Proposed Order RE: Partial Summary Judgment
Public Court Documents
June 7, 1991
19 pages
Cite this item
-
Case Files, Matthews v. Kizer Hardbacks. Proposed Order RE: Partial Summary Judgment, 1991. b1c857cb-5c40-f011-b4cb-7c1e5267c7b6. LDF Archives, Thurgood Marshall Institute. https://ldfrecollection.org/archives/archives-search/archives-item/c09c7903-4ef3-4781-9ce4-d14441487183/proposed-order-re-partial-summary-judgment. Accessed February 21, 2026.
Copied!
O
0
0
N
T
O
ae
r
N
e
e
[A
oa
-
-
po
t
fe
ps
t
fe
t
ay
bo
lt
p
t
po
t
~
~
©
WV
0
0
~
3
O
n
W
h
pb
W
W
O
N
H
O
iM 18
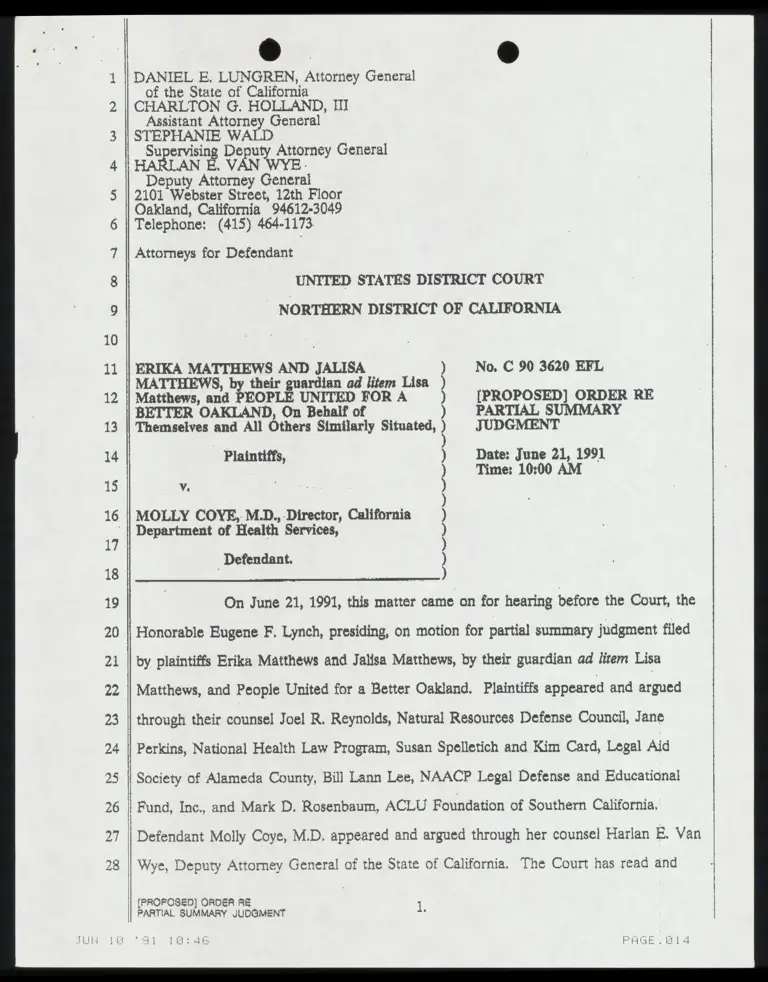
DANIEL E. LUNGREN, Attorney General
of the State of California
CHARLTON G. HOLLAND, III
Assistant Attorney General
STEPHANIE WALD
Supervising Deputy Attorney General
LAN E. VAN WYE
Deputy Attorney General
2101 Webster Street, 12th Floor
Oakland, California 94612-3049
Telephone: (415) 464-1173
Attorneys for Defendant
UNITED STATES DISTRICT COURT
NORTHERN DISTRICT OF CALIFORNIA
No. C 90 3620 EFL
[PROPOSED] ORDER RE
PARTIAL SUMMARY
JUDGMENT
Date: June 21, 1991
Time: 10:00 AM
ERIKA MATTHEWS AND JALISA
MATTHEWS, by their guardian ad litem Lisa
Matthews, and PEOPLE UNITED FOR A
BETTER OAKLAND, On Behalf of
Themselves and All Others Similarly Situated,
Plaintiffs,
|
MOLLY COYE, M.D, Director, California
Department of Health Services,
Defendant.
N
r
”
Y
a
”
Sa
ge
Sa
g”
Sp
t?
Na
nt
”
“
o
t
t
ni
t
“
e
t
?
o
p
t
”
“n
at
?
“s
ag
t”
“
v
t
“
a
t
”
“
u
t
”
On June 21, 1991, this matter came on for hearing before the Court, the
Honorable Eugene F. Lynch, presiding, on motion for partial summary judgment filed
by plaintiffs Erika Matthews and Jalisa Matthews, by their guardian ad lirem Lisa
Matthews, and People United for a Better Oakland, Plaintiffs appeared and argued
through their counsel Joel R. Reynolds, Natural Resources Defense Council, Jane
Perkins, National Health Law Program, Susan Spelletich and Kim Card, Legal Aid
Society of Alameda County, Bill Lann Lee, NAACP Legal Defense and Educational
Fund, Inc., and Mark D. Rosenbaum, ACLU Foundation of Southern California.
Defendant Molly Coye, M.D. appeared and argued through her counsel Harlan E. Van
Wye, Deputy Attorney General of the State of California. The Court has read and
(PROPOSED) ORDER RE 1
PARTIAL SUMMARY JUDGMENT .
21 10:40 PAGE.RL14
MI
O0
0
ed
O
n
c
ae
ur
fr
e
considered the moving and responding papers, all supporting papers and appended
documents, the record as a whole and the oral arguments of counsel. The issue having
been duly heard, decision is rendered as follows:
IT I$ HEREBY ORDERED, ADJUDGED AND DECREED:
1 Plaintiffs’ Motion for Partial Summary Judgment is denied on the
grounds that there are no triable issues of fact and that Defendant Molly Coye, M.D,
is entitled to judgment as a maiter of law in that there has been no showing that she
has failed to perform any duty to enforce the Medicaid Act, 42 U, S. C. Sections |
1396a(a)(43), 1396a(a)(4)(B), & (1), as construed in the State Medicaid Manual Section
5123.2(D), by not instructing health care providers who participate in the Medicaid
program to screen all Medicaid-cligible children ages 1-5 for lead poisoning by sing
the erythrocyte protoporphyrin (EP) test as the primary screening test and to perform
venous blood measurements on children with elevated EP levels; |
2 Summary judgment is entered in favor of Defendant Molly Coye,
M.D, igs
3 The Court declares that the Defendant Molly Coye, M.D. isinot in.
violation of 42 U.S.C. Sections 1396a(a)(43), d(2)(4)(B) and (r), as construed by the
State Medicaid Manual, Section 5123.2(D). |
4, Plaintiffs Erika Matthews, et al., are to take nothing; and
!
5 Defendant Molly Coye, M.D., is awarded her costs and fees herein.
DATED:
Prepared by:
DATED: June 7, 1991 "DANIEL E. LUNGREN, Attorney General
of the State of California
bt ithle
Deputy Attorney General
[ei\varwys\maithews.pod] Attorneys for Defendant
PROPOSED] ORDER RE 5
ARTIAL SUMMARY JUDGMENT :
"51. 1047 PAGE. IIS
DANIEL E. LUNGREN, Attorney General
of the State of California
CHARLTON G. HOLLAND, III
Assistant Attorney General
STEPHANIE WALD
Supervising Deputy Attorney General
TAN E VAN WYE |
Deputy Attorney General
2101 Webster Street, 12th Floor
Oakland, California 94612-3049
Telephone: (413) 464-1173
o
s
Attorneys for Defendant
UNITED STATES DISTRICT COURT
NORTHERN DISTRICT OF CALIFORNIA yo
og
~J
oy
]
Ln
fe
sd
bo
ek
oO
No. C 90 3620 EFL
DECLARATION OF MARIDEE
ANN GREGORY, M.D.
ERIKA MATTHEWS AND JALISA
MATTHEWS, by their guardian ad litem Lisa
Matthews, and PEOPLE UNITED FOR A
BETTER OAKLAND, On Behalf of
Themselves and All Others Similarly Situated,
Plaintiffs,
E
E
S
T
S
S
FR
EI
Wa
ol
e
0
Ve.
MOLLY COYE, M.D., Director, California
Department of Health Services,
[
S
S
~J
on
)
)
)
)
)
)
)
Defendant. :
—
Co
| o
o
T
E
ic
V
E
R
E
I, MARIDEE ANN GREGORY, declare:
1 1 am a Doctor of Medicine and a Board Certified Pediatrician. I have
N
N
N
e
spent my entire professional career since 1965 in the area of maternal and child health.
23 || I was first employed by the State Department of Health Services in 1981 as Chief of
24 || Maternal and Child Health. Since 1987 I have served as chief of the California
25 || Childrens Services Branch within the Department. I also serve as medical consultant to
26 || the Child Health and Disability Prevention Branch of the Department and have been
27 || the medical consultant in the drafting of program letters regarding lead screening and DECLARATION OF MARIDEE ANN GREGORY, M.D.
Jil 18 Sl adn PAGE .B1E
w
w
0
0
~
~
G
v
W
n
p
x
WW
N
N
Fo
SE
oF
E
E
2°
EE
r
t
c
d
a
d
m
R
=
SO
0
S
y
S
O
S
y
|
N
N
=
O
O
Ww
W
0
0
9
0
R
h
n
h
A
W
N
=
D
D
23
testing matters within the last four or five years.
2 The matters stated below are personally known to me and if called as a
witness I could and would testify competently concerning the same,
3 The Department of Health Services does not dispute the seriousness of
the problem of lead poisoning in children. In fact, as recently as March 12, 1991, the
Department’s former Director, Dr. Kenneth Kizer stated that: "Lead poisoning is the
most significant environmental health problem facing California children today, and
insufficient consideration is being given to this potential problem during routine child
health evaluations."y What the Department does dispute is whether either the law or
good medical practice requires the actual testing of children’s blood for the presence of
lead in all cases, and particularly very young children in the Early and Periodic
Screening, Diagnostic and Treatment ("EPSDT") Program of the Federal Medicaid
Program (known as the Medi-Cal program in California, and administered by the
Department of Health Services). |
4, The Department believes that neither applicable laws nor good medical
practice requires that all EPSDT children receive blood lead tests as a part of the
mandatory screening process. Rather, it is the Department's position that young (i.e,
under 6 years old) EPDST children should first be screened by their treating physicians
for both the presence of objective medical indications and/or environmental factors
which might indicate the possibility of lead toxicity. If either or both are present then
a blood test would be indicated. |
5 A blood test is an intrusive procedure which causes some degree of
discomfort, and in the vast majority of cases is simply unnecessary to determine
whether a child is at risk of lead poisoning. Further, there is a significant cost factor
involved in completing a blood test which must be considered in an age of limited
JUN 13
1. CDHP Provider Information Notice #91.6, included as Exhibit C in the
Exhibits In Support Of Plaintiffs’ Motion For Partial Summary Judgment.
2
DECLARATION OF MARIDEE ANN GREGORY, M.D.
SY Dean FREE B17
v
v
o
o
3
9
O
n
U
n
p
b
W
W
O
N
O
8
S
E
AS
E
E
r
l
a
r
d
ee
ee
oe
=
SE
=
SR
=
O
O
W
Y
0
0
0
«
3
‘
o
n
W
h
5
3
J
=
TD
resources, although the Department has been absolutely LA in its communications
with physician/providers that the cost of a blood test for lead is a covered cost in the
Child Health and Disability Prevention Program (see the penultimate paragraph of
CHDP Provider Information Notice #91-6). The message the Department sends to
physicians is that blood lead tests should be given to young EPSDT children whenever
and wherever medically indicated and that cost is not a factor -- good medical
judgment is.
6. While it is recognized that certain pediatricians advocate universal blood
lead testing for young children, that position is not universally shared. On March 3,
1987, the American Academy of Pediatrics published its Statement On Childhood Lead
Poisoning in its journal Pediatrics While recognizing as an ideal the concept of
anlversal blood lead testing, the Statement recognized that ". . . the incidence of lead
may be so low in certain areas that pediatricians may prudently consider their patients
to be at little risk of lead toxicity . . "& and set out priority guidelines to assist
pediatricians in deciding whether the need for a blood lead test was indicated.
i On June 4, 1991, I spoke by telephone with Raymond J. Koteras, M.H.A,,
Director of the Division of Technical Committees, of the Department of Maternal,
Child and Adolescent Health of the American Academy of Pediatrics. Mr. Koteras
confirmed to me that, while the matter of child blood lead testing is currently under
review by several Academy committees, the aforementioned Statement is and remains
the position of the Academy.
8. The Department believes that its position is consistent with the
requirements of the Health Care Financing Administration's ("HCFA") State Medicaid
Manual (included as Plaintiffs’ Exhibit N) wherein it is stated that a blood lead level
2. A copy of this Statement is attached hereto as Exhibit A.
3. Op. cit, at p. 463.
DECLARATION OF MARIDEE ANN GREGORY, M.D.
‘91 10:49 PAGE OLE
po
t
O
o
0
0
~
1
O
v
b
h
B
B
W
O
=
O
O
N
N
N
N
R
N
R
N
=
p
d
F
S
p
t
e
d
p
e
d
e
t
ea
d
~~
h
n
a
n
B
W
N
O
E
DO
O
W
O
0
0
N
h
l
R
W
N
R
C
assessment is mandatory where age and risk factors so inaicate. (Ex. N, at p. 5-14)
The Manual goes on to specifically require that all Medicaid eligible children ages 1-3
be screened for lead poisoning. However, the Manual section wherein the requirement
to screen is contained also contains several significant caveats concerning testing:
"Physicians providing screening/assessment services under the EPSDT program use their
medical judgment in determining the applicability of the laboratory tests or analysis to
be performed. ... As appropriate, conduct the following laboratory tests: . .. 1 In
general, use the EP test as the primary screening test." (Ex. N, at p. 5-14 through J-
15) Clearly, the ultimate decision as to whether a blood lead test should be given has
been left to the determination of the physician.
0. It is the present belief of the Department that universal blood lead
testing of young EPSDT children is not medically indicated, legally required nor fiscally
prudent.
I declare under penalty of perjury that the foregoing is true and correct.
Executed at Sacramento, California this 6th day of June, 1991.
Hunecdter Kom Biug ong Wp
DECLARATION OF MARIDEE ANN GREGORY, M.D.
EXHIBIT A
FAGE . B26 J 18 a0 10:80
Ef
a
. aT
pe
FE
8
*t
Kd
c
a
tn
tn
e
vr
ra
re
:
im
g
m
A
T
T
MEY
N
V
A
Go
ds
n
y
s
f
t
des
Le
m
T
a
H
e
Aq
Cle
h
o
li
en
El
ar
Er
a
L
R
S
T
C
R
R
N
pi
E
R
T
E
N
a
E
bs
.
e
a
pe
a
Lis.
+
To
e
h
d
d
p
T
Poa
gl
i
-
A
r
C
i
t
i
i
p
e
i
l
s
R
E
E
N
E
i
Committee on Environmental Hazards
Committee on Accident and Poison Prevention
Statement on Childhood Lead Poisoning
!
Lead remains a significant hazard to the health
of American children. Virtually all children in
the United States are exposed to lead that has been
dispersed in air, dust, and soil by the combustion
of leaded gasoline, Several hundred thousand chil-
dren, most of them living in older houses, are at
risk of ingesting lead-based paint as well as lead-
bearing soil and house dust contaminated by the
deterioration of lead-based paint. Although the in-
cidence of symptomatic lead poisoning and of lead-
related mortality has declined dramatically,’ date
from targeted screening programs’ and from a na-
tional survey” show that there are many asympto-
matic children with increased absorption of lead in
—
—
—
—
—
_
_
—
—
_
—
—
—
i
>
all regions of the United States. It is particularly
prevalent in areas of urban poverty.
Childhood lead poisoning can readily be detected
by_ simple and inexpensive screening’ techniques;
however, screening is sporadic and in some areas
not available. :
Despite wide recognition of the importance of
preventing children’s exposure to lead, state and
federal funding for the screening of children and
for the removal of environmental lead hazards has
diminished in recent years. Thus, pediatricians at-
tempting to address the problem of childhood lead
exposure face serious economic and administrative
obstacles to effective intervention,
This statement reviews current approaches to the
diagnosis, treatment, and prevention of lead poi-
soning, and it recommends steps to reduce the
pervasive impact of lead on children’s health. Some
of these recommendations are addressed to practi-
tioners and others to agencies of state and federal
government. It is important to recognize that vir-
tually all of these preventive steps are after the
fact, Ideally, in keeping with the precepts of pri-
mary prevention, lead should have been prohibited
from ever having become dispersed in the modern
environment.
PEDIATRICS (ISSN 0031 4005). Copyright © 1887 by the
American Academy of Padiatrics. ;
BACKGROUND AND DEFINITIONS
Lead has no biologic value. Thus, the ideal whole
blood lead level is 0 ug/dl.. According to the Second
National Health and Nutrition Examination Sur-
vey (NHANES II), conducted from 1876 to 1980,
the mean blood lead level in American preschool
children was approximately 16 ug/dL. Substantially
Jower lead levels are seen in persons remote from
modern industrialized civilization® and in the re-
mains of prehistoric men.
Until recently, whole blood lead levels as high as
30 ug/dL wera considered acceptable. However, dia-
turbances in biochemical function are demonstrable
at concentrations well below that figure, For ex-
ample, inhibition of 3-aminolevulinic acid dehy
drase, an enzyme important to the synthesis of
heme, occurs at whole blood lead levels below 10
pg/dL.¥® Also, the enzyme ferrochelatase, which
converts protoporphyriti to heme, is inhibited in
children at a blood lead concentration of approxi:
mately 156 pg/dL; thus, elevations in erythrocyte
protoporphyrin above normal background become
evident at blood lead levels above 15 pg/dL.? In
addition, depression of circulating. levels of 1,25:
dihydroxyvitamin D (the active form of vitamin D)
is seen at blood lead levels well below 25 ug/dL, 1!
Neuropsychologic dysfunction, characterized by
reduction in intelligence and alteration in behavior,
Ww
has been shown conclusively to occur in asympto:
matic children with elevated blood lead levels. et
The results of clitiical And epidefiiclogic “studies
matic childr
conducted in the United States,” Germany,” and
England" indicate clearly that blood lead levels
below 50 ug/dl. cause neuropsychologic deficits in |
asymptomatic children. Recent clinical and exper:
imental studies suggest that neuropsychologic dam:
age may be produced in children with blood lead
levels below 35 pg/dL.!®
Short stature, decreased weight, and diminished
chest circumferenre have recently been found in
analyses of data'ft,m the NHANES II survey to be
significantly associated with blood lead levels in
American children youngér. than 7 years of age,
PEDIATRICS Vol. 78 No. 3 March 1987 ~~ 457
PRISE. B21
after controlling for age, “= and nutritional earth’s crust, lea y be found in drinking water,
.gtatus. Although the effectN@le small, the results soil, and vegeta its Jow melting point, malles. ARNE
are statistically robust, bility, and high density, as well as its ability to form
In light of these data, an expert Advisory Com- alloys, have made lead useful for myriad purposes,
mittee to the Centers for Disease Control (CDC) --Many of these uses (eg, radiation shields, storage CHEE]
has determined that a blood lead level of 25 ug/dl. batteries) are not intrinsically dangerous, However,
or above indicates excessive lead absorption in chil- when lead is used for purposes other than intended IER
dren and constitutes grounds for intervention.) . (eg, burning of storage battery casings), when it js
Increased lead sbsorption was previously defined incorrectly applied or removed (eg, improper use of
by a blood lead level of 30 g/dL. Furthermore, the lead ceramic glazes, burning and sanding of old
CDC committee has now defined childhood lead leaded paint), when it is disseminated rather than
poisoning 8s a blood lead level of 25 ug/dL in reused (combustion of lead additives in automotive
association with an erythrocyte protoporphyrin fuels), or when it is improperly discarded, lead
level of 85 ug/dL or more.’ The Academy concurs enters the human environment in potentially haz-
in these definitions. Also, the Academy anticipates ardous form.
that as evidence of the low-dose toxicity of lead For purposes of estimating risk to children, bad
continues to develop, these definitions will be low. sources may be categorized as low, intermediate,
ered still further, and high dose (Table 1).
: : Low~Dose Sources. These sources of lead include ;
PREVALENCE OF LEAD POISONING air, food, and drinking watar, Together, these
Data from NHANES II? indicate that between EOUTCES, which have accounted for an average esti |
1976 and 1980 the national prevalence of blood lead ~~ ated blood lead concentration of approximately 3
levels of 30 ug/dL or hicher was 4% amonz Amer. 10 #8/dL in the recent past, probably now account 3
loart 0080 141 BL os High 5 years of age. ac for a blood level concentration of about 6 ug/dL. 2
this rate to US census data, it may be estimated Mean ambient air lead concentrations currently 3
that, between 1876 and 1980, 780,000 American Everage less than 1 ug/m’ of sir, although in areas
preschool children had excess levels of lead in their ~~ P&T lead smelters, concentrations may be Retin: 2
blood. In the NHANES II data, there was wide tially higher. et |
disparity in the prevalence of elevated blood lead Average dietary intake of lead increases from 20 4 ii Ht
levels between black children (12%) and white chil. #&/d during early infancy to 60 to 80 4g/d by 5 to" = x]
dren (2.0%) irrespective of social class or place of © Years of age. Except in isolated areas, it would: JE
residence. A similar disparity was noted in mean 2PPear that the majority of public drinking water 3 5
blood lead levels, which were 21 pg/dL in black supplies in the United States have a lead concen-. a |
preschool-aged children and 15 g/dL in white chil- tation of less than 20 g/dL. However, these data S4t=
dren of the same age. Prevalence rates for elevated T2Y be misleading if, as is generally the case, the “ZoE
blood lead levels were highest among families in Water samples have been obtained from the distri-
densely populated urban areas and in those with Pution plant prior to the distribution of water
incomes of less than $15,000 per year, However, it through a plumbing system that contains lead,
should be noted that cases of lead poisonings were pipes. The lead solvency of drinking water can be;
found also in families of higher income and in rura] ~ éduced by reducing acidity of water supplies an
settings. by abandoning the use of lead-based solder at pip
Between 1976 and 1980, the average blood lead J0ints in new and replacement plumbing. Compu
level in Americans of all ages decreased from 15.8 nities with excessive lead in water have successfully
t0 10.0 ug/dL according to the NHANES IL# This used each of these remedial approaches.
decrease coincided with a reduction in the use of TABLE 1. Common Sources of Lead
lead additives in gasoline. Additional factors in this Low Goce
_ reduction may have included a simultaneous reduc- Food
tion in the Jead content of foodstuffs, the impact of Ambient alr
targeted screening programs in high-risk areas, and Drinking watar
an increase in public awareness of the hazards of Intermediate dose
lead. Dust (housahold)
Interior paint removal
Soil contaminated by automobile accident
Industrial sources
: : Improper ve Envirenmenis Sources ali moval of exterior paint
Intsrior and sxterior pamt
SOURCES OF LEAD
Lead is ubiquitous. A natural constituent of the
458 LEAD POISONING
J
!
1
+
[4
H
I
}
Pont |
UF
a
—
—
—
—
—
—
—
—
—
—
r
r
a
0
e
S
B
a
r
SY
o
n
r
e
rag
: | 5 Intermediate-Dose Source
¥= clude dust and soil in children's play areas. Dust
¥. and soil are contaminated principally by automo-
hese sources in-
tive exhaust and by the weathering and deteriora-
i tion of old lead paint (both interior and exterior).
Although background soil lead contaminants in
3 rural areas are generally less than 200 ppm, concen-
BE {rations of lead in urban soil can exceed 8,000 ppm.
Ei In industrial areas where lead smelters have been
BE Gituated (eg, El Paso, TX; Kellogg, ID), the lead
: *" sontent of dust can, however, exceed 100,000 ppm,'®
5% thus producing significant elevations in children’s
L>. blood lead levels. Each increase of 100 ppm in the
: 4 ." lead content of surface soil above a level of 500 ppm
8%. is associated with a mean increase in children's
r
N
-
i
"
.
SAN
I
L
s
A
r
T
CS
S
E
A
N
ot
Ri
n:
snr
ri
de
r
i
d
A
T
T
o
m
e
p
t
a
u
t
4
I
T
E
R
L
O
R
E
L
S
E
pr
ic
e.
io
}
a
l
e
R
d
R
E
M
HE
RR
ETS
+
4
a
a
t
EE
Sk
ca
li
d
a
t
a
cs
La
o
*5
oy
—
—
—
3 2 whole blood lead levels of 1 to 2 pg/dL. When dust
and soil are the only sources of exposure to lead,
5 symptoms are rarely encountered, although lead
toxicity may occur. Soil lead may, however, be
‘extremely difficult to abate, and chronic low-grade
ingestion may continue undetected even after a
child has come to medical attention. The proper
sita for disposal of 1sad waste, such as Jsad-contam-
inated soil, is a hazardous waste facility that has
been approved by the US Environmental Protec-
tion Agency. :
High-Dose Sources. These sources are those in
which the concentrations of lead are sufficient to
produce acute and potentially fatal illness, Lead-
based paint on both the interior and exterior sur-
faces of housing remains the most common high.
dose source of lead for preschool-aged children. It
continues to be the experience of most pediatricians
that virtually all cases of symptomatic lead poison-
ing and blood lead levels greater than 70 ug/dL
result from the ingestion of lead paint chips.
Lead-based paint, is still widespread. A 1878 US
census survey found that 8 million of the 27 million
occupied dwellings in the United States, which had
been built prior to 1940 when use of lead-based
paint was common,?® were deteriorated or dilapi-
dated. An additional 22 million dwellings were built
between 1940 and 1960, and 76% of these units are
estimated to contain lead-based paint. Nationally,
according to the 1978 census survey of housing, 8%
of rental units have peeling paint.
Although the use and manufacture of interior
lead-based paint declined dramatically during the
1950s, exterior lead-based paint continued to be
available until the mid-1970s and is still available
for maritime use, farm and outdoor equipment, road
stripes, and other special purposes. Thus, potential
for domestic misuse of lead-based paint continues
to exist. Manufacturers could voluntarily decrease
the lead content of interior paint until 1977, when
the US Consumer Product Safety Commission en-
acted regulations ing the sale in interstate
commerce of paints yor exposed interior and exte-
rior residential surfaces containing ‘more than
0.08% lead by weight in final, dry solid form.
A previously unforeseen, but increasingly recog-
nized, danger is that of improper removal of load.
based paint from older houses during renovation
or, ironically, during cleaning to protect children.
"Torches, heat guns, and sanding machines are par-
ticularly dangerous because they can create a lead
fume. Sanding not only distributes lead as & fine
dust throughout the house but also creates small
particles that are more readily absorbed than paint
chips. The greatest hazard in paint removal appeats
to be to the person doing the “deleading” and to
the youngest children in the dwelling. There may
be significant morbidity, Persons who perform this
work should comply with the standards for occu-
pational exposure to lead which have been devel.
oped by the US Occupational Safety and Health
Administration. Pregnant women, infants, and
children should be removed from the house until
deleading is completed and cleanup accomplished.
Proper cleaning of the dust and chips produced in
deleading must include complete removal of all
chipping and peeling paint and vacuuming and
thorough wet mopping, preferably with high-phos-
phate detergents. This waste must be discarded in
a secure site, |
Another previously unrecognized hazard lies in
sandblasting. This technique is commonly used to
_ remove lead from exterior surfaces. There are no
standardized safeguards. Recent case reports of lead
poisoning among sandblasters underscore the haz-
ard. Sandblasting creates large amounts of lead-
laden dust and debris which, if improperly disposed
or not properly removed, redouble the hazard,
Uncommon Sources (Table 2)
Additional lead sources include hobbies such ‘as
artwork with stained glass and ceramics, particu-
larly when conducted in the home. Folk medicines
TABLE 2. Uncommon Sources of Lead
Metallic objects (shot, fishing weight)
Lead glazed ceramics
Qld toys and furniture
Storage battery casings
(Gasoline sniffing
Lead plumbing
Exposed lead solder in cans
Imported canned foods and toys
Folk medicines (eg, azarcon, Grata) -
Leaded glass artwork
Cosmatics
Antique pewter
Farm equipment hi
AMERICAN ACADEMY OF PEDIATRICS 459
PAGE . 827
Jead and mercuric or arseni
‘480
iiments may contain
alts. Recent reports
have noted lead poisoning from use of azarcon (lead
tetroxide)* and Greta (lead monoxide) among Mex-
ican-Americans and from use of Pay-loo-ah, a
used to treat gastrointestin
Chinese folk remedy,” among Hmong refugee chil- _
dren. Cosmetics (ceruse, surma, or kohl), particu-
larly those from Asia, may contain white lead or
lead sulfide®*” and have caused severe lead poison-
ing. Another source of lead is improperly soldered
cans, particularly those containing acidie food-
stuffs. Food should not be heated in such cans, as
heating increases the dissolution of lead. Pediatri-
cians should realize as a practical matter that the
lead content of imported earthenware toys, medi-
cines, or canned foods cannot readily be regulated,
In addition, antique toys, cribs, and utensils may
have a significant lead’ content.
Lead-glazed pottery is ‘a potential | source of lead
int food and drink, If not fired at high temperatures, ii
lead may be released from the glaze in large
amounts when such pottery is used for cooking or
for storage of acidic foodstuffs. Also, if pottery
vesgels are washed frequently, even a properly fired
glaze can deteriorate, releasing unsafe levels of pre-
viously adherent lead.” Sporadic cases of plumbizm
have been traced to lead-glazed pottery.®
Among the oldest sources of lead in America is
antique pewter. Food should not be cooked or stored
in antique pewter vessels or dishes. Although un-
common, many of the above sources have been
associated with severe, symptomatic, and even fatal
lead poisoning.
Finally, a number of cases of lead poisoning have
been reported among the children of workers in
smelters, foundries, battery factories, and other
lead-related industries. ® These workers can bring
home highly concentrated lead dust on their ekin,
shoes, clothing, and automobiles. This source of
exposure can be avoided by providing showers at
work, by providing workers with a change of cloth-
ing, and by having clothing laundered at the work-
place.
In summary, it can be inferred from the
NHANES I] data that most children in the United
States with increased lead absorption have been
#xposad to low-dose or to intermediate-dose lead
sources. Four percent of children have blood lead
levels in excess of 30 ug/dL, but only 0.1% have
levels exceeding 50 pg/dL.?
ROUTES OF ABSORPTION
Ingestion is the principal route of lead absorption
in children. Because of the high density of leadt®
ingestion of surprisingly small quantities may pro-
duce toxic effects. A lead paint chip weighing only
LEAD POISONING
. containing 5% le
lead poisoning. However, most ingested chips pre
"of the lead containad in them unavailable for ab-
tivenesé of normal hand-to-mouth activity ss =a
means for the transfer of lead-laden dust from the
though still an important risk factor, need not/be
sorption for children, Lead absorbed by way of the
‘Tungs contributes in additive fashion to the total
by ciliary action and then are either expectorated 3
Rk 1 em’ in purface area) and
weight will deliver a potential . I'§
dose of 50 mg (50,000 ug); by comparison, the safe ~i8
upper limit for daily intake of lead by children js 5 1%
pg/kg of body weight.) Because ingestion of such OJ
chips is not uncommon, it might be expected
large numbers of children would have symptomatic
1 g (approxima
swallowed whole or in barge pieces, rendering much
sorption.
Several recent studies have reported the effec- |
iR
Ba
d.
..
oi
a
i
n
iy
a
)
he
ar
th
i
C
o
p
rT
e
a
Pt
Sa
ga
=
-
"
x
y,
F
k
.
Fi
T
e
AOR
F
e
a
P
T
S
R
I
R
F
Rak
oo
ii
n
t
e
,
H
T
re
environment into children, ®* True pica (the in-
discriminate ingestion of nonfood substances), al
du
“a
d
ii
:
[TI
NY
present.
Inhalation is the second major route of lead ab.
body lead burden. The efficiency of respiratory 8
absorption depends on the diameter of airborne WE
lead particles, For most common lead aerosols of
mixed particle size, it has been estimated thet be. - 38
tween 30% and 50% of total inhaled lead is con- “H¥
tained in particles of sufficiently small diameter HE
(less than 5 um) to be retained in the Jungs and THR
absorbed. Larger particles deposit in the nose, ih
throat, and upper airways where they are cleajed SH
or swallowed. g
(x3
PREDISPOSING FACTORS J
Factors known to increase stsmeptiitity to lead
toxicity include nutritional deficiencies and age-
related oral behavior (with or without pica) (Table
3).
Anima] and human studies®’ have shown that ; 3
deficiencies of iron, calcium, and zine all resultiin “EEE.
increased gastrointestinal absorption of lead. of i: :
particular concern is the effect of lack of iron,” :X because the prevalence of iron deficiency in infancy &
is at least 156% and may be higher. * Iron deficiency, if
even in the absence of anemia, appears to be the*%
single most important predisposing factor for in a
creased absorption of lead, Conspicuous example
of nutritional iron deficiency include-breest.fed in-°
fants and “milk babies” who may receive little food 3
TABLE 3. Predisposing Factors for Lead Poisoning
Nutritional deficiency of iron, calcium, TrR2ANE |
Sickle cell diseases
Young age
Hand-to-mouth activity, including pica
Metabolic diseases
-,
FAGE . B2
-
r
d
i
(
L
p
SL
REN
-
oF
g
a
g
=
*
>
1
Pa
ce
v
3
L
a
b
da
4
n
-
L
E
B
r
i
J
fr
ie
&
ng
t
e
r
r
e
dt
:
A
ey
Sols
pied
dhe
,
f
o
r
t
=
: =
:
E
e
“=
.
i
b
.
iL
©
1
e
t
g
e
a
t
e
eb
=
Bother chan milk until 12 ("18 months of age. In
K...the presence of ifon deficiency insufficient to pro-
duce anemia, gastrointestinal absorption of lead is
2, increased aeveralfold.
SCREENING
Screening for lead poisoning is sporadic, Methods
used have included determination of blood lead
level, erythrocyte protoporphyrin level, or both,
A risk settings or with significant predisposing
BY - tors.'” To guide the interpretation of screen:
=. sults, the CDC has developed a series of guidelines
= (Tables 4 and §).
The erythrocyte protoporphyrin determination
provides a sensitive and inexpensive screen for both
increased lead absorption and iron deficiency, two
of the most common preventable health problems
in childhood; elevation in the erythrocyte proto-
porphyrin level can reflect iron deficiency before
anemia becomes clinically evident. There is increas-
ing interest, therefore, in adopting the erythrocyte
protoporphyrin determination as a screening tool
for both problems, particularly because it is more
sensitive to iron deficiency than the hematocrit. ™
Both capillary tubes and filter paper have been
B® ced for obtaining screening samples. Capillary
tubes are cumbersome but have the advantage of
providing sufficient blood for concomitant lead de-
TABLE 4. Zinc Protoporphytin by Hematofluorometer:
Risk Classification of Asymptomatic Children for Prior-
ity Medical Evaluation”
Erythrocyte
Protoporphyrin
: (ug/dL)
“35 35-74 75-174 >176
1 1
Ia 1
III IT1
II Iv
IV IV
* Diagnostic evaluation is more urgent than the classifi-
cation indicates for (1) children with any symptoms
compatible with lead toxicity, (2) children younger than
"36 months of age, (3) children whose blood lead and
erythrocyteprotoporphyrin levels place them in the upper
part of a particular-class, (4) children whose siblings are
in a higher class, These guidelines refer to the interpre-
tation of screening results, but the fina] diagnosis and
+ disposition reshon.a more complete medical and labora-
tory exanitpnioneiithe child,’
t Blood lead test-needed to estimate risk. bi
+ Erythropoietic. protoporphyria. Iron deficiency may
cause elavated erythrocyta protoporphyrifiievels up to
300 ug/dL, but this is rare. :
§ In practicgsthis combination of results is not generally
observed: ifi¥ is observed, immediately retest with whols
TABLE 6. erie Protoporphyrin (EP) by Extrac-
tion: Risk Classification of Asymptomatic Children for
Priority Medical Evaluation®
Blood Lead
(ug/dL)
Not done
EP (ug/dL)
«35 85-108 110-248
1 t t
1 Ia Ia
Ib II II
8 II go
i 4 NN
* Diagnostic evaluation is more urgent than the classifi-
cation indicates for (1) children with any symptoms
compatible with lead toxicity, (2) children younger than
38 months of age, (3) children whoae blood lead and EP
lavels place them in the upper part of a particular class,
(4) children whose siblings are in a higher class, These
guidelines refer to the interpretation of screening results,
but the final disgnosis and disposition rest on a more
complete medical and laboratory examination of the
child. Screening tests are not diagnostic, Therefore, every
child with a positive screening test result should be
referred to a physician for evaluation, with the degree of
urgency indicated by the risk classification. At the first
diagnostic evaluation, if the screening tast was done on
capillary blood, & venous blood lead level should be de-
tarmined in a laboratory that participates in the Centers
for Disease Control's blood lead proficiency-testing pro-
gram. Even when tests are done by experienced person-
nel, blood lead lavals may vary 10% to 15%, depending
on the level being testad. Tests for the same child may
vary as much as £5 ug/dL in a 24-hour period. Thus,
direction should not necessarily be Interpreted as indie-
ative of actual changes in the child's lead absorption or
excretion.
t Blood lead test needed to estimate risk.
} Ervthropoistic protoporphyria. Iron deficiency may
cause alevated EP levels up to 300 pg/dL, but this is rare,
§ In practice, this combination of results is not generally
Shietvad if it is observed, immediately retest with whole
blo ;
termination if the erythrocyte protoporphyrin level
is elevated. Filter paper sampling provides ease of
collection and transport, but the accuracy of anal.
yases based on filter paper samples is not yet estab-
lished. Determination of the blood lead level by
fingerstick sampling is subject to contamination by
lead on the skin, whether collection is by capillary
tube or filter paper. Such contamination does not
affect the determination of the erythrocyte proto-
porphyrin level,
Two analytical techniques are available for de-
termination of erythrocyte protoporphyrin: (1) ex-
traction of protoporphyrin from erythrocytes and
subsequent measurement in a fluorimeter and (2)
dirsct fluorimetry of a thin layer of RBCs (hema-
tofluorometer). Because values derived from these
two methods may differ (Tables 4 and 6), a pedia-
trician should be aware of which is in use. When in
doubt, the extraction method is preferred, because:
of its greater reprodudibility, particularly at lower
concentrations of erythrocyte protoporphyrin.
AMERICAN ACADEMY OF PEDIATRICS 461°
PAGE. OFS
i
}
!
It is most important that screening tests
are not diagnostic. EveM®child with a positive
screening test result should be referred to a pedia-
trician for further evaluation, with the urgency of
referral indicated by the risk classification (Tables
4 and 5). At the first diagnostic evaluation, if the
sereaning test was performed on capi od, &
venous blood lead level should be i p
“laboratory that participates in en aggredited blood
lead proficiency-testing program. To reduce the
RRSTooT ot TElseoetye roFalts, lead-free ay-
ringes, needles, and tubes must be used in obtaining
venous blood samples for lead analysis,
The developmentally disabled who reside in
“halfway houses” or cornmunity residences or who
attend school in older buildings deserve special
attention in lead-screening programs, Because this
population may be older than preschool age, pro-
tective statutes may not recognize their high-risk
status, particularly with respect to piea behaviors,
Physicians caring for developmentally disabled pa-
tients should be aware that their risk of lead inges-
tion may continue long beyond the age of & years.
INTERVENTION
Once a diagnosis of increased lead absorption has
been confirmed by venous blood lead determina-
tion, the sine qua non of intervention is the prompt
and complete termination of any further exposure
to lead.*® This intervention requires accurate iden-
tification of the source of lead and either its removal
or removal of the child from the unsafe environ-
ment, Some states (eg, Massachusetts) have passed
stringent legislation requiring prompt removal of
lead hazards in cases of lead poisoning, and there
are strong penalties for failure to comply. At all
costs, a child should not be permitted to enter or to
be present in a leaded environment during deleading
until the deleading, subsequent cleanup, and rein.
spection have been satisfactorily completed, Al-
though some regulations call only for removal of
leaded paint from “chewable” surfaces (eg, window
sills and door frames) or up to a height of 1.2 m (4
ft), all chipping and peeling paint should be re-
moved from all surfaces, particularly from ceilings,
After deleading, the house must be thoroughly
cleaned and reinspected to assure compliance with
safety regulations. Indeed, repeated thorough clean-
ing is advisable, especially in the case of deterio-
rated or dilapidated housing, High-phosphate de-
tergents are particularly useful in removing lead
dust. Children should not return home until ¢clean-
ing is completed.
Medical intervention should begin with thro-
rough clinical evaluation iIn®4ding diagnostic stud-
les of lead toxicity and, when indicated, & lead
mobilization test.** Diagnostic studies should in-
482 LEAD POISONING
clude a blood gl count with RBC indices, a retic-
ulocyte count, Qt, if indicated and available, tests
of serum iron and iron-binding capacity, and a
serum ferritin assay. Routine urinalysis might be
considered. Because chelating agents are poten-
tially nephrotoxic, BUN and/or serum creatinine
values should be determined before chelation to
rule out occult renal disease either secondary to
plumbism or preexisting,*’ Roentgenographic stud-
ies to be considered include & film of the abdomen
to detect radiopaque paint chips or other leaded
materials in the gastrointestinal tract and a film of
the metaphyseal plate of a growing “long” (bone,
usually the proximal fibula, to detect interférence
with calcium deposition, the so-called “lead line,”
Because this phenomenon is usually seen only after
several weeks of increased lead absorption in chil-
dren whose blood lead levels may exceed 50 ug/dL,
its presence or absence may help to determine the
duration of increased lead exposure.
Once a diagnosis of plumbism has been made, a
child's condition and the effect of intervention
should be monitored by serial venous determina-
tions of the blood lead and, if available, erythrocyte
protoporphyrin levels. If iron deficiency is présent,
iron studies should also be repeatad periodically to
monitor compliance with iron replacement therapy.
The lead mobilization test may be used to dssess
the “mobilizable” pool of lead in a child for whom
chelation therapy is contemplated. Lead moHiliza-
tion is determined by measuring lead diuresis in &
timed urine collection following a single dose of
chelating agent.®# This test is most helpful in
determining which children with blood lead concen-
trations in the range of 25 to 55 ug/dL will require
a full course of chelation therapy and also in deter-
mining the advisability of further chelation in a
child already receiving therapy. It should be noted
that the erythrocyte protoporphyrin level is hot a
useful predictor of the amount of chelatable lead
and may, in fact, be misleading in this regard.
-
e
r
p
b
i
h
aT
E
E
.
ai
s
r
r
Ay
SW
NH
BE
RL
IN
E
1
O
sc
E
R
E
:
-
-
'
-
=
EE
F
E
e
L
r
E
L
s
e
t
s
Therapeutic modalities include removing the -.;
child from lead exposure, improving nutrition,
administration of iron supplements, and chelation 3:
therapy.***~4" In children with mild increased lead
absorption, the efficacy of chelation therapy to ]
modify neurobehayioral outcomes-of-lead. toxicity
13 unproven: but, in children who have blood lead
levels between 25 and 55 pg/dL and a positive lead
mobilization test, it is highly desirable to rapidly
decrease the readily mobile, potentially most toxic
f
bs
ay
fraction of body lead stores by three to five days of >
CaNay-ethylenediaminetetraacetic acid (caltium 3)
disodium EDTA) therapy, *
Long-term follow-up is indicated in all cases of 2;
lead exposure. Children near or at school age who 70
have a history of plumbism should have a neuro- 2
a
n
e
B
t
t
e
h
e
r
s
i
x
D
E
a
a
>
a
*
-
—
—
—
k |
-
T
H
u
~
"
.
i
=
p
.
psychologic evaluation to » potential learn-
ing handicaps, and school authorities should be
8 encouraged to offer appropriate guidance.
RECOMMENDATIONS
Our recommendations rest on three premises: (1)
that exposure to lead is widespread; (2) that lead
causes neuropsychologic and other serious impair-
ments in children at relatively low levels of expo-
© sure; and (3) that the neuropsychologic effects of
: lead, even in asymptomatic children, are largely
irreversible. Guided by these premises, the goal of
>. our recommendations is to prevent lead absorption.
O
Pediatricians must play a central role in this
prevention. Although our recommendations are di-
vided into two categories—those directed princi-
pally to practitioners and those directed to govern-
ment agencies——the distinction is somewhat artifi-
cial. Throughout the past five decades, pediatri-
cians, acting individually, as well as collectively
through the Academy, have been prime movers in
stimulating the agencies of government to protect
the children of the United States against exposure
to lead. It is important that this tradition of public
involvement continue and that pediatricians con-
tinue to act publicly as advocates for the health of
children.
Recommendations for Practitioners
1. The Academy recommends that the erythro-
cyte protoporphyrin test be used for screening chil-
dren for lead toxicity, when that test is available.
Additionally, the erythrocyte protoporphyrin test
is a sensitive indicator of subclinical iron deficiency
and may add complementary information to the
determination of hematocrit values. It will not,
however, identify children with anemia due to acute
blood loss or hemoglobin C, 88, 8C, or E disease.
The Academy encourages clinical and hospital lab-
oratories to make the erythrocyte protoporphyrin
test widely and economically available,
2, Upon consideration of recent CDC recommen-
dations, the Academy recommends tnat, 1aeally, all
‘preschool children should be screened tor ead ab-
sarption.by_mesns..of the srihrooyie DIAG
Dv Lh uel in-
cidence of Si exXpOosy ow ip certain
areas that pediatricians may. Sr consider
their patients to be at little risk of Tead toxicity;
therefore, the following priority y guidelines ranked’
from -highegt, to lowest are offered to assist ¢ pedia-
tricians in deciding which children to sci to screen. (a)
children, 12 12 1 10.36 months of ' age, | who Ii live ir in or are
frequent visitors in ol older, _dil lapidated housing
(highest); (b) children, 8 power of to 6 years of age,
who are siblings, housemates, ‘visitors, ang, play-
d toxicity; (c)
lire, none gs ap I ie
lead smelters and processing pl »
«amis or.other househo es
lead-rela ation or ‘hobby. Frequency
screening should be flexible but should be guided
by consideration of a child's age, nutrition and iron
status, and housing age, housing condition, and
population density. The first erythrocyte protopor-
phyrin test should generally occur at the same time
as the determination of the hematocrit, which typ-
ically is performed between 9 and 15 months of age.
Because the prevalence of lead poisoning increases
sharply at 18 to 24 months of age, any child judged
to be at elevated risk of plumbism should have ia
second erythrocyte protoporphyrin test performed
at or about 18 months of age and at frequent
intervals (3 to 6 months) thereafter appropriate to
the degree of risk. Surveillance should continue
routinely up to age 6 years and, if appropriate,
longer.
3. The Academy sidommends that any child, in
whom increased lead absorption or lead poisoning
has been confirmed by venous blood lead determi-
nation, be followed closaly by means of repeat ve-
nous tests. For such children, ‘abatement of envi-
ronmental sources of lead is essential.
4. The Academy notes that some predisposing
factors for lead poisoning, iron deficiency in partie-
ular, are preventable. Pediatricians should make
vigorous efforts to identify and correct iron defi.
ciency, calcium deficiency, and other nutritional
deficiencies, particularly in children from areas of
high lead exposure.
5. The Academy recommends that pediairiclavs
attempt vigorously to educate parents, particularly
parents of children in high-risk populations, about
the hazards of lead, its sources and routes of ab-
sorption, and safe approaches to the prevention of
exposure. :
Recommendations for Public Agencles
1. The Academy recommends that reporting of
cases of lead poisoning to state health departments
be mandatory in all states.
2. The Academy notes that, in the present ap-
proach to screening for lead, inspection of a child's
environment is generally undertaken only when an
elevated blood lead level is found. In effect, children
are used as biologic monitors for environmental
lead. The Academy recommends that this sequence
be reversed. A national program for systematic
screening of lead hazards in housing is overdue.
The enormity of the task favors a stepwise ap-
AMERICAN ACADEMY OF PEDIATRICS 463
a
y
—
—
n
e
t
—
—
—
—
—
—
—
—
—
proach. Suggested ap hes might include:
screening of oldest houMg, followed by newer
housing; screening of housing in inner cities, then
in less densely populated areas; and targeted
screening of housing with small children.
8. The Academy supports the prompt, vigorous,
and safe abatement of all environmental lead haz-
ards. The US Department of Housing and Urban
Development, state health departments, and local
health departments should require that all hazard.
ous lead-based paint (exterior and interior) be re-
moved from all housing. Development of methods
of abatement, which are safer and more effective
than those currently in use (torches, heat guns, and
sanders) must be given high priority to prevent the
further endangering of lead-poisoning victims. The
US Environmental Protection Agency is urged to
persist in its laudable plan to promptly and finally
remove all lead from gasoline.
4. The Academy urges the US Congress and the
US Department of Health and Human Services to
become fully cognizant of the high prevalence of
childhood lead poisoning in the United States, its
irreversible consequences, and its great human and
fiscal costs. Restoration of funding is urgently
needed for screening, hazard identification, and
hazard abatement.
5. The Academy recommends that state health
departments and Academy chapters exert their
maximum influence to assure that state licensing
agencies permit laboratories to perform blood lead
and erythrocyte protoporphyrin tests only if those
laboratories consistently meet criteria for accuracy
and repeatability as determined by their perform-
ance in interlaboratory proficiency-testing pro-
STAs.
SUMMARY
Patterns of childhood lead poisoning have
changed substantially in the United States. The
mean blood lead level has declined, and acute in-
toxication with encephalopathy has become uncom-
mon, Nonetheless, between 1976 and 1880, 780,000
children, 1 to 8 years of age, had blood lead concen-
trations of 30 ug/L or above. These levels of ab-
sorption, previously thought to be safe, are now
known to cause loss of neurologic and intellectual
function, even in asymptomatic children. Because
this logs is largely irreversible and cannot fully be
restored by medical treatment, pediatricians’ ef-
forts must be directed toward prevention. Preven-
tion js achieved by reducing children’s exposure to
lead and by early detection of increased absorption.
Childho&# lead poisoning is now defined by the
Academy as a whole blood lead concentration of 25
ug/L or more, together with an erythrocyte proto-
464 LEAD POISONING
- ‘ACKNOWLEDGMENT
porphyrin ley 35 pg/dL or above, This defini-
tion does not 6 the presence of symptoms. Jt
is identical with the new definition of the US Public
Health Service. Lead poisoning in children previ-
ously was defined by a blood lead concentration of
30 pg/dL with an erythrocyte protoporphyrin level
of 50 ug/dL.
To prevent lead exposure in children, the Acad. = SF"
emy urges public agencies to develop safe and effee-
tive methods for the removal and proper disposal
of all lead-based paint from public and private
housing, Also, the Academy urges the rapid and
complete removal of all lead from gasoline, |
To achieve early detection of lead poisoning, the,
Acade ends ildren in the
United States at risk of exposure to lead be screens
“for lead absorption at ApproTimataly. 12 months of
“2ge by means of the i Tin
test, when that test is available, Furthermore, the
Academy recommends follow-up erythrocyte pro-
toporphyrin testing of children judged to be at high
risk of lead absorption. Reporting of lead poigoning
should be mandatory in all states. :
Wa are grateful for the assistance of J, Julian CHisolm, Bi
Jr, MD, Jane L. Lin-Fu, MD, Vernon Houk, MD, John :/g&
Stevenson, MD, and John F. Rosen, MD. : "EE
COMMITTEE ON ENVIRONMENTAL.
- HAZARDS, 1984-1986
Philip J. Landrigan, MD, Chairman
John H. DiLiberti, MD
Stephen H. Gehlbach, MD
John W. Graef, MD
James W. Hanson, MD
Richard J, Jackson, MD
Gerald Nathenson, MD
Liaison Representatives
Henry Falk, MD
Robert W, Miller, MD
Walter Rogan, MD
Diane Rowley, MD 3
COMMITTEE ON ACCIDENT AND Pd1sON | Ji
PREVENTION, 1984-1988 :
Joseph Greensher, MD, Chairman |
Regine Aronow, MD :
"Joel L, Bass, MD
William E. Boyle, Jr, MD
Leonard Krassner, MD
Ronald B. Mack, MD
Sylvia Mieik, MD
Mark David Widome, MD
Liaison Representatives
Andre I’Archeveque, MD
PAGE . B28
t
r
-
—
—
—
a
e
.
3
ow
ay
A
a
r
y
-
:
f
s
G
a
.
i
| o
e
C
JH
1
Gerald M. Breitzer®00
Chuck Williams, MD
AAP Section Liaison
Jerry Foster, MD
Joyce A. Schild, MD
ft REFERENCES
Centers for Dissase Control: Burveillancs of childhood lead
poisoning—United States, MM WR 1882;31:132-134
2. Mahaffey KR, Annast JL, Roberts J, et al: National eati.
matas of blood lead levels: United States 1978-1980: Asso-
ciated with selectad demographic and socioeconomic factors,
N Engl J Mud 1882;807:573-579
8, Klein R: Lead poisoning, Adv Pediatr 1077;24:108-132
8
7
+ 4. Annest JL, Pirkle JL, Makue D, et al: Chrondlogical trend
in blood lead levels between, 1976 and 1080, N Engl J Med
1883:808:1873-1877
. Plomall 8, Corash L, Coraah MB, et zl: Blood jaad concen-
trations in A remote Himalayan population. Sciange 1980;
210:1136-1137
Grandjean P, Fjerdingstad E, Nielsen OV: Lead concentra-
tion in mummified nubian brains, Pressntad at the Intsr-
national Conference on Heavy Mstals in the Environment,
Toronto, Canada, Oct 27-31, 1975
Hernbarg 8: Biochemical and clinical effacts and rRBpONEES
as indicated by blood concentration, in Singhal RL, Thomas
J8 (eds): Lead Toxicity. Baltimore, Urban & Schwarzenberg,
Ine, 1880
. Berlin A, Schaller KH, Grimes H, ot al: Environmental
exposure to lead: Analytical and epidemiological investiga.
. tions using the European standardized method for blood
11
12,
18.
14.
15,
16.
12. Centers for Dissage Control: Pray
_-young children. MMWR 1885;34:67-68
delta-aminolevulinic acid dehydratase activity determina.
tion. Int Arch Occup Environ Haalth 1877;38:135~141
_ Piomell §, Seaman C, Zullow D, at al: Threshold fot lead
damage to ham synthesis i in urban children. Proc Natl Acad
Sei USA 1682;79:3335-3338
. Mahaffey KR, Rosan JF, Chesney RW, at al: Association
batwean age, blood lead concentration, and ssrum 1,25.
dihydrozycalcifaro] lavels in children, Am J Clin Nutr
1982:35:1327-1331
Rossn JF, Chesney RW, Hamstra A, et al: Reduction in
125-dihydroxyvitamin Dio children with increased lead
absorption. N Engi J Med 1880;302:1128-1131
Needlernan H, Gunnoe C, Leviton A, ut al: Deficits in
paychologie and classroom performance of children with
elevated dentine lead levels, N Engl J Med 1879;300:885-
695
Winneke G, Kramer G, Brockhaus A, st al: Neuropsycho-
logical studies in children with elevated tooth lead concen-
tration. Int Arch Occup Environ Health 1982:51:169-183
Yule W, Lansdowne R, Millar IB, et al: The relationship
between blood lead concentrations, intelligence and attain-
ment in a school population: A pilot study. Dev Mad Child
Naurol 1881:23:5687-576
Rutter M: Low leval lead exposure: Sources, affects, and
implications, in Rutter M, Jones RR, (ads): Lead vs. Health,
Naw York; John Wiley & Sons, 1883, pp 333-370
Schwartz J, Angle C, Pitcher H: Relationship batween child-
hood blood Jead lsvels and stature, Pediatrics 1986;77:281-
288
venting lead poisoning in
1%; Landrigan PJ, Gehlbach ARSE BF, et al; Epidemic
lead absorption near an ore smelter: The role of particulata
lead N Engl J Med 1975; 292:128-122
18. Assessment of the Safety of Lead and Lead Saits in Food: A
20.
Report of the Nutrition Foundation’s Expert Advisory Com.
Wttee, Washington, DC, The Nutrition Foundation, 1982
Bureau of the Cansus. Statistics! Abstracts of the Unitad
States, 1980, ed 101. Washington, DC, US Department of
Commerce, 1880
21.
22.
24.
25.
26.
27.
28,
30,
aL
32.
33.
8,
35.
Bureau of the colli: Housing Survey, 1978, Cur-
rent Housing reporta series H-150-78. Washington DC, US -
Department of Commerce, 1879
Fischbein A, Anderson KE, Sassa 8, et al: Lead poisoning
from “do-it-yourself” heat guns for removing lead based
paint: Report of two cases, Environ Ras 1981;24:425-431
23. Landrigan PJ, Baker EL, Himmelstein JS, ot al: E
to lsad from the Mystic river bridge: The dilemma of
leading, N Engl J Med 1882;308:873-878 .
Bose A, Vashistha K, O'Loughlin Bd: Azareén por Empa-
cho—Another cause of lead toxicity, Pediatrics 1988.72: 106-
108
Centers for Discase Control: Folk ramedy-aasociated | ad
poisoning in Hmong ¢hildren-—Minnesota, MMWR 18
32:556-666
Ali AR, Smalls ORC, Aslam M: Surma and lead poisoning.
Br Med J 1878;3:815+818
Shaltout A, Yaish 8A, Fernando N: Laad encephalopathy in
infants in Kuwait. Ann Trop Paediatr 1981;1:2080-215
Miller C: The pottery and plumbism puszle, Med J Austr
1882:30:44 2-443
29, Ostarud HT, Tufts E, Holmes M8: Plumbism at the Green
Parrot goat farm. Clin Toxicol 1978:8:1-7
Baker EL Jz, Folland DE, Taylor TA, et al: Lead poisoning
in lead workers and their children: Home contamination
with industrial dust. N Engl J Med 1977:206:260-261
Chisolm JJ Jr: Fouling one's own nest. Pediatrics
1078;62:61 4-817
Ziegler EE, Edwards BB, Jansen RL, ot al: Absorption and
retention of lead by infants. Pediatr Res 1978;12:26-34
Roels HA, Buchet JP, Lauwerys RR, et al: Exposure to lead
- by the oral and the pulmonary routes of children living in
tha vicinity of a primary lead amelter. Environ Res
1980,22:81-94
Bayre JW, Charney E, Vostal J, ot al: House and band dist
as a potential source of c lead exposure. Am J Dis
Child 1974;127:187-171
Charney E, Kessler B, Farfel M, ot al: Childhood ui
poisoning: A controlled trial of the effect of dust-eon
Bees on blood lead levels, N Engl J Med 1083;308:1
109
38. Barltrop D: ‘The prevalence of pica. Am J Dis Chi
37.
1566;112:116-128
Mahaffey KR: Nutritional factors in lsad poisoning, Nutr
Rev 1981:39:353-362
38. Nathan D, Oski F: Hematology of Infancy and Childhood, ed
a8.
40.
41.
42,
47,
AMERICAN ‘ACADEMY OF PEDIATRICS
2 Philadelphia, WE Saundars Co, 1881
Yip R, Schwartz 8, Deinard AS: Screening for iron deft-
clancy with tha srythrocyte protoporphyrin test. Pediatrics
1983:72:214-219
Piomelli 8, Rosen JF, Chisolm JJ Jr, ot al: Management of
childhood lead poisoning. J Padiatr 1684;105:523-532
Praventing Lead Poisoning in Young Children, publication
No. 00-2629. Atlanta, Centers for Disease Control, April
1878
Blickman JH, Wilinson R, Grasf J: The isad ling revisited
AJR 1086;74:88-83
Markowitz ME, Rosen JF: Asssssment of lead stotesiin
children: Validation of 8-hour CaANa*EDTA provocative tést,
J Pediair 1884;104:337-341
. Taisingsr J, Srbova J: The value of mobilization of lead by
calcium sthylene diaminetetrancetate in the diagnosis of
lead poisoning. Br J Ind Med 1558;18:148-153
. Chisolm JJ Jz, Baritrop D: Recognition and management of
children with increased lead absorption. Arch Diz Child
1979;64:248-262
Graef JW: Clinical outpatient management of childhood
lead poisoning, in Chisolm JJ Jr, O'Hara D (ads): Lead
Absorption in Children. Baltimore, Urban & Schwarzenberg,"
1882, pp 153-184
Chisolm JJ Jr: Management of increased lead shsorphiott?
Nustrative cases, in Chisolm JJ Jr, O'Hara D (eds): Lead
Absorption in Children. Baltimore, Urban & Schwarzenberg,
1882, pp 172-182 4
FRIGE .
465"
5
DANIEL E. LUNGREN, Attorney General
of the State of California
CHARLTON G. HOLLAND, III
Assistant fsusy paul
STEPHANIE W orl
may General
yi} “hg i fy 12th Floor
i 94612-3042
Pelephone: (415) 464-1173
Attorneys for Defendant
UNITED STATES DISTRICT COURT
NORTHERN DISTRICT OF CALIFORNIA WV
O
D
O
w
h
o
r
E
&
I
N
N
ee
11 | ERIKA MATTHEWS AND JALISA ) No. C 90 3620 EFL
§ MATTHEWS, by their ad Hiem Lisa
12 | Matthews, and PEOPLE UNITED FOR A DECLARATION OF RUTH 8.
BETTER OAKLAND, On Behalf of RANGE, MPH. P.HN.
13 || Themselves and All Others Similarly Stinated,
14 Plaintifls,
15 Ya
16 | MOLLY OD Director, Califbrnin
Department of Health Services,
Defendant.
“
a
r
a
t
Me
pt
e
t
ew
“a
”
“a
gr
™
va
nt
’
20 { I, RUTH 8S. RANGE, declare:
21 1. 1hold an M.S, degree in Nursing. I have spent my entire professional
22 { carcer stocu 1958 in the area of public health, 1 have been employed by the State
23 {| Department of Health Services since 1977 as Chief of the Regional Operations Section
24 || of the Child Health and Disability Prevention Branch of the Departinent. As such I
25 { have been significantly involved in lead screening and testing matters within the Jast
26 || decade.
27 2. The matters stated below are personally known to me and if called as a
L
DECLARATION OF RUTH 8. RANGE, M.S. PHN.
JUN 18781 1 180 PAGE . B30
QO
oN
d
C
W
e
W
N
T
I
a
W
y
&
WB
W
w
=
0
9
witness I could and would testify competently concerning vd SRTDE,
3 The Department of Health Services does not dispute the seriousness of
the problem of lead poisoning in children, In fact, as recently as March 12, 1991, the
Department's former Director, Dr, Kenneth Kizer stated that: "Lead poisoning is the
most significant environmental health problem facing California children today, and
ingufficient consideration is being given to this potential problem during routine child
health evaluations™ What the Department docs dispute is whether either the law or
good medical practice requires the actual testing of children’s blood for the presance of
lead in all cases, and particularly very young children in the Early and Periodic
Screening, Diagnostic and Treatment ("EPSDT") Program of the Federal Medicaid
Program (known as tho Medi-Cal program in California, and administered by the
Department of Health Services).
4, The Department belicves that neither applicable laws nor good medical
practice requires that all EPSDT children receive blood lead tests as a part of the
mandatory screening process. Rather, it is the Department's position that young (is.
wnder 6 years old) EPSDT children should first be screensad by their treating physicians
for bath the presence of objective medical indications and/or environmental factors
I which might indicate the possibility of lead taxicity, If cither or both are present the
a blood test would be indicated. While the State Medicaid Manual (Plaintiffs’ Exhibit
N) recommends the erythrocyte protoporphyrin (“EP”) test as the "primary screening
test” (Ex. N, at p. 5-15), this test is falling into disfavor due 10 its relative unreliability
vis-a-vis a blood lead test. (The former is a "pinprick” tat while the latter draws a
sample of venous blood.)
5. A blood test is an intrusive procedure which causcs some degree of
discomfort, and in the vast majority of cases is simply unnecessary to determine
1. CDHPF Provider Information Notice #91-6, inchudad as Exhibit C in the
Exhibits In Support Of Plaindffs’ Motion For Partial Summary Judgment,
2 DECLARATION OF RUTH B, RANGE, M8, PHN.
| »
whether a child is at risk of lead poisoning. Further, there is a significant cost factor
involved in completing a blood test which musi be considered In an age of limited
resources. In Fiscal Year 1989-00 Department records indicate that there were 539,576
children under the age of six in the Medi-Cal program. The cost of an EP test is
$7.50, so the total cost of providing each of these children with such a test would be
$4,046,820. The cost of the moro reliable blood lead test is $22.50, so the total cot of
providing each of these children with such a test would be $12,140,460, |
6. It is the present beliaf of the Department that universal blood lead
testing of young EPSDT children is not medically indicated, legally required nor fiscally
prudent.
W
O
sd
O
h
W
h
B
W
N
e
S
e
No
=
D
I declare under penalty of perjury that the foregoing is true and correct.
Executed at Sacramento, California this 7th day of June, 1991.
: gt i
* » 4
P
e
N
S
A]
N
E
B
R
B
E
3 DECLARATION OF AUTH 4. RANGE, M3, PHN,
TN IE ral 11a a BE CoE