening, even as early as the neonatal examination, indicates
that dental services are needed at an earlier age, provide the
needed dental services.
The requirement of a direct referral to a dentist can be met in
settings other than a dentist's office. The necessary element is
that the child be examined by a dentist or other dental
professional under the supervision of a dentist. In an area where
dentists are scarce or not easy to reach, dental examinations in
a clinic or group setting may make the service more appealing to
recipients while meeting the dental periodicity schedule. 1£
continuing care providers have dentists on their staff, the direct
referral to a dentist requirement is met. Dental
paraprofessionals under direct supervision of a dentist may
perform routine services when in compliance with State practice
acts.
Determine whether the screening provider or the agency does the
direct referral to a dentist. You are ultimately responsible for
assuring that the direct referral is made and that the child gets
to the dentist's office in a timely manner. ;
Developed for the Risk Management Subcommittee, Committee
to Coordinate Environmental Health and Related Programs,
U.S. Department of Health and Human Services.
February 1991
= U.S. DEPARTMENT OF HEALTH
3 AND HUMAN SERVICES
1 Public Health Service
%,
Centers for Disease Control
ayg1a
water, food, and air would help reduce the prevalence of lead poisoning and would help
protect children with blood lead levels below the current definition of lead poisoning
from adverse effects.
The role of exposure to soil lead, both directly and through the contribution of soil lead
to lead in housedust, is still being investigated. The nature and degree of soil lead
abatement that would be appropriate is unclear. The research needed to resolve the soil
lead issues will take years. However, since so many children are being poisoned by
lead-based paint, significant action on lead-based paint abatement should not be delayed
while we await the results of research. Decisions on how to set up rational soil lead
abatement programs will have to be made separately as more data become available.
(However, it is critical not to further contaminate the soil during lead-based paint
abatement efforts.)
We have made substantial progress in reducing exposure to lead; deaths and severe
illness from lead poisoning (e.g., encephalopathy) are now rare. The results of recent
studies indicate, however, that blood lead levels previously believed to be safe are
adversely affecting the health of children. Millions of children in the United States are
believed to have blood lead levels high enough to affect intelligence and development.
The need to deal with preventing exposure at these lower levels will require increased
efforts. The Administration is responding to this problem with increased resources. In
FY 1992, the President’s budget calls for $14.95 million for the lead poisoning prevention
program at the Centers for Disease Control and $25 million for the new HOME
abatement program of the Department of Housing and Urban Development.
In many ways, the tone of this report is one of understatement. The enormity of the task
of eliminating childhood lead poisoning and the extensive public health benefits to be
gained are very clear. This strategic plan is at best a first step. More detailed plans for
implementation must follow, and then the work itself must be done.
Childhood lead poisoning has already affected millions of children, and it could affect
millions more. Its impact on children is real, however silently it damages their brains
and limits their abilities. Deciding to develop a strategic plan for the elimination of
childhood lead poisoning is a bold step, and achieving the goal would be a great
advance.
iii
STRATEGIC PLAN FOR THE
ELIMINATION OF CHILDHOOD LEAD POISONING
EXECUTIVE SUMMARY
The U.S. Public Health Service Year 1990 and Year 2000 Objectives for the Nation aim
for progressive declines in the numbers of lead-poisoned children in the United States,
leading to the elimination of this disease. We believe that a concerted society-wide
effort could virtually eliminate this disease as a public health problem in 20 years.
This plan, developed for the Committee to Coordinate Environmental Health and
Related Programs of the U.S. Department of Health and Human Services, provides an
agenda for the first 5 years of a comprehensive society-wide effort to eliminate childhood
lead poisoning. The results and experience from this 5-year program will lead to the
agenda for the following 15 years.
Lead is a poison that affects virtually every system of the body. Results of recent studies
have shown that lead’s adverse effects on the fetus and child occur at blood lead levels
previously thought to be safe; in fact, if there is a threshold for the adverse effects of
lead on the young, it may be close to zero.
Lead poisoning remains the most common and societally devastating environmental
disease of young children. Enormous strides have been made in the past 5 to 10 years
that have increased our understanding of the damaging, long-term effects of lead on
children’s intelligence and behavior. Today in the United States, millions of children
from all geographic areas and socioeconomic strata have lead levels high enough to
cause adverse health effects. Poor, minority children in the inner cities, who are already
disadvantaged by inadequate nutrition and other factors, are particularly vulnerable to
this disease.
Childhood lead exposure costs the United States billions of dollars from medical and
special education costs for poisoned children, decreased future earnings, and mortality of
newborns from intrauterine exposure to lead. Childhood lead poisoning continues in our
society primarily because of lead exposure in the home environment, with lead-based
paint being the principal high-dose source. It is the most important source for the
highest-risk children (e.g., those with blood lead levels > 25 ug/dL); preventive actions
for such exposures should receive the highest priority.
X1
The CDC Categorical Grant Program was authorized by the Lead Contamination
Control Act of 1988. This program provides for childhood lead screening by State and
local agencies, referral of children with elevated blood lead levels for treatment and
environmental interventions, and education about childhood lead poisoning prevention.
Money for this program was first appropriated in FY 1990. The President’s budget for
FY 1992 contains $14.95 million for this program, an increase of $7.16 million from FY
1991.
Other government-funded child health programs also conduct some childhood lead
screening. These programs include Medicaid’s Early and Periodic Screening, Diagnostic,
and Treatment Program (EPSDT); the Supplemental Food Program for Women, Infants,
and Children (WIC); and Head Start.
EPSDT is a comprehensive prevention and treatment program available to
Medicaid-eligible persons under 21 years of age. In 1989, of the 10 million eligible
persons, more than 4 million received initial or periodic screening health examinations.
These are provided at a variety of sites (for example, physician offices, public health
clinics, and community health centers) by private or public sector providers. Screening
services, defined by statute, must include a blood lead assessment "where age and risk
factors indicate it is medically appropriate." (The requirements for a blood lead
assessment are not further defined.) In addition, the EP test is recommended for
children ages 1 to 5 years to screen for iron deficiency. Because this test is also useful in
identifying children with blood lead levels > 25 ug/dL, many children being screened for
iron deficiency are screened for lead poisoning at the same time. The guidelines for
States indicate that environmental investigations for lead-poisoned children are covered
under EPSDT, although abatement is not. However, specific criteria for screening and
the determination of what Medicaid will cover are decided on a State-by-State basis.
Thus, many States do not conduct much screening or do not pay for environmental
investigations for poisoned children. National data are not available on the numbers of
children screened for lead poisoning through EPSDT, since State-reported Medicaid
performance and fiscal data are not broken down to such specific elements.
The U.S. Department of Agriculture’s WIC program serves pregnant and postpartum
women and children under 5 years of age in low-income households. Program benefits
include supplemental food, nutrition education, and encouragement and coordination for
the use of other existing health services. As of March 1988, an estimated 1.63 million
children ages 1 to 4 years were participating in WIC. Although children must undergo a
medical or nutritional assessment or both to be certified to receive benefits, Federal
WIC regulations permit States to establish their own requirements for WIC certification
examinations. These regulations permit the use of an EP test for certification and define
lead poisoning as a nutritionally-related medical condition that can be the basis of
certifying a child to receive WIC benefits. Most WIC programs that perform EP tests
use them to screen for iron deficiency, although hematocrit or hemoglobin measurements
are most commonly used for this purpose. The nutritional education and supplemental
food provided by WIC are undoubtedly important in reducing lead absorption in many
children and pregnant women.
Page 18
The expansion of screening programs will result in a demand for training programs on
childhood lead screening and the investigation of environmental sources. The Louisville,
Kentucky, training program can serve as a model for other such programs. This program
provides methods for assessing lead poisoning in high-risk populations and demonstrates
the integration of lead screening with basic child health services and the technical and
management skills needed for an effective and efficient childhood lead poisoning
prevention program.
In addition, increased screening will lead to a demand for increased laboratory services.
In 1991 CDC will likely issue new recommendations suggesting that screening programs
attempt to identify children with blood lead levels below 25 ug/dL. This change will
mean that blood lead measurements must be used for childhood lead screening instead
of EP measurements. When this happens, the demand for increased blood lead testing
will far exceed current capacity. In addition, cheaper, easier to use, and portable
instrumentation for blood lead testing will need to be developed. Furthermore, existing
programs for proficiency testing and certification of laboratories will have to be
expanded. With concen about health effects at low blood lead levels, laboratories will
be called upon to do better measurements in the 4 to 5 ug/dL range. As a result, major
efforts will be needed to improve laboratory quality assurance and control at these lower
levels. Reference materials for laboratories performing blood lead measurements and
technical assistance will be required to improve laboratory quality.
Page 23
Studies should be conducted on the cost-effectiveness of different strategies for
childhood lead screening. These strategies include screening in inner-city emergency
rooms to reach children who have no ongoing source of care and "cluster testing” of all
children in multiple dwelling units where cases of childhood lead poisoning have been
identified. The usefulness of screening in day care centers and nursery schools should
also be evaluated. In addition, Federal programs now funding childhood lead screening
should be evaluated to see how they can work together for a most efficient use of
resources.
At present it is much cheaper and easier to perform an EP test than a blood lead
measurement; however, the EP test is not a useful screening test for blood lead levels
below 25 ug/dL. Both because of the expected increase in screening and because of the
concern about the health effects of lower blood lead levels, the demand for blood lead
testing is likely to increase. The development of portable, easy-to-use, cheaper
instrumentation for blood lead measurement is extremely important.
Because capillary (or fingerstick) blood samples may be easily contaminated with lead on
the skin, venous blood must be used to confirm lead poisoning in children. Several
capillary blood collection devices now on the market purport to collect blood free of
surface finger contamination from lead. These devices should be evaluated for ease of
use and ability to collect an uncontaminated sample.
The education of families about lead poisoning by childhood lead poisoning prevention
programs often includes information about the importance of nutrition. Because of our
growing concern about the adverse effects of low blood lead levels, nutritional
interventions are likely to be recommended for more children. A number of nutritional
factors have been shown experimentally to influence the absorption of lead and its
concentrations in tissues. Intervention studies or clinical trials should be conducted to
establish that increasing the regularity of meals and ensuring adequate dietary intake of
iron and calcium can reduce blood lead levels.
Educational strategies for increasing medical care provider and public awareness of lead
poisoning should also be evaluated for their efficacy in reducing children’s blood lead
levels and preventing lead poisoning.
Page 40
i ! VI,
+" 1
{
{
i
( A STATEMENT BY THE CENTERS FOR DISEASE CONTROL — OCTOBER 1991
oR tyvqya
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES / Public Health Service / Centers for Disease Control
RN)
<x
0)
=
~
-'
<
wd
*
°
No
.
51
13
PLAINTIFF'S
EXHIBIT 2
§ CA3-85-,2/0-0
2 WALKER v. NUD
Large numbers of children continue to have blood lead levels high enough to cause
adverse effects.
:
Substantial progress has been made, however, in reducing blood lead levels in the
United States.
Lead-based paint remains the major source of high-dose lead poisoning in the United
States.
The Agency for Toxic Substances and Disease Registry estimated that in 1984, 17% of all
American preschool children had blood lead levels that exceed 15 pg/dL (ATSDR, 1988).
Although all children are at risk for lead toxicity, poor and minority children are dispropor-
tionately affected. Lead exposure is at once a by-product of poverty and a contributor to the
cycle that perpetuates and deepens the state of being poor.
Substantial progress has been made in reducing blood lead levels in U.S. children. Perhaps
the most important advance has been the virtual elimination of lead from gasoline. Close
correlations have been demonstrated between the decline in the use of leaded gasoline and
declines in the blood lead levels of children and adults between 1976 and 1980 (Annest, 1983)
(Figure 2-5). Levels of lead in food have also declined significantly, as a result both of the
decreased use of lead solder in cans and the decreasing air lead levels.
Lead-based paint remains the major source of high-dose lead poisoning in the United States.
Although the Consumer Products Safety Commission (CPSC) limited the lead content of new
residential paint starting in 1978, millions of houses still contain old leaded paint. The
Department of Housing and Urban Development estimates that about 3.8 million homes with
young children living in them have either nonintact lead-based paint or high levels of lead in
dust (HUD, 1990).
Figure 2-5. Change in blood lead levels in relation to a decline in use of leaded
gasoline, 1976-1980
110
|
: : 16
100 - Lead used in gasoline
Zz
15
ud
- 14
80 { Average blood
lead levels
ro
(1
p/
3r
1)
sp
aa
1
pe
a
po
or
He
sm
y
To
ta
l
Le
ad
Us
ed
Pe
r
6
M
o
n
t
h
Pe
ri
od
(1
00
0
To
ns
)
70 A
60 -
11
50 1 ;
.
- 10
> : I
T T T T T Ir ;
T1976 1977 1978 1979 1980
Year
Source: Annest JL, 1983.
12
f' SCREENING METHOD
Screening should be done using a blood lead test.
Since erythrocyte protoporphyrin (EP) is not sensitive enough to identify more than a small
percentage of children with blood lead levels between 10 and 25 pg/dL. and misses many
children with blood lead levels =25 pg/dL (McElvaine et al., 1991), measurement of blood lead
levels should replace the EP test as the primary screening method. Unless contamination of
capillary blood samples can be prevented, lead levels should be measured on venous samples.
Obtaining capillary specimens is more feasible at many screening sites. Contamination of
capillary specimens obtained by finger prick can be minimized if trained personnel follow
proper technique (see Appendix I for a capillary sampling protocol). Elevated blood lead results
obtained on capillary specimens should be considered presumptive and must be confirmed using
venous blood. At the present time, not all laboratories will measure lead levels on capillary
specimens.
Programs will need to increase their capacity to perform blood lead testing. During the
transition to the use of the blood lead test as the primary screening method, some programs will
temporarily continue to use EP as a screening test. In addition, some nutrition programs (for
example, the Supplemental Food Program for Women, Infants, and Children (WIC)) use the EP
test to identify children with iron deficiency.
For a discussion of the units used to report EP results (Page 48). All EP test results of =35
pg/dL if standardized using 241 L cm-1 mmol-1, >28 pg/dL if standardized using 297 L cm-1
mmol-1, or =70 pmol 7nPP/mol heme, if the hematofluorometer reports in these units, must be
followed by a blood lead test (preferably venous) and an evaluation for iron deficiency (Page 53).
Work on developing easy-to-use, cheap, portable instruments for blood lead testing is ongoing.
ANTICIPATORY GUIDANCE AND ASSESSING RISK
Anticipatory guidance helps prevent lead poisoning by educating parents on ways to
reduce lead exposure.
Questions about housing and other factors are used to identify which children are at
greatest risk for high-dose lead exposure.
Anticipatory guidance and assessment of risk should be tailored to important sources
and pathways of lead exposure in the child’s community.
4
Guidance on childhood lead poisoning prevention and assessment of the risk of lead poisoning
should be part of routine pediatric care. Anticipatory guidance is discussed in more detail in
Chapter 4. The guidance and risk assessment should emphasize the sources and exposures that
are of greatest concern in the child’s community (Chapter 3). Because lead-based paint has been
used in housing throughout the United States, in most communities it will be necessary to focus
on this source.
41
® - ®
( state medicaid manual Fi in
Part 5 — Early and Periodic Screening, oie fun
Diagnosis, and Treatment
Transmittal No. 4
Date JULY 1990
REVISED MATERIAL REVISED PAGES REPLACED PAGES
Table of Contents
Part 5 5-1 (1 p.) 5-1 (1 p.) Sec. 5123.2 (Cont.) 5-15-5-16(2pp.) 5-15-5-16(2pp.) Sec. 5140 : 5-19 - 5-20(2 pp.) 5-19 - 5-20(2 pp.) Sec. 5320.2 (Cont.) 5-39-5-40 (2 pp.) 5-39-5-40 (2 pp.) Sec. 5350-5360 9-55-5-58 (4 pp.) 5-55 (1 p.)
CORRECTION—EFFECTIVE DATE: April 1, 1990
Section 5§123.2.D.1, Lead Toxicity Screening, is clarified to define lead poisoning and recommended testing.
;
Section 5140, Periodicity Schedule, issued in Transmittal 3, April 1890, incorrectly included a sentence which was inappropriate and misleading in the second paragraph ( under §5140.
NEW PROCEDURE—EFFECTIVE DATE: JULY-1,-1990 Ere ELA
___Sectioh 5320.2.D., Records or Information on Services and Recipients-Program ~~" Reports, is revised to briefly describe the content of the annual report (HCFA-416) which replaces the Quarterly report on the EPSDT program (HCFA-420),
Section 5360, Annual Participation Goals, describes the methods for setting annual and State-specific participation goals for early and periodic screening, diagnostic, and treatment services as required by §1905(r) of the Act, amended by §6403(c) of OBRA 89.
HCFA-Pub. 45-5
|
EARLY AND PERIODIC SCREENING,
07-90 DIAGNOSTIC AND TREATMENT SERVICES, 5123.2(Cont.)
Screen all Medicaid eligible children ages 1-5 for lead poisoning. Lead poisoning is
defined as an elevated venous blood lead level (i.e., greater than or equal to 25
micrograms per deciliter (ug/dl) with an elevated erythrocyte protoporphyrin (EP) level
(greater than or equal to 35 ug/dl of whole blood). In general, use the EP test as the
primary screening test. Perform venous blood lead measurements on children with
elevated EP levels.
Children with lead poisoning require diagnosis and treatment which includes periodic re-
evaluation and environmental evaluation to identify the sources of lead.
2. Anemia Test.—The most easily administered test for anemia is a
microhematocrit determination from venous blood or a fingerstick.
3. Sickle Cell Test.--Diagnosis for sickle cell trait may be done with sickle cell
preparation or a hemoglobin solubility test. If a child has been properly tested once for
sickle cell disease, the test need not be repeated.
4. Tuberculin Test.—Give a tuberculin test to every child who has not received
one within a year. ,
5. Others.—In addition to" the tests above, there are several other tests to
consider, Their appropriateness are determined by an individual's age, sex, health
history, clinical symptoms and exposure to disease. These include a urine screening,
pinworm slide, urine culture (for girls), serological test, drug dependency screening, stool
specimen for parasites, ova,blood, and HIV screening.
E. Health Education.—Health education is a required component of screening
services and includes anticipatory guidance. At the outset, the physical and dental
assessment, or screening, gives you the initial context for providing health education.
Health education and counselling to both parents (or guardians) and children is required
and is designed to assist in understanding what to expect in terms of the child's
development and to provide information about the benefits of healthy lifestyles and
practices as well as accident and disease prevention.
F. Vision and Hearing Screens.—Vision and hearing services are subject to their own
periodicity schedules (as described in §5140). However, where the periodicity schedules
coincide with the schedule for screening services (defined in §5122 A), you may include
vision and hearing screens as a part of the required minimum screening services.
1. Appropriate Vision Screen.—Administer an age-appropriate vision
assessment. Consultation by opthalmologists and optometrists can help determine the
type of procedures to use and the criteria for determining when a child should be referred
for diagnostic examination, :
: 2. Appropriate Hearing Screen.—Administer an age-appropriate hearing
assessment. Obtain consultation and suitable procedures for screening and methods of
administering them from audiologists, or from State health or education departments.
Rev. 4&4 i 5-15
The Nature and Extent of
Lead Poisoning 1 | g in Chi
In the United States: Lelrg
A Report to Congress
on G4 Ean
AR bg fs
Ah) A ALS As,
PLAINTIFF
EXHIBIT Be
(A3- s—]& 107
cer. v NUD
Bl
um
be
rg
No
.
51
13
AR aay
oy oS i tpt
i E wiasd
gh
SRE RE See
\
A
wl
bi
yet be routinely employed in screening programs. The kinetic, toxicological, and practical aspects of biological monitoring and other approaches to assess- ing lead exposure have been extensively discussed by U.S. EPA (1986a).
In young children, effects monitoring for lead exposure is primarily based on lead's impact on the heme biosynthetic pathway, as shown by (1) changes in the activity of key enzymes delta-aminolevulinic acid dehydratase (ALA-D) and delta-aminolevulinic acid synthetase (ALA-S), (2) the accumulation of copropor- phyrin in urine (CP-U), and (3) the accumulation of protoporphyrin in erythro- cytes (EP). For methodological and practical reasons, the EP measure is the effect index most often used in screening children and other population groups.
Effects monitoring for exposure in general and lead exposure in particular has drawbacks (Friberg, 1985). Effects monitoring is most useful when the endpoint being measured is specific to lead and sensitive to Tow levels of lead. Since EP levels can be elevated by iron deficiency,
young children
the other.
which is common in
, indexing one relationship requires quantitatively adjusting for
An elevated Pb-B level and, consequently, increased lead absorption may exist even when the EP value is within normal limits, now £35 micrograms (ug) EP/deciliter (d1) of whole blood. We might expect that in high-risk, low socioeconomic status (SES),
urban areas,
nutrient (including iron)-deficient children in
chronic Pb-B elevation would invariably accompany persistent EP
Analysis of data from the second National Health and Nutrition Examination Survey (NHANES II) by Mahaffey and Annest (1986) indicates that Pb-B levels in children can be elevated even when EP levels are normal. Of 118 children with Pb-B levels above 30 pg/dl (the CDC criterion level at the time of NHANES II), 47% had EP levels at or below 30 Mg/dl, and 58% (Annest and Mahaffey, 1984) had EP levels less than the current EP cutoff value of 35 ug/dl (cbc, 1985). This means that reliance on EP level for ini
can result in a significant incidence of false ne
toxic Pb-B levels.
elevation.
tial screening
gatives or failures to detect
This finding has important implications for the interpreta- tion of screening data, as discussed in Chapter V.
3. Environmental Sources of Lead in the United States with Reference to
Young Children and Other Risk Groups
As graphically depicted in Figure II-1, several environmental sources of lead exposure pose a risk for young children and fetuses. Many sources not
I1-9